Orthodontic Management in Pediatric Patients with Rare Diseases: Case Reports
Abstract
1. Introduction
2. Case Presentation
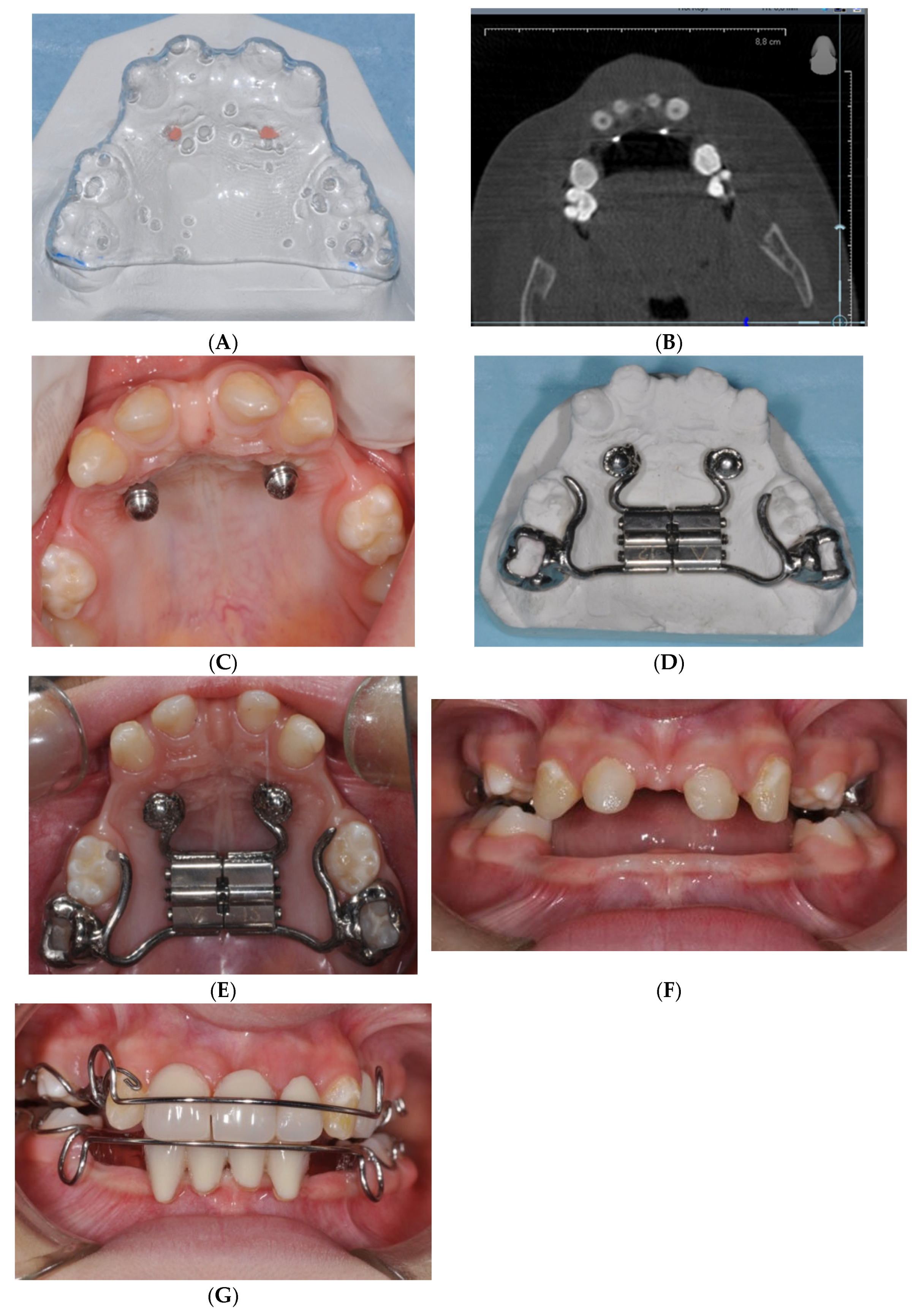
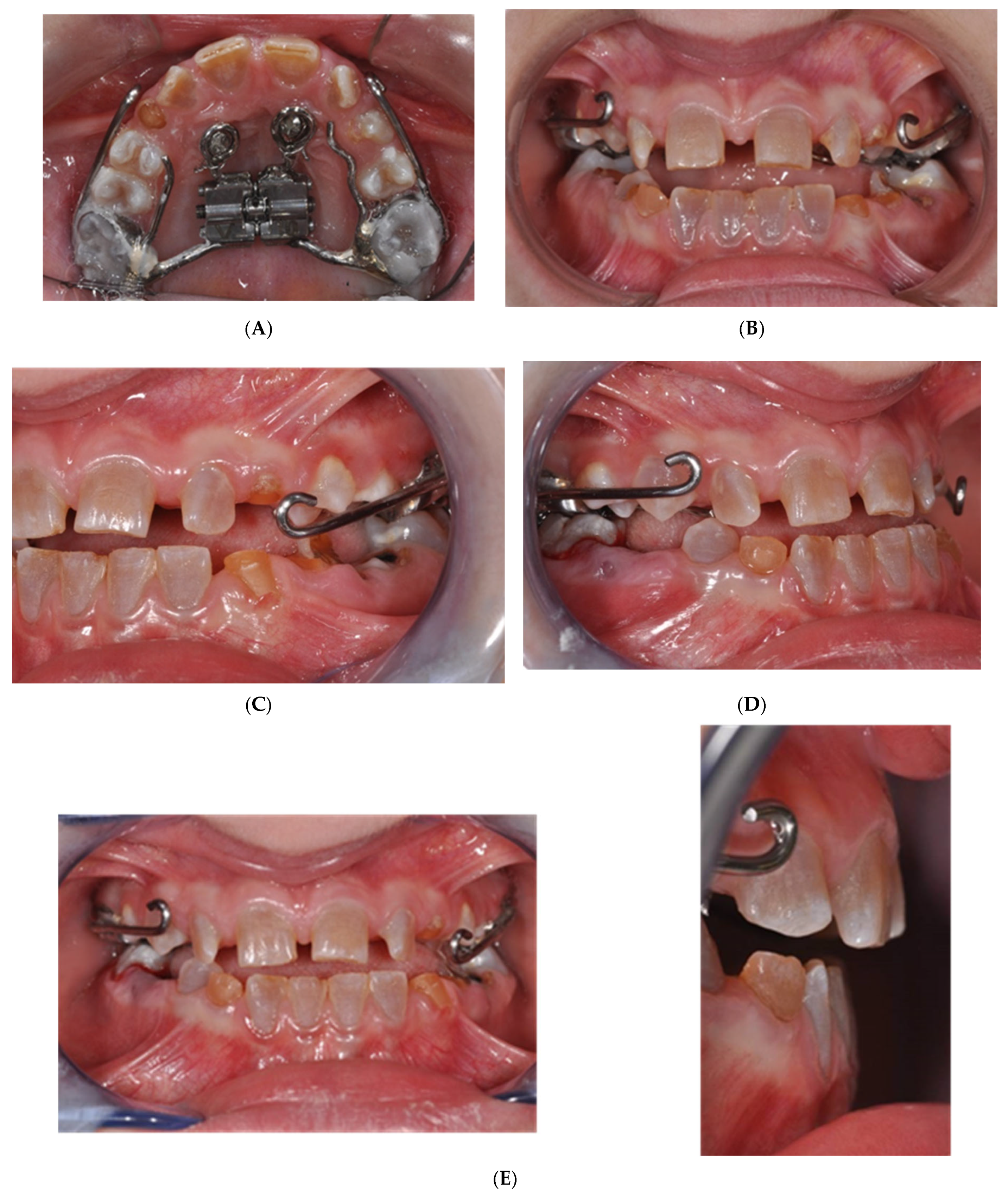
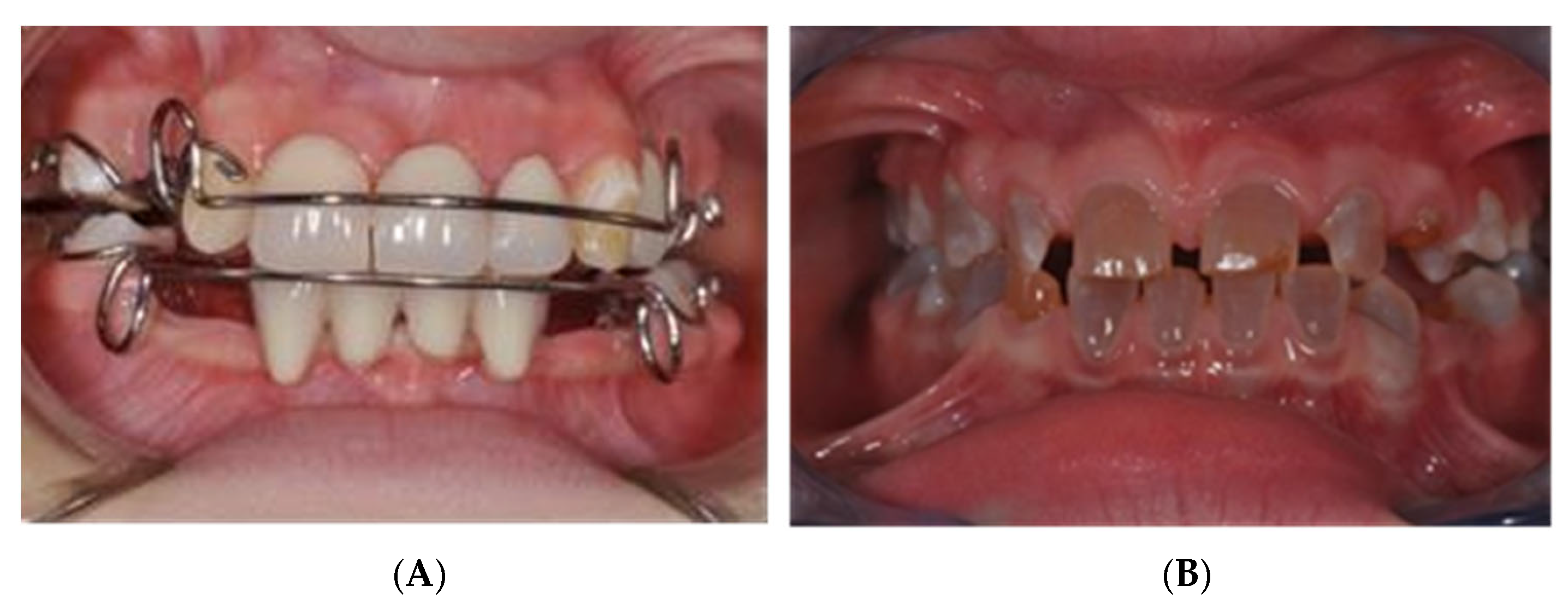
2.1. MSE Treatment in Patient with Ectodermal Dysplasia
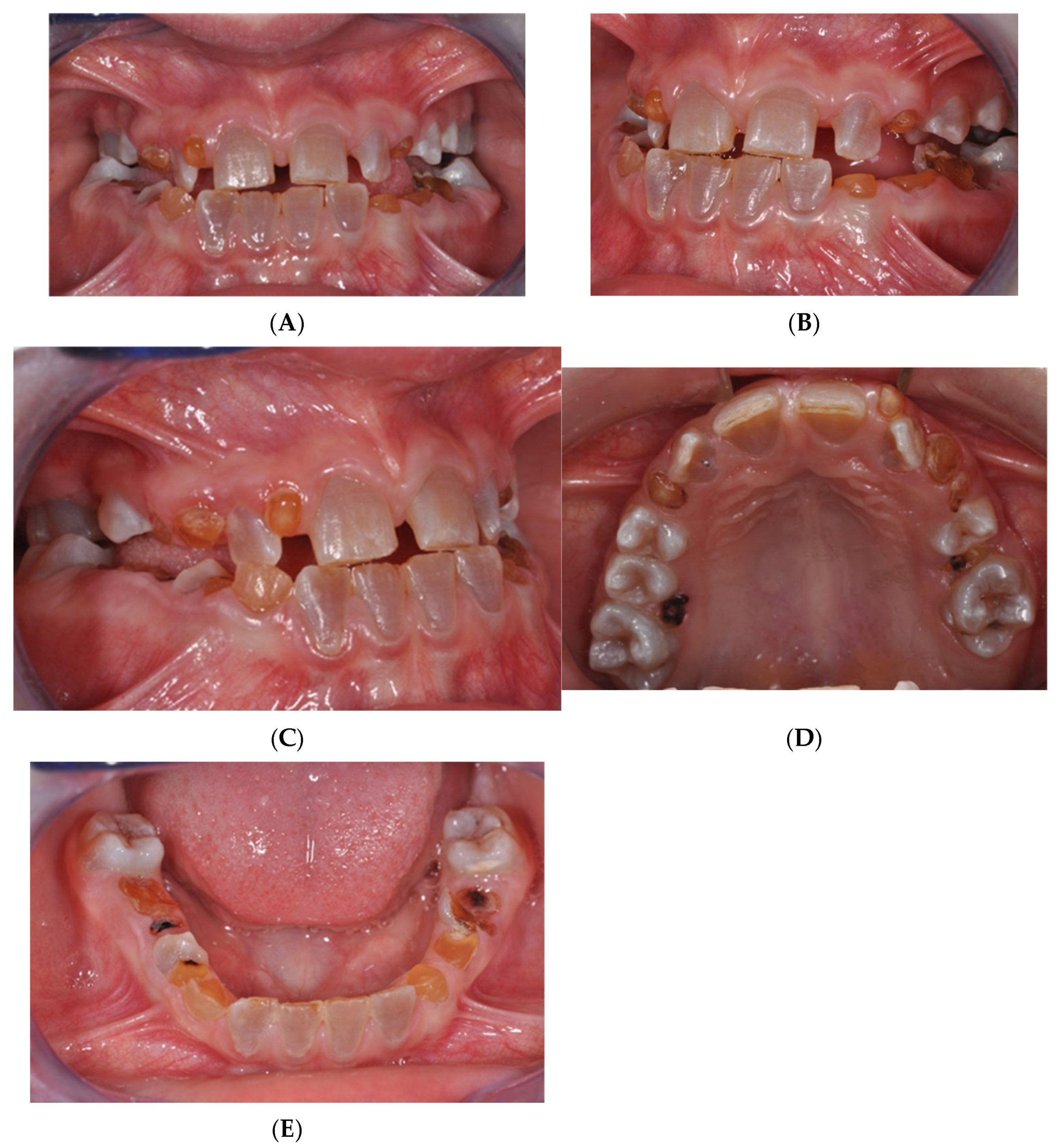
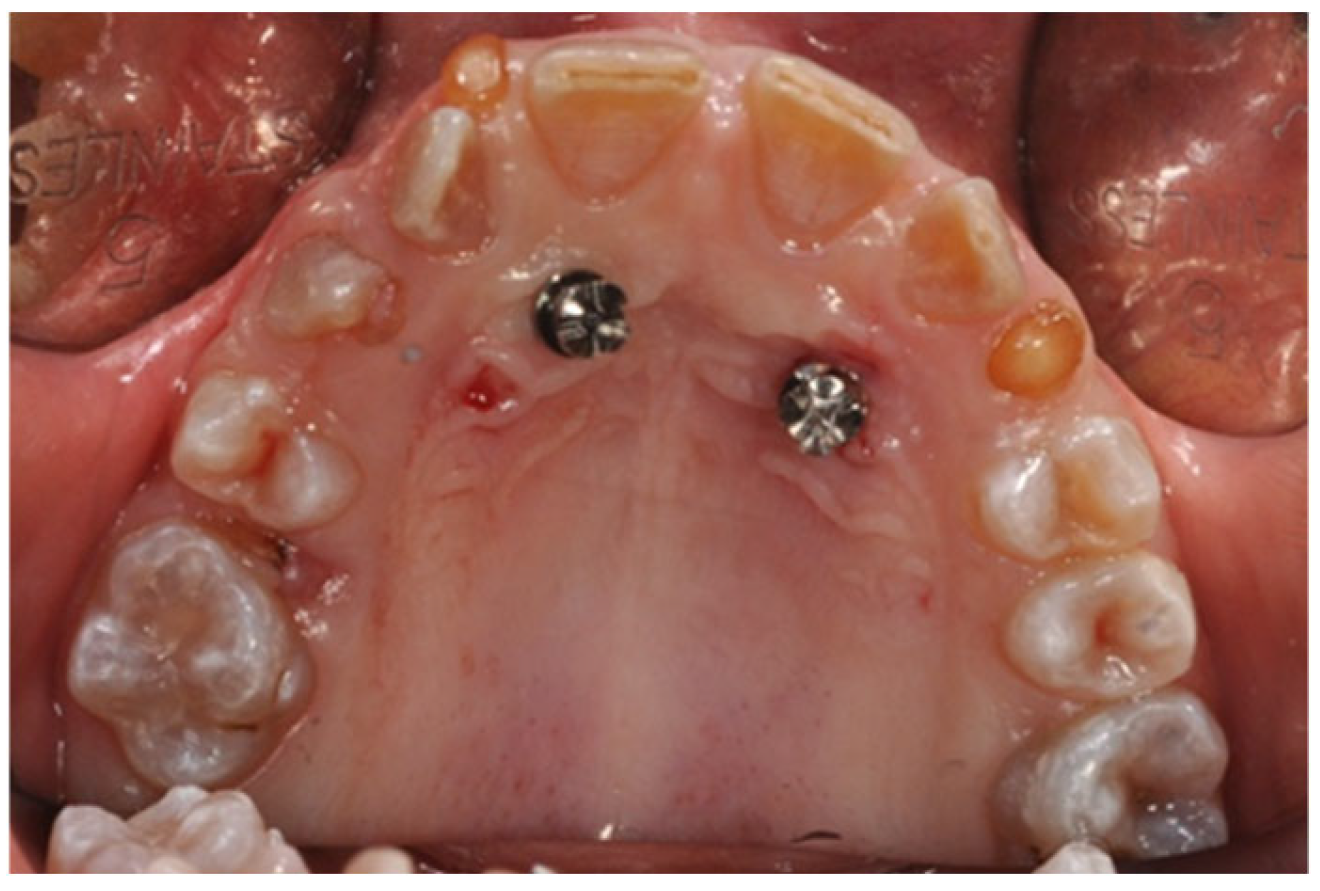
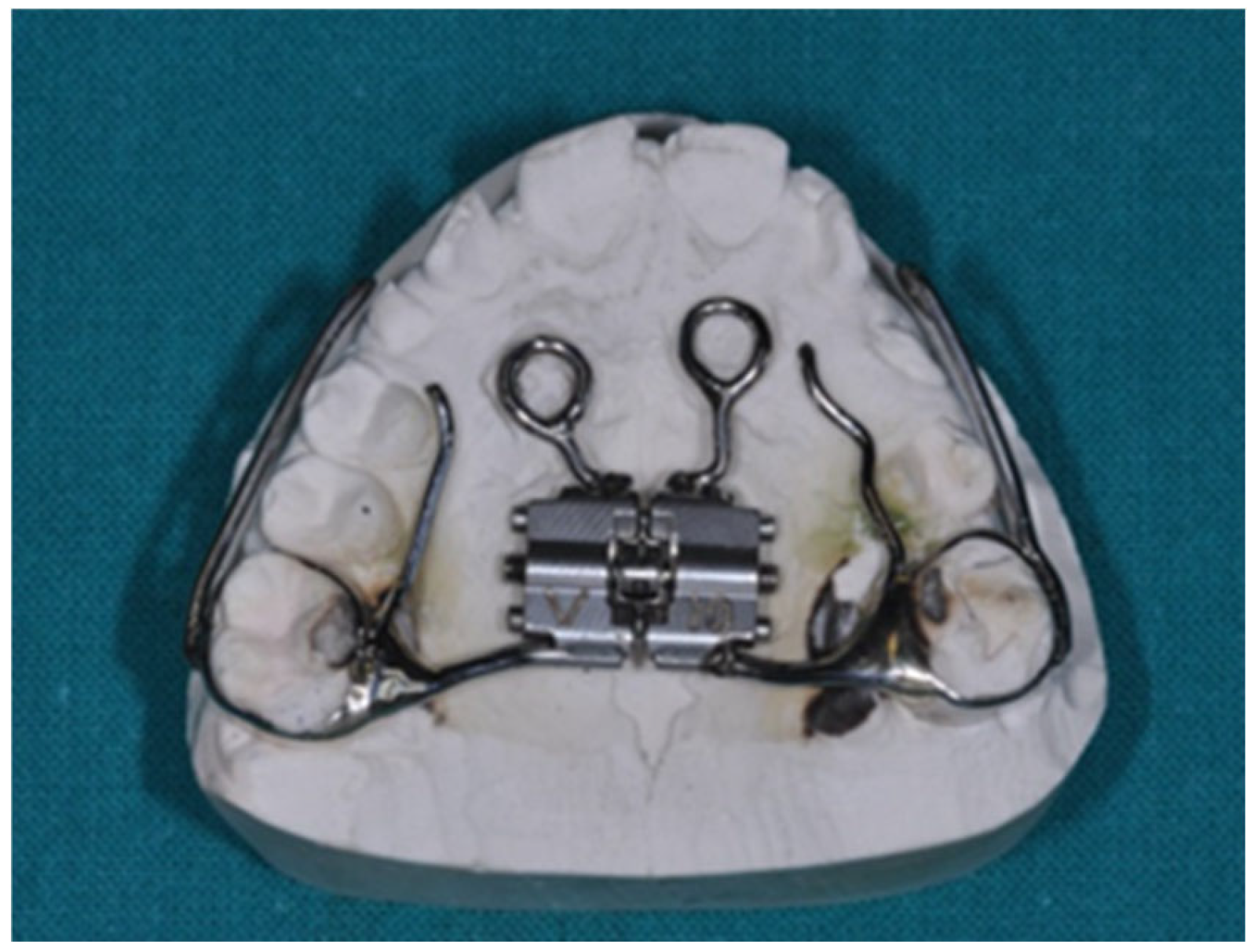
2.2. MSE Treatment in Patients with Osteogenesis Imperfecta and Dentinogenesis Imperfecta
3. Discussion
Limitation of the Study
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Reyes-Reali, J.; Mendoza-Ramos, M.I.; Garrido-Guerrero, E.; Méndez-Catalá, C.F.; Méndez-Cruz, A.R.; Pozo-Molina, G. Hypohidrotic ectodermal dysplasia: Clinical and molecular review. Int. J. Dermatol. 2018, 57, 965–972. [Google Scholar] [CrossRef] [PubMed]
- Sfeir, E.; Nassif, N.; Moukarzel, C. Use of mini dental implants in ectodermal dysplasia children: Follow-up of three cases. Eur. J. Paediatr. Dent. 2014, 15, 207–212. [Google Scholar] [PubMed]
- Hashem, A.; Kelly, A.; O’Connell, B.; O’Sullivan, M. Impact of moderate and severe hypodontia and amelogenesis imperfecta on quality of life and self-esteem of adult patients. J. Dent. 2013, 41, 689–694. [Google Scholar] [CrossRef] [PubMed]
- Kratochvilova, L.; Dostalova, T.; Schwarz, M.; Macek, M., Jr.; Marek, I.; Malíková, M.; Míšová, E. Ectodermal dysplasia: Important role of complex dental care in its interdisciplinary management. Eur. J. Paediatr. Dent. 2022, 23, 140–146. [Google Scholar] [CrossRef] [PubMed]
- Forlino, A.; Marini, J.C. Osteogenesis imperfecta. Lancet 2016, 387, 1657–1671. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Maines, E.; Monti, E.; Doro, F.; Morandi, G.; Cavarzere, P.; Antoniazzi, F. Children and adolescents treated with neridronate for osteogenesis imperfecta show no evidence of any osteonecrosis of the jaw. J. Bone Miner. Metab. 2012, 30, 434–438. [Google Scholar] [CrossRef]
- Prado, H.V.; Teixeira, S.A.; Rabello, F.; Vargas-Ferreira, F.; Borges-Oliveira, A.C.; Abreu, L.G. Malocclusion in individuals with osteogenesis imperfecta: A systematic review and meta-analysis. Oral Dis. 2022, 28, 314–325. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.S.; Binh, H.D.; Nguyen, K.M.; Maasalu, K.; Kõks, S.; Märtson, A.; Saag, M.; Jagomägi, T. Occlusal features and need for orthodontic treatment in persons with osteogenesis imperfecta. Clin. Exp. Dent. Res. 2017, 3, 19–24. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shroff, B.; Lindauer, S.J. Temporary Anchorage Devices: Biomechanical Opportunities and Challenges. In Current Therapy in Orthodontics; CHAPTER 22—Temporary Anchorage Devices: Biomechanical Opportunities and Challenges; pp. 278–290. Available online: https://typeset.io/papers/chapter-22-temporary-anchorage-devices-biomechanical-2e1aoi2si5 (accessed on 27 December 2010).
- Melsen, B. Mini-implants: Where are we? J. Clin. Orthod. 2005, 39, 539–547. [Google Scholar]
- Carvalho Ferreira, F.P.; Barbosa Lima, A.P.; de Paula, E.C.; Ferreira Conti, A.C.; Valarelli, D.P.; de Almeida-Pedrin, R.R. Orthodontic Protocol Using Mini-Implant for Class II Treatment in Patient with Special Needs. Case Rep. Dent. 2016, 2016, 1057263. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hartono, N.; Soegiharto, B.M.; Widayati, R. The difference of stress distribution of maxillary expansion using rapid maxillary expander (RME) and maxillary skeletal Expander (MSE)—A finite element analysis. Prog. Orthod. 2018, 19, 33. [Google Scholar] [CrossRef] [PubMed]
- Annarumma, F.; Aghazada, H.; Pandolfi, S. L’espansione Scheletrica Mascellare in Epoca Post-Puberale Attraverso L’utilizzo delle Miniviti Palatali. Ortho Specialized. Available online: https://www.ortospecialized.it/wp-content/uploads/2018/03/Espansione-schelettrica4.pdf (accessed on 13 November 2024).
- Baumgaertel, S.; Hans, M.G. Buccal cortical bone thickness fr mini-implant placement. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 230–235. [Google Scholar] [CrossRef] [PubMed]
- Carano, A.; Velo, S.; Incorvati, C.; Poggio, P. Clinical applications of the Mini-Screw-Anchorage-System (M.A.S.) in the maxillary alveolar bone. Prog. Orthod. 2004, 5, 212–235. (In Italian) [Google Scholar] [PubMed]
- McNamara, J.A., Jr.; Sigler, L.M.; Franchi, L.; Guest, S.S.; Baccetti, T. Changes in occlusal relationships in mixed dentition patients treated with rapid maxillary expansion. A prospective clinical study. Angle Orthod. 2010, 80, 230–238. [Google Scholar] [CrossRef]
- Derton, N.; Gracco, A.; Greco, A.M.; Luzi, C. Le Miniviti Ortodontiche—Guida All’utilizzo Clinico—Edizioni Martina; Elsevier Science: Amsterdam, The Netherlands, 2015; ISBN 978-88.7572-210-4. Available online: https://www.infona.pl/resource/bwmeta1.element.elsevier-45b36db9-b8a0-3788-9db8-c77557123d7e (accessed on 13 November 2024).
- Moyers, R.E. Manuale di Ortodonzia, 4th ed.; Moyers Robert, E., Ed.; Scienza Tecnica Dentistica, 1991; ISBN/EAN: 350005; Available online: https://www.medicalinformation.it/manuale-di-ortodonzia-moyers.html (accessed on 13 November 2024).
- Cope, J.B. Temporary devices in orthodontic: A paradigm shift. Semin. Orthod. 2005, 11, 3–9. [Google Scholar] [CrossRef]
- Wehrbein, H.; Gollner, P. Skeletal anchorage in orthodontics—Basics and clinical application. J. Orofac. Orthop. 2007, 68, 443–461. [Google Scholar]
- Kakali, L.; Alharbi, M.; Pandis, N.; Gkantidis, N.; Loukos, D. Success of palatal implants or miniscrews placed median or paramedian for the reinforcement of anchora during orthodontic treatment: A systematic review. Eur. J. Orthod. 2019, 41, 9–20. [Google Scholar] [CrossRef]
- Bernhart, T.; Vollgruber, A.; Gahleitner, A.; Dortbudak, O.; Haas, R. Alternative to the median region of the palate for placement of an orthodontic implant. Clin. Oral Implant. Res. 2000, 11, 595–601. [Google Scholar] [CrossRef]
- Papadopoulos, M.A.; Tarawneh, F. The use of miniscrews implants for temporary skeletal anchorage in orthodontics: A comprehensive review. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2007, 103, e6–e15. [Google Scholar]
- Leo, M.; Cerroni, L.; Pasquantonio, G.; Condò, S.G.; Condò, R. Temporary anchorage deviced (TADs) in orthodontics: Review of the factors that influence the clinical success rate of the mini-implants. Clin. Ter. 2016, 167, e70–e77. [Google Scholar]
- Elfituri, A.A.; De Nova, M.J.; Najirad, M. The impact of osteogenesis imperfecta severity on oral health-related quality of life in Spain: A cross-sectional study. Orphanet. J. Rare Dis. 2024, 19, 108, Erratum in Orphanet. J. Rare Dis. 2024, 19, 166. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Manni, A.; Cozzani, M.; Tamborrino, F. Factors influencing the stability of miniscrews. A retrospective study on 300 miniscrews. Eur. J. Orthod. 2011, 33, 388–395. [Google Scholar] [CrossRef] [PubMed]
- Ierardo, G.; Luzzi, V.; Sfasciotti, G.L.; Nardacci, G.; Polimeni, A.; Vozza, I. Using of modified rapid palate expander with miniscrews in a patient affected by ectodermic dysplasia. Clin Ter. 2019, 170, e168–e173. [Google Scholar] [CrossRef] [PubMed]
- Moon, C.H.; Park, H.K.; Nam, J.S.; Im, J.S.; Baek, S.H. Relationship between vertical skeletal pattern and success rate of orthodontic mini-implants. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Giancotti, A.; Germano, F.; Muzzi, F.A. miniscrew-supported intrusion auxiliary for open-bite treatment with Invisalign. J. Clin. Orthod. 2014, 48, 348–358. [Google Scholar]
- Janssen, K.I.; Raghoebar, G.M.; Vissink, A.; Sandham, A. Skeletal anchorage in orthodontics--a review of various systems in animal and human studies. Int. J. Oral Maxillofac. Implant. 2008, 23, 75–88. [Google Scholar] [PubMed]
- Giancotti, A.; Greco, M.; Mampieri, G. Palatal-implant anchorage in an adult class II patient. J. Clin. Orthod. 2011, 45, 627–634. [Google Scholar]
- Justens, E.; De Bruyn, H. Clinical outcome of mini-screws used as orthodontic anchorage. Clin. Implant. Dent. Relat. Res. 2008, 10, 174–180. [Google Scholar] [CrossRef]
- Lee, S.J.; Ahn, S.J.; Lee, J.W. Survival analysis of orthodontic mini-implants. Am. J. Orthod. Dentofac. Orthop. 2010, 137, 194–199. [Google Scholar] [CrossRef]
- Jaramillo-Bedoya, D.; Villegas-Giraldo, G.; Agudelo-Suárez, A.A.; Ramírez-Ossa, D.M. A Scoping Review about the Characteristics and Success-Failure Rates of Temporary Anchorage Devices in Orthodontics. Dent. J. 2022, 10, 78. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Reznikov, N.; Dagdeviren, D.; Tamimi, F.; Glorieux, F.; Rauch, F.; Retrouvey, J.M. Cone-Beam Computed Tomography of Osteogenesis Imperfecta Types III and IV: Three-Dimensional Evaluation of Craniofacial Features and Upper Airways. J. Bone Miner. Res. Plus 2019, 3, e10124. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Messineo, D.; Luzzi, V.; Pepe, F.; Celli, L.; Turchetti, A.; Zambrano, A.; Celli, M.; Polimeni, A.; Ierardo, G. New 3D Cone Beam CT Imaging Parameters to Assist the Dentist in Treating Patients with Osteogenesis Imperfecta. Healthcare 2020, 8, 546. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Di Carlo, G.; Saccucci, M.; Ierardo, G.; Luzzi, V.; Occasi, F.; Zicari, A.M.; Duse, M.; Polimeni, A. Rapid Maxillary Expansion and Upper Airway Morphology: A Systematic Review on the Role of Cone Beam Computed Tomography. Biomed. Res. Int. 2017, 2017, 5460429. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Uribe, F.; Mehr, R.; Mathur, A. Failure rates of mini-implants placed in the infrazygomatic region. Prog. Orthod. 2015, 16, 31. [Google Scholar] [CrossRef] [PubMed]
- Wu, T.Y.; Kuang, S.H.; Wu, C.H. Factors associated with the stability of mini-implants for orthodontic anchorage: A study of 414 samples in Taiwan. J. Oral Maxillofac. Surg. 2009, 67, 1595–1599. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luzzi, V.; Fioravanti, M.; Mitrano, L.; Marasca, B.; Saccucci, M.; Celli, M.; Celli, L.; Vozza, I.; Ierardo, G. Orthodontic Management in Pediatric Patients with Rare Diseases: Case Reports. J. Clin. Med. 2025, 14, 55. https://doi.org/10.3390/jcm14010055
Luzzi V, Fioravanti M, Mitrano L, Marasca B, Saccucci M, Celli M, Celli L, Vozza I, Ierardo G. Orthodontic Management in Pediatric Patients with Rare Diseases: Case Reports. Journal of Clinical Medicine. 2025; 14(1):55. https://doi.org/10.3390/jcm14010055
Chicago/Turabian StyleLuzzi, Valeria, Miriam Fioravanti, Lilia Mitrano, Beatrice Marasca, Matteo Saccucci, Mauro Celli, Luca Celli, Iole Vozza, and Gaetano Ierardo. 2025. "Orthodontic Management in Pediatric Patients with Rare Diseases: Case Reports" Journal of Clinical Medicine 14, no. 1: 55. https://doi.org/10.3390/jcm14010055
APA StyleLuzzi, V., Fioravanti, M., Mitrano, L., Marasca, B., Saccucci, M., Celli, M., Celli, L., Vozza, I., & Ierardo, G. (2025). Orthodontic Management in Pediatric Patients with Rare Diseases: Case Reports. Journal of Clinical Medicine, 14(1), 55. https://doi.org/10.3390/jcm14010055






