4.1. Literature Findings
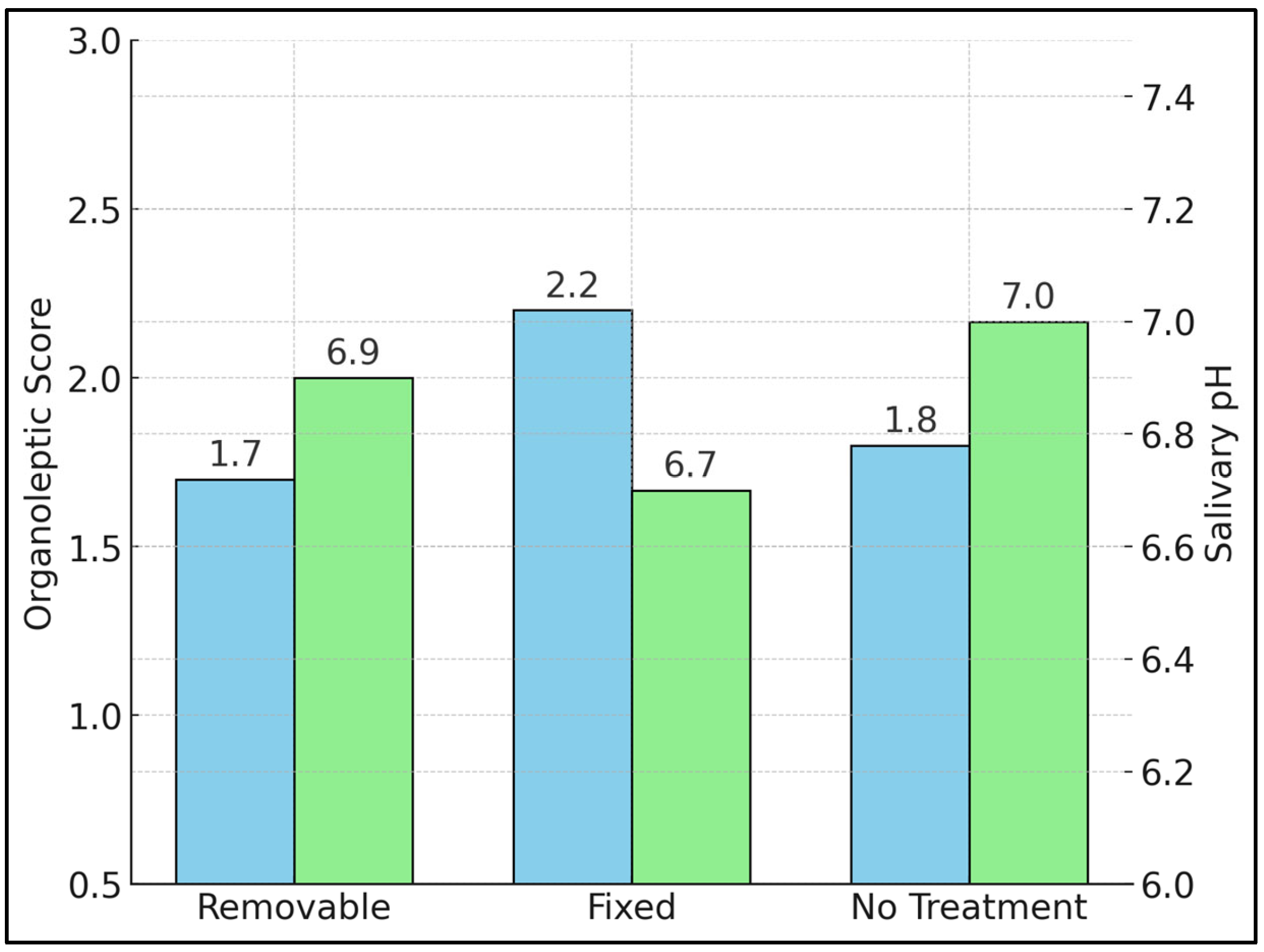
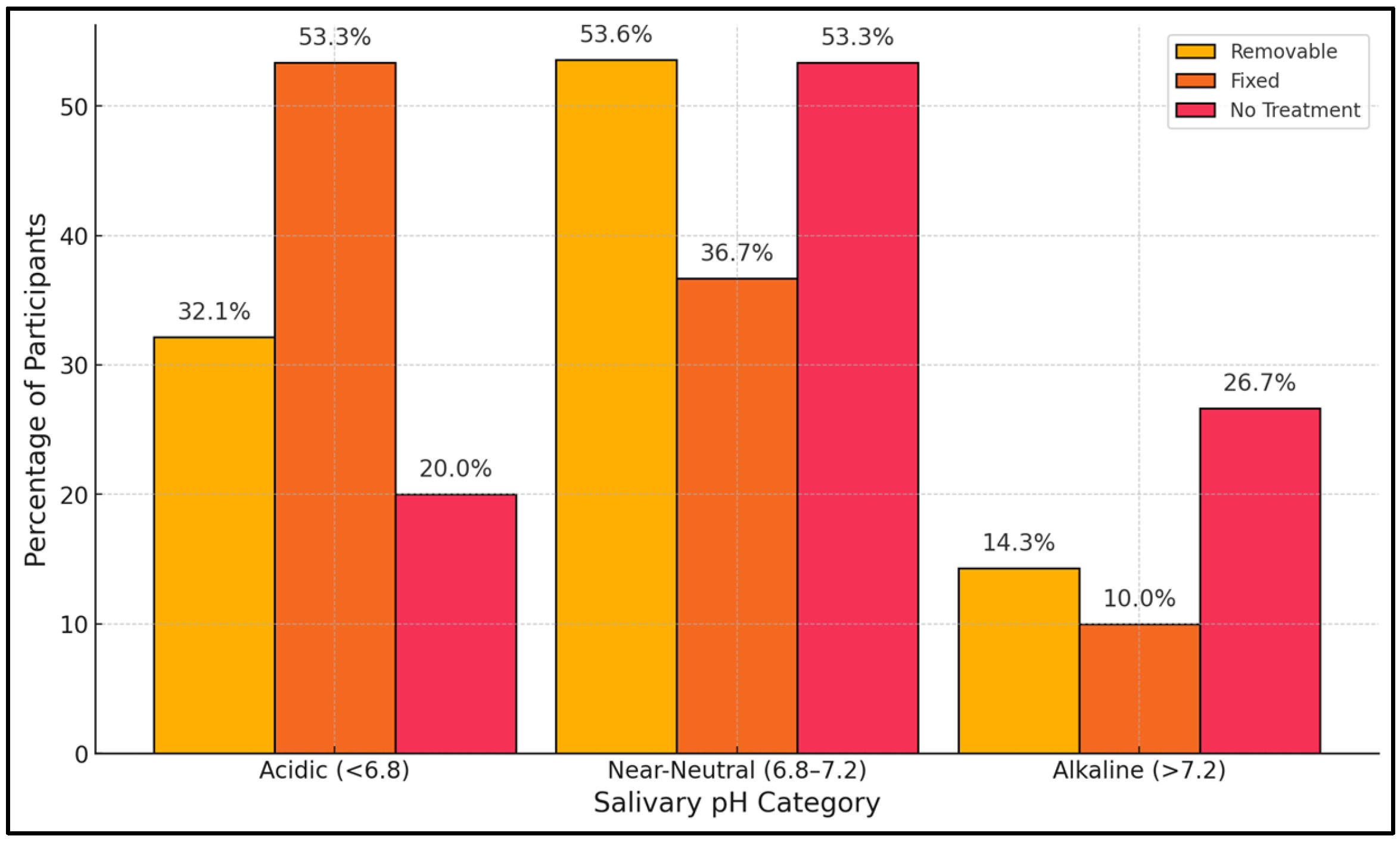
This cross-sectional study explored the interplay among orthodontic retainer type, salivary pH, and halitosis in adolescents and young adults. Our findings indicate that fixed retainers correlate with a higher prevalence of acidic saliva and more severe malodor, both clinically (organoleptic scores) and subjectively (HALT). In contrast, removable retainer wearers demonstrated somewhat milder levels of halitosis, possibly due to the device’s lower plaque-retentive potential and the ease of removing it for cleaning. Participants without orthodontic appliances tended to show near-neutral or slightly alkaline salivary pH, aligning with relatively lower halitosis indicators.
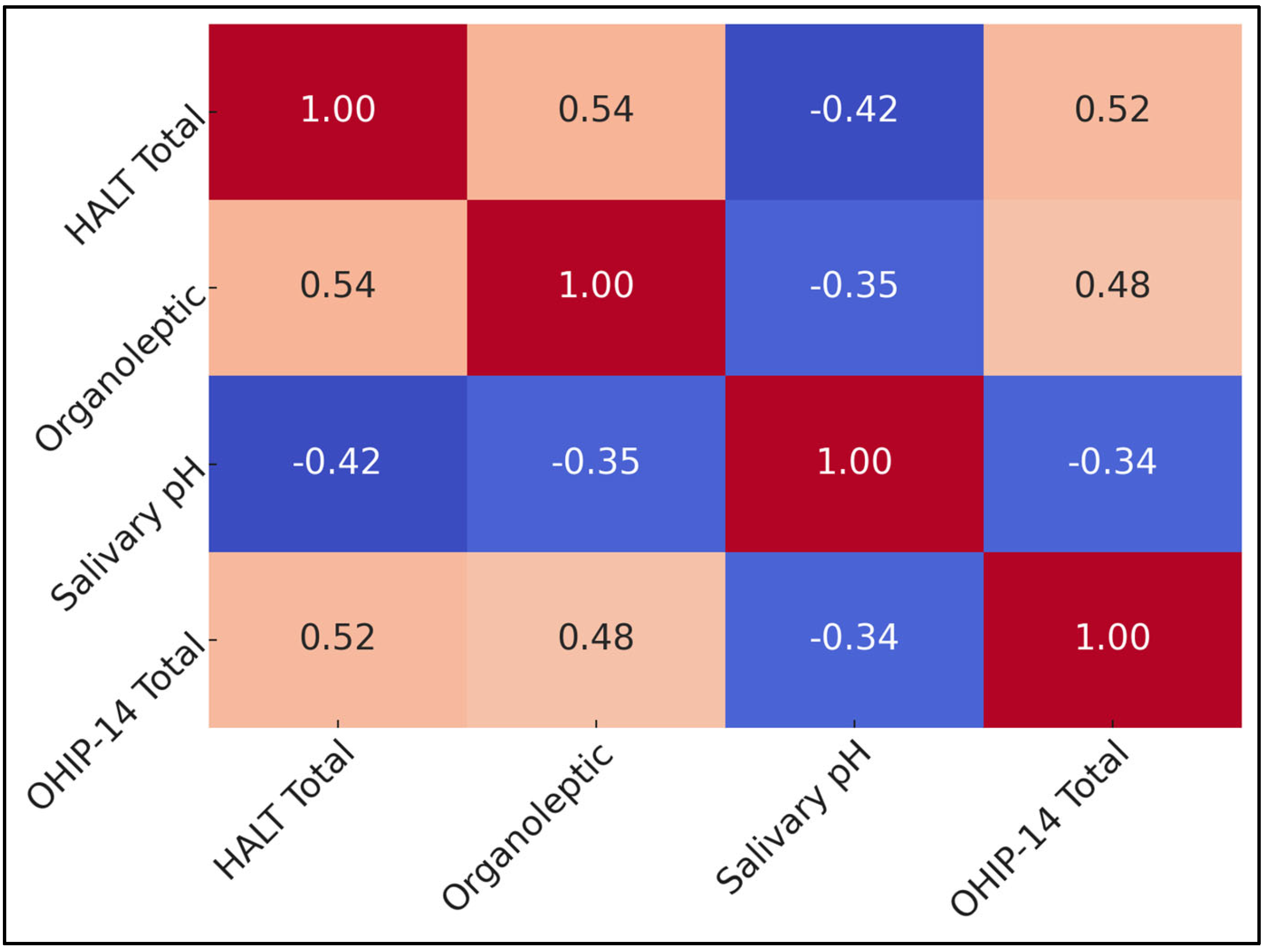
Salivary pH emerged as a critical modifier, with acidic conditions linked to elevated HALT and organoleptic scores across all groups. This relationship underscores how oral chemistry can shape bacterial ecology, enabling odor-causing microbes to thrive. Our correlation analysis showed that halitosis severity aligns with psychological distress, as measured by HALT and OHIP-14. These data affirm that beyond a mere biological phenomenon, malodor can substantially erode young individuals’ social confidence and emotional well-being, especially in an age group prone to heightened self-consciousness.
Taken together, the evidence suggests an integrated approach to halitosis management among adolescent and young adult retainer wearers. Oral health professionals should emphasize salivary pH assessment, regular retainer cleaning, and periodic professional follow-up to detect early signs of malodor. Removable retainers appear to pose fewer halitosis risks, but consistent hygiene remains essential. Interventions that aim to maintain or restore neutral pH, e.g., dietary modifications, saliva stimulants, and improved brushing protocols, might mitigate both the clinical and psychosocial burdens of malodor. Prospective, longitudinal research could further elucidate how retainer duration, evolving dentition, and ongoing maturity influence these outcomes over time.
In a similar manner to the study by Settineri et al. [
21], which found significant associations between self-reported halitosis and various factors, such as relational dental anxiety, alcohol consumption, and poor oral hygiene, among others, in an Italian cohort (ORs ranging from 0.39 to 1.04), the research by Elif Yıldızer Keriş and colleagues also explored the impact of orthodontic appliances on halitosis [
22]. However, unlike Settineri et al.’s findings that linked behavioral and psychological factors with halitosis, Keriş’s study, conducted on a younger demographic using fixed and removable space maintainers, concluded that these appliances did not significantly alter oral health status or halitosis over time, with all
p-values exceeding 0.05 [
21,
22]. This suggests that while adult halitosis can be influenced by psychological and hygiene-related factors, in children, the type of orthodontic appliance might not have a measurable impact on halitosis, indicating a possible age-related difference in the factors contributing to halitosis. Both studies underline the complexity of halitosis, which is influenced by a variety of biological, psychological, and care-related factors that manifest differently across age groups.
In the study by Arwa A Banjar et al. [
7], 41.5% of young adults undergoing orthodontic treatment reported experiencing halitosis, with a significant 62.5% noticing the issue during or after their treatment. Furthermore, a statistically significant correlation was identified, highlighting that regular dental visits were associated with a reduction in halitosis among those with fixed orthodontic appliances. In contrast, the systematic review by Raluca Briceag et al. [
23] compiled results from various studies, revealing that the prevalence of self-reported halitosis among adolescents and young adults ranged significantly, from 23.1% to 77.5%, with an average of 44.7%. This review also noted psychological effects, as those affected reported increased feelings of anxiety and depression, measured using tools like the OHIP-14 and SCL-9-R. These findings emphasize the pervasive impact of halitosis not just on physical dental health but also on the emotional and social well-being of individuals, highlighting the necessity of comprehensive care strategies that include both dental treatment and psychological support to manage halitosis effectively.
In examining the interplay between orthodontic appliances and oral health, Lucchese et al. [
24] conducted a systematic review that revealed that the use of orthodontic appliances significantly altered the oral microbiota, with a notable increase in cariogenic and periodontopathogenic bacteria, such as Streptococcus mutans, Lactobacillus spp., and various Gram-negative species, like Porphyromonas gingivalis and Fusobacterium nucleatum, suggesting a heightened risk for caries and periodontal disease during orthodontic treatment. In a similar manner, the longitudinal prospective study by Gámez Medina et al. [
25] assessed the effects of fixed retainers on oral-health-related quality of life (OHRQoL) and found that upper retainers negatively impacted OHRQoL at baseline (
p = 0.018), with overall OHIP-14 scores worsening over time (T0 to T1,
p = 0.014). Notably, fractures or debonding of retainers were significantly associated with poorer patient-reported outcomes (
p = 0.05). While Lucchese et al. focused on the microbiological implications of appliance use, Gámez Medina et al. provided patient-centered evidence indicating that mechanical complications may have long-term psychosocial consequences. Together, these studies underscore the importance of comprehensive clinical management during the retention phase, not only for microbial control but also to preserve patients’ quality of life.
Our findings accord with Kanzow et al. [
26], who demonstrated that even transient pH reductions (<6.8) intensified VSC release after 4 h of mask wearing in young adults. Likewise, Muniz et al. [
27] reported a 51% prevalence of self-reported malodor in institutionalized adolescents, driven by cariogenic burden and psychosocial stressors. These population data reinforce our correlation between HALT, OHIP-14, and organoleptic scores.
Short-term interventional work also suggests that restoring pH toward neutrality ameliorates odor. A randomized crossover trial using lemon essential oil mouthrinses raised salivary pH by ≈ 0.3 units and suppressed VSCs for 60 min [
28]. The present study extends those physiological observations by linking chronic acidic profiles to quality of life decrements in retainer wearers.
Stress-related cortisol and heightened gingival inflammation reshape the plaque proteome, enriching Fusobacterium, Prevotella, and Gram-negative anaerobes that liberate hydrogen–sulphide and methyl–mercaptan. This ecological drift, documented in longitudinal adolescent cohorts with fixed appliances, offers a plausible biological bridge between our salivary pH signal and clinical malodor. Finally, our 24 h mouth-wash wash-out aligns with pharmacodynamic data showing that CHX/CPC substantivity falls below bactericidal thresholds within 12–16 h, making a one-week exclusion unnecessary while preserving ecological validity.