The Effect of Thermal-Softened Endotracheal Tubes on Postoperative Sore Throat and Other Complications—A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.1.1. Participants
2.1.2. Interventions
2.1.3. Comparators
2.1.4. Outcomes
2.2. Search Strategy and Study Selection
2.3. Data Extraction and Methodological Quality Appraisal
2.4. Statistical Analysis
2.5. Subgroup and Sensitivity Analysis
2.6. Assessment of Publication Bias
2.7. Certainty of Evidence (GRADE Assessment)
3. Results
3.1. Study Selection
3.2. Characteristics of the Included Studies
3.2.1. Intubation Methods
3.2.2. Cuff Pressure Management
3.2.3. Participant Demographics and Inclusion Criteria
3.2.4. Use of Adjunctive Medications
3.2.5. Thermal Softening Protocols
| Study | Inclusion Criteria | No. of Patients (Male) | Age | Intubation Method | Types of Tube | Cuff Pressure | Premedication with Dexamethasone or Lidocaine | Intervention |
|---|---|---|---|---|---|---|---|---|
| Bi et al., 2022 [20] | Smokers for >5 years One-lung anesthesia surgery | C = 129 (100) TS = 129 (97) | >18 | Direct laryngoscope | PVC DLT | Tracheal: <25 cmH2O Bronchial: <44 cmH2O | No | 40 °C NS for 10 min |
| Hosseinzadeh et al., 2013 [15] | Elective maxillofacial surgery | C = 30 TS = 30 | 15–65 | Blind nasal intubation | Nasal tube | n/a | No | 50 °C for 5 min |
| Mohseni et al., 2022 [17] | Elective surgery except for head and chest surgery | C = 29 (12) TS = 29 (13) | 19–69 | N/A | SLT | Inflate until no leak | Lidocaine | 40 °C for 7–8 min |
| Pasha et al., 2015 [16] | Elective maxillofacial surgery | C = 40 (25) TS = 40 (21) | 18–65 | Blind nasal intubation | Nasal tube | n/a | Dexamethasone | 50 °C for 5 min |
| Seo et al., 2016 [21] | Elective thoracic surgery under one-lung anesthesia | C = 70 (37) TS = 70 (40) | 20–75 | Direct laryngoscope | PVC DLT | Tracheal: <25 cmH2O Bronchial: <44 cmH2O | No | 40 °C for 10 min |
| Song et al., 2019 [18] | Elective laparoscopic cholecystectomy or ovarian cystectomy | C = 34 (12) L = 33 (11) TS = 35 (10) TS+L = 34 (8) | 20–70 | Direct laryngoscope | SLT | 20–25 cm H2O | No | L: 2% lidocaine jelly TS: 40 °C for 5 min |
| Yan et al., 2023 [22] | Prior SARS CoV-2 3 months prior to surgery Thoracoscopic lung surgery | C = 60 (31) TS = 60 (33) | 18–75 | Video-laryngoscope | PVC DLT | Tracheal: <25 cmH2O Bronchial: <44 cmH2O | No | 50 °C saline for 10 min |
| Yu et al., 2021 [19] | Elective nose surgery | C = 91 (52) TS = 94 (70) | >18 | Video-laryngoscope | Oral RAE | 20–25 cmH2O | Dexamethasone | 40 °C saline for 10 min |
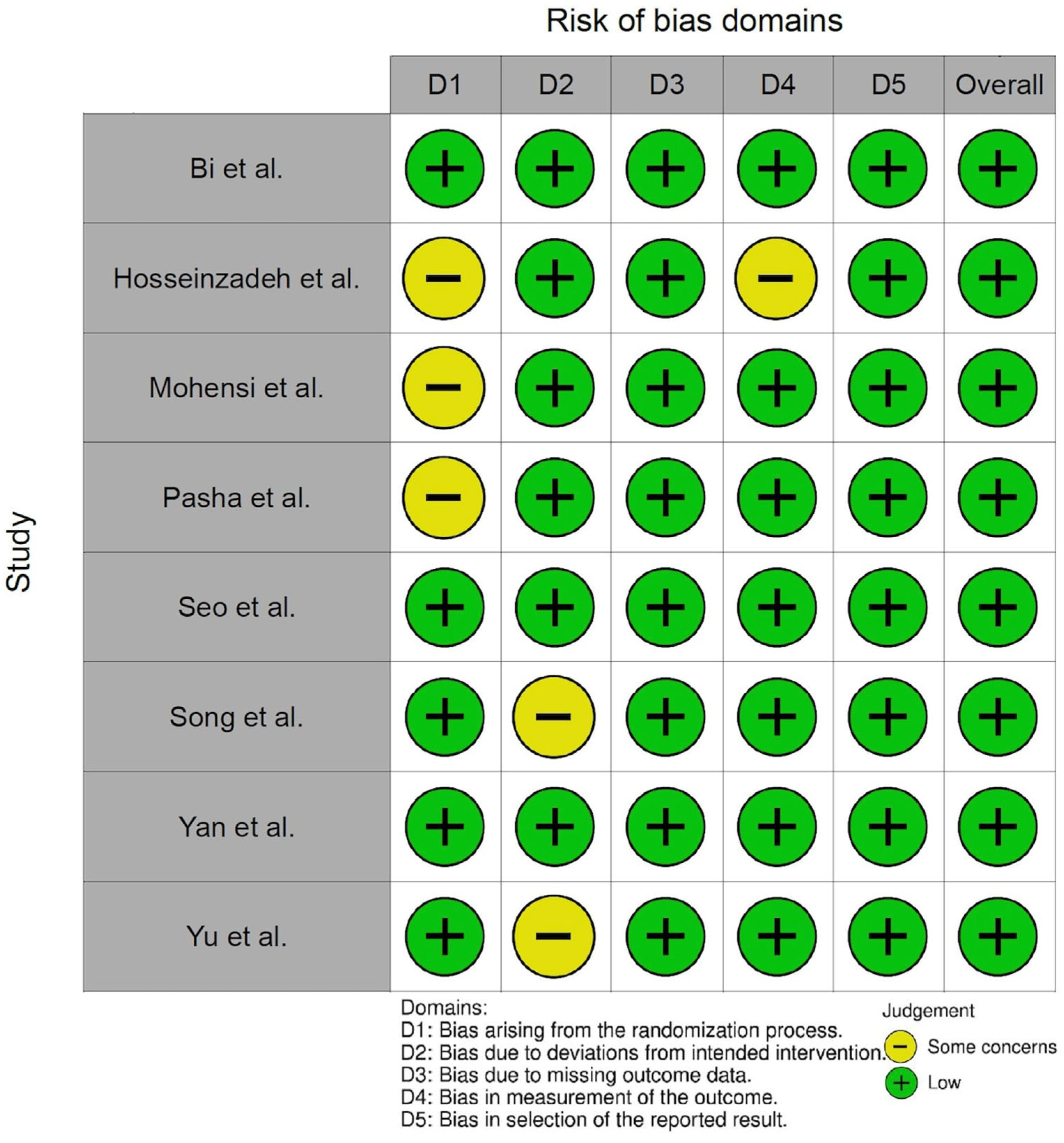
3.3. Risk of Bias Assessment
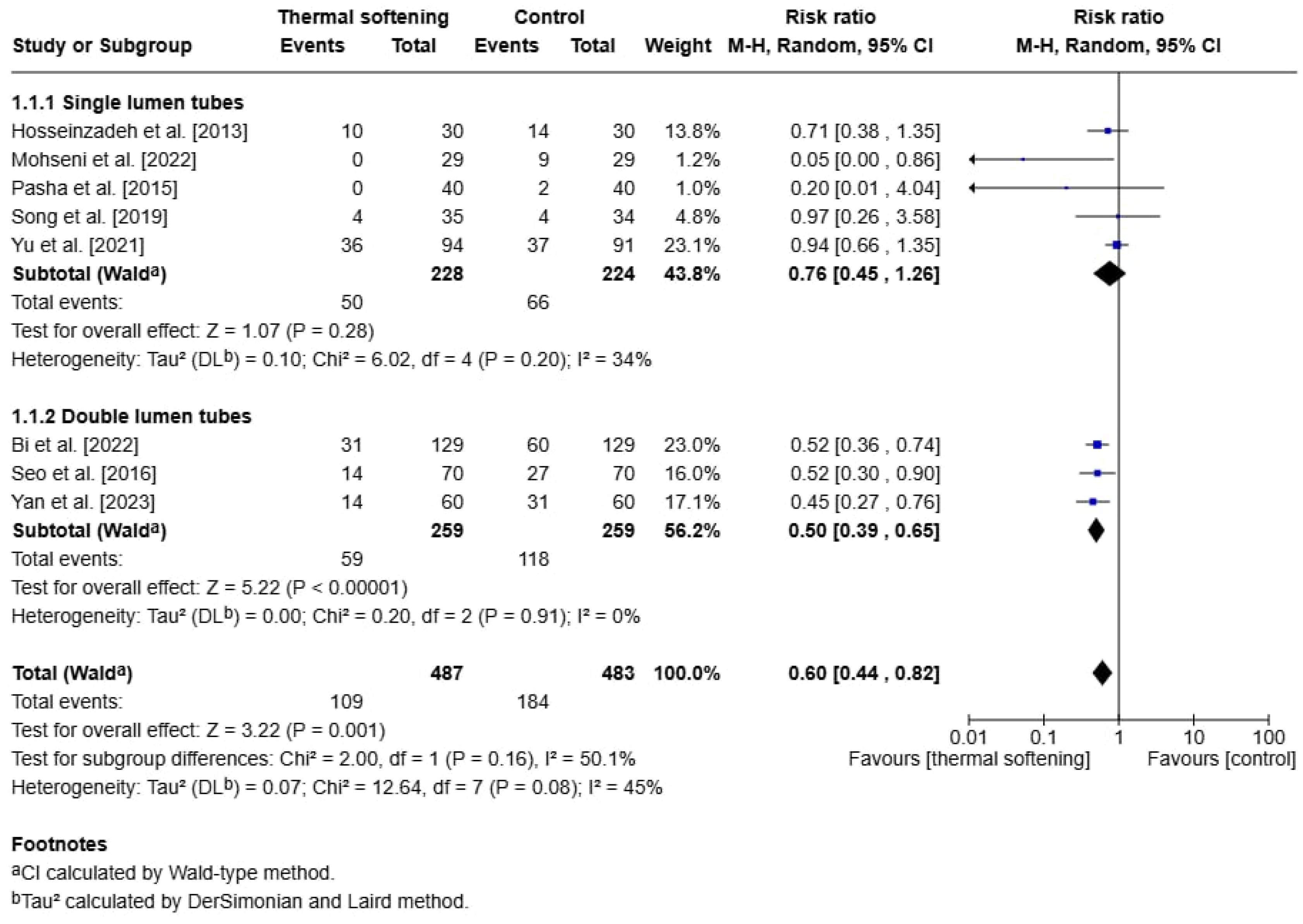
3.4. Primary Outcome: Postoperative Sore Throat
3.4.1. Pooled Analysis
3.4.2. Subgroup Analyses
3.4.3. Sensitivity Analysis
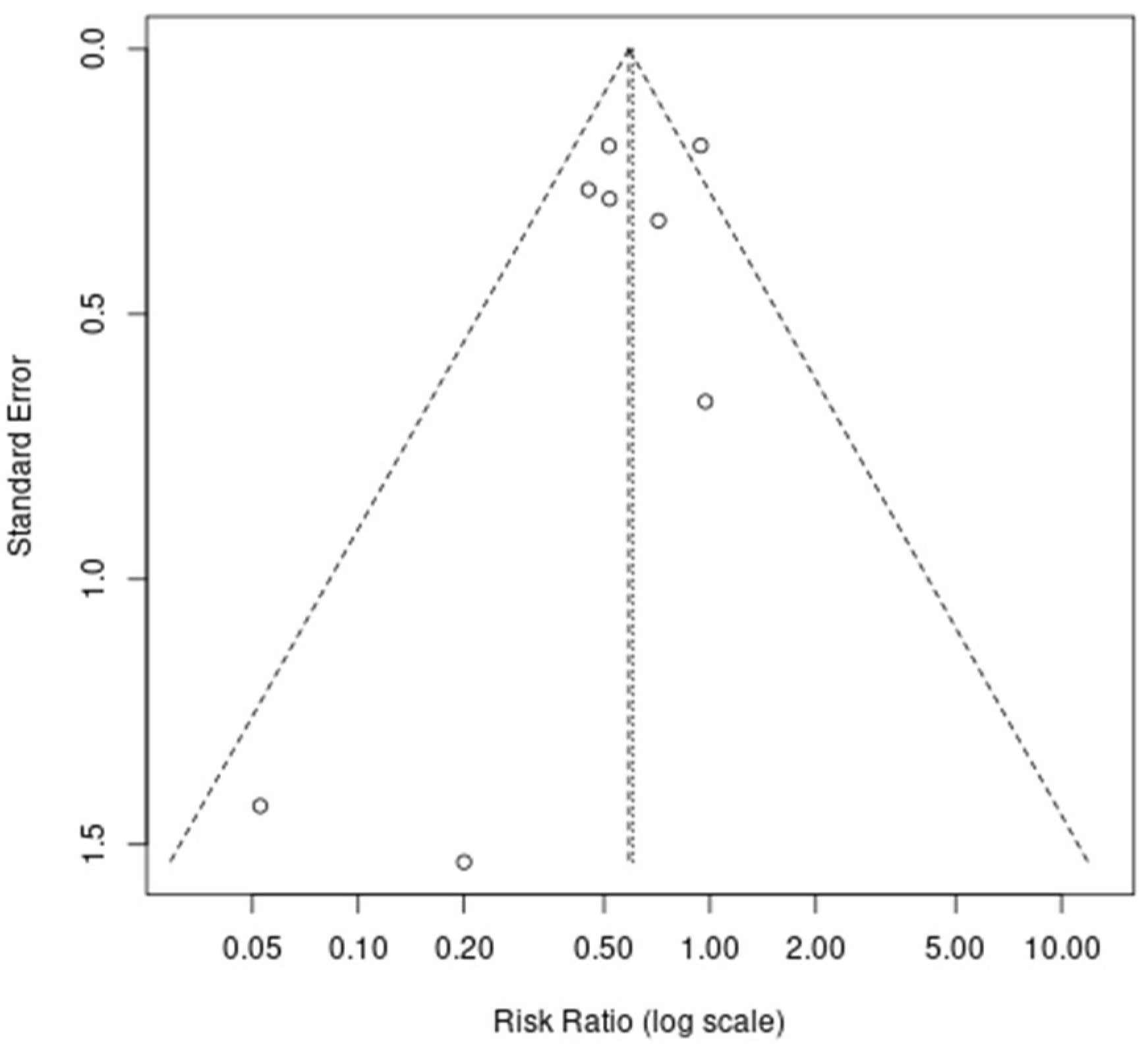
3.4.4. Publication Bias
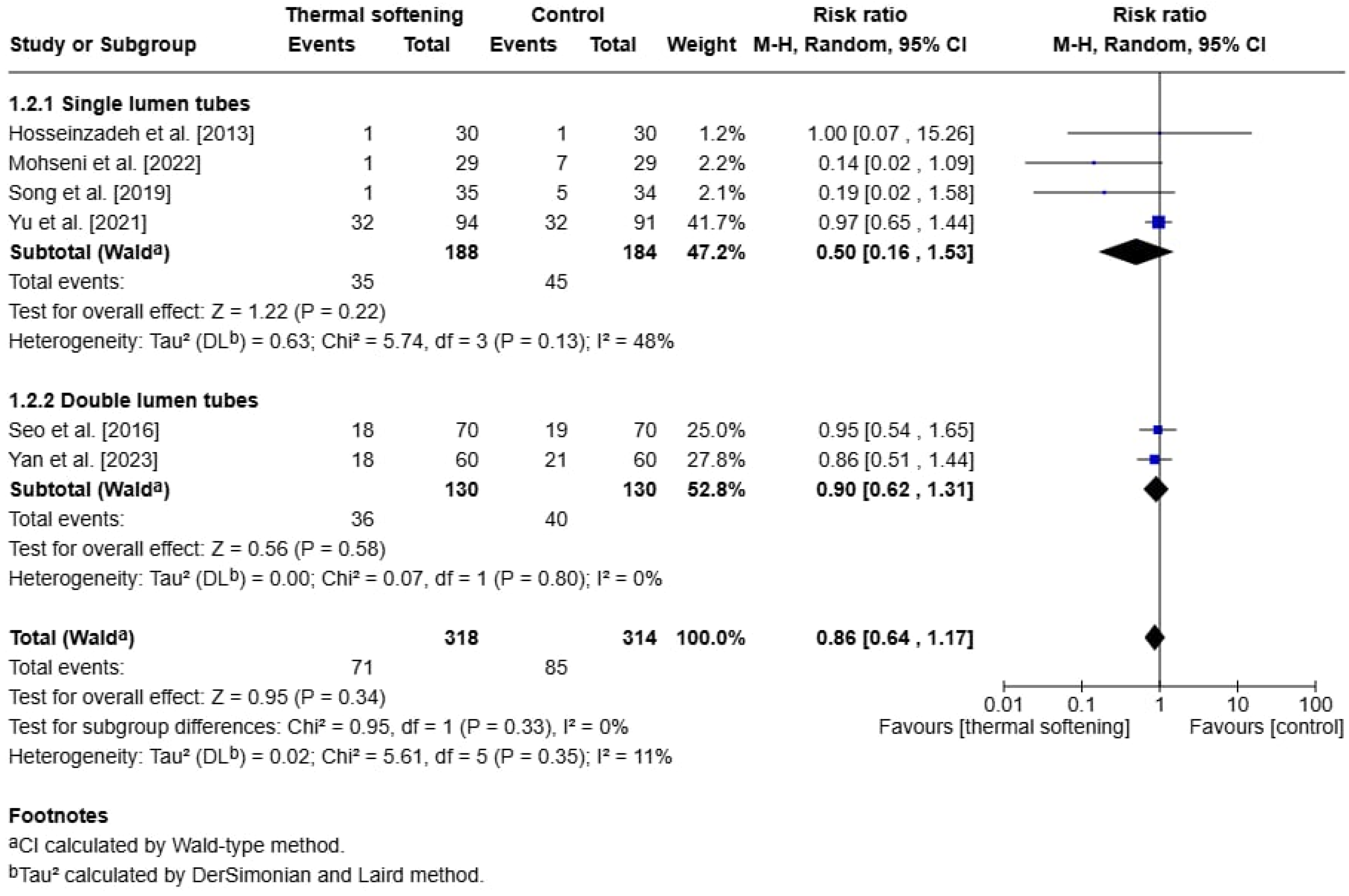
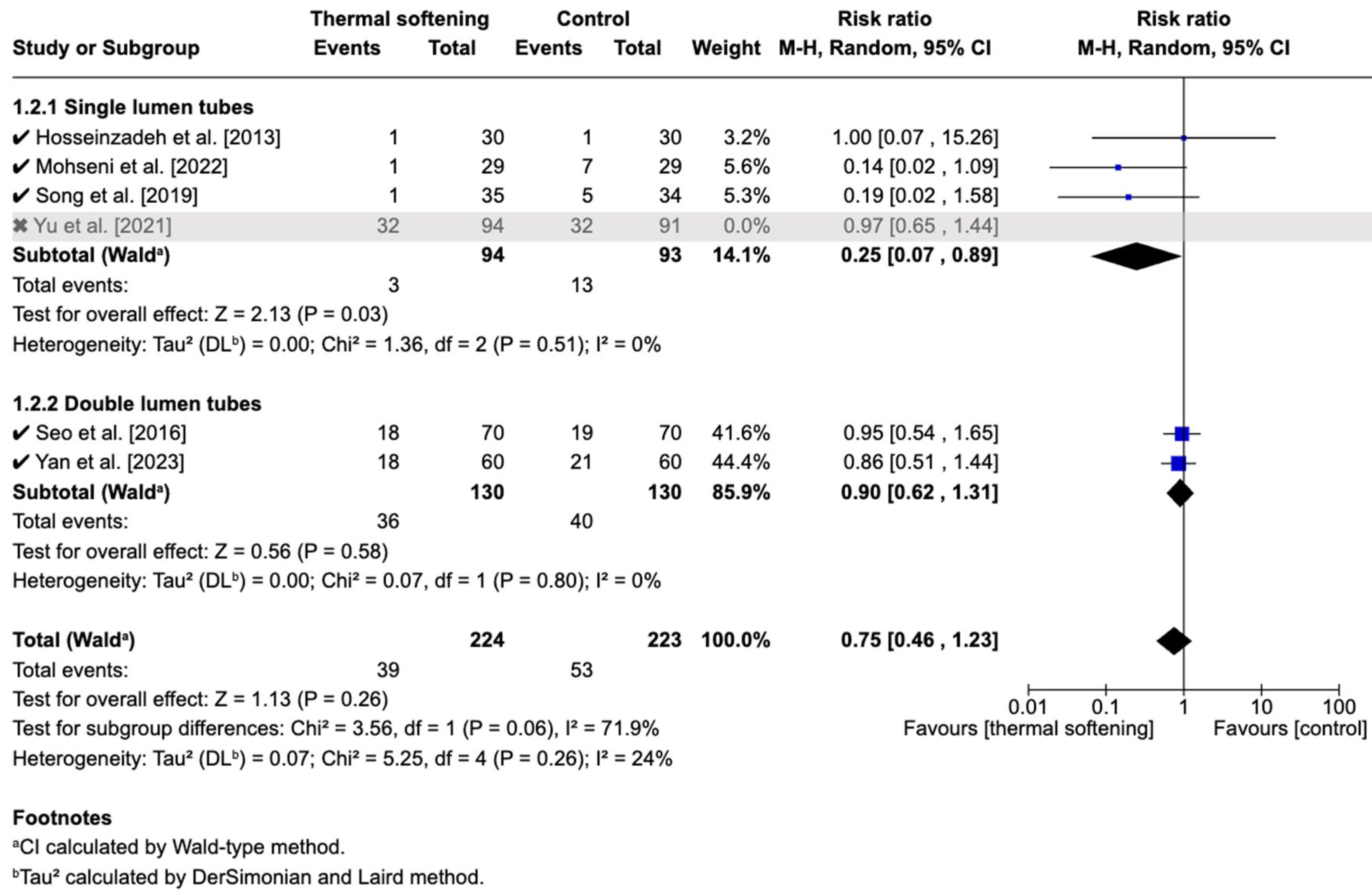
3.5. Secondary Outcome: Postoperative Hoarseness
3.5.1. Pooled Analysis
3.5.2. Subgroup Analysis
3.5.3. Sensitivity Analysis
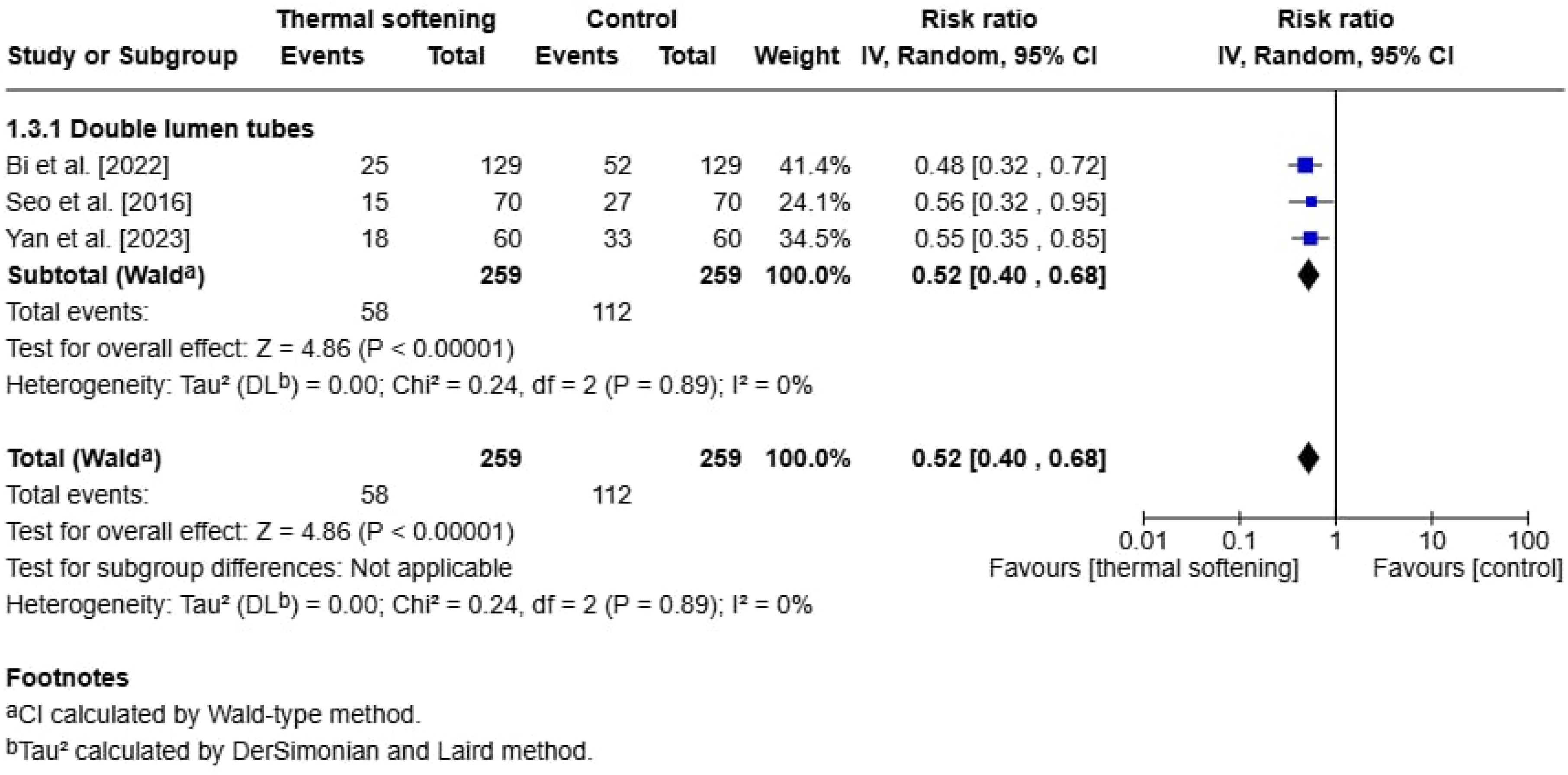
3.6. Secondary Outcome: Vocal Cord Lesions
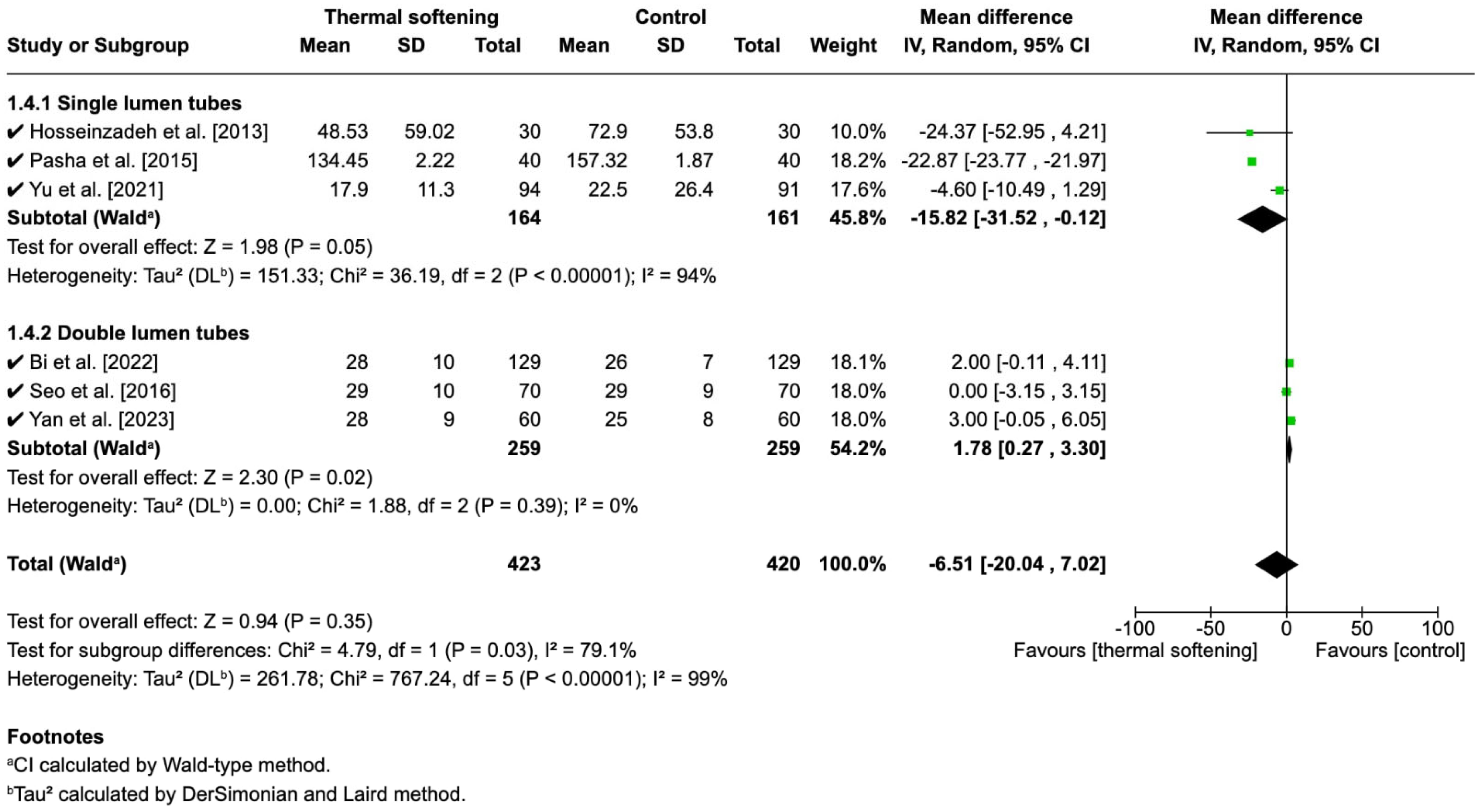
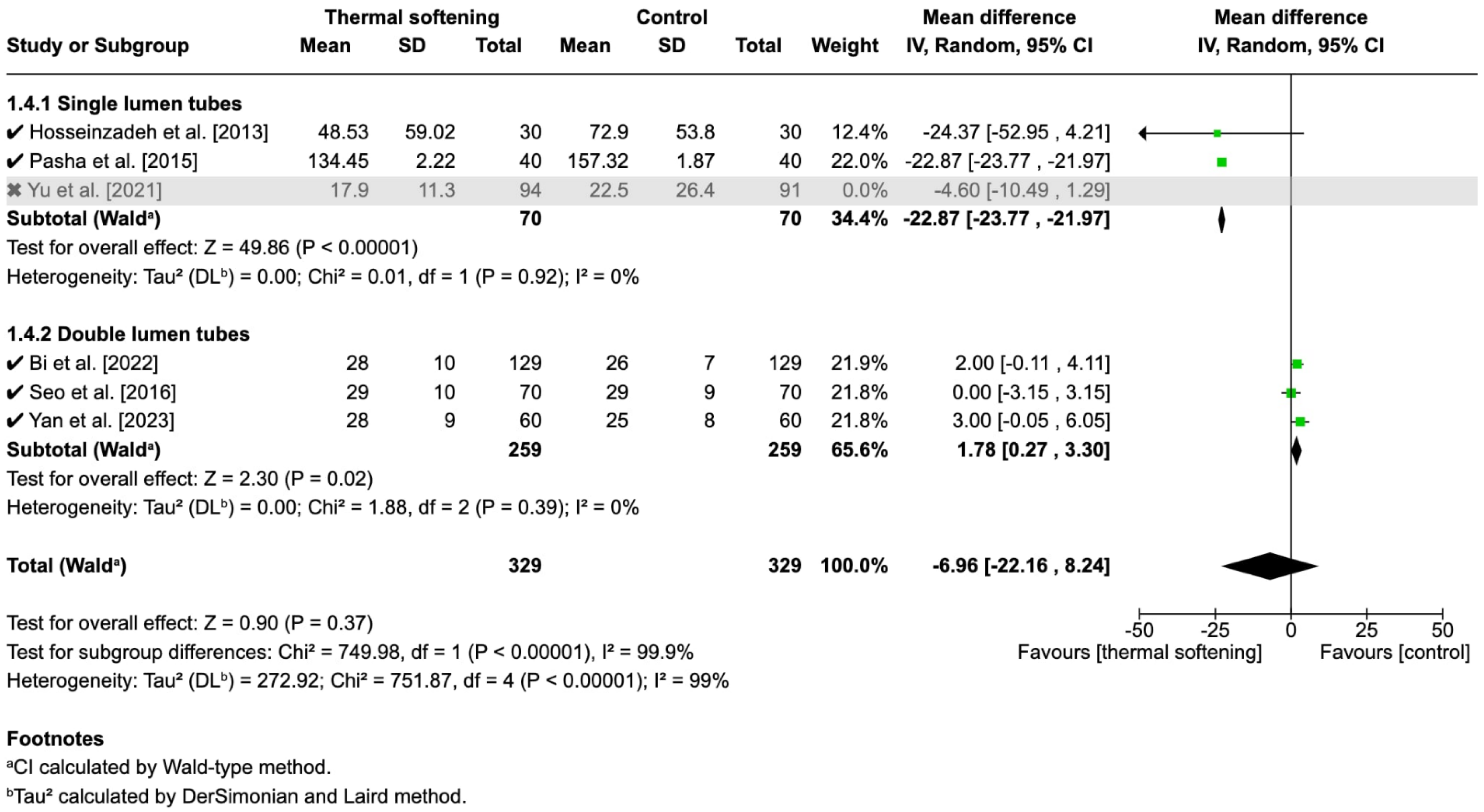
3.7. Secondary Outcome: Time to Intubation
3.7.1. Pooled Analysis
3.7.2. Subgroup Analysis
3.7.3. Sensitivity Analysis
3.8. Summary of Certainty of Evidence
4. Discussion
4.1. Postoperative Sore Throat
4.2. Hoarseness
4.3. Vocal Cord Lesions
4.4. Time to Intubation
4.5. Route of Endotracheal Intubation
4.6. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ETT | Endotracheal tube |
| GA | General anesthesia |
| RCTs | Randomized controlled trials |
| RRs | Risk ratios |
| MDs | Mean differences |
| PROSPERO | Prospective Register of Systematic Reviews |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-analysis |
| SLT | Single-lumen endotracheal tube |
| DLT | Double-lumen endotracheal tube |
References
- El-Boghdadly, K.; Bailey, C.R.; Wiles, M.D. Postoperative sore throat: A systematic review. Anaesthesia 2016, 71, 706–717. [Google Scholar] [CrossRef] [PubMed]
- Macario, A.; Weinger, M.; Truong, P.; Lee, M. Which Clinical Anesthesia Outcomes Are Both Common and Important to Avoid? The Perspective of a Panel of Expert Anesthesiologists. Anesth. Analg. 1999, 88, 1085–1091. [Google Scholar] [CrossRef]
- Mitobe, Y.; Yamaguchi, Y.; Baba, Y.; Yoshioka, T.; Nakagawa, K.; Itou, T.; Kurahashi, K. A Literature Review of Factors Related to Postoperative Sore Throat. J. Clin. Med. Res. 2022, 14, 88–94. [Google Scholar] [CrossRef]
- Maruyama, K.; Sakai, H.; Miyazawa, H.; Toda, N.; Iinuma, Y.; Mochizuki, N.; Hara, K.; Otagiri, T. Sore throat and hoarseness after total intravenous anaesthesia. Br. J. Anaesth. 2004, 92, 541–543. [Google Scholar] [CrossRef]
- Chinachoti, T.; Pojai, S.; Sooksri, N.; Rungjindamai, C. Risk factors of post-operative sore throat and hoarseness. J. Med. Assoc. Thai 2017, 100, 463–468. [Google Scholar]
- Mencke, T.; Echternach, M.; Plinkert, P.K.; Johann, U.; Afan, N.; Rensing, H.; Noeldge-Schomburg, G.; Knoll, H.; Larsen, R. Does the Timing of Tracheal Intubation Based on Neuromuscular Monitoring Decrease Laryngeal Injury? A Randomized, Prospective, Controlled Trial. Anesth. Analg. 2006, 102, 306–312. [Google Scholar] [CrossRef]
- Wang, G.; Qi, Y.; Wu, L.; Jiang, G. Comparative Efficacy of 6 Topical Pharmacological Agents for Preventive Interventions of Postoperative Sore Throat After Tracheal Intubation: A Systematic Review and Network Meta-analysis. Anesth. Analg. 2021, 133, 58–67. [Google Scholar] [CrossRef]
- Kalil, D.M.; Silvestro, L.S.; Austin, P.N. Novel preoperative pharmacologic methods of preventing postoperative sore throat due to tracheal intubation. Aana J. 2014, 82, 188–197. [Google Scholar]
- Özsoy, H.; Yeşilyaprak, T. Non-pharmacological methods in the management of postoperative sore throat in patients undergoing endotracheal intubation: A systematic review. Bezmialem Sci. 2024, 12, 137–144. [Google Scholar] [CrossRef]
- Celik, S.S.; Chalkias, A.; Sariköse, S.; Arslan, H.N.; Bahramifar, A.; Rahimi-Bashar, F.; Hssain, A.A.; Hashemi, S.; Vahedian-Azimi, A. Effect of peri-intubation non-pharmacological interventions on postoperative laryngeal symptoms: A systematic review with meta-analysis and meta-regression. Intensive Crit. Care Nurs. 2024, 84, 103728. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Jia, Q.; Zhou, L.; Liu, Z.; Liang, S.; Yang, Z.; Wan, Q. Appropriate tube temperature for fiberoptic bronchoscope-guided intubation of thermally softened double-lumen endotracheal tubes: A CONSORT-compliant article. Medicine 2022, 101, e29999. [Google Scholar] [CrossRef]
- Kim, E.M.; Chung, M.H.; Lee, M.H.; Choi, E.M.; Jun, I.J.; Yun, T.H.; Ko, Y.K.; Kim, J.H.; Jun, J.H. Is Tube Thermosoftening Helpful for Videolaryngoscope-Guided Nasotracheal Intubation?: A Randomized Controlled Trial. Anesth. Analg. 2019, 129, 812–818. [Google Scholar] [CrossRef]
- Hosseinzadeh, H.; Talesh, K.T.; Golzari, S.E.J.; Gholizadeh, H.; Lotfi, A.; Hosseinzadeh, P. Warming endotracheal tube in blind nasotracheal intubation throughout maxillofacial surgeries. J. Cardiovasc. Thorac. Res. 2013, 5, 147–151. [Google Scholar] [CrossRef]
- Pasha, A.K.; Farhat, K.; Iqbal, A. Evaluating effectiveness of warming endotracheal tube in blind nasotracheal intubation in maxillofacial surgery. J. Postgrad. Med. Inst. 2015, 29, 279–283. [Google Scholar]
- Mohseni, M.; Rad, R.F.; Jafarian, A.A.; Zarisfi, A.H.; Masoudi, N. The Effect of Softening of Endotracheal Tubes on the Decrement of Postoperative Hoarseness and Sore Throat. Anesthesiol. Pain Med. 2022, 12, e123910. [Google Scholar] [CrossRef]
- Song, J.-A.; Lee, S.; Choi, J.-I.; Lee, H.G.; Park, S.Y.; Hwang, J.Y.; Park, S.; Jeong, S. Effect of a combination of 2% lidocaine jelly and thermally softened endotracheal tube on postoperative sore throat. Anesth. Pain Med. 2019, 14, 158–164. [Google Scholar] [CrossRef]
- Yu, J.H.; Paik, H.S.; Ryu, H.G.; Lee, H. Effects of thermal softening of endotracheal tubes on postoperative sore throat: A randomized double-blinded trial. Acta Anaesthesiol. Scand. 2021, 65, 213–219. [Google Scholar] [CrossRef]
- Bi, X.; Wen, J.; Chen, Q.; Zhang, X. Effects of Thermal Softening of Double-Lumen Endobronchial Tubes on the Prevention of Postoperative Sore Throat in Smokers: A Randomized Controlled Trial. J. Cardiothorac. Vasc. Anesth. 2022, 36, 3109–3113. [Google Scholar] [CrossRef]
- Seo, J.H.; Cho, C.W.; Hong, D.M.; Jeon, Y.; Bahk, J.H. The effects of thermal softening of double-lumen endobronchial tubes on postoperative sore throat, hoarseness and vocal cord injuries: A prospective double-blind randomized trial. Br. J. Anaesth. 2016, 116, 282–288. [Google Scholar] [CrossRef] [PubMed]
- Yan, W.; Cai, J.; Zhu, C.; Chen, Y.; Fang, J.; Xu, H.; Zheng, X.; Zhou, Y.; Xie, Y.; Zhang, M.; et al. Effect of thermal softening of double-lumen endobronchial tubes on postoperative sore throat in patients with prior SARS-CoV-2 infection: A randomized controlled trial. BMC Anesthesiol. 2023, 23, 403. [Google Scholar] [CrossRef]
- Liu, J.; Zhang, X.; Gong, W.; Li, S.; Wang, F.; Fu, S.; Zhang, M.; Hang, Y. Correlations Between Controlled Endotracheal Tube Cuff Pressure and Postprocedural Complications: A Multicenter Study. Anesth. Analg. 2010, 111, 1133–1137. [Google Scholar] [CrossRef]
- McHardy, F.E.; Chung, F. Postoperative sore throat: Cause, prevention and treatment. Anaesthesia 1999, 54, 444–453. [Google Scholar] [CrossRef]
- Yang, S.S.; Wang, N.N.; Postonogova, T.; Yang, G.J.; McGillion, M.; Beique, F.; Schricker, T. Intravenous lidocaine to prevent postoperative airway complications in adults: A systematic review and meta-analysis. Br. J. Anaesth. 2020, 124, 314–323. [Google Scholar] [CrossRef]
- Park, S.Y.; Kim, S.H.; Lee, A.R.; Cho, S.H.; Chae, W.S.; Jin, H.C.; Lee, J.S.; Kim, Y.I. Prophylactic effect of dexamethasone in reducing postoperative sore throat. Korean J. Anesthesiol. 2010, 58, 15–19. [Google Scholar] [CrossRef]
- Subedi, A.; Tripathi, M.; Pokharel, K.; Khatiwada, S. Effect of Intravenous Lidocaine, Dexamethasone, and Their Combination on Postoperative Sore Throat: A Randomized Controlled Trial. Anesth. Analg. 2019, 129, 220–225. [Google Scholar] [CrossRef]
- Sterne, J.A.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias Visualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2020, 12, 55–61. [Google Scholar] [CrossRef]
- Higgins, P.P.; Chung, F.; Mezei, G. Postoperative sore throat after ambulatory surgery. Br. J. Anaesth. 2002, 88, 582–584. [Google Scholar] [CrossRef]
- Zhou, Z.; Gao, L.; Lv, Z.; Chen, L.; Lu, K.; Cai, J.; Sun, J.; Chen, X. Prediction of Postoperative Sore Throat in Patients After Day-case Surgery With General Anesthesia: A Retrospective Study. J. PeriAnesthesia Nurs. 2025, 40, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Stout, D.M.; Bishop, M.J.; Dwerstec, J.F.; Cullen, B.F. Correlation of endotracheal tube size with sore throat and hoarseness following general anesthesia. Anesthesiology 1987, 67, 419–421. [Google Scholar] [CrossRef]
- Matta, R.I.; Halan, B.K.; Sandhu, K. Postintubation recurrent laryngeal nerve palsy: A review. J. Laryngol. Voice 2017, 7, 25–28. [Google Scholar] [CrossRef]
- Rubin, A.D.; Hawkshaw, M.J.; Moyer, C.A.; Dean, C.M.; Sataloff, R.T. Arytenoid Cartilage Dislocation: A 20-year Experience. J. Voice 2005, 19, 687–701. [Google Scholar] [CrossRef]
- Wei, R.; De Jesus, O. Tapia syndrome. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Lewis, S.R.; Butler, A.R.; Parker, J.; Cook, T.M.; Schofield-Robinson, O.J.; Smith, A.F. Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation: A Cochrane Systematic Review. BJA Br. J. Anaesth. 2017, 119, 369–383. [Google Scholar] [CrossRef]
- Benumof, J. Airway Management: Principles and Practice; Mosby: Philadelphia, PA, USA, 1996. [Google Scholar]
- Wu, L.; Shen, L.; Zhang, Y.; Zhang, X.; Huang, Y. Association between the use of a stylet in endotracheal intubation and postoperative arytenoid dislocation: A case-control study. BMC Anesthesiol. 2018, 18, 59. [Google Scholar] [CrossRef]
- Lykoudis, E.G.; Seretis, K. Tapia’s syndrome: An unexpected but real complication of rhinoplasty: Case report and literature review. Aesthetic Plast. Surg. 2012, 36, 557–559. [Google Scholar] [CrossRef]
- Seo, J.-H.; Kwon, T.-K.; Jeon, Y.; Hong, D.; Kim, H.; Bahk, J.-H. Comparison of techniques for double-lumen endobronchial intubation: 90 or 180 rotation during advancement through the glottis. Br. J. Anaesth. 2013, 111, 812–817. [Google Scholar] [CrossRef]
- Risse, J.; Schubert, A.-K.; Wiesmann, T.; Huelshoff, A.; Stay, D.; Zentgraf, M.; Kirschbaum, A.; Wulf, H.; Feldmann, C.; Meggiolaro, K.M. Videolaryngoscopy versus direct laryngoscopy for double-lumen endotracheal tube intubation in thoracic surgery—A randomised controlled clinical trial. BMC Anesthesiol. 2020, 20, 150. [Google Scholar] [CrossRef]
- Kim, Y.C.; Lee, S.H.; Noh, G.J.; Cho, S.Y.; Yeom, J.H.; Shin, W.J.; Lee, D.H.; Ryu, J.S.; Park, Y.S.; Cha, K.J.; et al. Thermosoftening Treatment of the Nasotracheal Tube Before Intubation Can Reduce Epistaxis and Nasal Damage. Anesth. Analg. 2000, 91, 698–701. [Google Scholar] [CrossRef]
- Kumar, R.; Mathur, A.; Kumar, S.; Gupta, N.; Kumar, N.G.; Gupta, E. Blind nasal intubation in a ‘breathing’ manikin—An idea. J. Anaesthesiol. Clin. Pharmacol. 2022, 38, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Borenstein, M.; Hedges, L.V.; Higgins, J.P.; Rothstein, H.R. Introduction to Meta-Analysis; John Wiley & Sons: Hoboken, NJ, USA, 2021. [Google Scholar]
- Tsukamoto, M.; Taura, S.; Kadowaki, S.; Hitosugi, T.; Miki, Y.; Yokoyama, T. Risk Factors for Postoperative Sore Throat After Nasotracheal Intubation. Anesth. Prog. 2022, 69, 3–8. [Google Scholar] [CrossRef]

| Outcomes | Number of Participants (Studies) | Certainty of the Evidence (GRADE) | Relative Effect (95% CI) | Anticipated Absolute Effects | |
|---|---|---|---|---|---|
| Risk with Room-Temperature ETT | Risk Difference with Thermal-Softened ETT | ||||
| Postoperative sore throat | 969 (5 RCTs) | ⬤⬤⬤⬤ High | RR 0.60 (0.44–0.82) | 381 per 1000 | 152 fewer per 1000 (27 to 84 fewer) |
| Postoperative hoarseness | 632 (4 RCTs) | ⬤⬤⬤◯ Moderate a | RR 0.86 (0.64–1.17) | 271 per 1000 | 38 fewer per 1000 (97 fewer to 46 more) |
| Vocal cord lesions | 518 (3 RCTs) | ⬤⬤⬤⬤ High | RR 0.52 (0.40–0.68) | 432 per 1000 | 208 fewer per 1000 (138 to 259 fewer) |
| Time to intubation | 843 (4 RCTs) | ⬤⬤◯◯ Low b | MD −6.51 s (−20.04 to 7.02) | — | MD 6.51 s shorter |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hee, H.-Z.; Chiu, C.-H.; Lu, C.-W. The Effect of Thermal-Softened Endotracheal Tubes on Postoperative Sore Throat and Other Complications—A Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 3620. https://doi.org/10.3390/jcm14113620
Hee H-Z, Chiu C-H, Lu C-W. The Effect of Thermal-Softened Endotracheal Tubes on Postoperative Sore Throat and Other Complications—A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2025; 14(11):3620. https://doi.org/10.3390/jcm14113620
Chicago/Turabian StyleHee, Hui-Zen, Chen-Hsi Chiu, and Cheng-Wei Lu. 2025. "The Effect of Thermal-Softened Endotracheal Tubes on Postoperative Sore Throat and Other Complications—A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 14, no. 11: 3620. https://doi.org/10.3390/jcm14113620
APA StyleHee, H.-Z., Chiu, C.-H., & Lu, C.-W. (2025). The Effect of Thermal-Softened Endotracheal Tubes on Postoperative Sore Throat and Other Complications—A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 14(11), 3620. https://doi.org/10.3390/jcm14113620