Association of High BMI with Dental History, Sociodemographic Characteristics, and DMFT Index in Female Students at Taif University Sports Center: A Cross-Sectional Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Location, and Time
2.2. Study Participants
- (1)
- Control group (BMI between 18.5 and 24.9 kg/m2) and
- (2)
- Obese group (BMI ≥ 30 kg/m2), according to the World Health Organization (WHO) classification [21].
2.3. Sampling Methodology
2.4. Ethical Considerations
2.5. Data Collection
2.6. Data Calculation
3. Results
3.1. Sample Characteristics
3.2. BMI in Relation to Dental History
3.3. BMI in Relation to Medical, Behavioural and Social Characteristics
3.4. BMI in Relation to DMFT Index
3.5. Association Between DMFT and BMI Adjusted for Age and Diabetes Mellitus Type 2
4. Discussion
4.1. Dental History and BMI
4.2. Medical, Behavioral, and Social Characteristics
4.3. DMFT Index and BMI
4.4. Implications for Public Health and Future Research
4.5. Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alghofaili, A.A.; Aladel, A.I.; Alsoghier, A.M.; Othman, F.; Shoqeair, M.M.; Alqahtani, S.M.; Alnughaimish, A.M.; Alanazi, B.A.; AI Mosallam, S.A.; Alharbi, A.S. Association of Oral and General Health with Nutritional Status of Older Adults Attending Two Medical Centers in Riyadh, Saudi Arabia: A Cross-Sectional Study. Nutrients 2023, 15, 4032. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, S.A.; Aljohar, A.; Almulhim, B.; Alassaf, A.; Bhardwaj, S.S.; Thomas, J.T.; Almalki, A.; Aljuaid, A.O.; Mallineni, S.K. Correlation between BMI and Oral Health Status (DMFT, PI, MSBI, and Salivary 1,5-AG) among the Pediatric Population in Saudi Arabia: A Clinico-Biochemical Study. Children 2022, 9, 1017. [Google Scholar] [CrossRef] [PubMed]
- Alwafi, A.M.A.; Rajeh, H.; Farsi, N.J. Association between Obesity and Dental Caries in Adults: An Analysis of WHR, and DMFT Score. Obes. Facts 2024, 18, 39–47. [Google Scholar]
- Taghat, N.; Lingström, P.; Mossberg, K.; Fändriks, L.; Eliasson, B.; Östberg, A.-L. Oral Health by Obesity Classification in Young Obese Women–a Cross-Sectional Study. Acta Odontol. Scand. 2022, 80, 596–604. [Google Scholar] [CrossRef]
- Howe, L.D.; Kanayalal, R.; Harrison, S.; Beaumont, R.N.; Davies, A.R.; Frayling, T.M.; Davies, N.M.; Hughes, A.; Jones, S.E.; Sassi, F. Effects of Body Mass Index on Relationship Status, Social Contact and Socio-Economic Position: Mendelian Randomization and within-Sibling Study in UK Biobank. Int. J. Epidemiol. 2020, 49, 1173–1184. [Google Scholar] [CrossRef]
- Seum, T.; Meyrose, A.-K.; Rabel, M.; Schienkiewitz, A.; Ravens-Sieberer, U. Pathways of Parental Education on Children’s and Adolescent’s Body Mass Index: The Mediating Roles of Behavioral and Psychological Factors. Front. Public Health 2022, 10, 763789. [Google Scholar] [CrossRef]
- Langley-Evans, S.C.; Pearce, J.; Ellis, S. Overweight, Obesity and Excessive Weight Gain in Pregnancy as Risk Factors for Adverse Pregnancy Outcomes: A Narrative Review. J. Hum. Nutr. Diet. 2022, 35, 250–264. [Google Scholar] [CrossRef]
- Messer, T.A.; Blank, F.; Grand-Guillaume-Perrenoud, J.A.; Aubry, E.M. The Impact of Obesity on Childbirth Expectations. J. Midwifery Womens. Health 2025, 70, 96–103. [Google Scholar] [CrossRef]
- Ahmed, M.A.; Jouhar, R.; Faheemuddin, M.; AlJafar, A.; Alabawi, H.; Alhumaidi, B.; Al Madeh, M. Assessment of Oral Health Knowledge, Attitude, Practice and DMFT Scores among Patients at King Faisal University, Al-Ahsa. Medicina 2023, 59, 688. [Google Scholar] [CrossRef]
- Adam, T.R.; Hamed, A.M.; Mohammed, H.S.M.; Elshareef, T.E.E.; Mushaeb, H.; Al Harbi, A.N.A.; Bawarith, B.M.; Almalki, A.A.; Alzaheb, N.; Alqarni, A.H. Prevalence of Childhood Obesity Among Children and Adolescents in Saudi Arabia: A Systematic Review. Cureus 2024, 16, e70135. [Google Scholar] [CrossRef]
- Alqarni, A.; AlHarthi, S.; Felemban, M.; Abed, H.; Shukr, B.; Al-Johani, K.; AlShamrani, A.; Sharka, R. The Prevalence and Patterns of Common Chief Complaints among Patients at Taif University Dental Hospital, Saudi Arabia. Saudi J. Health Sci. 2024, 13, 49–55. [Google Scholar] [CrossRef]
- Chapain, K.P.; Rampal, K.G.; Gaulee Pokhrel, K.; Adhikari, C.; Hamal, D.; Pokhrel, K.N. Influence of Gender and Oral Health Knowledge on DMFT Index: A Cross Sectional Study among School Children in Kaski District, Nepal. BMC Oral Health 2023, 23, 59. [Google Scholar] [CrossRef] [PubMed]
- Chang, Q.; Cheng, M.; Xu, M.; Du, S.; Wang, X.; Feng, X.; Tai, B.; Hu, D.; Lin, H.; Wang, B.; et al. Decomposing Socioeconomic Inequalities in Dental Caries among Chinese Adults: Findings from the 4th National Oral Health Survey. BMC Oral Health 2023, 23, 372. [Google Scholar] [CrossRef]
- Alshammari, F.R.; Alamri, H.; Aljohani, M.; Sabbah, W.; O’Malley, L.; Glenny, A.-M. Dental Caries in Saudi Arabia: A Systematic Review. J. Taibah Univ. Med. Sci. 2021, 16, 643–656. [Google Scholar] [CrossRef] [PubMed]
- Teshome, A.; Muche, A.; Girma, B. Prevalence of Dental Caries and Associated Factors in East Africa, 2000–2020: Systematic Review and Meta-Analysis. Front. Public Health 2021, 9, 645091. [Google Scholar] [CrossRef]
- Hefzollesan, S.; Sharififard, N.; Mahboobi, Z.; Faramarzi, E. Relationship between DMFT Index and Reproductive History-a Cross-Sectional Study on Enrollment Phase of Azar Cohort Study. BMC Oral Health 2022, 22, 518. [Google Scholar] [CrossRef]
- Gizem, A.; Burak, D.; ŞAHİN, Ş.; Evren, B. Investigation of DMFT Index and Saliva Values in Morbidly Obese and Obese Patients. Konuralp Med. J. 2023, 15, 91–98. [Google Scholar]
- Issrani, R.; Reddy, J.; Bader, A.K.; Albalawi, R.F.; Alserhani, E.D.; Alruwaili, D.S.; Alanazi, G.R.; Alruwaili, N.S.; Sghaireen, M.G.; Rao, K. Exploring an association between body mass index and oral health: A scoping review. Diagnostics 2023, 13, 902. [Google Scholar] [CrossRef]
- Alonazi, M.A.; Algarni, H.A.; Alqarni, M.N.S.; Almaeen, S.H.; Khattak, O.; Iqbal, A. Obesity and Dental Caries in Saudi Arabia: A Correlated Study. BMC Oral Health 2024, 24, 1329. [Google Scholar] [CrossRef]
- Cheong, A.S.; Suvan, J.E. Considerations in the treatment of individuals with obesity and periodontitis. Clin. Obes. 2025, 15, e70002. [Google Scholar] [CrossRef]
- Weir, C.B.; Jan, A. BMI Classification Percentile and Cut Off Points. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2024. [Google Scholar]
- John, M.T.; Omara, M.; Su, N.; List, T.; Sekulic, S.; Häggman-Henrikson, B.; Visscher, C.M.; Bekes, K.; Reissmann, D.R.; Baba, K. Recommendations for Use and Scoring of Oral Health Impact Profile Versions. J. Evid. Based. Dent. Pract. 2022, 22, 101619. [Google Scholar] [CrossRef] [PubMed]
- Ashour, A.A.; Alqarni, A.A. Prevalence of Dental Abnormalities, Soft Tissue Pathologies and Occlusion Disorders in Patients with High BMI: A Cross-Sectional Study. Oral Health Prev. Dent. 2024, 22, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Černelič-Bizjak, M.; Guiné, R.P.F. Predictors of Binge Eating: Relevance of BMI, Emotional Eating and Sensivity to Environmental Food Cues. Nutr. Food Sci. 2022, 52, 171–180. [Google Scholar] [CrossRef]
- Abogazalah, N.; Yiannoutsos, C.; Soto-Rojas, A.E.; Bindayeld, N.; Yepes, J.F.; Martinez Mier, E.A. Distal and Proximal Influences on Self-Reported Oral Pain and Self-Rated Oral Health Status in Saudi Arabia: Retrospective Study Using a 2017 Nationwide Database. JMIR Public Health Surveill. 2024, 10, e53585. [Google Scholar] [CrossRef]
- Alwadeai, K.S.; Alhammad, S.A. Prevalence of Type 2 Diabetes Mellitus and Related Factors among the General Adult Population in Saudi Arabia between 2016–2022: A Systematic Review and Meta-Analysis of the Cross-Sectional Studies. Medicine 2023, 102, e34021. [Google Scholar] [CrossRef]
- AlShahrani, M.S. Prevalence of Obesity and Overweight among Type 2 Diabetic Patients in Bisha, Saudi Arabia. J. Fam. Med. Prim. Care 2021, 10, 143–148. [Google Scholar] [CrossRef]
- Nazar, H.; Shyama, M.; Ariga, J.; Almutawa, S.; Mahomed, O. Assessment of Oral Health Knowledge and Practices and Its Association With Sociodemographic Factors Among Government Employes and Their Clients in Kuwait: A Cross-Sectional Study. Int. J. Dent. 2025, 2025, 8880948. [Google Scholar] [CrossRef]
- Hwang, S.; Oh, H.; Rhee, M.; Kang, S.; Kim, H. Association of Periodontitis, Missing Teeth, and Oral Hygiene Behaviors with the Incidence of Hypertension in Middle-aged and Older Adults in Korea: A 10-year Follow-up Study. J. Periodontol. 2022, 93, 1283–1293. [Google Scholar] [CrossRef]
- Iwashita, M.; Hayashi, M.; Nishimura, Y.; Yamashita, A. The Link between Periodontal Inflammation and Obesity. Curr. Oral Health Rep. 2021, 8, 76–83. [Google Scholar] [CrossRef]
- Jepsen, S.; Suvan, J.; Deschner, J. The Association of Periodontal Diseases with Metabolic Syndrome and Obesity. Periodontology 2020, 83, 125–153. [Google Scholar] [CrossRef]
- Martínez-García, M.; Hernández-Lemus, E. Periodontal inflammation and systemic diseases: An overview. Front. Physiol. 2021, 12, 709438. [Google Scholar] [CrossRef] [PubMed]
- Jouhar, R.; Ahmed, M.A.; Khurshid, Z.; Bokhari, S.A. Association of BMI, Diet, Physical Activity, and Oral Hygiene Practices with DMFT Index of Male Dental Students at King Faisal University, Al-Ahsa. Nutrients 2021, 13, 224. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, S.; Deep, S.; Aggarwal, P.; Chauhan, B.; Khan, F.; Sagir, A.H. Association between Dental Caries and Body Mass Index (Bmi) among Children of 6-12 Years in Ghaziabad, UP: A Original Research. Baba Farid Univ. Dent. J. 2023, 13, 11–15. [Google Scholar]
- Almusawi, M.A.; Gosadi, I.; Abidia, R.; Almasawi, M.; Alrashood, S.T.; Ekhzaimy, A.; Alhomida, A.S.; Khan, H.A. Association between Salivary Factors and Cariogenic Bacteria in Type-2 Diabetes Patients. J. King Saud Univ. 2020, 32, 2617–2621. [Google Scholar] [CrossRef]
- Zhou, G.; Shu, X.; Long, Y.; Cao, Y.; Wang, J.; Liao, G.; Zou, L. Dental Caries and Salivary Alterations in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis. J. Dent. 2024, 150, 105321. [Google Scholar] [CrossRef]
| Variables | Control Group | Obese Group |
|---|---|---|
| Mean ± S.D. | Mean ± S.D. | |
| Age | 20.3 (±1.2) | 21 (±2.4) |
| Height | 1.59 (±0.05) | 1.54 (±0.07) |
| Weight | 52.2 (±5.8) | 102 (±11.9) |
| Body Mass Index (BMI) | 20.7 (±2.1) | 42.8 (±4.3) |
| Number of Teeth | 27.6 (±0.9) | 26.6 (±1.5) |
| Decayed Teeth (D) | 4.37 (±3.4) | 5.5 (±3.9) |
| Missing Teeth (M) | 0.62 (±1.2) | 1.6 (±1.6) |
| Filled Teeth (F) | 1.8 (±2.7) | 0.7 (±1.3) |
| DMFT score | 7.4 (±4.2) | 7.8 (±4.2) |
| Total | Control | Obese | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Total | 138 | 100.0 | 52 | 100.0 | 86 | 100.0 |
| ≤40 kg/m2 | 76 | 55.1 | 52 | 100.0 | 24 | 27.9 |
| 40–45 | 35 | 25.4 | 0 | 0 | 35 | 40.7 |
| >45 kg/m2 | 27 | 19.6 | 0 | 0 | 27 | 31.4 |
| BMI Range | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Control | 30–39.9 kg/m2 | 40–44.9 kg/m2 | >45 kg/m2 | Total | ||||||
| N | % | N | % | N | % | N | % | N | % | |
| Total | 41 | 100.0 | 3 | 100.0 | 9 | 100.0 | 9 | 100.0 | 62 | 100.0 |
| Examination | 4 | 9.8 | 0 | 0.0 | 2 | 22.2 | 1 | 11.1 | 7 | 11.3 |
| Pain | 17 | 41.5 | 3 | 100.0 | 7 | 77.8 | 7 | 77.8 | 34 | 54.8 |
| Swelling and pain | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 1 | 11.1 | 1 | 1.6 |
| Follow-up | 20 | 48.8 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 20 | 32.3 |
| BMI Range | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Control | 30–39.9 kg/m2 | 40–44.9 kg/m2 | >45 kg/m2 | Total | ||||||
| N | % | N | % | N | % | N | % | N | % | |
| Total | 52 | 100.0 | 24 | 100.0 | 35 | 100.0 | 27 | 100.0 | 138 | 100.0 |
| Healthy | 48 | 92.3 | 19 | 79.2 | 30 | 85.7 | 17 | 63.0 | 114 | 82.6 |
| Asthma | 2 | 3.8 | 4 | 16.7 | 5 | 14.3 | 1 | 3.7 | 12 | 8.7 |
| Diabetes type 2 | 1 | 1.9 | 1 | 4.2 | 0 | 0.0 | 9 | 33.3 | 11 | 8.0 |
| BMI Range | p Value Results of the Spearman’s Rank Correlation Coefficient and F-Test ANOVA | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | 30–39.9 kg/m2 | 40–44.9 kg/m2 | >45 kg/m2 | Total | ||||||||
| N | % | N | % | N | % | N | % | N | % | |||
| Father Education | Total | 52 | 100.0 | 24 | 100.0 | 35 | 100.0 | 27 | 86 | 138 | 100.0 | rS = −0.09; p = 0.413 |
| None | 0 | 0 | 1 | 4.2 | 3 | 8.6 | 4 | 8 | 8 | 5.8 | ||
| Elementary | 5 | 9.6 | 7 | 29.2 | 6 | 17.1 | 6 | 19 | 24 | 17.4 | ||
| Primary | 4 | 7.7 | 3 | 12.5 | 5 | 14.3 | 6 | 14 | 18 | 13.0 | ||
| High school | 18 | 34.6 | 7 | 29.2 | 11 | 31.4 | 5 | 23 | 41 | 29.7 | ||
| University | 25 | 48.1 | 6 | 25.0 | 10 | 28.6 | 6 | 22 | 47 | 34.1 | ||
| Mother Education | Total | 52 | 100.0 | 24 | 100.0 | 35 | 100.0 | 27 | 86 | 138 | 100.0 | rS = 0.00; p = 0.981 |
| None | 1 | 1.9 | 0 | 0.0 | 6 | 17.1 | 2 | 8 | 9 | 6.5 | ||
| Elementary | 6 | 11.5 | 4 | 16.7 | 7 | 20.0 | 7 | 18 | 24 | 17.4 | ||
| Primary | 6 | 11.5 | 6 | 25.0 | 4 | 11.4 | 6 | 16 | 22 | 15.9 | ||
| High school | 10 | 19.2 | 10 | 41.7 | 5 | 14.3 | 3 | 18 | 28 | 20.3 | ||
| University | 29 | 55.8 | 4 | 16.7 | 13 | 37.1 | 9 | 26 | 55 | 39.9 | ||
| Parents Relationship | Total | 52 | 100.0 | 24 | 100.0 | 35 | 100.0 | 27 | 86 | 138 | 100.0 | 0.751 (F) |
| Married | 41 | 78.8 | 17 | 70.8 | 22 | 62.9 | 15 | 54 | 95 | 68.8 | ||
| Separated | 3 | 5.8 | 4 | 16.7 | 6 | 17.1 | 7 | 17 | 20 | 14.5 | ||
| F/M died | 8 | 15.4 | 3 | 12.5 | 7 | 20.0 | 5 | 15 | 23 | 16.7 | ||
| Total | Control | Obese | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| Total | 138 | 100.0 | 52 | 100.0 | 86 | 100.0 |
| Rural | 72 | 52.2 | 7 | 13.5 | 65 | 75.6 |
| Village | 22 | 15.9 | 1 | 1.9 | 21 | 24.4 |
| City | 44 | 31.9 | 44 | 84.6 | 0 | 0.0 |
| BMI Range | p Value Results of the 2-Sample t-Test and Spearman’s Rank Correlation Coefficient | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Control | 30–39.9 kg/m2 | 40–44.9 kg/m2 | >45 kg/m2 | Total | ||||||||
| N | % | N | % | N | % | N | % | N | % | |||
| Brushing type | Total | 52 | 100.0 | 19 | 100.0 | 31 | 100.0 | 22 | 100.0 | 124 | 100.0 | 0.606 (t) |
| Brush | 50 | 96.2 | 13 | 68.4 | 26 | 83.9 | 16 | 72.7 | 105 | 84.7 | ||
| Miswak | 2 | 3.8 | 5 | 26.3 | 5 | 16.1 | 6 | 27.3 | 18 | 14.5 | ||
| Both | 0 | 0.0 | 1 | 5.3 | 0 | 0.0 | 0 | 0.0 | 1 | 0.8 | ||
| Brushing frequency | Total | 52 | 100.0 | 24 | 100.0 | 35 | 100.0 | 27 | 100.0 | 138 | 100.0 | rS = 0.02; p = 0.880 |
| Never | 1 | 1.9 | 6 | 25.0 | 4 | 11.4 | 6 | 22.2 | 17 | 12.3 | ||
| Once | 9 | 17.3 | 14 | 58.3 | 21 | 60.0 | 17 | 63.0 | 61 | 44.2 | ||
| Twice | 33 | 63.5 | 4 | 16.7 | 10 | 28.6 | 4 | 14.8 | 51 | 37.0 | ||
| Toothpaste Usage | Total | 52 | 100.0 | 19 | 100.0 | 31 | 100.0 | 22 | 100.0 | 124 | 100.0 | 0.690 (t) |
| Not using | 2 | 3.8 | 7 | 36.8 | 9 | 29.0 | 8 | 36.4 | 26 | 21.0 | ||
| Fluoride | 46 | 88.5 | 12 | 63.2 | 22 | 71.0 | 14 | 63.6 | 94 | 75.8 | ||
| Frequency of dental visits | Total | 52 | 100.0 | 24 | 100.0 | 35 | 100.0 | 27 | 100.0 | 138 | 100.0 | 0.366 (t) |
| Never | 8 | 15.4 | 21 | 87.5 | 26 | 74.3 | 18 | 66.7 | 73 | 52.9 | ||
| Less than 3 times | 28 | 53.8 | 3 | 12.5 | 4 | 11.4 | 7 | 25.9 | 42 | 30.4 | ||
| I don’t know | 3 | 5.8 | 0 | 0.0 | 5 | 14.3 | 2 | 7.4 | 10 | 7.2 | ||
| Daily frequency of healthy food | Total | 24 | 100.0 | 35 | 100.0 | 27 | 100.0 | 86 | 100.0 | rS = −0.01; p = 0.958 | ||
| Never | 9 | 37.5 | 4 | 11.4 | 9 | 33.3 | 22 | 25.6 | ||||
| Once | 8 | 33.3 | 19 | 54.3 | 12 | 44.4 | 39 | 45.3 | ||||
| Twice | 4 | 16.7 | 6 | 17.1 | 3 | 11.1 | 13 | 15.1 | ||||
| Three times | 3 | 12.5 | 6 | 17.1 | 3 | 11.1 | 12 | 14.0 | ||||
| Daily frequency of processed food | Total | 24 | 100.0 | 35 | 100.0 | 27 | 100.0 | 86 | 100.0 | rS = −0.08; p = 0.460 | ||
| Once | 3 | 12.5 | 5 | 14.3 | 4 | 14.8 | 12 | 14.0 | ||||
| Twice | 5 | 20.8 | 5 | 14.3 | 10 | 37.0 | 20 | 23.3 | ||||
| Three times | 12 | 50.0 | 16 | 45.7 | 9 | 33.3 | 37 | 43.0 | ||||
| BMI Range | p Value Results of Pearson’s r Correlation Coefficient | ||||||
|---|---|---|---|---|---|---|---|
| Control | 30–39.9 kg/m2 | 40–44.9 kg/m2 | >45 kg/m2 | Total | |||
| Decayed Teeth (D) | Mean | 4.37 | 5.79 | 5.31 | 5.44 | 5.07 | r = −0.03; p = 0.781 |
| Standard Deviation | 3.45 | 3.76 | 3.44 | 4.64 | 3.76 | ||
| Missing Teeth (M) | Mean | 0.62 | 1.25 | 1.80 | 1.85 | 1.27 | r = 0.20; p = 0.065 |
| Standard Deviation | 1.24 | 1.03 | 1.83 | 1.77 | 1.57 | ||
| Filled Teeth (F) | Mean | 1.81 | 0.46 | 0.94 | 0.44 | 1.09 | r = −0.06; p = 0.593 |
| Standard Deviation | 2.69 | 1.02 | 1.70 | 1.09 | 2.04 | ||
| DMFT | Mean | 6.79 | 7.50 | 8.06 | 7.74 | 7.42 | r = 0.03; p = 0.782 |
| Standard Deviation | 4.25 | 4.04 | 4.13 | 4.66 | 4.26 | ||
| Beta | 95% CI | p-Value (* p < 0.05) | |
|---|---|---|---|
| DMFT | |||
| BMI | 0.06 | −0.18 0.30 | 0.616 |
| Age | 0.06 | −0.34 0.46 | 0.759 |
| Diabetes Mellitus Type 2 | |||
| No | 0 | ||
| Yes | −1.47 | −4.55 1.61 | 0.346 |
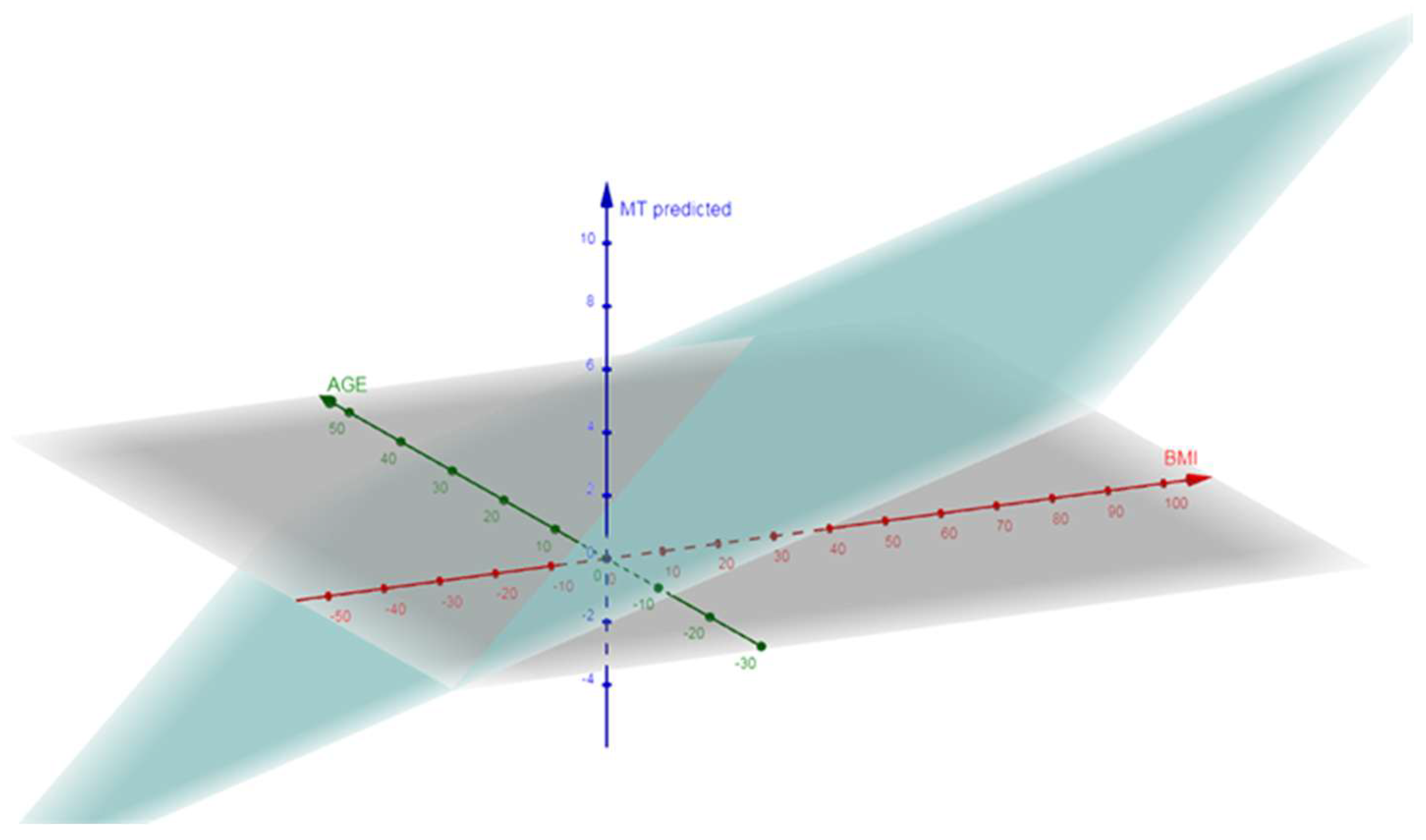
| Missing Teeth (MT) | |||
| BMI | 0.09 | 0.00 0.18 | 0.045 * |
| Age | −0.14 | −0.29 0.01 | 0.056 |
| Diabetes Mellitus Type 2 | |||
| No | 0 | ||
| Yes | 0.26 | −0.88 1.40 | 0.649 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alqarni, A.A.; Qahtani, A.A.; Albalooshy, A.M.; Shukr, B.S.; Alarabi, S.M.; Algahtani, F.S.; Alhazmi, A.O.; Felemban, M.F.; Ashour, A.A. Association of High BMI with Dental History, Sociodemographic Characteristics, and DMFT Index in Female Students at Taif University Sports Center: A Cross-Sectional Analysis. J. Clin. Med. 2025, 14, 3464. https://doi.org/10.3390/jcm14103464
Alqarni AA, Qahtani AA, Albalooshy AM, Shukr BS, Alarabi SM, Algahtani FS, Alhazmi AO, Felemban MF, Ashour AA. Association of High BMI with Dental History, Sociodemographic Characteristics, and DMFT Index in Female Students at Taif University Sports Center: A Cross-Sectional Analysis. Journal of Clinical Medicine. 2025; 14(10):3464. https://doi.org/10.3390/jcm14103464
Chicago/Turabian StyleAlqarni, Ali Abdullah, Abeer Ali Qahtani, Amal Mohammad Albalooshy, Bandar Saud Shukr, Shaimaa Mohammed Alarabi, Fahad Saeed Algahtani, Azzah Owayimer Alhazmi, Mohammed Fareed Felemban, and Amal Adnan Ashour. 2025. "Association of High BMI with Dental History, Sociodemographic Characteristics, and DMFT Index in Female Students at Taif University Sports Center: A Cross-Sectional Analysis" Journal of Clinical Medicine 14, no. 10: 3464. https://doi.org/10.3390/jcm14103464
APA StyleAlqarni, A. A., Qahtani, A. A., Albalooshy, A. M., Shukr, B. S., Alarabi, S. M., Algahtani, F. S., Alhazmi, A. O., Felemban, M. F., & Ashour, A. A. (2025). Association of High BMI with Dental History, Sociodemographic Characteristics, and DMFT Index in Female Students at Taif University Sports Center: A Cross-Sectional Analysis. Journal of Clinical Medicine, 14(10), 3464. https://doi.org/10.3390/jcm14103464






