The Efficacy of the RME II System Compared with the Sander Bite-Jumping Appliance: A Retrospective Study
Abstract
1. Introduction
2. Material and Methods
- (1)
- Full Class II molar relationships;
- (2)
- Overjet of >5 mm;
- (3)
- Skeletal Class II division 1 malocclusion with mandibular retrusion assessed by cephalometric evaluation;
- (4)
- Age between 9 and 13 years;
- (5)
- Skeletal age between CS2 and CS3 according to the cervical vertebral maturation method.
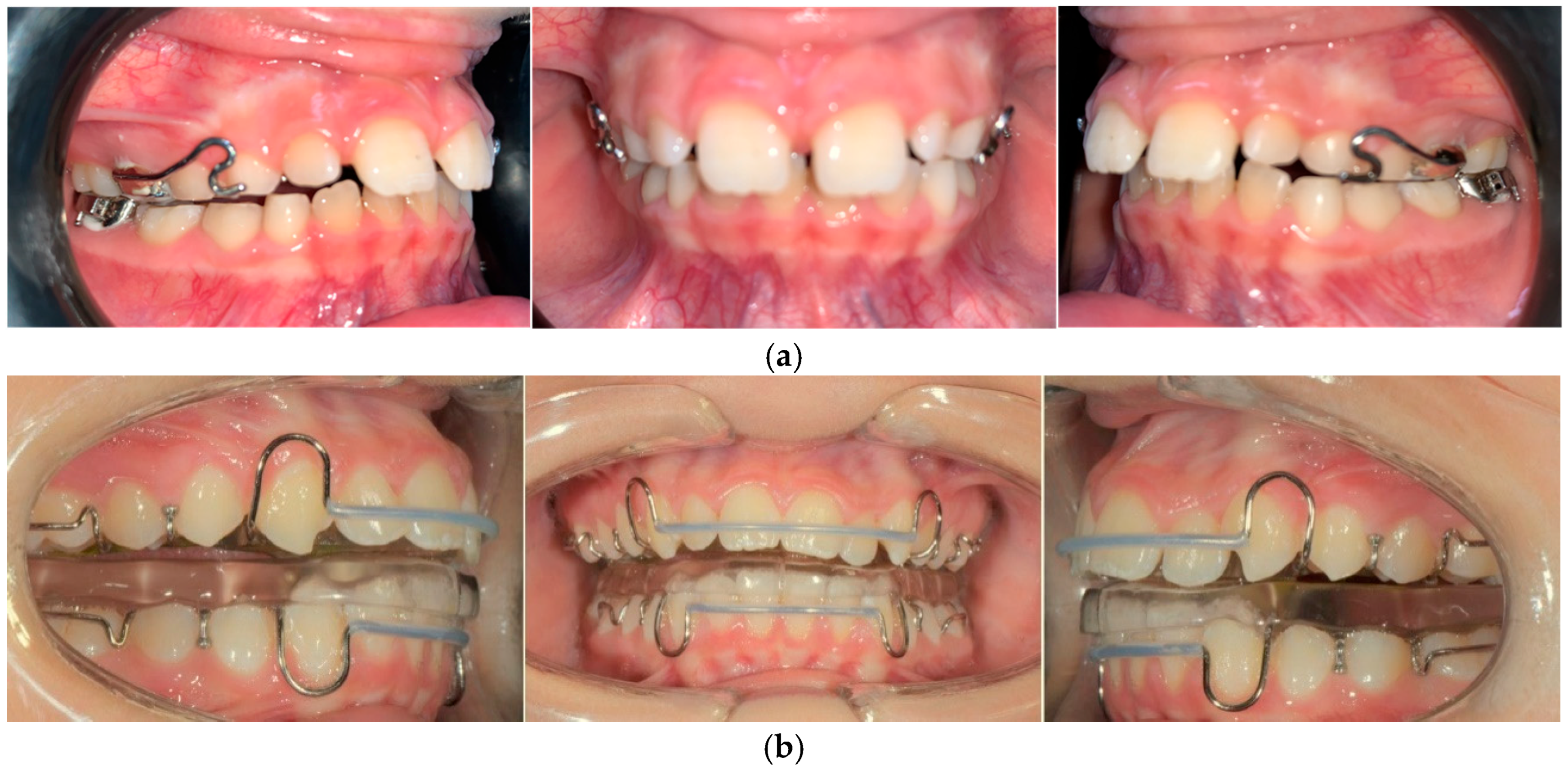
2.1. Group R
2.2. Group S
2.3. Group C
2.4. Cephalometric Analysis
2.5. Statistical Analysis
3. Results
| Group R | Group S | Group C | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T0 | T1 | p | T0 | T1 | p | T0 | T1 | p | |||||||
| Mean | Std Dev. | Mean | Std Dev. | Mean | Std Dev. | Mean | Std Dev. | Mean | Std Dev. | Mean | Std Dev. | ||||
| SN-MP | 34.41 | 4.23 | 32.87 | 4.51 | 0.001 | 33.92 | 4.24 | 32.08 | 4.61 | 0.55 | 34.21 | 3.76 | 33.76 | 3.95 | 0.05 |
| LFH | 65.29 | 6.21 | 64.33 | 4.71 | 0.396 | 61.94 | 4.98 | 64.80 | 5.31 | 0.001 | 64.11 | 9.24 | 63 | 8.80 | 0.372 |
| CO-GN | 101.7 | 4.79 | 106.6 | 4.29 | 0.001 | 100.7 | 6.41 | 105.1 | 6.31 | 0.001 | 103.9 | 12.6 | 103.4 | 13.93 | 0.4 |
| 1 + SN | 106.4 | 7.18 | 103.8 | 5.29 | 0.031 | 106.20 | 5.65 | 103.74 | 6.04 | 0.03 | 107 | 4.78 | 105.9 | 5.78 | 0.001 |
| IMPA | 95.33 | 6.37 | 96.2 | 6.19 | 0.863 | 93.77 | 8.1 | 97.48 | 8.46 | 0.001 | 90.85 | 6.43 | 91.18 | 7.18 | 0.354 |
| Overbite | 1.61 | 1.54 | 2.84 | 1.26 | 0.001 | 2.73 | 1.94 | 1.85 | 1.03 | 0 | 3.37 | 3.16 | 3.72 | 1.40 | 0.002 |
| Overjet | 6.81 | 1.78 | 3.34 | 1.24 | 0.001 | 7.73 | 2.17 | 3.81 | 1.12 | 0.001 | 6.31 | 1.55 | 5.5 | 2.51 | 0.005 |
| ANB | 5.57 | 1.11 | 2.78 | 0.89 | 0.002 | 5.84 | 1.16 | 3.96 | 1.02 | 0.001 | 5.61 | 1.5 | 5.2 | 1.01 | 0.22 |
- (1)
- The divergence angle was 1.81° greater in the control group than in the RME II System group, and 2.51° greater in the Sander group compared to the RME II System group;
- (2)
- Lower facial height (LFH) was 5.46 mm greater in the control group than in the RME II System group, and 3.11 mm greater in the Sander group compared to the RME II System group;
- (3)
- The mandibular length (CO-GN) was 4.33 mm shorter in the control group than in the RME II System group and 6.08 mm shorter in the control group compared to the Sander group;
- (4)
- Lower incisor inclination (IMPA) was 3.34° lower in the control group than in the Sander group and 4.01° greater in the Sander group compared to the RME II System group;
- (5)
- The overbite was 3.07 mm greater in the control group than in the Sander group and 1.96 mm lower in the Sander group compared to the RME II System group;
- (6)
- The overjet was 3.59 mm greater in the control group than in the RME II System group and 4.88 mm greater in the control group compared to the Sander group;
- (7)
- The ANB angle was 2.15° greater in the control group than in the RME II System group and 1.38° greater in the Sander group compared to the RME II System group.
4. Discussion
Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Zhao, H.; Sun, R.; Cao, S.; Han, J. Treatment of Class II Malocclusion with Orthodontic Microimplant Anchorage. Int. Dent. J. 2024, 74, 536–542. [Google Scholar] [CrossRef] [PubMed]
- Geiger, A.M. Malocclusion as an etiologic factor in periodontal disease: A retrospective essay. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 112–115. [Google Scholar] [CrossRef] [PubMed]
- De Ridder, L.; Aleksieva, A.; Willems, G.; Declerck, D.; Cadenas de Llano-Pérula, M. Prevalence of Orthodontic Malocclusions in Healthy Children and Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 7446. [Google Scholar] [CrossRef]
- McNamara, J.A., Jr.; Peterson, J.E., Jr.; Alexander, R.G. Three-dimensional diagnosis and management of Class II malocclusion in the mixed dentition. Semin. Orthod. 1996, 2, 114–137. [Google Scholar] [CrossRef]
- Gao, J.; Wang, X.; Qin, Z.; Zhang, H.; Guo, D.; Xu, Y.; Jin, Z. Profiles of facial soft tissue changes during and after orthodontic treatment in female adults. BMC Oral Health 2022, 22, 257. [Google Scholar] [CrossRef] [PubMed]
- Santori, F.; Masedu, F.; Ciavarella, D.; Staderini, E.; Chimenti, C.; Tepedino, M. Effect of Class II functional treatment on facial attractiveness, as perceived by professionals and laypeople. Sci. Rep. 2021, 11, 13989. [Google Scholar] [CrossRef]
- Booij, J.W.; Kuijpers-Jagtman, A.M.; Bronkhorst, E.M.; Livas, C.; Ren, Y.; Kuijpers, M.A.; Katsaros, C. Class II Division 1 malocclusion treatment with extraction of maxillary first molars: Evaluation of treatment and post-treatment changes by the PAR Index. Orthod. Craniofacial Res. 2021, 24, 102–110. [Google Scholar] [CrossRef]
- Evrard, A.; Tepedino, M.; Cattaneo, P.; Cornelis, M. Which factors influence orthodontists in their decision to extract? A questionnaire survey. J. Clin. Exp. Dent. 2019, 11, e432–e438. [Google Scholar] [CrossRef]
- Tepedino, M.; Esposito, R.; Potrubacz, M.I.; Xhanari, D.; Ciavarella, D. Evaluation of the relationship between incisor torque and profile aesthetics in patients having orthodontic extractions compared to non-extractions. Clin. Oral Investig. 2023, 27, 5233–5248. [Google Scholar] [CrossRef]
- Verma, S.L.; Sharma, V.P.; Singh, G.P.; Sachan, K. Comparative assessment of soft-tissue changes in Class II Division 1 patients following extraction and non-extraction treatment. Dent. Res. J. 2013, 10, 764–771. [Google Scholar]
- Ceratti, C.; Serafin, M.; Del Fabbro, M.; Caprioglio, A. Effectiveness of miniscrew-supported maxillary molar distalization according to temporary anchorage device features and appliance design: Systematic review and meta-analysis. Angle Orthod. 2024, 94, 107–121. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.M.; Inchingolo, A.D.; Carpentiere, V.; Del Vecchio, G.; Ferrante, L.; Di Noia, A.; Inchingolo, F. Predictability of Dental Distalization with Clear Aligners: A Systematic Review. Bioengineering 2023, 10, 1390. [Google Scholar] [CrossRef]
- Brierley, C.A.; DiBiase, A.; Sandler, P.J. Early Class II treatment. Aust. Dent. J. 2017, 62 (Suppl. S1), 4–10. [Google Scholar] [CrossRef] [PubMed]
- McNamara, J.A., Jr.; Franchi, L. The cervical vertebral maturation method: A user’s guide. Angle Orthod. 2018, 88, 133–143. [Google Scholar] [CrossRef]
- Moreno-Fernandez, A.; Iranzo-Cortés, J.E.; Paredes-Gallardo, V.; García-Sanz, V.; Tarazona-Álvarez, B.; Almerich-Silla, J.M.; Bellot-Arcís, C.; Montiel-Company, J.M. Effectiveness of removable appliances with temperature sensors in orthodontic patients: A systematic review and meta-analysis. Eur. J. Orthod. 2022, 44, 134–145. [Google Scholar] [CrossRef]
- Baccetti, T.; Franchi, L.; Toth, L.R.; McNamara, J.A. Treatment timing for Twin-block therapy. Am. J. Orthod. Dentofac. Orthop. 2000, 118, 159–170. [Google Scholar] [CrossRef] [PubMed]
- Ahlgren, J. A Longitudinal Clinical and Cephalometric Study of 50 Malocclusion Cases Treated with Activator Appliances. Transactions; European Orthodontic Society: London, UK, 1972; pp. 285–293. [Google Scholar]
- Ciavarella, D.; Lorusso, M.; Fanelli, C.; Cazzolla, A.P.; Maci, M.; Ferrara, D.; Muzio, L.L.; Tepedino, M. The Correlation between Mandibular Arch Shape and Vertical Skeletal Pattern. Medicina 2023, 59, 1926. [Google Scholar] [CrossRef]
- Ciavarella, D.; Lorusso, M.; Fanelli, C.; Ferrara, D.; Laurenziello, M.; Montaruli, G.; Esposito, R.; Tepedino, M. Evaluation of occlusal force in Class II subdivision malocclusion. J. Oral Rehabil. 2024, 51, 1813–1820. [Google Scholar] [CrossRef]
- Moro, A.; Borges, S.W.; Spada, P.P.; Morais, N.D.; Correr, G.M., Jr.; Cevidanes, L.H.S. Twenty-year clinical experience with fixed functional appliances. Dent. Press J. Orthod. 2018, 23, 87–109. [Google Scholar] [CrossRef]
- Sander, F.G.; Weinreich, A. [The bite-jumping-appliance]. Dtsch. Stomatol. 1991, 41, 195–198. [Google Scholar]
- Santamaria-Villegas, A.; Manrique-Hernandez, R.; Alvarez-Varela, E.; Restrepo-Serna, C. Effect of removable functional appliances on mandibular length in patients with class II with retrognathism: Systematic review and meta-analysis. BMC Oral Health 2017, 17, 52. [Google Scholar] [CrossRef] [PubMed]
- Ciavarella, D.; Lorusso, M.; Fanelli, C.; Ferrara, D.; Esposito, R.; Laurenziello, M.; Esperouz, F.; Russo, L.L.; Tepedino, M. The Efficacy of the RME II System Compared with a Herbst Appliance in the Treatment of Class II Skeletal Malocclusion in Growing Patients: A Retrospective Study. Dent. J. 2024, 12, 254. [Google Scholar] [CrossRef] [PubMed]
- Marinelli, A.; Mariotti, M.; Defraia, E. Transverse dimensions of dental arches in subjects with Class II malocclusion in the early mixed dentition. Prog. Orthod. 2011, 12, 31–37. [Google Scholar] [CrossRef]
- Sayin, M.O.; Turkkahraman, H. Comparison of dental arch and alveolar widths of patients with Class II, division 1 malocclusion and subjects with Class I ideal occlusion. Angle Orthod. 2004, 74, 356–360. [Google Scholar]
- Yu, Y.; Wu, M.; Chen, X.; Li, W. Correction of the transverse discrepancy-induced spontaneous mandibular protrusion in Class II Division 1 adolescent patients. Australas. Orthod. J. 2016, 32, 148–154. [Google Scholar] [CrossRef]
- Baratieri, C.; Alves, M., Jr.; Bolognese, A.M.; Nojima, M.C.G.; Nojima, L.I. Changes in skeletal and dental relationship in Class II Division I malocclusion after rapid maxillary expansion: A prospective study. Dent. Press J. Orthod. 2014, 19, 75–81. [Google Scholar] [CrossRef]
- McNamara, J.A., Jr.; Sigler, L.M.; Franchi, L.; Guest, S.S.; Baccetti, T. Changes in occlusal relationships in mixed dentition patients treated with rapid maxillary expansion. A prospective clinical study. Angle Orthod. 2010, 80, 230–238. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for reporting observational studies. Int. J. Surg. 2014, 12, 1495–1499. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis. Curr. Dir. Psychol. Sci. 1992, 1, 98–101. [Google Scholar] [CrossRef]
- Houston, W.J. The analysis of errors in orthodontic measurements. Am. J. Orthod. 1983, 83, 382–390. [Google Scholar] [CrossRef]
- Dahlberg, G. Statistical Methods for Medical and Biological Students; G. Allen & Unwin Limited.: Crows Nest, NSW, Australia, 1940. [Google Scholar]
- Wahl, N. Orthodontics in 3 millennia. Chapter 9: Functional appliances to midcentury. Am. J. Orthod. Dentofac. Orthop. 2006, 129, 829–833. [Google Scholar] [CrossRef] [PubMed]
- Martina, R.; Cioffi, I.; Galeotti, A.; Tagliaferri, R.; Cimino, R.; Michelotti, A.; Valletta, R.; Farella, M.; Paduano, S. Efficacy of the Sander bite-jumping appliance in growing patients with mandibular retrusion: A randomized controlled trial. Orthod. Craniofacial Res. 2013, 16, 116–126. [Google Scholar] [CrossRef] [PubMed]
- Sambale, J.; Jablonski-Momeni, A.; Korbmacher-Steiner, H.M. Impact of initial lip competence on the outcome of class II functional appliances therapy. Clin. Oral Investig. 2024, 28, 126. [Google Scholar] [CrossRef]
- Michele, T.; Elisabetta, C.L.; Nota, A.; Simona, T.; Cozza, P.; Pavoni, C. Dentoskeletal effects of the bitejumping appliance and the twin-block appliance in the treatment of skeletal class ii malocclusion: A retrospective controlled clinical trial. Oral Implantol. 2018, 11, 210–219. [Google Scholar]
- Sander, F.G.; Wichelhaus, A. [Skeletal and dental changes during the use of the bite-jumping plate. A cephalometric comparison with an untreated Class-II group]. Fortschr. Kieferorthop. 1995, 56, 127–139. [Google Scholar] [CrossRef]
- Gazzani, F.; Ruellas, A.C.d.O.; Faltin, K.; Franchi, L.; Cozza, P.; Bigliazzi, R.; Cevidanes, L.H.S.; Lione, R. 3D Comparison of Mandibular Response to Functional Appliances: Balters Bionator versus Sander Bite Jumping. Biomed. Res. Int. 2018, 2018, 2568235. [Google Scholar] [CrossRef]
- Faccioni, P.; De Santis, D.; Sinigaglia, S.; Zarantonello, M.; Zotti, F.; Pancera, P.; Iurlaro, A.; Finotti, M.; Marchiori, M.; Bazzanella, S.; et al. Effects of the sander bite jumping appliance in patients with class ii malocclusion before growth peak. J. Biol. Regul. Homeost. Agents 2020, 34 (Suppl. S2), 1–7. [Google Scholar]
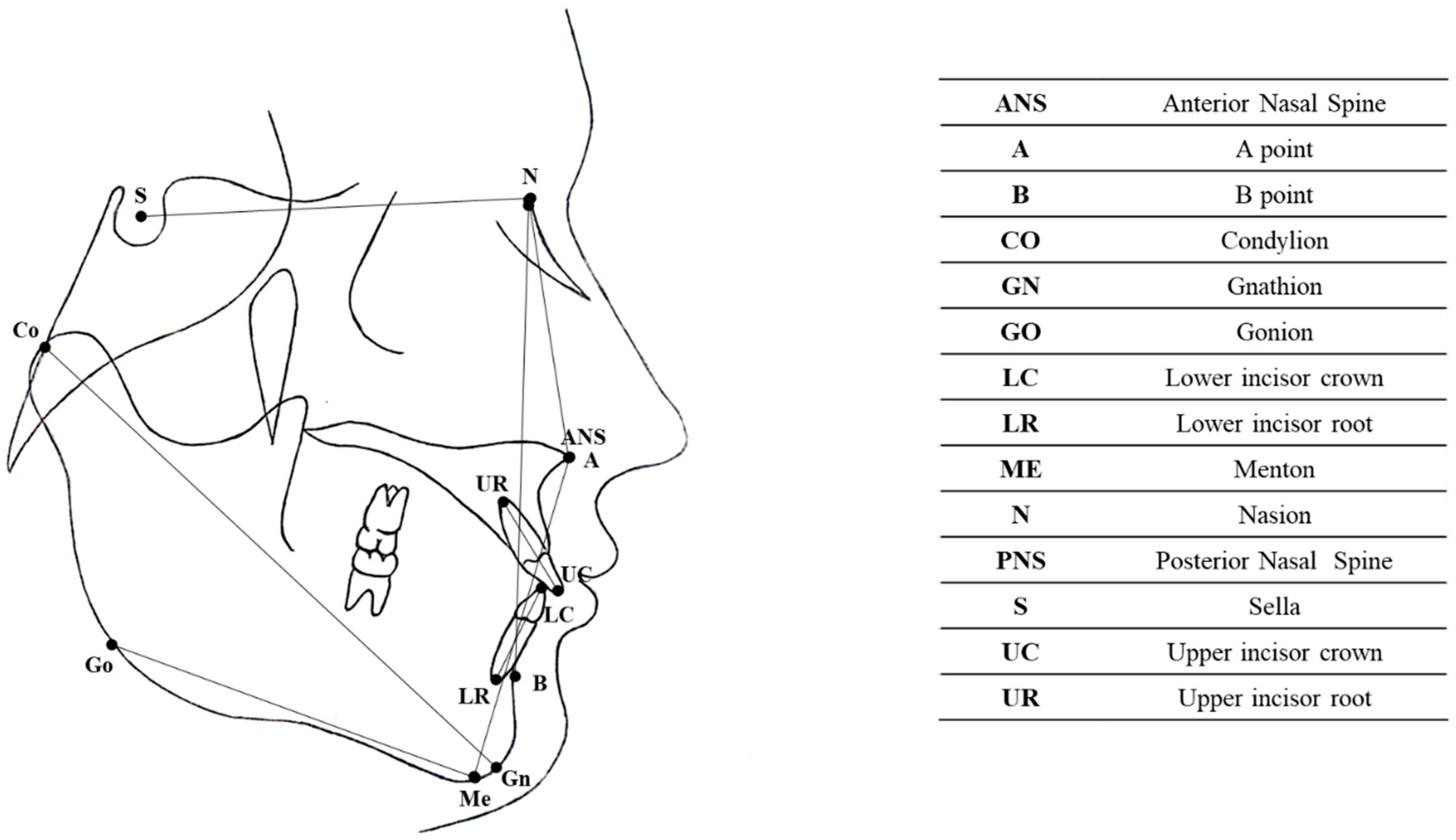
| Measurement | Description |
|---|---|
| Skeletal measurements | |
| SN-MP | Angle between the sella–nasion (SN) line and the mandibular plane (MP) |
| ANB | Angle between the N–A line and N–B line |
| LFH (lower face height) | Distance between the anterior nasal spine (ANS) and the menton (ME) |
| MANDIBULAR LENGTH (CO-GN) | Distance between the condylion and the gnathion |
| Dental measurements | |
| 1 + SN | Angle between the upper incisor and the sella–nasion line |
| IMPA | Angle between the lower incisor and the mandibular plane (GO–ME) |
| OVERJET | Horizontal distance between the incisal border of the upper and lower incisors |
| OVERBITE | Vertical distance between the incisal border of the upper and lower incisors |
| Sum of Squares | df | Mean Square | F | p | ||
|---|---|---|---|---|---|---|
| SN-MP | Between groups | 100,987 | 2 | 50,494 | 16,378 | 0.001 ** |
| Within groups | 268,216 | 88 | 3083 | |||
| Total | 369,204 | 90 | ||||
| Lower Face Height | Between groups | 451,207 | 2 | 225,603 | 19,052 | 0.001 ** |
| Within groups | 1,030,216 | 88 | 11,842 | |||
| Total | 1,481,423 | 90 | ||||
| CO-GN | Between groups | 589,342 | 2 | 294,671 | 15,295 | 0.001 ** |
| Within groups | 1,676,171 | 88 | 19,266 | |||
| Total | 2,265,513 | 90 | ||||
| 1 + SN | Between groups | 212,339 | 2 | 106,169 | 2299 | 0.106 |
| Within groups | 4,018,160 | 88 | 46,186 | |||
| Total | 4,230,499 | 90 | ||||
| IMPA | Between groups | 277,328 | 2 | 138,664 | 8244 | 0.001 ** |
| Within groups | 1,463,357 | 88 | 16,820 | |||
| Total | 1,740,685 | 90 | ||||
| Overbite | Between groups | 144,986 | 2 | 72,493 | 17,797 | 0.001 ** |
| Within groups | 354,379 | 88 | 4073 | |||
| Total | 499,365 | 90 | ||||
| Overjet | Between groups | 384,078 | 2 | 192,039 | 42,226 | 0.001 ** |
| Within groups | 395,669 | 88 | 4548 | |||
| Total | 779,746 | 90 | ||||
| ANB | Between groups | 71,239 | 2 | 35,619 | 13,691 | 0.001 ** |
| Within groups | 226,353 | 88 | 2602 | |||
| Total | 297,592 | 90 | ||||
| Dependent Variable | (I) Group | (J) Group | Mean Difference (I–J) | Std Error | p | 95% Confidence Interval | |
|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||||
| SN-MP | C | R | 1.81 * | 0.453 | 0.001 | 0.734 | 2.896 |
| C | S | −0.698 | 0.453 | 0.277 | −1.779 | 0.382 | |
| S | R | 2.51 * | 0.453 | 0.001 | 1.432 | 3.594 | |
| Lower Face Height | C | R | 5.46 * | 0.888 | 0.001 | 3.348 | 7.585 |
| C | S | 2.35 | 0.888 | 0.026 | 0.235 | 4.472 | |
| S | R | 3.11 * | 0.888 | 0.002 | 0.994 | 5.232 | |
| CO-GN | C | R | −4.83 * | 1.133 | 0.001 | 1.632 | 7.037 |
| C | S | −6.08 * | 1.133 | 0.001 | 3385 | 8.790 | |
| S | R | 1.75 | 1.133 | 0.274 | 4.455 | 0.94 | |
| 1 + SN | C | R | 3.25 | 1.754 | 0.159 | −0.934 | 7.434 |
| C | S | 3.26 | 1.754 | 0.156 | −0.917 | 7.450 | |
| S | R | −0.01 | 1.754 | 1.001 | −4.208 | 4.167 | |
| IMPA | C | R | 0.66 | 1.058 | 0.807 | −1.864 | 3.186 |
| C | S | −3.34 * | 1.058 | 0.006 | −5.874 | −0.824 | |
| S | R | 4.01 * | 1.058 | 0.001 | 1.485 | 6.535 | |
| Overbite | C | R | 1.11 | 0.521 | 0.09 | −0.132 | 2.352 |
| C | S | 3.07 * | 0.521 | 0.001 | 1.8274 | 4.312 | |
| S | R | −1.96 * | 0.521 | 0.001 | −3.202 | −0.717 | |
| Overjet | C | R | 3.59 * | 0.550 | 0.001 | 2.277 | 4.903 |
| C | S | 4.88 * | 0.550 | 0.001 | 3.570 | 6.196 | |
| S | R | −1.29 | 0.550 | 0.054 | −2.606 | 0.019 | |
| ANB | C | R | 2.15 * | 0.416 | 0.001 | 1.156 | 3.143 |
| C | S | 0.76 | 0.416 | 0.162 | −0.226 | 1.759 | |
| S | R | 1.38 * | 0.416 | 0.004 | 0.390 | 2.376 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lorusso, M.; Tepedino, M.; Ferrara, D.; Cazzolla, A.P.; Esperouz, F.; Esposito, R.; Lo Russo, L.; Ciavarella, D. The Efficacy of the RME II System Compared with the Sander Bite-Jumping Appliance: A Retrospective Study. J. Clin. Med. 2025, 14, 3700. https://doi.org/10.3390/jcm14113700
Lorusso M, Tepedino M, Ferrara D, Cazzolla AP, Esperouz F, Esposito R, Lo Russo L, Ciavarella D. The Efficacy of the RME II System Compared with the Sander Bite-Jumping Appliance: A Retrospective Study. Journal of Clinical Medicine. 2025; 14(11):3700. https://doi.org/10.3390/jcm14113700
Chicago/Turabian StyleLorusso, Mauro, Michele Tepedino, Donatella Ferrara, Angela Pia Cazzolla, Fariba Esperouz, Rosa Esposito, Lucio Lo Russo, and Domenico Ciavarella. 2025. "The Efficacy of the RME II System Compared with the Sander Bite-Jumping Appliance: A Retrospective Study" Journal of Clinical Medicine 14, no. 11: 3700. https://doi.org/10.3390/jcm14113700
APA StyleLorusso, M., Tepedino, M., Ferrara, D., Cazzolla, A. P., Esperouz, F., Esposito, R., Lo Russo, L., & Ciavarella, D. (2025). The Efficacy of the RME II System Compared with the Sander Bite-Jumping Appliance: A Retrospective Study. Journal of Clinical Medicine, 14(11), 3700. https://doi.org/10.3390/jcm14113700









