Short-Term Efficacy of a Multi-Modal Intervention Program to Improve Custom-Made Footwear Use in People at High Risk of Diabetes-Related Foot Ulceration
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
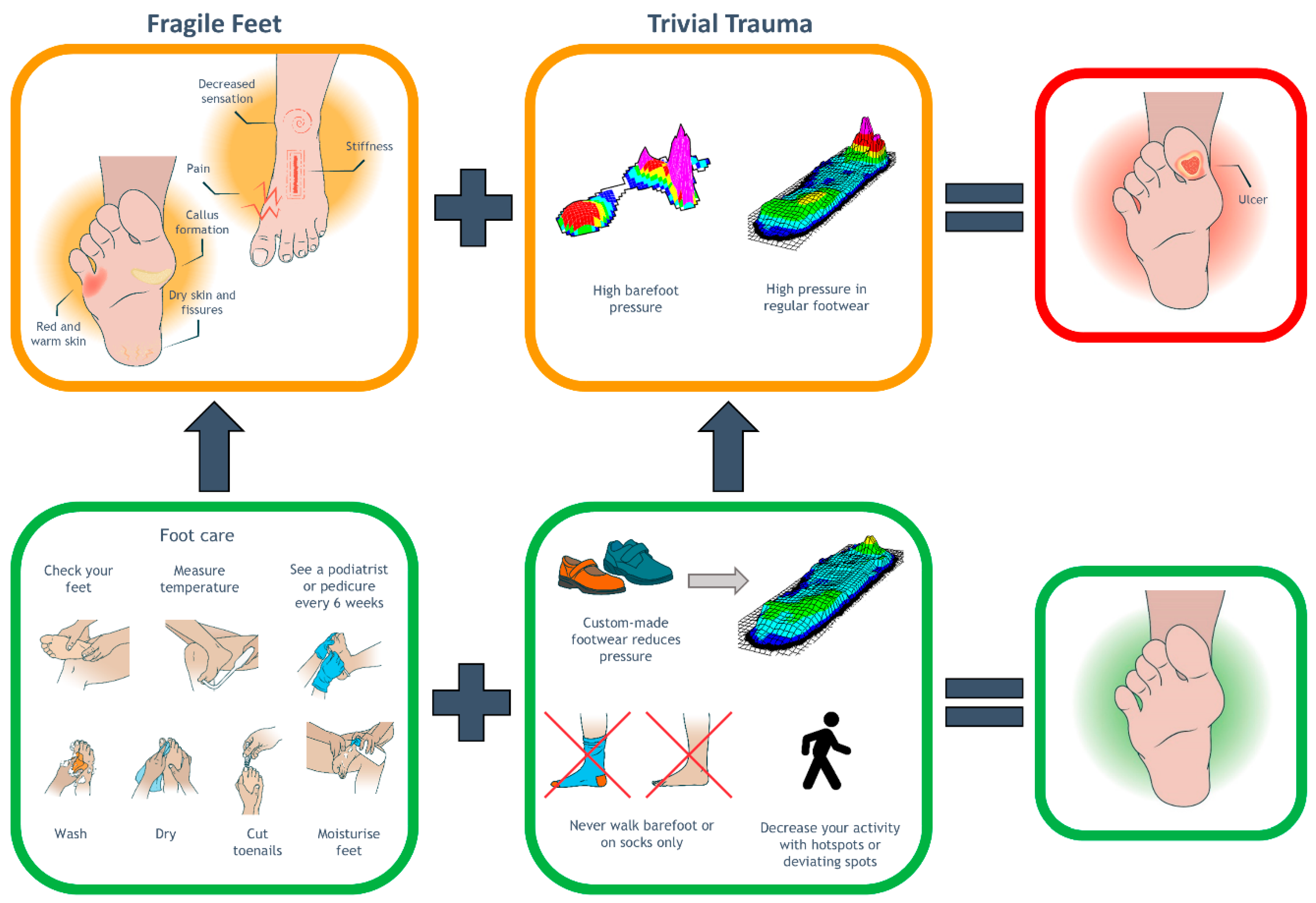
Development of the Intervention
2.2. Participants and Setting
2.3. Procedures
2.3.1. Modality 1: Structured and Personalised Education
2.3.2. Modality 2: Motivational Interviewing (MI)
2.3.3. Modality 3: Custom-Made Indoor Footwear
2.4. Outcomes
2.5. Statistical Analyses
3. Results
3.1. Baseline Characteristics
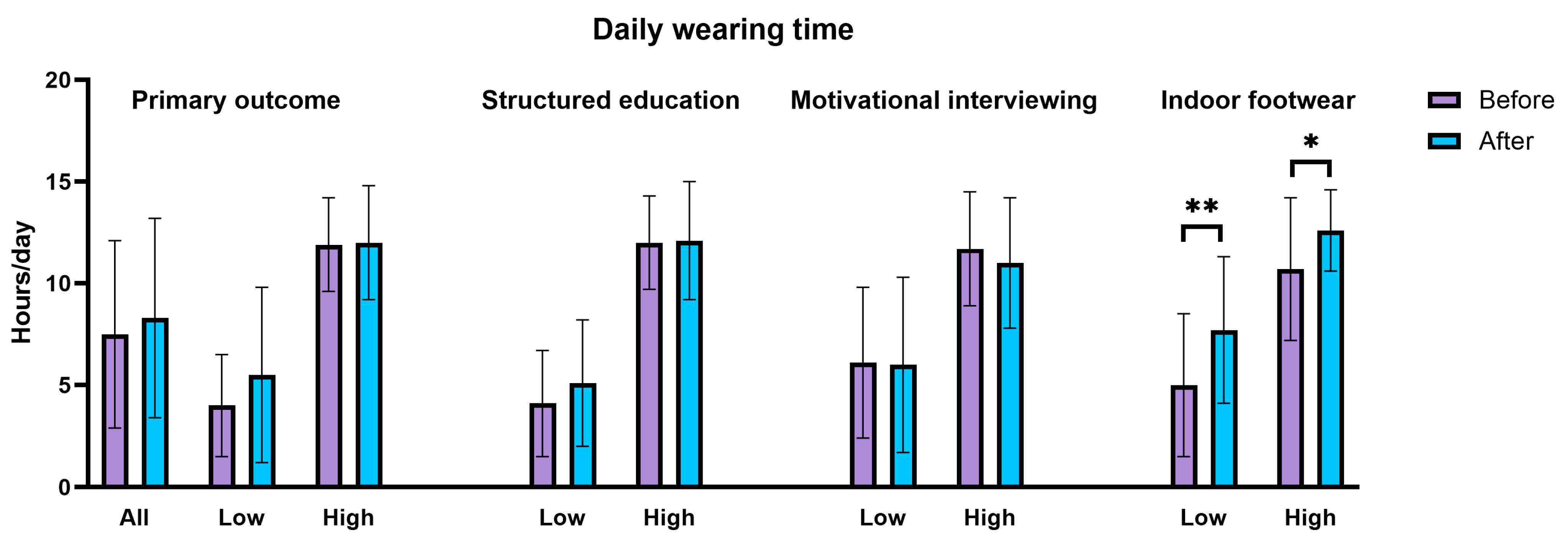
3.2. Primary and Secondary Outcomes
3.3. Assessment of MI-Fidelity
3.4. Factors Associated with Increased Wearing Time
3.5. Assessment of the Behavioural Components of the Intervention
4. Discussion
4.1. Modality 1: Structured and Personalised Education
4.2. Modality 2: Motivational Interviewing (MI)
4.3. Modality 3: Custom-Made Indoor Footwear
4.4. Strengths and Limitations
4.5. Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| RCT | Randomized Controlled Trial |
| MI | Motivational Interviewing |
| FF–TT | Fragile Feet–Trivial Trauma |
| MITI | Motivational Interviewing Treatment Integrity |
| COM-B | Capability, Opportunities, Motivation-Behaviour |
References
- Armstrong, D.G.; Tan, T.W.; Boulton, A.J.M.; Bus, S.A. Diabetic Foot Ulcers: A Review. JAMA 2023, 330, 62–75. [Google Scholar] [CrossRef] [PubMed]
- Bus, S.A.; Sacco, I.C.N.; Monteiro-Soares, M.; Raspovic, A.; Paton, J.; Rasmussen, A.; Lavery, L.A.; van Netten, J.J. Guidelines on the prevention of foot ulcers in persons with diabetes (IWGDF 2023 update). Diabetes Metab. Res. Rev. 2024, 40, e3651. [Google Scholar] [CrossRef] [PubMed]
- Bus, S.A.; Zwaferink, J.B.; Dahmen, R.; Busch-Westbroek, T.E. New design protocol and algorithm for custom-made footwear for people with diabetes. Diabetes Metab. Res. Rev. 2020, in press. [Google Scholar] [CrossRef]
- Jarl, G.; Lundqvist, L.O. Adherence to wearing therapeutic shoes among people with diabetes: A systematic review and reflections. Patient Prefer. Adherence 2016, 10, 1521–1528. [Google Scholar] [CrossRef] [PubMed]
- Jarl, G.; Hulshof, C.M.; Busch-Westbroek, T.E.; Bus, S.A.; van Netten, J.J. Adherence and Wearing Time of Prescribed Footwear among People at Risk of Diabetes-Related Foot Ulcers: Which Measure to Use? Sensors 2023, 23, 1648. [Google Scholar] [CrossRef]
- Exterkate, S.H.; Jongebloed-Westra, M.; Ten Klooster, P.M.; Koffijberg, H.; Bode, C.; van Gemert-Pijnen, J.; van Baal, J.G.; van Netten, J.J. Objectively assessed long-term wearing patterns and predictors of wearing orthopaedic footwear in people with diabetes at moderate-to-high risk of foot ulceration: A 12 months observational study. J. Foot Ankle Res. 2023, 16, 60. [Google Scholar] [CrossRef]
- Waaijman, R.; Keukenkamp, R.; de Haart, M.; Polomski, W.P.; Nollet, F.; Bus, S.A. Adherence to wearing prescription custom-made footwear in patients with diabetes at high risk for plantar foot ulceration. Diabetes Care 2013, 36, 1613–1618. [Google Scholar] [CrossRef]
- Keukenkamp, R.; Van Netten, J.J.; Busch-Westbroek, T.E.; Bus, S.A. Custom-made footwear designed for indoor use increases short-term and long-term adherence in people with diabetes at high ulcer risk. BMJ Open Diabetes Res. Care 2022, 10, e002593. [Google Scholar] [CrossRef]
- Ehrmann, D.; Spengler, M.; Jahn, M.; Niebuhr, D.; Haak, T.; Kulzer, B.; Hermanns, N. Adherence Over Time: The Course of Adherence to Customized Diabetic Insoles as Objectively Assessed by a Temperature Sensor. J. Diabetes Sci. Technol. 2018, 12, 695–700. [Google Scholar] [CrossRef]
- López-Moral, M.; Lázaro-Martínez, J.L.; García-Morales, E.; García-Álvarez, Y.; JavierÁlvaro-Afonso, F.; Molines-Barroso, R.J. Clinical efficacy of therapeutic footwear with a rigid rocker sole in the prevention of recurrence in patients with diabetes mellitus and diabetic polineuropathy: A randomized clinical trial. PLoS ONE 2019, 14, e0219537. [Google Scholar] [CrossRef]
- Racaru, S.; Bolton Saghdaoui, L.; Roy Choudhury, J.; Wells, M.; Davies, A.H. Offloading treatment in people with diabetic foot disease: A systematic scoping review on adherence to foot offloading. Diabetes Metab. Syndr. 2022, 16, 102493. [Google Scholar] [CrossRef] [PubMed]
- Van Netten, J.J.; Raspovic, A.; Lavery, L.A.; Monteiro-Soares, M.; Paton, J.; Rasmussen, A.; Sacco, I.C.N.; Bus, S.A. Prevention of foot ulcers people with diabetes at risk of ulceration: A systematic review and meta-analysis. Diabetes Metab. Res. Rev. 2024, 40, e3652. [Google Scholar] [CrossRef]
- Miller, W.R.; Rollnick, S. Motivational Interviewing: Helping People Change, 3rd ed.; Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Keukenkamp, R.; Merkx, M.J.; Busch-Westbroek, T.E.; Bus, S.A. An Explorative Study on the Efficacy and Feasibility of the Use of Motivational Interviewing to Improve Footwear Adherence in Persons with Diabetes at High Risk for Foot Ulceration. J. Am. Podiatr. Med. Assoc. 2018, 108, 90–99. [Google Scholar] [CrossRef] [PubMed]
- Jongebloed-Westra, M.; Exterkate, S.H.; van Netten, J.J.; Kappert, K.D.R.; Koffijberg, H.; Bode, C.; van Gemert-Pijnen, J.; Ten Klooster, P.M. The effectiveness of motivational interviewing on adherence to wearing orthopedic shoes in people with diabetes at low-to-high risk of foot ulceration: A multicenter cluster-randomized controlled trial. Diabetes Res. Clin. Pract. 2023, 204, 110903. [Google Scholar] [CrossRef] [PubMed]
- van Netten, J.J.; Dahmen, R.; Holtkamp, F.; Aussems, J.P.; Jansen, G.; Mik, E.; Bus, S.A. Development of a research agenda for medical grade footwear in the Netherlands: A multidisciplinary multiphase project to determine the key research questions to advance scientific knowledge in the field. J. Foot Ankle Res. 2024, 17, e12016. [Google Scholar] [CrossRef]
- Michie, S.; van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. IS 2011, 6, 42. [Google Scholar] [CrossRef]
- Vossen, L.E.; van Netten, J.J.; Bakker, C.D.; Berendsen, H.A.; Busch-Westbroek, T.E.; Peters, E.J.G.; Sabelis, L.W.E.; Dijkgraaf, M.G.W.; Bus, S.A. An integrated personalized assistive devices approach to reduce the risk of foot ulcer recurrence in diabetes (DIASSIST): Study protocol for a multicenter randomized controlled trial. Trials 2023, 24, 663. [Google Scholar] [CrossRef]
- Binning, J.; Woodburn, J.; Bus, S.A.; Barn, R. Motivational interviewing to improve adherence behaviours for the prevention of diabetic foot ulceration. Diabetes Metab. Res. Rev. 2019, 35, e3105. [Google Scholar] [CrossRef]
- Paton, J.; Abey, S.; Hendy, P.; Williams, J.; Collings, R.; Callaghan, L. Behaviour change approaches for individuals with diabetes to improve foot self-management: A scoping review. J. Foot Ankle Res. 2021, 14, 1. [Google Scholar] [CrossRef]
- Price, C.; Parker, D.; Nester, C. Validity and repeatability of three in-shoe pressure measurement systems. Gait Posture 2016, 46, 69–74. [Google Scholar] [CrossRef]
- Bus, S.A.; de Lange, A. A comparison of the 1-step, 2-step, and 3-step protocols for obtaining barefoot plantar pressure data in the diabetic neuropathic foot. Clin. Biomech. 2005, 20, 892–899. [Google Scholar] [CrossRef] [PubMed]
- van Schooten, K.S.; Rispens, S.M.; Elders, P.J.; Lips, P.; van Dieen, J.H.; Pijnappels, M. Assessing physical activity in older adults: Required days of trunk accelerometer measurements for reliable estimation. J. Aging Phys. Act. 2015, 23, 9–17. [Google Scholar] [CrossRef]
- Rabin, R.; de Charro, F. EQ-5D: A measure of health status from the EuroQol Group. Ann. Med. 2001, 33, 337–343. [Google Scholar] [CrossRef] [PubMed]
- Ware, J.E., Jr.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care. 1992, 30, 473–483. [Google Scholar] [CrossRef] [PubMed]
- Lutjeboer, T.; van Netten, J.J.; Postema, K.; Hijmans, J.M. Validity and feasibility of a temperature sensor for measuring use and non-use of orthopaedic footwear. J. Rehabil. Med. 2018, 50, 920–926. [Google Scholar] [CrossRef]
- Hulshof, C.M.; van Netten, J.J.; Oosterhof, C.M.; van der Poel, J.; Pijnappels, M.; Bus, S.A. New biomechanical models for cumulative plantar tissue stress assessment in people with diabetes at high risk of foot ulceration. J. Biomech. 2024, 163, 111940. [Google Scholar] [CrossRef]
- Reaney, M.; Gladwin, T.; Chmiel, N.; Churchill, S. Encouraging foot care in people with and without diabetes through narrative communication. J. Health Psychol. 2022, 27, 1993–2012. [Google Scholar] [CrossRef]
- Heng, M.L.; Kwan, Y.H.; Ilya, N.; Ishak, I.A.; Jin, P.H.; Hogan, D.; Carmody, D. A collaborative approach in patient education for diabetes foot and wound care: A pragmatic randomised controlled trial. Int. Wound J. 2020, 17, 1678–1686. [Google Scholar] [CrossRef]
- Satehi, S.B.; Zandi, M.; Derakhshan, H.B.; Nasiri, M.; Tahmasbi, T. Investigating and Comparing the Effect of Teach-Back and Multimedia Teaching Methods on Self-Care in Patients With Diabetic Foot Ulcers. Clin. Diabetes 2021, 39, 146–152. [Google Scholar] [CrossRef]
- Jarl, G.; van Netten, J.J.; Lazzarini, P.A. Fragile Feet and Trivial Trauma: Communicating the Etiology of Diabetic Foot Ulcers to Patients. J. Am. Podiatr. Med. Assoc. 2023, 113, 21-027. [Google Scholar] [CrossRef]
- Pascal, B. Pensées de M. Pascal sur la Religion et sur Quelques Autres Sujets; Guillaume Desprez: Paris, France, 1669. [Google Scholar]
- Kaczmarek, T.; Kavanagh, D.J.; Lazzarini, P.A.; Warnock, J.; Van Netten, J.J. Training diabetes healthcare practitioners in motivational interviewing: A systematic review. Health Psychol. Rev. 2021, 16, 430–449. [Google Scholar] [CrossRef] [PubMed]
- Teeter, B.S.; Kavookjian, J. Telephone-based motivational interviewing for medication adherence: A systematic review. Transl. Behav. Med. 2014, 4, 372–381. [Google Scholar] [CrossRef][Green Version]
- Spencer, J.C.; Wheeler, S.B. A systematic review of Motivational Interviewing interventions in cancer patients and survivors. Patient Educ. Couns. 2016, 99, 1099–1105. [Google Scholar] [CrossRef]
- Jelsma, J.G.; Mertens, V.C.; Forsberg, L.; Forsberg, L. How to Measure Motivational Interviewing Fidelity in Randomized Controlled Trials: Practical Recommendations. Contemp. Clin. Trials. 2015, 43, 93–99. [Google Scholar] [CrossRef]
- Moyers, T.B.; Manuel, J.K.; Ernst, D. Motivational Interviewing Treatment Integrity Coding Manual 4.2.1. 2014. Available online: https://motivationalinterviewing.org/sites/default/files/miti4_2.pdf (accessed on 16 May 2025).
- Keukenkamp, R.; van Netten, J.J.; Busch-Westbroek, T.E.; Nollet, F.; Bus, S.A. Users’ needs and expectations and the design of a new custom-made indoor footwear solution for people with diabetes at risk of foot ulceration. Disabil. Rehabil. 2021, 44, 8493–8500. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; Richardson, M.; Johnston, M.; Abraham, C.; Francis, J.; Hardeman, W.; Eccles, M.P.; Cane, J.; Wood, C.E. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: Building an international consensus for the reporting of behavior change interventions. Ann. Behav. Med. 2013, 46, 81–95. [Google Scholar] [CrossRef] [PubMed]
- Kaczmarek, T.; Van Netten, J.J.; Lazzarini, P.A.; Kavanagh, D. Effects of training podiatrists to use imagery-based motivational interviewing when treating people with diabetes-related foot disease: A mixed-methods pilot study. J. Foot Ankle Res. 2021, 14, 12. [Google Scholar] [CrossRef]
- Jongebloed-Westra, M.; Bode, C.; Bente, B.E.; de Jonge, J.M.; Ten Klooster, P.M.; Koffijberg, H.; Exterkate, S.H.; van Netten, J.J.; van Gemert-Pijnen, J. Attitudes and experiences towards the application of motivational interviewing by podiatrists working with people with diabetes at high-risk of developing foot ulcers: A mixed-methods study. J. Foot Ankle Res. 2022, 15, 62. [Google Scholar] [CrossRef]
- Bus, S.A.; Aan de Stegge, W.B.; van Baal, J.G.; Busch-Westbroek, T.E.; Nollet, F.; van Netten, J.J. Effectiveness of at-home skin temperature monitoring in reducing the incidence of foot ulcer recurrence in people with diabetes: A multicenter randomized controlled trial (DIATEMP). BMJ Open Diabetes Res. Care 2021, 9, e002392. [Google Scholar] [CrossRef]
- Hancox, J.E.; Chaplin, W.J.; Hilton, C.E.; Vadaszy, N.; Gray, K.; Game, F.; Vedhara, K. Motivation communication training programme for healthcare professionals to support adherence in patients with diabetic foot ulcers: Proof of concept study. PLoS ONE 2024, 19, e0295180. [Google Scholar] [CrossRef]
- Magill, M.; Gaume, J.; Apodaca, T.R.; Walthers, J.; Mastroleo, N.R.; Borsari, B.; Longabaugh, R. The technical hypothesis of motivational interviewing: A meta-analysis of MI’s key causal model. J. Consult. Clin. Psychol. 2014, 82, 973–983. [Google Scholar] [CrossRef] [PubMed]
- Pace, B.T.; Dembe, A.; Soma, C.S.; Baldwin, S.A.; Atkins, D.C.; Imel, Z.E. A multivariate meta-analysis of motivational interviewing process and outcome. Psychol. Addict. Behav. 2017, 31, 524–533. [Google Scholar] [CrossRef]
- van Netten, J.J.; Jannink, M.J.; Hijmans, J.M.; Geertzen, J.H.; Postema, K. Use and usability of custom-made orthopedic shoes. J. Rehabil. Res. Dev. 2010, 47, 73–81. [Google Scholar] [CrossRef]
- van Netten, J.J.; Francis, A.; Morphet, A.; Fortington, L.V.; Postema, K.; Williams, A. Communication techniques for improved acceptance and adherence with therapeutic footwear. Prosthet. Orthot. Int. 2017, 41, 201–204. [Google Scholar] [CrossRef]
- World Health Organization. Adherence to Long-Term Therapies: Evidence for Action; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Jarl, G.; Tranberg, R.; Johansson, U.; Alnemo, J.; Lundqvist, L.O. Predictors of adherence to wearing therapeutic footwear among people with diabetes. J. Foot Ankle Res. 2020, 13, 45. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.; Wong, D.; Barson, E.; Staunton, E.T.; Fisher, C.A. Psychological and Cognitive Barriers to Diabetes-Related Foot Complication Treatment: Clinicians’ Perspectives. Int. J. Low. Extrem. Wounds. 2022, 21, 617–631. [Google Scholar] [CrossRef] [PubMed]
- Norman, G.; Westby, M.J.; Vedhara, K.; Game, F.; Cullum, N.A. Effectiveness of psychosocial interventions for the prevention and treatment of foot ulcers in people with diabetes: A systematic review. Diabet. Med. 2020, 37, 1256–1265. [Google Scholar] [CrossRef]
- Arts, M.L.; Waaijman, R.; de Haart, M.; Keukenkamp, R.; Nollet, F.; Bus, S.A. Perceived usability and use of custom-made footwear in diabetic patients at high risk for foot ulceration. J. Rehabil. Med. 2014, 46, 357–362. [Google Scholar] [CrossRef]


| Variable | N = 53 |
|---|---|
| General characteristics | |
| Sex (female/male) | 17% (9)/83% (44) |
| Age (years) | 65.7 ± 10 |
| BMI (kg/m2) | 29.6 ± 5.7 |
| Ethnicity (Caucasian) | 94% (58) |
| Level of education | |
| Low | 34% (18) |
| Medium | 40% (21) |
| High | 26% (14) |
| Living situation (alone/together) | 28% (15)/72% (38) |
| Work situation (employed/unemployed) | 30% (16)/70% (37) |
| Smoking | |
| Yes | 9% (5) |
| No | 32% (17) |
| History of smoking | 59% (31) |
| Alcohol | |
| Yes | 53% (28) |
| Special occasions | 11% (6) |
| No | 36% (19) |
| Use of a walking aid | 32% (17) |
| Quality of life (EQ5D) a | 4.1 ± 0.6 |
| Quality of life—physical functioning b | 53 ± 24 |
| Quality of life—physical limitations b | 45 ± 42 |
| Quality of life—emotional limitations b | 68 ± 39 |
| Quality of life—energy and fatigue b | 57 ± 21 |
| Quality of life—emotional wellbeing b | 77 ± 18 |
| Quality of life—social functioning b | 72 ± 25 |
| Quality of life—pain b | 68 ± 22 |
| Quality of life—general health b | 46 ± 18 |
| Daily steps | 5246 ± 3538 |
| Footwear adherence | 64% ± 24% |
| Footwear adherence indoor | 57% ± 29% |
| Footwear adherence outdoor | 77% ± 27% |
| Diabetes-related characteristics | |
| Type of diabetes (1/2) | 17% (9)/83% (44) |
| Duration of diabetes (years) | 19.1 ± 11 |
| HbA1c (mmol/mol) | 60.5 ± 18 |
| Neuropathy | 100% (53) |
| Inability to feel 10 g monofilament | 96% (51) |
| Inability to feel tuning fork | 94% (50) |
| Comorbidities | |
| Intermittent claudication | 28% (15) |
| Retinopathy | 77% (41) |
| Laser therapy | 24% (10) |
| Nephropathy | 38% (20) |
| Dialysis | 4% (2) |
| Foot-related characteristics | |
| Time since healing last ulcer (months) | 6.1 ± 9.3 |
| History of Charcot | 15% (8) |
| Amputations | |
| Absent | 60% (32) |
| Digiti 2–5 | 11% (6) |
| Hallux | 6% (3) |
| Metatarsal region | 19 (10) |
| Forefoot or higher | 4% (2) |
| Foot deformities c | |
| Absent | 0% (0) |
| Mild | 6% (3) |
| Moderate | 76% (40) |
| Severe | 18% (10) |
| Personal risk assessments | |
| How bad would you feel if you get a new ulcer? d | 72 ± 27 |
| How do you assess your risk of getting a new ulcer? d | 37 ± 28 |
| n | Before (Hours/Day) | After (Hours/Day) | Difference (95% CI) | p-Value | |
|---|---|---|---|---|---|
| Primary outcome (ITT) | |||||
| All | 53 | 7.5 (4.6) | 8.3 (4.9) | 0.9 (−0.2–1.9) | 0.095 |
| Low baseline adherence | 30 | 4.0 (2.5) | 5.5 (4.3) | 1.5 (−0.1–3.1) | 0.068 |
| High baseline adherence | 23 | 11.9 (2.3) | 12.0 (2.8) | 0.1 (−1.1–1.3) | 0.898 |
| Primary outcome (PP) | |||||
| Low baseline adherence | 24 | 3.7 (2.4) | 5.1 (3.9) | 1.4 (−0.5–3.2) | 0.136 |
| High baseline adherence | 16 | 11.9 (2.6) | 12.5 (2.3) | 0.6 (−0.8–1.9) | 0.405 |
| Modality analyses | |||||
| Low baseline adherence | |||||
| Structured education | 24 | 4.1 (2.6) | 5.1 (3.1) | 1.0 (−0.2–2.2) | 0.098 |
| Motivational interviewing | 25 | 6.1 (3.7) | 6.0 (4.3) | −0.2 (−1.2–0.9) | 0.763 |
| Indoor footwear | 19 | 5.0 (3.5) | 7.7 (3.6) | 2.7 (1.0–4.4) | 0.004 |
| High baseline adherence | |||||
| Structured education | 19 | 12.0 (2.3) | 12.1 (2.9) | 0.0 (−0.9–0.9) | 0.967 |
| Motivational interviewing | 15 | 11.7 (2.8) | 11.0 (3.2) | −0.7 (−2.4–1.0) | 0.383 |
| Indoor footwear | 16 | 10.7 (3.5) | 12.6 (2.0) | 2.0 (0.5–3.4) | 0.010 |
| MITI Variable | DIASSIST | Comparison | |||
|---|---|---|---|---|---|
| All (n = 20) | Change (n = 12) | Sustain (n = 8) | AU (n = 11) | NL (n = 14) | |
| Global scores—technical a | |||||
| Change talk | 3.9 (0.8) | 3.8 (0.8) | 3.9 (0.8) | 3.1 (1.3) | 3.2 (1.0) |
| Soften sustain | 3.3 (0.6) | 3.0 (0.6) | 3.6 (0.5) * | 1.4 (1.6) | 3.0 (0.6) |
| Global scores—relational a | |||||
| Partnership | 3.0 (0.9) | 2.8 (0.6) | 3.3 (1.3) | 3.1 (1.0) | 2.7 (0.7) |
| Empathy | 4.0 (0.7) | 4.0 (0.5) | 4.0 (0.9) | 3.1 (1.0) | 3.6 (0.8) |
| Behaviour counts b | |||||
| Giving information | 5.4 (3.1) | 4.1 (2.0) | 7.3 (3.5) * | 13.4 (5.1) | 2.9 (2.1) |
| Questions | 16.7 (9.1) | 18.0 (9.8) | 14.8 (8.2) | 18.9 (5.3) | 13.8 (7.7) |
| Simple reflection | 10.9 (4.6) | 10.0 (4.3) | 12.3 (4.9) | 2.4 (1.7) | 9.1 (5.6) |
| Complex reflection | 7.8 (4.8) | 8.1 (5.1) | 7.2 (4.7) | 1.1 (1.2) | 3.0 (2.7) |
| Persuade with permission | 0.8 (1.2) | 0.8 (0.9) | 0.9 (1.7) | 0.1 (0.3) | 0.6 (0.9) |
| MI-adherent behaviour b,c | |||||
| Affirm | 4.0 (1.9) | 3.2 (1.6) | 5.1 (1.9) * | 0.6 (0.8) | 3.8 (3.3) |
| Seeking collaboration | 2.7 (2.2) | 2.2 (1.8) | 3.4 (2.7) | 2.9 (2.3) | 0.6 (0.9) |
| Emphasising autonomy | 0.1 (0.4) | 0 (0) | 0.3 (0.7) | 0.4 (0.6) | 0.1 (0.3) |
| MI non-adherent behaviour b,d | |||||
| Persuade | 2.0 (1.6) | 2.2 (1.9) | 1.6 (1.2) | 0.4 (0.7) | 3.4 (2.7) |
| Confront | 0.3 (0.7) | 0.3 (0.5) | 0.4 (1.0) | - | 0.5 (1.0) |
| MITI summary scores | |||||
| Relational score a | 3.5 (0.7) | 3.4 (0.5) | 3.6 (1.0) | - | 3.1 (0.7) |
| Technical score a | 3.6 (0.6) | 3.4 (0.6) | 3.8 (0.6) | - | 3.1 (0.7) |
| Reflection:question ratio e | 1.5 (1.1) | 1.2 (0.6) | 2.0 (1.6) | - | 1.0 (0.6) |
| % complex reflections f | 40 (17) | 43 (20) | 36 (13) | - | 23 (15) |
| MI consistent b | 6.8 (2.9) | 5.4 (1.8) | 8.8 (3.1) ** | - | 4.4 (3.9) |
| MI inconsistent b | 2.3 (1.7) | 2.4 (1.8) | 2.0 (1.7) | - | 3.9 (3.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van Netten, J.J.; Vossen, L.E.; Driebergen, F.M.; Wolthuis, D.; Merkx, M.J.M.; Bus, S.A. Short-Term Efficacy of a Multi-Modal Intervention Program to Improve Custom-Made Footwear Use in People at High Risk of Diabetes-Related Foot Ulceration. J. Clin. Med. 2025, 14, 3635. https://doi.org/10.3390/jcm14113635
Van Netten JJ, Vossen LE, Driebergen FM, Wolthuis D, Merkx MJM, Bus SA. Short-Term Efficacy of a Multi-Modal Intervention Program to Improve Custom-Made Footwear Use in People at High Risk of Diabetes-Related Foot Ulceration. Journal of Clinical Medicine. 2025; 14(11):3635. https://doi.org/10.3390/jcm14113635
Chicago/Turabian StyleVan Netten, Jaap J., Lisa E. Vossen, Faye M. Driebergen, Danne Wolthuis, Maarten J. M. Merkx, and Sicco A. Bus. 2025. "Short-Term Efficacy of a Multi-Modal Intervention Program to Improve Custom-Made Footwear Use in People at High Risk of Diabetes-Related Foot Ulceration" Journal of Clinical Medicine 14, no. 11: 3635. https://doi.org/10.3390/jcm14113635
APA StyleVan Netten, J. J., Vossen, L. E., Driebergen, F. M., Wolthuis, D., Merkx, M. J. M., & Bus, S. A. (2025). Short-Term Efficacy of a Multi-Modal Intervention Program to Improve Custom-Made Footwear Use in People at High Risk of Diabetes-Related Foot Ulceration. Journal of Clinical Medicine, 14(11), 3635. https://doi.org/10.3390/jcm14113635







