Intrahospital Prevalence of Diabetes and Prediabetes in Medical Departments in Upper Austria
Abstract
1. Introduction
2. Methods
2.1. Study Sites
2.2. Study Participants
2.3. Ethical Approval
2.4. Statistics
3. Results
3.1. General Patient Characteristics
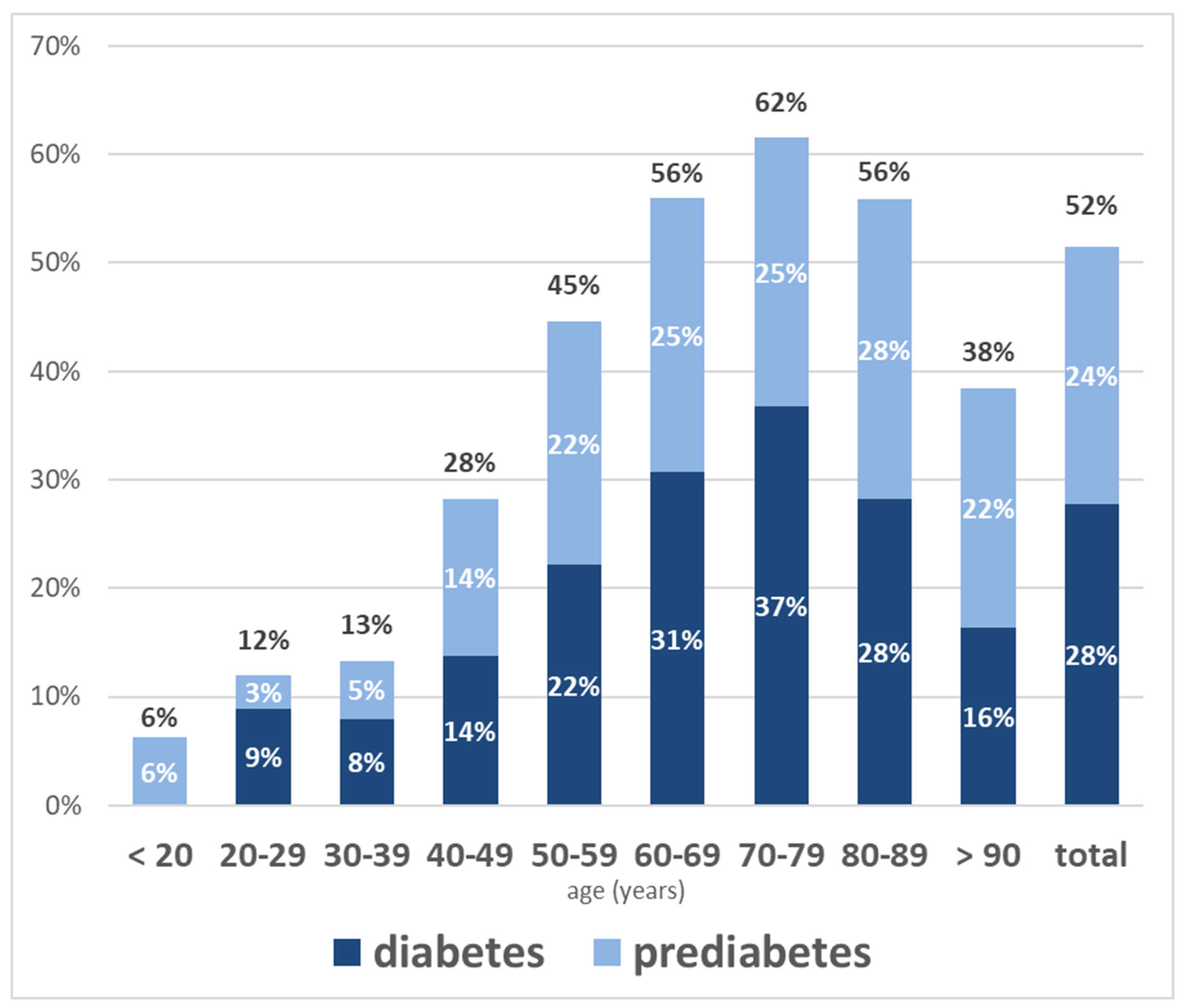
3.2. Diabetes and Prediabetes Prevalence
3.3. Relationships Between Glycemic Status and Cardiovascular Illness
3.4. Relationships Between Glycaemic Status, Medications, BMI, and Mortality
4. Discussion
4.1. Prevalence of Diabetes and Prediabetes Prevalence in Hospitalised Patients
4.2. Comorbidities, Antidiabetic Therapy, and Mortality
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CRP | C-reactive protein |
| eGFR | Estimated glomerular filtration rate |
| HbA1c | Glycated haemoglobin A1 |
| HDL | High-density lipoprotein |
| ICH-GCP | International Conference on Harmonization Good Clinical Practice |
| IFG | Impaired fasting glucose |
| IGT | Impaired glucose tolerance |
| IQR | Interquartile range |
| LDL | Low-density lipoprotein |
| OR | Odds ratio |
| SD | Standard deviation |
References
- Rawshani, A.; Rawshani, A.; Gudbjornsdottir, S. Mortality and Cardiovascular Disease in Type 1 and Type 2 Diabetes. N. Engl. J. Med. 2017, 377, 300–301. [Google Scholar] [CrossRef] [PubMed]
- Booth, G.L.; Kapral, M.K.; Fung, K.; Tu, J.V. Relation between age and cardiovascular disease in men and women with diabetes compared with non-diabetic people: A population-based retrospective cohort study. Lancet 2006, 368, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Rao Kondapally Seshasai, S.; Kaptoge, S.; Thompson, A.; Di Angelantonio, E.; Gao, P.; Sarwar, N.; Whincup, P.H.; Mukamal, K.J.; Gillum, R.F.; Holme, I.; et al. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N. Engl. J. Med. 2011, 364, 829–841. [Google Scholar]
- Echouffo-Tcheugui, J.B.; Perreault, L.; Ji, L.; Dagogo-Jack, S. Diagnosis and Management of Prediabetes: A Review. JAMA 2023, 329, 1206–1216. [Google Scholar] [CrossRef]
- Rawshani, A.; Rawshani, A.; Franzén, S.; Sattar, N.; Eliasson, B.; Svensson, A.M.; Zethelius, B.; Miftaraj, M.; McGuire, D.K.; Rosengren, A.; et al. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N. Engl. J. Med. 2018, 379, 633–644. [Google Scholar] [CrossRef]
- Magliano, D.J.; Boyko, E.J. International Diabetes Federation Committee. In IDF Diabetes Atlas; International Diabetes Federation: Brussels, Belgium, 2021. [Google Scholar]
- National Center for Health Statistics (Ed.) Prevalence of Total, Diagnosed, and Undiagnosed Diabetes in Adults: United States, August 2021–August 2023; National Center for Health Statistics: Hyattsville, MD, USA, 2024. [CrossRef]
- Clodi, M.; Abrahamian, H.; Brath, H.; Schernthaner, G.; Brix, J.; Ludvik, B.; Drexel, H.; Saely, C.H.; Fasching, P.; Rega-Kaun, G.; et al. Antihyperglycemic treatment guidelines for diabetes mellitus type 2; Update 2023. Wien. Klin. Wochenschr. 2023, 135, 32–44. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 2. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes—2024. Diabetes Care 2024, 47 (Suppl. S1), S20–S42. [Google Scholar] [CrossRef]
- Rooney, M.R.; Fang, M.; Ogurtsova, K.; Ozkan, B.; Echouffo-Tcheugui, J.B.; Boyko, E.J.; Magliano, D.J.; Selvin, E. Global prevalence of prediabetes. Diabetes Care 2023, 46, 1388–1394. [Google Scholar] [CrossRef]
- Breyer, M.K.; Ofenheimer, A.; Altziebler, J.; Hartl, S.; Burghuber, O.C.; Studnicka, M.; Purin, D.; Heinzle, C.; Drexel, H.; Franssen, F.M.E.; et al. Marked differences in prediabetes- and diabetes-associated comorbidities between men and women-Epidemiological results from a general population-based cohort aged 6–80 years—The LEAD (Lung, hEart, sociAl, boDy) study. Eur. J. Clin. Investig. 2020, 50, e13207. [Google Scholar] [CrossRef]
- Fröschl, B.; Bär, B.; Habimana, K.; Habl, C.; Nagel, A.; Stradner, A. Interdisziplinäre und Multiprofessionelle Versorgung bei Diabetes Mellitus Typ 2; Gesundheit Österreich Forschungs- und Planungs GmbH: Wien, Austria, 2023; Available online: https://emedien.arbeiterkammer.at/resolver?urn=urn:nbn:at:at-akw:g-6627770 (accessed on 12 September 2024).
- Frey, V.; Langthaler, P.; Raphaelis, E.; Ring-Dimitriou, S.; Kedenko, L.; Aigner, E.; Martinz, J.; Gostner, I.; Bathke, A.C.; Sungler, P.; et al. Paracelsus 10,000: An Observational Cohort Study About the Health Status of the Population of Salzburg, Austria. Rationale, Objectives and Study Design. Paracelsus Proc. Exp. Med. 2023, 2, 1–17. [Google Scholar]
- Kaleta, M.; Leutner, M.; Thurner, S.; Endel, G.; Kiss, N.; Robausch, M.; Klimek, P.; Kautzky-Willer, A. Trends in diabetes incidence in Austria 2013–2017. Sci. Rep. 2023, 13, 8715. [Google Scholar] [CrossRef] [PubMed]
- Kar, P.; Jones, K.L.; Horowitz, M.; Deane, A.M. Management of critically ill patients with type 2 diabetes: The need for personalised therapy. World J. Diabetes 2015, 6, 693–706. [Google Scholar] [CrossRef]
- Plummer, M.P.; Bellomo, R.; Cousins, C.E.; Annink, C.E.; Sundararajan, K.; Reddi, B.A.; Raj, J.P.; Chapman, M.J.; Horowitz, M.; Deane, A.M. Dysglycaemia in the critically ill and the interaction of chronic and acute glycaemia with mortality. Intensive Care Med. 2014, 40, 973–980. [Google Scholar] [CrossRef]
- Karakonstantis, S.; Kassotaki, I.; Korela, D.; Arna, D.; Milaki, K.; Tsigaridaki, M.; Lydakis, C.; Pappas, A. In-hospital screening for diabetes mellitus with HbA1c in an internal medicine department was not useful; a prospective pilot study. Rom. J. Intern. Med. 2019, 57, 315–321. [Google Scholar] [CrossRef]
- Valentine, N.A.; Alhawassi, T.M.; Roberts, G.W.; Vora, P.P.; Stranks, S.N.; Doogue, M.P. Detecting undiagnosed diabetes using glycated haemoglobin: An automated screening test in hospitalised patients. Med. J. Aust. 2011, 194, 160–164. [Google Scholar] [CrossRef]
- Wexler, D.J.; Nathan, D.M.; Grant, R.W.; Regan, S.; Van Leuvan, A.L.; Cagliero, E. Prevalence of elevated hemoglobin A1c among patients admitted to the hospital without a diagnosis of diabetes. J. Clin. Endocrinol. Metab. 2008, 93, 4238–4244. [Google Scholar] [CrossRef]
- Kufeldt, J.; Kovarova, M.; Adolph, M.; Staiger, H.; Bamberg, M.; Haering, H.-U.; Fritsche, A.; Peter, A. Prevalence and distribution of diabetes mellitus in a maximum care hospital: Urgent need for HbA1c-screening. Exp. Clin. Endocrinol. Diabetes 2018, 126, 123–129. [Google Scholar] [CrossRef]
- Mazurek, J.A.; Hailpern, S.M.; Goring, T.; Nordin, C. Prevalence of hemoglobin A1c greater than 6.5% and 7.0% among hospitalized patients without known diagnosis of diabetes at an urban inner city hospital. J. Clin. Endocrinol. Metab. 2010, 95, 1344–1348. [Google Scholar] [CrossRef][Green Version]
- Muller-Wieland, D.; Merkel, M.; Hamann, A.; Siegel, E.; Ottillinger, B.; Woker, R.; Fresenius, K. Survey to estimate the prevalence of type 2 diabetes mellitus in hospital patients in Germany by systematic HbA1c measurement upon admission. Int. J. Clin. Pract. 2018, 72, e13273. [Google Scholar] [CrossRef]
- American Diabetes Association Professional Practice Committee. 2. Diagnosis and Classification of Diabetes: Standards of Care in Diabetes—2025. Diabetes Care 2025, 48 (Suppl. S1), S27–S49. [Google Scholar] [CrossRef]
- Harreiter, J.; Roden, M. Diabetes mellitus: Definition, classification, diagnosis, screening and prevention; Update 2023. Wien. Klin. Wochenschr. 2023, 135 (Suppl. S1), 7–17. [Google Scholar] [CrossRef] [PubMed]
- Rooney, M.R.; Rawlings, A.M.; Pankow, J.S.; Tcheugui, J.B.E.; Coresh, J.; Sharrett, A.R.; Selvin, E. Risk of progression to diabetes among older adults with prediabetes. JAMA Intern. Med. 2021, 181, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Richter, B.; Hemmingsen, B.; Metzendorf, M.I.; Takwoingi, Y. Development of type 2 diabetes mellitus in people with intermediate hyperglycaemia. Cochrane Database Syst. Rev. 2018, 2018, CD012661. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association. 3. Prevention or Delay of Type 2 Diabetes: Standards of Medical Care in Diabetes—2020. Diabetes Care 2020, 43, S32–S36. [Google Scholar] [CrossRef]
- Schlesinger, S.; Neuenschwander, M.; Barbaresko, J.; Lang, A.; Maalmi, H.; Rathmann, W.; Roden, M.; Herder, C. Prediabetes and risk of mortality, diabetes-related complications and comorbidities: Umbrella review of meta-analyses of prospective studies. Diabetologia 2022, 65, 275–285. [Google Scholar] [CrossRef]
- Cai, X.; Zhang, Y.; Li, M.; Wu, J.H.; Mai, L.; Li, J.; Yang, Y.; Hu, Y.; Huang, Y. Association between prediabetes and risk of all cause mortality and cardiovascular disease: Updated meta-analysis. BMJ 2020, 370, m2297. [Google Scholar] [CrossRef]
- Capece, U.; Iacomini, C.; Mezza, T.; Cesario, A.; Masciocchi, C.; Patarnello, S.; Giaccari, A.; Di Giorgi, N. Real-world evidence evaluation of LDL-C in hospitalized patients: A population-based observational study in the timeframe 2021–2022. Lipids Health Dis. 2024, 23, 224. [Google Scholar] [CrossRef]
- Cavagnolli, G.; Comerlato, J.; Comerlato, C.; Renz, P.B.; Gross, J.L.; Camargo, J.L. HbA(1c) measurement for the diagnosis of diabetes: Is it enough? Diabet. Med. 2011, 28, 31–35. [Google Scholar] [CrossRef]
- Schneider, A.L.; Kalyani, R.R.; Golden, S.; Stearns, S.C.; Wruck, L.; Yeh, H.C.; Coresh, J.; Selvin, E. Diabetes and Prediabetes and Risk of Hospitalization: The Atherosclerosis Risk in Communities (ARIC) Study. Diabetes Care 2016, 39, 772–779. [Google Scholar] [CrossRef]
- Khalid, J.M.; Raluy-Callado, M.; Curtis, B.H.; Boye, K.S.; Maguire, A.; Reaney, M. Rates and risk of hospitalisation among patients with type 2 diabetes: Retrospective cohort study using the UK General Practice Research Database linked to English Hospital Episode Statistics. Int. J. Clin. Pract. 2014, 68, 40–48. [Google Scholar] [CrossRef]
- La Sala, L.; Prattichizzo, F.; Ceriello, A. The link between diabetes and atherosclerosis. Eur. J. Prev. Cardiol. 2019, 26 (Suppl. S2), 15–24. [Google Scholar] [CrossRef]
- Ohkuma, T.; Harris, K.; Woodward, M.; Hamet, P.; Harrap, S.; Mancia, G.; Marre, M.; Poulter, N.; Chalmers, J.; Zoungas, S.; et al. Intensive Glucose Lowering and Its Effects on Vascular Events and Death According to Age at Diagnosis and Duration of Diabetes: The ADVANCE Trial. Diabetes Care 2025, 48, 279–284. [Google Scholar] [CrossRef] [PubMed]
- Pop-Busui, R.; Januzzi, J.L.; Bruemmer, D.; Butalia, S.; Green, J.B.; Horton, W.B.; Knight, C.; Levi, M.; Rasouli, N.; Richardson, C.R. Heart Failure: An Underappreciated Complication of Diabetes. A Consensus Report of the American Diabetes Association. Diabetes Care 2022, 45, 1670–1690. [Google Scholar] [CrossRef] [PubMed]
- Thrainsdottir, I.S.; Aspelund, T.; Thorgeirsson, G.; Gudnason, V.; Hardarson, T.; Malmberg, K.; Sigurdsson, G.; Ryden, L. The association between glucose abnormalities and heart failure in the population-based Reykjavik study. Diabetes Care 2005, 28, 612–616. [Google Scholar] [CrossRef]
- Packer, M.; Anker, S.D.; Butler, J.; Filippatos, G.; Pocock, S.J.; Carson, P.; Januzzi, J.; Verma, S.; Tsutsui, H.; Brueckmann, M.; et al. Cardiovascular and Renal Outcomes with Empagliflozin in Heart Failure. N. Engl. J. Med. 2020, 383, 1413–1424. [Google Scholar] [CrossRef]
- Solomon, S.D.; McMurray, J.J.V.; Anand, I.S.; Ge, J.; Lam, C.S.P.; Maggioni, A.P.; Martinez, F.; Packer, M.; Pfeffer, M.A.; Pieske, B.; et al. Angiotensin-Neprilysin Inhibition in Heart Failure with Preserved Ejection Fraction. N. Engl. J. Med. 2019, 381, 1609–1620. [Google Scholar] [CrossRef]
- Solomon, S.D.; McMurray, J.J.V.; Claggett, B.; de Boer, R.A.; DeMets, D.; Hernandez, A.F.; Inzucchi, S.E.; Kosiborod, M.N.; Lam, C.S.P.; Martinez, F.; et al. Dapagliflozin in Heart Failure with Mildly Reduced or Preserved Ejection Fraction. N. Engl. J. Med. 2022, 387, 1089–1098. [Google Scholar] [CrossRef]
- Anker, S.D.; Butler, J.; Filippatos, G.; Ferreira, J.P.; Bocchi, E.; Bohm, M.; Brunner-La Rocca, H.P.; Choi, D.J.; Chopra, V.; Chuquiure-Valenzuela, E.; et al. Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N. Engl. J. Med. 2021, 385, 1451–1461. [Google Scholar] [CrossRef]
- Lehrke, M.; Marx, N. Diabetes mellitus and heart failure. Am. J. Cardiol. 2017, 120, S37–S47. [Google Scholar] [CrossRef]
- Jia, G.; Hill, M.A.; Sowers, J.R. Diabetic Cardiomyopathy: An Update of Mechanisms Contributing to This Clinical Entity. Circ. Res. 2018, 122, 624–638. [Google Scholar] [CrossRef]
- Bugger, H.; Abel, E.D. Molecular mechanisms of diabetic cardiomyopathy. Diabetologia 2014, 57, 660–671. [Google Scholar] [CrossRef] [PubMed]
- Mahase, E. GLP-1 shortages will not resolve this year, EMA warns, amid concern over off-label use. BMJ 2024, 385, 1448. [Google Scholar] [CrossRef] [PubMed]
- Enomoto, L.M.; Shrestha, D.P.; Rosenthal, M.B.; Hollenbeak, C.S.; Gabbay, R.A. Risk factors associated with 30-day readmission and length of stay in patients with type 2 diabetes. J. Diabetes Complicat. 2017, 31, 122–127. [Google Scholar] [CrossRef]
- de Miguel-Yanes, J.M.; Jiménez-García, R.; Hernández-Barrera, V.; Méndez-Bailón, M.; de Miguel-Díez, J.; Lopez-de-Andrés, A. Impact of type 2 diabetes mellitus on in-hospital-mortality after major cardiovascular events in Spain (2002–2014). Cardiovasc. Diabetol. 2017, 16, 126. [Google Scholar] [CrossRef]
- Palaiodimos, L.; Chamorro-Pareja, N.; Karamanis, D.; Li, W.; Zavras, P.D.; Chang, K.M.; Mathias, P.; Kokkinidis, D.G. Diabetes is associated with increased risk for in-hospital mortality in patients with COVID-19: A systematic review and meta-analysis comprising 18,506 patients. Hormones 2021, 20, 305–314. [Google Scholar] [CrossRef]

| Diabetes n = 840 | Prediabetes n = 717 | Normal Glucose Status n = 1468 | Total n = 3025 | |
|---|---|---|---|---|
| Mean ± SD or Median (IQR) | Mean ± SD or Median (IQR) | Mean ± SD or Median (IQR) | Mean ± SD or Median (IQR) | |
| Duration of stay (days) a,b | 5 (3–8) | 4 (3–7) | 4 (2–7) | 4 (3–7) |
| Age (years) a,c | 72.9 ± 11.9 | 73.8 ± 12.6 | 68.3 ± 18.4 | 70.9 ± 15.7 |
| Height (cm) | 171.9 ± 8.6 | 171.7 ± 8.8 | 171.6 ± 9.3 | 171.7 ± 9.0 |
| BMI (kg/m2) a,b,c | 28.4 ± 6.4 | 26.7 ± 5.2 | 25.6 ± 4.9 | 26.6 ± 5.5 |
| HbA1c (%) a,b,c | 7.1 ± 1.7 | 5.9 ± 0.3 | 5.2 ± 0.3 | 5.9 ± 1.2 |
| LDL (mg/dL) a,b,c | 80.4 ± 39.4 | 87.8 ± 41.5 | 98.2 ± 42.3 | 90.8 ± 42.0 |
| HDL (mg/dL) a,b,c | 43.6 ± 17.3 | 48.0 ± 16.7 | 51.0 ± 19.9 | 48.3 ± 18.6 |
| Total cholesterol (mg/dL) a,c | 150.3 ± 48.3 | 154.3 ± 47.8 | 168.0 ± 47.9 | 160.3 ± 48.6 |
| Triglycerides (mg/dL) a,b | 120.0 (92–164) | 104.5 (79–145) | 100.0 (76–134) | 105.0 (79–142) |
| eGFR (mL/min/1.73 m²) a,c | 62.2 ± 24.7 | 64.1 ± 22.5 | 72.1 ± 23.5 | 67.5 ± 24.0 |
| Creatinine (mg/dL) a,c | 1.34 ± 0.80 | 1.27 ± 0.97 | 1.14 ± 0.79 | 1.23 ± 0.84 |
| Haemoglobin (g/dL) a,b | 12.8 ± 2.4 | 13.2 ± 2.2 | 13.1 ± 2.3 | 13.1 ± 2.3 |
| CRP (mg/dL) | 1.0 (0.2–4.0) | 0.6 (0.2–3.4) | 0.5 (0.1–3.3) | 0.6 (0.1–3.6) |
| Diabetes n = 840 | Prediabetes n = 717 | Normal Glucose Status n = 1468 | Total n = 3025 | |||||
|---|---|---|---|---|---|---|---|---|
| Female | 221 | 26.3% | 235 | 32.8% | 530 | 36.1% | 986 | 32.6% |
| Male | 619 | 73.7% | 482 | 67.2% | 938 | 63.9% | 2039 | 67.4% |
| Coronary artery disease | 393 | 46.8% | 332 | 46.3% | 469 | 31.9% | 1194 | 39.5% |
| Acute coronary event | 36 | 4.3% | 43 | 6.0% | 65 | 4.4% | 144 | 4.8% |
| Heart failure | 291 | 34.6% | 222 | 31.0% | 320 | 21.8% | 833 | 27.5% |
| Atrial fibrillation | 273 | 32.5% | 252 | 35.1% | 431 | 29.4% | 956 | 31.6% |
| Arterial hypertension | 554 | 66.0% | 432 | 60.3% | 713 | 48.6% | 1699 | 56.2% |
| Cardiac disease * | 563 | 67.0% | 517 | 72.1% | 793 | 54.0% | 1873 | 61.9% |
| Atherosclerosis § | 494 | 58.8% | 380 | 53.0% | 543 | 37.0% | 1417 | 46.8% |
| Intrahospital mortality | 39 | 4.6% | 32 | 4.5% | 59 | 4.0% | 130 | 4.3% |
| Diabetes n = 840 | Prediabetes n = 717 | Normal Glucose Status n = 1468 | Total n = 3025 | |||||
|---|---|---|---|---|---|---|---|---|
| Metformin (preexisting) | 378 | 45.0% | 3 | 0.4% | 0 | 0.0% | 381 | 12.6% |
| Metformin initiated | 47 | 5.6% | 1 | 0.1% | 0 | 0.0% | 48 | 1.6% |
| SGLT2-I (preexisting) | 302 | 36.0% | 103 | 14.4% | 103 | 7.0% | 508 | 16.8% |
| SGLT2-I initiated | 75 | 8.9% | 35 | 4.9% | 60 | 4.1% | 170 | 5.6% |
| GLP-1-RA (preexisting) | 55 | 6.5% | 0 | 0.0% | 1 | 0.1% | 56 | 1.9% |
| GLP-1-RA initiated | 4 | 0.5% | 0 | 0.0% | 1 | 0.1% | 5 | 0.2% |
| DPP-IV-I (preexisting) | 201 | 23.9% | 0 | 0.0% | 0 | 0.0% | 201 | 6.6% |
| DPP-IV-I initiated | 39 | 4.6% | 1 | 0.1% | 0 | 0.0% | 40 | 1.3% |
| Antidiabetic medication | 718 | 85.5% | 144 | 20.1% | 165 | 11.2% | 1027 | 34.0% |
| Pioglitazone (preexisting) | 11 | 1.3% | 0 | 0.0% | 0 | 0.0% | 11 | 0.4% |
| Pioglitazone initiated | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% |
| Insulin (preexisting) | 198 | 23.6% | 0 | 0.0% | 0 | 0.0% | 198 | 6.5% |
| Insulin initiated | 80 | 9.5% | 3 | 0.4% | 1 | 0.1% | 84 | 2.8% |
| Statins (preexisting) | 440 | 52.4% | 338 | 47.1% | 418 | 28.5% | 1196 | 39.5% |
| Statins initiated | 62 | 7.4% | 65 | 9.1% | 88 | 6.0% | 215 | 7.1% |
| Ezetimibe (preexisting) | 137 | 16.3% | 131 | 18.3% | 143 | 9.7% | 411 | 13.6% |
| Ezetimibe initiated | 54 | 6.4% | 56 | 7.8% | 75 | 5.1% | 185 | 6.1% |
| PCSK9-I (preexisting) | 2 | 0.2% | 4 | 0.6% | 9 | 0.6% | 15 | 0.5% |
| PCSK9-I initiated | 1 | 0.1% | 0 | 0.0% | 0 | 0.0% | 1 | 0.0% |
| Bemp. Acid (preexisting) | 5 | 0.6% | 6 | 0.8% | 9 | 0.6% | 20 | 0.7% |
| Bemp. Acid initiated | 2 | 0.2% | 1 | 0.1% | 6 | 0.4% | 9 | 0.3% |
| Any lipid-lowering med. | 510 | 60.7% | 414 | 57.7% | 515 | 35.1% | 1439 | 47.6% |
| Aspirin | 372 | 44.3% | 306 | 42.7% | 495 | 33.7% | 1173 | 38.8% |
| β-blockade | 421 | 50.1% | 383 | 53.4% | 598 | 40.7% | 1402 | 46.3% |
| RAAS-I | 572 | 68.1% | 467 | 65.1% | 698 | 47.5% | 1737 | 57.4% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heinzl, M.W.; Resl, M.; Kellermair, J.; Steinwender, C.; Mayr, B.; Obereder, J.; Fellner-Färber, R.; Klammer, C.; Hartl, S.; Brandner, J.; et al. Intrahospital Prevalence of Diabetes and Prediabetes in Medical Departments in Upper Austria. J. Clin. Med. 2025, 14, 3668. https://doi.org/10.3390/jcm14113668
Heinzl MW, Resl M, Kellermair J, Steinwender C, Mayr B, Obereder J, Fellner-Färber R, Klammer C, Hartl S, Brandner J, et al. Intrahospital Prevalence of Diabetes and Prediabetes in Medical Departments in Upper Austria. Journal of Clinical Medicine. 2025; 14(11):3668. https://doi.org/10.3390/jcm14113668
Chicago/Turabian StyleHeinzl, Matthias W., Michael Resl, Jörg Kellermair, Clemens Steinwender, Bernhard Mayr, Jana Obereder, Renate Fellner-Färber, Carmen Klammer, Stefanie Hartl, Julia Brandner, and et al. 2025. "Intrahospital Prevalence of Diabetes and Prediabetes in Medical Departments in Upper Austria" Journal of Clinical Medicine 14, no. 11: 3668. https://doi.org/10.3390/jcm14113668
APA StyleHeinzl, M. W., Resl, M., Kellermair, J., Steinwender, C., Mayr, B., Obereder, J., Fellner-Färber, R., Klammer, C., Hartl, S., Brandner, J., Zierer, A., Bernhard, D., Rega-Kaun, G., Mader, J. K., Riedl, M., Stingl, H., Stechemesser, L., Ress, C., Fröhlich-Reiterer, E., ... Clodi, M. (2025). Intrahospital Prevalence of Diabetes and Prediabetes in Medical Departments in Upper Austria. Journal of Clinical Medicine, 14(11), 3668. https://doi.org/10.3390/jcm14113668









