4. Discussion
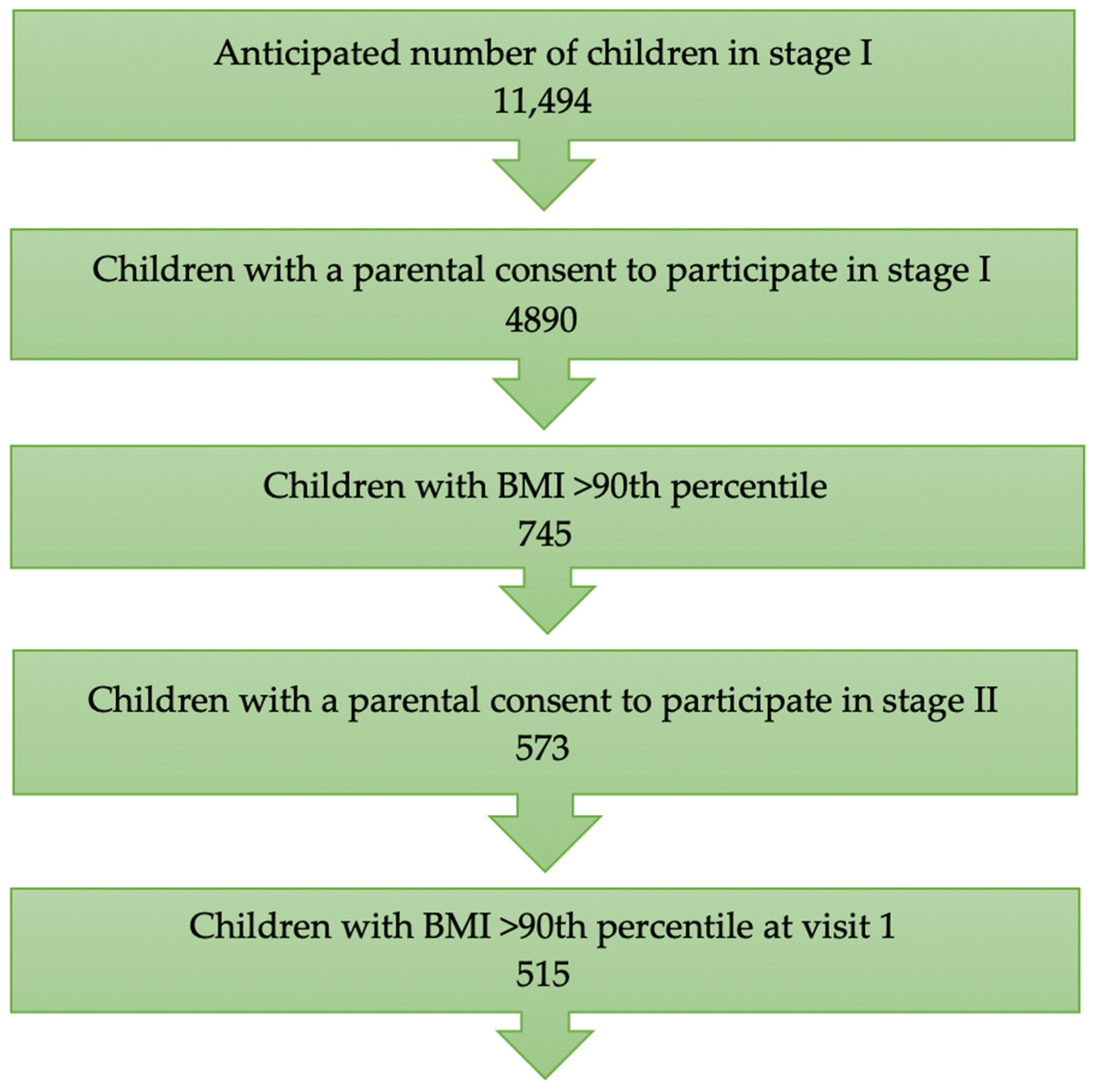
Although our team visited each school to inform parents about the program and its benefits, relatively few parents were interested in participating. A total of 4890 parents consented to their children participating in the program, which represented about 42% of the guardians. Programs focused on preventing and treating childhood overweight and obesity often face low to moderate parental engagement. Studies indicate that parents initiate participation in weight management programs out of concern for their children’s psychological well-being and health. However, despite their initial commitment, many parents withdraw from the program during the early stages [
24]. A low rate of parental consent for participation in this study may result from insufficient awareness of the seriousness of childhood overweight and its broad health and social consequences. Some caregivers who believe their children have a normal body weight do not see the need to verify their assessment using objective methods and, therefore, will not be interested in participating even in the first stage of the program. Fear or shame related to judgment and potential stigmatization of the child by other parents and peers is also a significant factor.
In the screening phase of our study, we diagnosed excess body weight in 23% of the children, including 16.9% who were overweight and 6.4% who were obese. Similar results were obtained in national population studies. In the OLAF study conducted between 2007 and 2012, excess body weight was diagnosed in 21.4% of 8-year-old boys and 17.9% of girls [
25]. In the COSI study conducted in 2015–2016, overweight was diagnosed in 23.2% of children aged 6–9 years (using IOTF criteria), with rates of 22.6% in boys and 23.7% in girls [
26]. Children who had reduced their BMI to values within the normal range by the time of the first visit in the second stage of the program were excluded from the intervention phase. This improvement was observed in 58 children, who achieved a normal BMI by the time of the first visit. This was one of the desired effects of our program. Conducting measurements at school and informing guardians about their child’s excess body weight, combined with simple recommendations for a healthy diet and increased physical activity, resulted in 10% of the children achieving a normal BMI by the time of their specialist visit (about 3–4 weeks).
Children who achieved the desired effect of a normal BMI (<90th percentile for age and sex) during the year-long program completed their participation in the project. Some children reached a normal BMI by the second or third visit. All children who achieved a normal BMI (the program’s best outcome) were not included in the final analysis of the results which took place after the fourth visit, which marked the end of the program. It is worth considering continued monitoring of this group of children in the future to assess the stability of the achieved outcomes.
The decreasing number of children participating in the program at each stage was due either to children achieving a normal BMI or, more commonly, due to them dropping out. Previous studies have shown varying dropout rates in childhood obesity treatment programs. Reviews of meta-analyses report dropout rates ranging from 25 to 50% or from 3 to 48% [
27,
28].
Although more children diagnosed in the screening phase had overweight rather than obesity, most of the children who participated in the intervention phase were classified as obese (76%). This may be because parents of children with obesity are more likely to perceive the problem as significant and thus decide to participate in the intervention program. However, according to a meta-analysis by Kelleher, their child’s BMI alone does not necessarily influence parents’ willingness to participate in an intervention program [
24]. It is also worth considering whether organizing the visits during the second phase of this study in a university hospital was an encouraging factor or, conversely, a deterrent to program participation. On one hand, such a facility emphasizes the seriousness of the problem and its health consequences; on the other hand, it may discourage some caregivers and children who perceive it as excessive medicalization. It also seems that implementing the intervention at an even earlier age [
29] and maintaining it over a longer period could more effectively help consolidate changes in eating habits and increase the daily physical activity of children who participate. In the future, it may be worth considering the inclusion in similar programs of not only children with overweight and obesity but also those at risk of developing overweight. However, attention should be paid to the challenges encountered in maintaining participation among children who reduced their BMI to below the 90th percentile at different stages. A large proportion of them dropped out of the program despite having the opportunity to continue. This indicates a low perceived threat, which may be related to poor health awareness concerning the complications of excessive body weight, including overweight. This highlights how much effort is still needed to promote this knowledge. A significant factor influencing continued participation in similar programs is often the lack of immediate results in terms of weight reduction. Despite discussions about expected outcomes and the pace of changes during the initial medical visits, this element is often decisive in the decision to discontinue participation. It is worth considering ways to increase the attractiveness of activities that promote physical activity and introduce healthy eating habits into everyday life. Given the organizational challenges faced daily by families with children, diversifying the available activities may help maintain engagement from both children and caregivers in the program.
During each visit, a desired reduction in both the mean BMI percentile and BMI z-score was achieved. The greatest reduction occurred between the first and second visits. Throughout the program, the number of children who experienced a decrease in their BMI percentile and z-score increased. Nearly 80% of the children showed a reduction in their BMI percentile and z-score during the year-long intervention. The initial mean BMI percentile was 97, and the z-score BMI was 1.9. After the year-long intervention, these values decreased to 95 and 1.7, respectively. In the meta-analysis by Ells, a slightly higher initial mean BMI z-score (2.25) was found in similar intervention programs for children with excess body weight, with a smaller average reduction in BMI z-score (0.05) [
30].
During each visit, the BMI percentile and z-score were higher in the boys than in the girls. Additionally, a higher percentage of boys were classified as obese compared to the girls at every visit. Notably, the decrease in the BMI percentile and z-score was greater in the girls than in the boys throughout the program, suggesting that the girls achieved better outcomes in reducing excess body weight in our program.
Previous randomized clinical trials have reported comparable percentages of children achieving a decrease in their BMI z-score during multidisciplinary interventions. In Reinehr’s study, a 12-month intervention resulted in a BMI z-score reduction in 72% of children [
31]. In another study by Reinehr, a reduction in BMI z-score was observed in 77% of children, and interestingly, the reduction was sustained in 66% of children three years later [
32]. In Mayerhofer’s study, a 5-month intervention resulted in a BMI z-score reduction in 79% of children, with similar effects observed in both boys and girls [
33].
A review of meta-analyses evaluating the impact of multidisciplinary interventions on children with excess body weight shows a reduction in BMI, but the results are not entirely consistent. In Hamid’s study, the effects of multidisciplinary interventions on children aged from 6 to 12 years with overweight and obesity were assessed. Four out of seven studies reported a significant reduction in the BMI z-score in the intervention group compared to the control group, while two studies found no significant differences between the groups [
34]. A meta-analysis of 21 studies evaluating changes in BMI and BMI z-score during interventions found moderate benefits in the study group compared to the control group across all studies [
35]. A meta-analysis of 14 studies comparing the effects of multidisciplinary interventions to a control group without intervention found improvements in BMI z-score, BMI, and body weight in the intervention group, both after the intervention and during follow-up several months later [
36]. Ells’ meta-analysis showed a positive effect of interventions on the BMI z-score of participants [
30]. Zolotarjova’s study, which evaluated the effects of multidisciplinary interventions on children aged 4–18 years with severe obesity, reported a reduction in the BMI and BMI z-score of participants in each study. However, despite the favourable impact on cardiovascular risk factors, weight loss was often not sustained. Younger children and boys showed better maintenance of weight loss [
37].
Differences in the results of meta-analyses may stem from the variety of interventions that are applied. Clinical studies vary significantly in terms of the interventions that are undertaken. Some studies involved isolated interventions, while others were multidisciplinary. The programs were conducted in different settings—at school, at home, in healthcare facilities, or a combination of these. The duration of interventions, frequency of visits, and intensity of physical activities also varied. Some studies merely provided guidance on recommended physical activity, while others included supervised exercise. The level of parental involvement in the intervention process also varied. This diversity in study designs makes it difficult to compare their results.
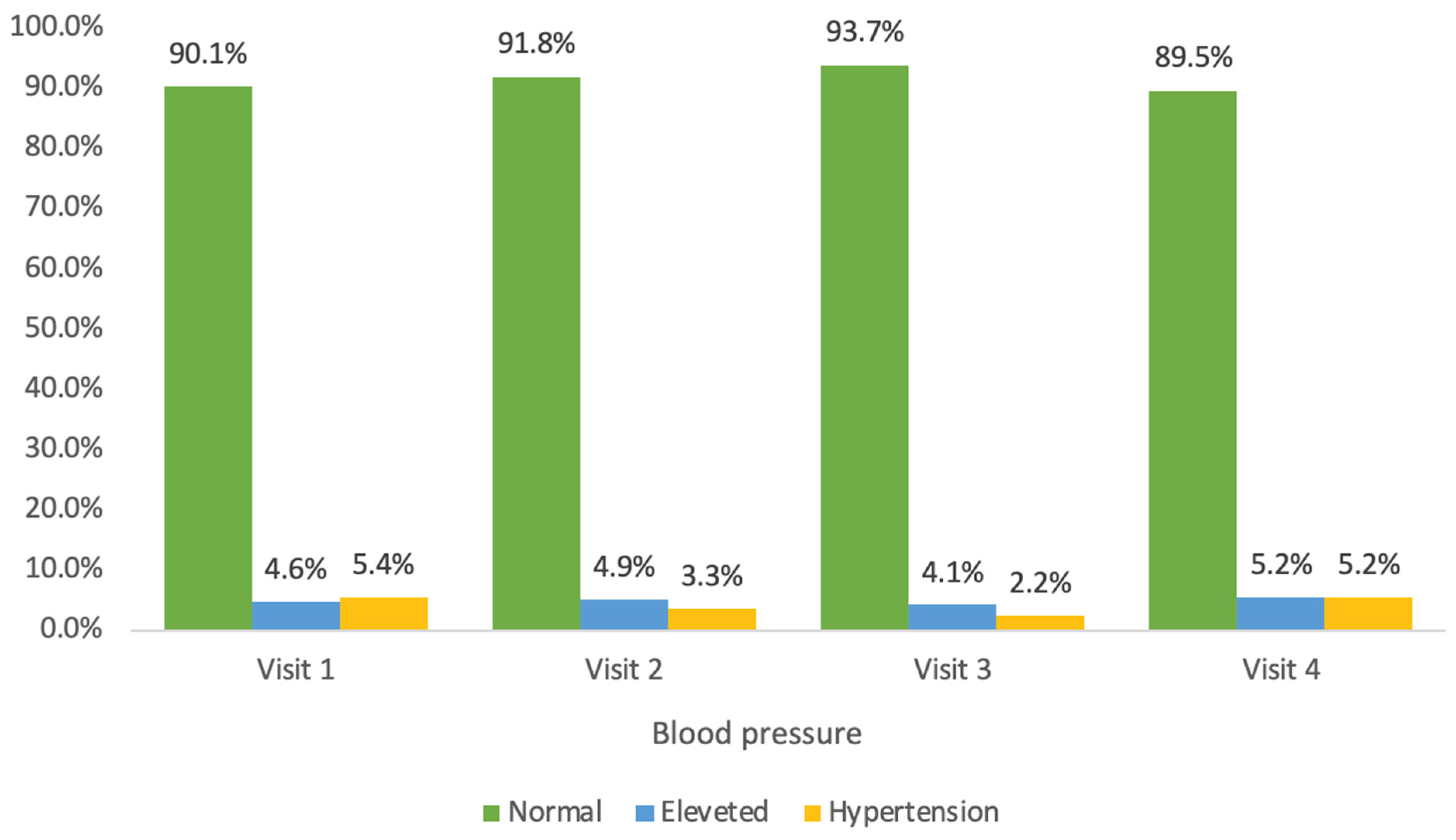
In our study, an alarmingly high percentage of children had abnormal blood pressure. Elevated systolic blood pressure was diagnosed in 10% of children, with hypertension detected in 5%. Nearly one-third of the children were found to have elevated diastolic blood pressure, with hypertension being diagnosed in 20%. During the year-long program, the percentage of children with normal diastolic blood pressure increased to 73%. However, no significant changes were observed for systolic blood pressure.
During the year-long intervention, a significant increase in the proportion of girls with normal systolic blood pressure was observed (from 92% to 96%). No such change was seen in the boys. A significant increase in the percentage of children with normal diastolic blood pressure was observed in both the girls (from 68% to 72%) and boys (from 65% to 74%).
The mean blood pressure, as well as the systolic and diastolic percentiles, were higher in the children with obesity than in those with overweight. Previous studies confirm that elevated systolic and diastolic blood pressure is more common in children with overweight and obesity compared to healthy children [
9,
10,
31,
38,
39,
40].
A review of previous meta-analyses indicates a positive effect of interventions on blood pressure values in children with excess body weight. Cai’s meta-analysis demonstrated a moderate impact of lifestyle change interventions on the blood pressure of children with excess body weight. Programs that focused solely on physical activity or dietary interventions did not show a significant effect of lowering blood pressure. However, interdisciplinary interventions significantly reduced the blood pressure of participants [
41,
42]. In Rajjo’s study, multidisciplinary interventions combining dietary education, physical activity, and behavioural therapy resulted in a significant reduction in both BMI and systolic and diastolic blood pressure. Most of the programs also observed improvements in body composition. Interestingly, in contrast to previously mentioned studies, interventions focused only on physical activity also led to a reduction in systolic blood pressure [
43]. Ho’s study found that short-term interventions lasting up to 6 months resulted in a decrease in diastolic blood pressure, while studies lasting more than a year showed a reduction in systolic blood pressure. The best results in regard to improving the blood pressure of children who are obese were achieved in an intensive, 12-week school program that included vigorous physical exercise and dietary counselling [
44]. Peirson’s study showed that even a moderate reduction in BMI in intervention programs had a significant effect on reducing the blood pressure in children with excess body weight [
35]. A significant decrease in blood pressure was observed in children with a BMI z-score reduction as small as 0.1 [
30]. A meta-analysis of interdisciplinary interventions in children with excess body weight demonstrated that a decrease in BMI during a program was associated with a reduction in blood pressure. In children who did not achieve a BMI reduction, there was no decrease in blood pressure [
42].
Due to the program’s organization in an outpatient clinic building and parental preferences, the visits took place in the afternoon (between 3 p.m. and 6 p.m.). One limitation of this study was that bioelectrical impedance analysis was not performed with the children fasting (the manufacturer recommends at least 4 h after a meal).
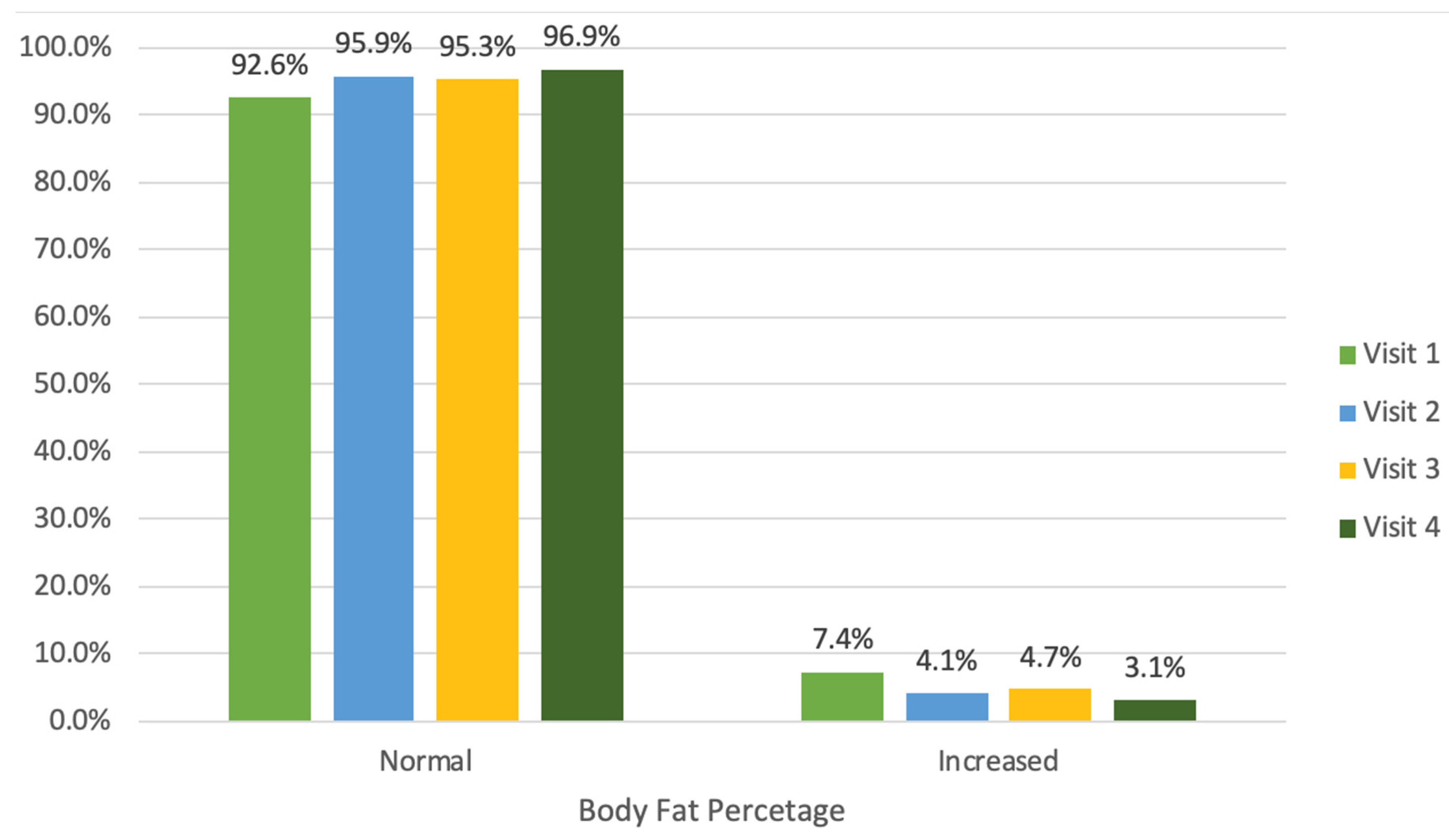
During the year-long program, there was an increase in both the average fat mass and muscle mass of the participating children. However, this is a physiological phenomenon during a child’s development. Therefore, changes in body fat percentage seems to be a more objective measure in children. There are no studies evaluating the normal values for fat mass or muscle mass in children. Furthermore, there are no studies determining the normal body fat percentage in the population of Polish children. The reference point in this study was the body fat norms for children developed from a German study involving over 22,000 children aged 3–16 years [
22].
Initially, the number of children with an abnormally high body fat percentage was 7%. Throughout the year-long program, the proportion of children with a normal body fat percentage significantly increased from 93% to 97%. During the initial visits, a significant decrease in the average body fat percentage, a decrease of 0.5% from 23.8%, was observed, although this trend was not noted during subsequent visits.
The relatively low percentage of children with elevated body fat in the study group may be related to the fact that, in children with obesity, the BIA method may underestimate the fat mass compared to the DEXA method [
45,
46]. Other studies have reported that measurements obtained through BIA indicated a lower fat percentage and mass, while the fat-free mass was higher than when measured using the DEXA method [
47,
48]. It has been shown that the agreement between BIA and DEXA results is greater in children with severe obesity than in those with mild or moderate obesity [
48].
Initially, a higher proportion of the girls (10%) had elevated body fat percentages compared to the boys (5%). However, during the year-long intervention, 98% of the girls achieved a body fat percentage within the normal range, while no significant change was observed in the boys. During the intervention, 57% of the girls and only 30% of the boys experienced a decrease in body fat percentage. The average body fat percentage decreased in the girls during the year-long program, while it increased in the boys. Therefore, the intervention resulted in a significantly better reduction in body fat percentage in the girls than in the boys. The largest number of children who achieved a decrease in fat mass was observed between the first and second visits (53% of children). During the year-long program, 17% of the children experienced a reduction in fat mass, while about 96% of the children showed an increase in muscle mass.
The average body fat percentage, fat mass, and muscle mass were higher in the children with obesity compared to the children with overweight. The change in average fat mass and muscle mass during the year-long program was independent of whether the children were in the overweight or obesity group.
Bioelectrical impedance analysis (BIA) has recently begun to be widely used in clinics, hospitals, and even commercial facilities. The widespread use of the BIA method is due to its ease of use, its non-invasiveness, and the increasing availability of this relatively inexpensive method. Importantly, body composition measurements using BIA provide reliable results [
11,
12,
13,
14]. Despite its limitations, BIA is particularly useful in monitoring changes in body composition during the treatment of excess body weight in children. Studies indicate that the greater body mass in children with obesity consists of both excess fat and fat-free mass, including bone and muscle tissue [
49].
A review of meta-analyses shows a positive effect of multidisciplinary interventions on the body composition of children with excess body weight [
50,
51,
52]. It has been shown that the desired effect was achieved especially in studies where dietary interventions were combined with physical exercise [
50]. Miguel-Etayo’s meta-analysis did not show a correlation between the duration of the intervention and improvement in the body composition of children and adolescents [
51]. Ho’s meta-analysis found a fat loss in study groups that was 3.2% greater than in control groups [
44]. Research shows that physical exercise interventions significantly affect reductions in BMI, body weight, and body fat percentage, but their effect on changes in fat-free mass, including muscle mass, is minimal [
53]. In Cai’s meta-analysis, about half of the analysed studies showed a positive effect on both fat loss and blood pressure reduction. However, nearly half of the studies showed an impact of lowering blood pressure despite having no effect on fat reduction [
41].
This study showed a strong correlation between body fat percentage and anthropometric parameters such as body weight, BMI, BMI percentile, and BMI z-score. A strong correlation was also found between fat mass and anthropometric parameters such as body weight, height, BMI, BMI percentile, BMI z-score, and muscle mass. Additionally, there was a strong correlation between muscle mass and age, as well as between anthropometric parameters such as body weight, height, and BMI.
Body composition parameters and blood pressure showed only a weak positive correlation with fat mass and systolic blood pressure. This relationship was not confirmed for diastolic blood pressure. A weak correlation was observed between elevated systolic blood pressure and body weight, as well as BMI. However, no correlation was found between elevated diastolic blood pressure and the examined parameters.
A strong correlation was found between an elevated body fat percentage and an elevated BMI, confirming that the BMI index correlates well with excess fat in children with obesity and overweight. No association was found between an elevated body fat percentage and elevated blood pressure. Similar results were obtained in Bohn’s multicentre study, which showed a stronger relationship between BMI and hypertension in children than between BMI and the fat mass measured by BIA [
54]. Other studies have confirmed the relationship between an elevated body fat percentage and elevated systolic and diastolic blood pressure in children who are both obese [
55,
56] and healthy [
57]. A study by the Polish team led by Łątka demonstrated a relationship between elevated blood pressure and fat mass, fat-free mass, and BMI [
58]. Differences in study results on the relationship between blood pressure and body composition parameters may be due to the relatively small sample sizes in the study groups.
Further monitoring studies are necessary to assess the percentage of children with excess body weight. Considering the proportion of children and the degree of BMI or fat tissue reduction during the one-year intervention, it is worth monitoring this group over a longer period to assess whether the results can be maintained in the following years, even after the intervention phase ends [
29].
Further research is also required to evaluate the effectiveness of therapeutic programs focusing on the treatment of excess body weight in children. The goal of interdisciplinary therapies is to reduce the health risks associated with obesity. A new approach to the treatment of children who are overweight and obese emphasizes not only weight loss but also the introduction of long-term, beneficial changes that lead to a healthy lifestyle.