Physiotherapy for Sexual Dysfunctions in Multiple Sclerosis Patients: A Review of Clinical Trials
Abstract
1. Introduction
1.1. Nature of Multiple Sclerosis
1.2. Epidemiology of Multiple Sclerosis
1.3. Types of Sexual Dysfunctions
- Primary—resulting from direct damage to the nervous system, which impairs a specific phase of the sexual response to stimulation (sensory disturbances, lubrication issues, erectile dysfunction, pain, orgasm disorders).
- Secondary—a consequence of disease symptoms, which indirectly impair or prevent the fulfillment of sexual functions (fatigue, spasticity, sphincter dysfunction, coordination problems, side effects of treatment).
- Tertiary—emotional, mood, and cognitive function disorders. These are responses to progressive disability, changes in body image, and social roles (low self-esteem, mood disturbances, feelings of guilt, changes in roles performed).
2. Pathogenetic Mechanisms and Prevalence of Sexual Dysfunction in Multiple Sclerosis Patients
3. Physiotherapy in Multiple Sclerosis-Related Sexual Dysfunction
4. Aim of Review
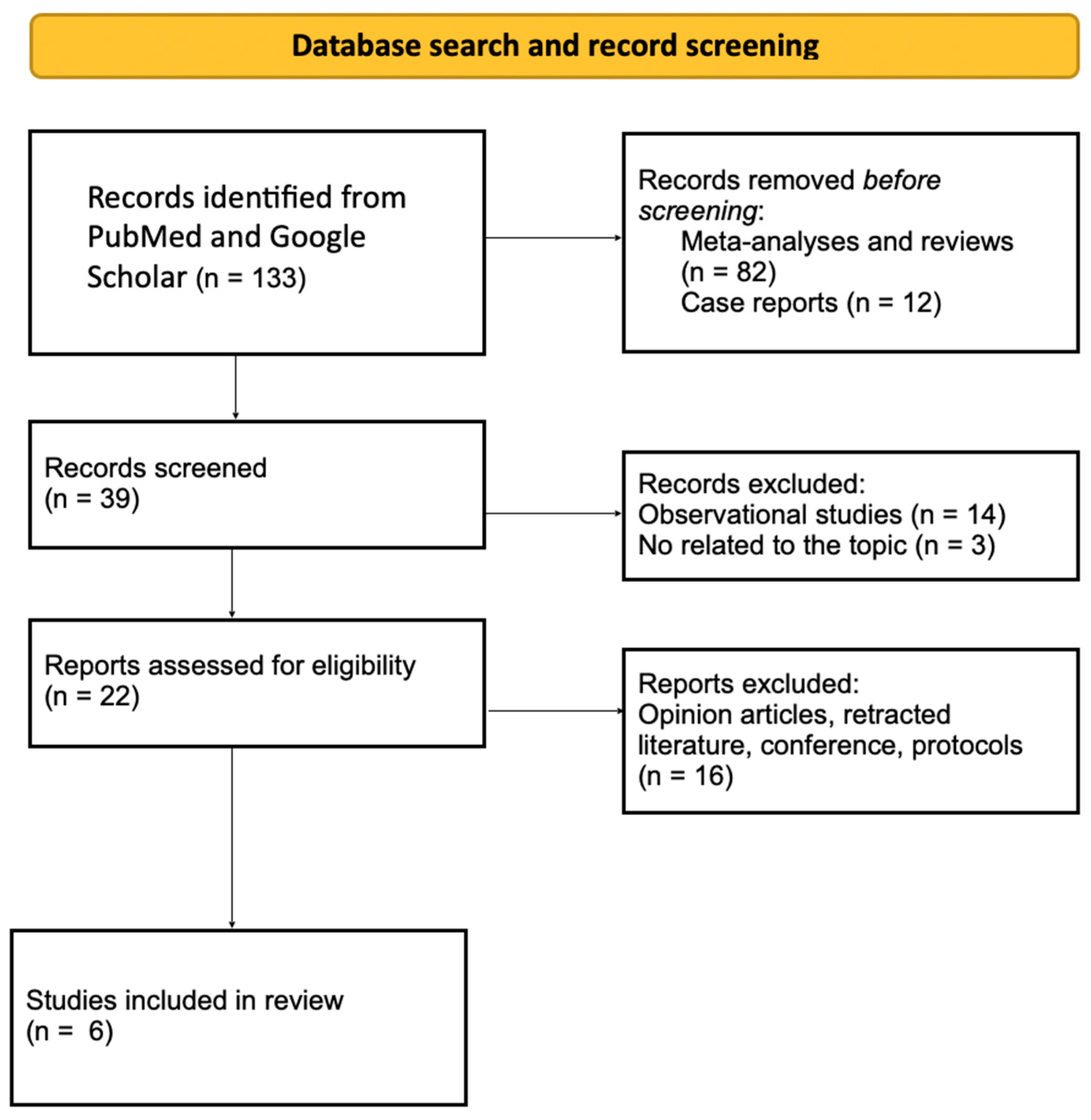
5. Methods
6. Results
6.1. Pelvic Floor Muscle Training
6.2. Tibial Nerve Stimulation
6.3. Clitoral Vacuum Suction/Vibratory Stimulation
6.4. Telerehabilitation
7. Discussion
- expanding research on the effectiveness of specific physiotherapeutic methods in the context of sexual dysfunction in MS patients, with larger study populations and longer follow-up periods;
- determining the optimal parameters of therapy (frequency, intensity, duration) that yield the best outcomes in improving sexual function and patients’ quality of life;
- investigating the effectiveness of a personalized therapeutic approach that includes interdisciplinary collaboration—particularly involving pelvic floor physiotherapists—as part of comprehensive patient care.
8. Conclusions
Funding
Conflicts of Interest
References
- Jankowska, A.; Chwojnicki, K.; Szurowska, E. The diagnosis of multiple sclerosis: What has changed in diagnostic criteria? Pol. J. Radiol. 2023, 88, e574–e581. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Al Worikat, N.; Zanotto, A.; Sosnoff, J.J.; Zanotto, T. Nida Mental health and frailty in people with multiple sclerosis: Unraveling a complex relationship. Front. Psychol. 2024, 15, 1387618. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dobson, R.; Giovannoni, G. Multiple sclerosis—A review. Eur. J. Neurol. 2018, 26, 27–40. [Google Scholar] [CrossRef] [PubMed]
- Haki, M.; Al-Biati, H.A.; Al-Tameemi, Z.S.; Ali, I.S.; Al-Hussaniy, H.A. Review of multiple sclerosis: Epidemiology, etiology, pathophysiology, and treatment. Medicine 2024, 103, e37297. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Balasooriya, N.N.; Elliott, T.M.; Neale, R.E.; Vasquez, P.; Comans, T.; Gordon, L.G. The association between vitamin D deficiency and multiple sclerosis: An updated systematic review and meta-analysis. Mult. Scler. Relat. Disord. 2024, 90, 105804. [Google Scholar] [CrossRef] [PubMed]
- Lorenzut, S.; Del Negro, I.; Pauletto, G.; Verriello, L.; Spadea, L.; Salati, C.; Musa, M.; Gagliano, C.; Zeppieri, M. Exploring the Pathophysiology, Diagnosis, and Treatment Options of Multiple Sclerosis. J. Integr. Neurosci. 2025, 24, 25081. [Google Scholar] [CrossRef] [PubMed]
- Nappi, R.E.; Cucinella, L.; Martella, S.; Rossi, M.; Tiranini, L.; Martini, E. Female sexual dysfunction (FSD): Prevalence and impact on quality of life (QoL). Maturitas 2016, 94, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Facio, F.; Colonnello, E.; Alzweri, L.; Citrin, E.; Dubinskaya, A.; Falsetta, M.; Fregonesi, A.; Kellogg-Spadt, S.; Lopes, L.S.; Jannini, E.A. Infection, inflammation, and sexual function in male and female patients-recommendations from the Fifth International Consultation on Sexual Medicine (ICSM 2024). Sex. Med. Rev. 2025, qeaf021. [Google Scholar] [CrossRef] [PubMed]
- Bartnik, P.; Wielgoś, A.; Kacperczyk, J.; Pisarz, K.; Szymusik, I.; Podlecka-Piętowska, A.; Zakrzewska-Pniewska, B.; Wielgoś, M. Sexual dysfunction in female patients with relapsing-remitting multiple sclerosis. Brain Behav. 2017, 7, e00699. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Manouchehri, E.; Saeedi, M.; Najmabadi, K.M. Evaluation of sexual self-efficacy and sexual function in women with multiple sclerosis in Mashhad, Iran, in 2019: A cross-sectional study. Curr. J. Neurol. 2021, 20, 23–31. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nazari, F.; Shaygannejad, V.; Sichani, M.M.; Mansourian, M.; Hajhashemi, V. Sexual dysfunction in women with multiple sclerosis: Prevalence and impact on quality of life. BMC Urol. 2020, 20, 15. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dobrakowski, P.; Machowska-Majchrzak, A.; Labuz-Roszak, B.; Niewiadomska, E.; Pierzchala, K. Sexual Satisfaction in Fully Ambulatory People with Multiple Sclerosis: Does Disability Matter? Behav. Neurol. 2020, 2020, 8857516. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dastoorpoor, M.; Zamanian, M.; Moradzadeh, R.; Nabavi, S.M.; Kousari, R. Prevalence of sexual dysfunction in men with multiple sclerosis: A systematic review and meta-analysis. Syst. Rev. 2021, 10, 10. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yeni, K.; Tulek, Z.; Terzi, M. Sexual dysfunction in female patients with multiple sclerosis: Relationship with functional status, fatigue, depression, sleep quality, and quality of life. J. Sex. Med. 2025, qdaf015. [Google Scholar] [CrossRef] [PubMed]
- Bronner, G.; Elran, E.; Golomb, J.; Korczyn, A.D. Female sexuality in multiple sclerosis: The multidimensional nature of the problem and the intervention. Acta Neurol. Scand. 2010, 121, 289–301. [Google Scholar] [CrossRef] [PubMed]
- Lew-Starowicz, M.; Rola, R. Prevalence of Sexual Dysfunctions Among Women with Multiple Sclerosis. Sex. Disabil. 2013, 31, 141–153. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gava, G.; Visconti, M.; Salvi, F.; Bartolomei, I.; Seracchioli, R.; Meriggiola, M.C. Prevalence and Psychopathological Determinants of Sexual Dysfunction and Related Distress in Women with and Without Multiple Sclerosis. J. Sex. Med. 2019, 16, 833–842. [Google Scholar] [CrossRef] [PubMed]
- Grech, L.B.; Allan, M.; de Courten, B. Sexual dysfunction in men with multiple sclerosis. Syst. Rev. 2021, 10, 86. [Google Scholar] [CrossRef]
- Podnar, S.; Vodušek, D.B. Place of perineal electrophysiologic testing in multiple sclerosis patients. Ann. Phys. Rehabil. Med. 2014, 57, 288–296. [Google Scholar] [CrossRef] [PubMed]
- Sparaco, M.; Bonavita, S. Pelvic Floor Dysfunctions and Their Rehabilitation in Multiple Sclerosis. J. Clin. Med. 2022, 11, 1941. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Blanco-Ratto, L.; Ramírez-García, I.; Kauffmann, S.; Farrés, M.G. Effectiveness of physiotherapy and its impact on the quality of life of patients compared to other therapeutic approaches in the management of female sexual dysfunction in non-menopausal adult population: A systematic review. Sex. Med. Rev. 2025, qeaf022. [Google Scholar] [CrossRef] [PubMed]
- Trudel, G.; Saint-Laurent, S. A comparison between the effects of Kegel’s exercises and a combination of sexual awareness relaxation and breathing on situational orgasmic dysfunction in women. J. Sex Marital. Ther. 1983, 9, 204–209. [Google Scholar] [CrossRef] [PubMed]
- Aalaie, B.; Tavana, B.; Rezasoltani, Z.; Aalaei, S.; Ghaderi, J.; Dadarkhah, A. Biofeedback versus electrical stimulation for sexual dysfunction: A randomized clinical trial. Int. Urogynecol. J. 2021, 32, 1195–1203. [Google Scholar] [CrossRef] [PubMed]
- Cyr, M.P.; Jones, T.; Brennen, R.; Colombage, U.; Frawley, H.C. Effectiveness of Pelvic Floor Muscle and Education-Based Therapies on Bladder, Bowel, Vaginal, Sexual, Psychological Function, Quality of Life, and Pelvic Floor Muscle Function in Females Treated for Gynecological Cancer: A Systematic Review. Curr. Oncol. Rep. 2024, 26, 1293–1320. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mosalanejad, F.; Afrasiabifar, A.; Zoladl, M. Investigating the combined effect of pelvic floor muscle exercise and mindfulness on sexual function in women with multiple sclerosis: A randomized controlled trial. Clin. Rehabil. 2018, 32, 1340–1347. [Google Scholar] [CrossRef] [PubMed]
- Lúcio, A.; D’ancona, C.; Lopes, M.; Perissinotto, M.; Damasceno, B. The effect of pelvic floor muscle training alone or in combination with electrostimulation in the treatment of sexual dysfunction in women with multiple sclerosis. Mult. Scler. J. 2014, 20, 1761–1768. [Google Scholar] [CrossRef] [PubMed]
- Dunya, C.P.; Tülek, Z.; Kürtüncü, M.; Gündüz, T.; Panicker, J.N.; Eraksoy, M. Evaluating the effects of transcutaneous tibial nerve stimulation or pelvic floor muscle training on sexual dysfunction in female multiple sclerosis patients reporting overactive bladder. Neurourol. Urodyn. 2021, 40, 1661–1669. [Google Scholar] [CrossRef] [PubMed]
- Giannopapas, V.; Smyrni, V.; Kitsos, D.K.; Chasiotis, A.K.; Stavrogianni, K.; Papagiannopoulou, G.; Tsivgoulis, G.; Voumvourakis, K.; Giannopoulos, S.; Bakalidou, D. Tibial nerve stimulation in the management of primary sexual dysfunction in patients with multiple sclerosis: A pilot randomized control trial. Neurol. Sci. 2024, 45, 5849–5858. [Google Scholar] [CrossRef] [PubMed]
- Alexander, M.; Bashir, K.; Alexander, C.; Marson, L.; Rosen, R. Randomized Trial of Clitoral Vacuum Suction Versus Vibratory Stimulation in Neurogenic Female Orgasmic Dysfunction. Arch. Phys. Med. Rehabil. 2018, 99, 299–305. [Google Scholar] [CrossRef] [PubMed]
- Deodato, M.; Fornasaro, M.; Martini, M.; Zelesnich, F.; Sartori, A.; Galmonte, A.; Stella, A.B.; Manganotti, P. Comparison of different telerehabilitation protocols for urogenital symptoms in females with multiple sclerosis: A randomized controlled trial. Neurol. Sci. 2024, 45, 5501–5509. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
| No. | Name | Sex It Concerns | Meaning |
|---|---|---|---|
| 1. | Sexual desire disorders | Male and Female | Decreased interest or lack of interest in sex; lack of sexual initiative and desire for sexual stimulation [7,8]. |
| 2. | Sexual arousal disorders | Female | Difficulties in achieving or maintaining an adequate level of sexual arousal, such as problems with vaginal lubrication [7]. |
| 3. | Orgasm disorders | Male and Female | Difficulties in achieving orgasm despite appropriate arousal; delayed or absent orgasm; in man often related to delayed ejaculation [7,8]. |
| 4. | Dyspareunia | Male and Female | Pain during penetration (female); pain in the genital area during sexual activity (male) [7,8]. |
| 5. | Vaginismus | Female | Tension and muscle spasm of the vagina that prevent penetration [7]. |
| 6. | Erectile dysfunctions | Male | Difficulties in achieving or maintaining an erection sufficient for penetration [8]. |
| 7. | Psychological and emotional disorders | Male and Female | Anxiety, stress, depression, and mood disorders that can affect sexual response [7,8]. |
| 8. | Medication-induced sexual dysfunction | Male and Female | Medications such as antidepressants, antihypertensive drugs, or painkillers can cause changes in sexual functioning [7,8]. |
| 9. | Disorders resulting from interpersonal issues | Male and Female | Relationship problems, difficulties in communication with a partner, sexual misunderstanding [7,8]. |
| No. | Name | Explanation |
|---|---|---|
| 1. | Individual and group pelvic floor muscle training [21] | Regular exercises can improve control over sphincters and influence blood circulation in the pelvis, which can positively affect sensations during intercourse. |
| 2. | Manual therapy [21] | Restoring proper muscle tension in the pelvic region can improve comfort during sexual activity and help reduce discomfort caused by spasticity. |
| 3. | Thermal therapy (heat and cold) [21] | Thermal stimulus can help reduce muscle tension and improve blood circulation, which can positively influence sexual function especially in cases involving pain. |
| 4. | Breathing exercises [22] | Breathing techniques are used to improve overall well-being, reduce stress, and enhance the sensation of sexual pleasure. |
| 5. | Electrostimulation [23] | Involves using electrical impulses to simulate the pelvic muscles. It is applied in the treatment of erectile dysfunction in men, as well as in the treatment of urinary incontinence and enhancement of sexual sensations in women. |
| 6. | Biofeedback [23] | Specifically tailored pelvic floor muscle training combined with visual stimulation influences sensory perception of the deep muscle layers in the pelvis, thereby improve sexual sensations. |
| 7. | Behavioral therapy [24] | May include discussions about intimacy and relationships, as well as relaxation techniques combined with physical exercises. |
| No. | First Author | Year of Publication | Sample Size | Control Group | Intervention Effect |
|---|---|---|---|---|---|
| 1. | Mosalanejad Fatemeh [25] | 2018 | 60 women with MS and sexual dysfunction. | 30 women without PF exercises. | The combination of pelvic floor muscle exercises and mindfulness techniques had a positive impact on the participants’ sexual function, increasing sexual satisfaction and reducing sexual dysfunction. |
| 2. | Lúcio AC [26] | 2014 | 45 women with MS and sexual dysfunction. | Groups of 15 women were assigned to: pelvic floor muscle exercises; electrostimulation; or a combination of both methods. | Both forms of intervention were effective in improving sexual function, with greater benefits observed in the group combining electrostimulation. |
| 3. | Giannopapas Vasileios [27] | 2024 | 40 patients with MS. | 20 patients without tibial nerve stimulation. | Tibial nerve stimulation proved to have a positive impact on sexual dysfunction. |
| 4. | Polat Dunya Cansu [28] | 2021 | 75 women with MS, overactive bladder and sexual dysfunction. | Groups of 25 women were assigned to: pelvic floor training; tibial nerve stimulation; or without any therapy. | Both methods improved sexual function. |
| 5. | Alexander Marcalee [29] | 2018 | 90 women with neurogenic orgasmic dysfunction. | Groups of 30 women were assigned to: vacuum suction; vibratory stimulation; or no stimulation (placebo). | Both interventions were effective in treating orgasmic dysfunction, with comparable results in both groups. |
| 6. | Deodato Manuela [30] | 2024 | 120 women with MS and urogenital symptoms. | Groups of 40 women were assigned to: rehabilitation through videoconferencing; self-exercises with a mobile app; or standard in-person rehabilitation. | Telerehabilitation may be an effective method for treating urogenital symptoms in women with MS. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reimus, M.; Siemiński, M. Physiotherapy for Sexual Dysfunctions in Multiple Sclerosis Patients: A Review of Clinical Trials. J. Clin. Med. 2025, 14, 3509. https://doi.org/10.3390/jcm14103509
Reimus M, Siemiński M. Physiotherapy for Sexual Dysfunctions in Multiple Sclerosis Patients: A Review of Clinical Trials. Journal of Clinical Medicine. 2025; 14(10):3509. https://doi.org/10.3390/jcm14103509
Chicago/Turabian StyleReimus, Michalina, and Mariusz Siemiński. 2025. "Physiotherapy for Sexual Dysfunctions in Multiple Sclerosis Patients: A Review of Clinical Trials" Journal of Clinical Medicine 14, no. 10: 3509. https://doi.org/10.3390/jcm14103509
APA StyleReimus, M., & Siemiński, M. (2025). Physiotherapy for Sexual Dysfunctions in Multiple Sclerosis Patients: A Review of Clinical Trials. Journal of Clinical Medicine, 14(10), 3509. https://doi.org/10.3390/jcm14103509






