Sexualized Drug Use and Chemsex among Men Who Have Sex with Men in Europe: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Searchers
- P (population): men who have sex with men;
- I (intervention): “chemsex”, “sexualized drug use”;
- C (comparator): men who have sex with men;
- O (outcomes): “sexually transmitted diseases”.
2.2. Study Selection
2.3. Data Extraction
2.4. Methodological Quality Assessment
2.5. Data Synthesis and Analysis
3. Results
3.1. Chemsex Definition
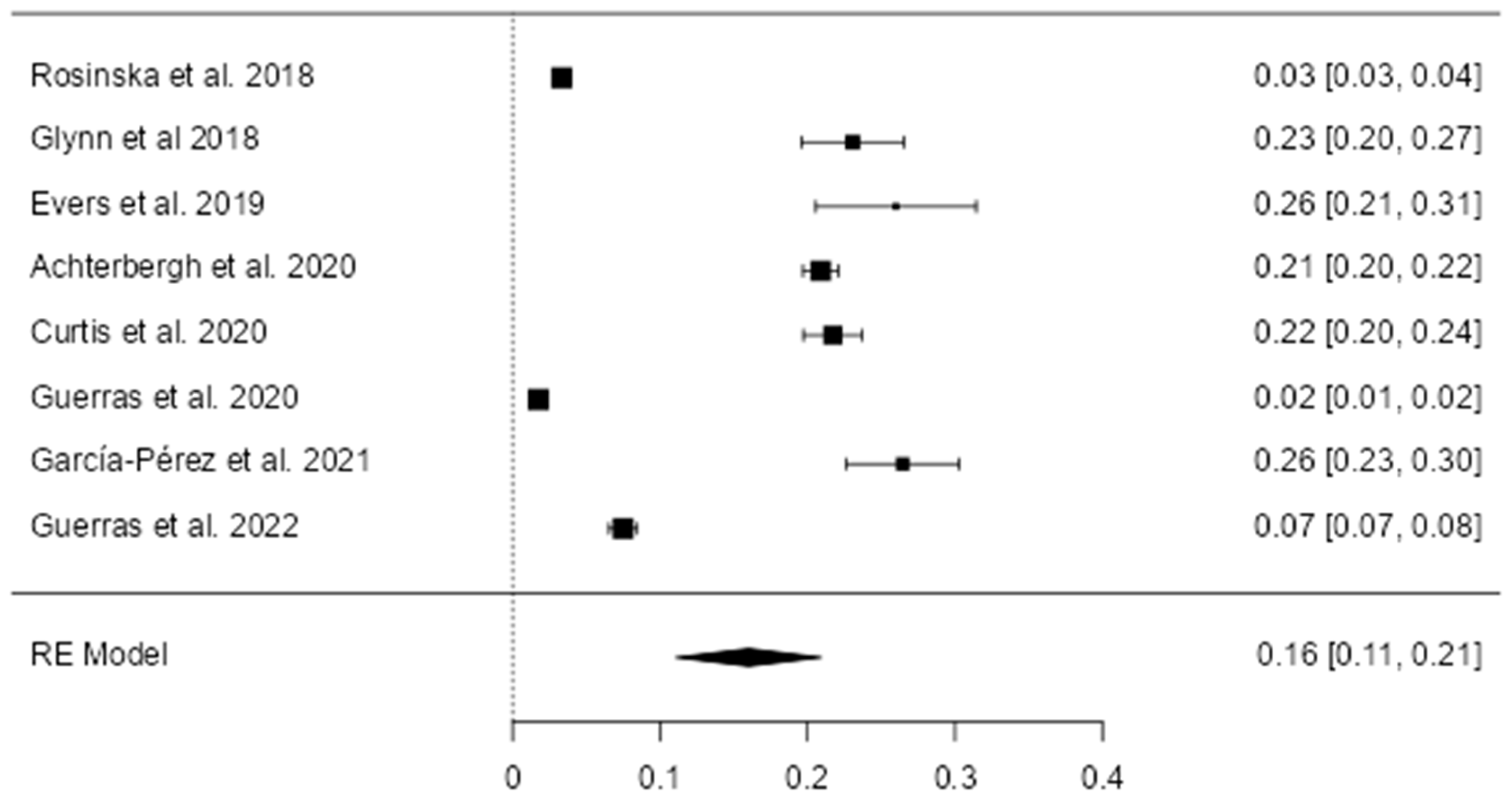
3.2. Prevalence of Chemsex and SDU
3.3. Sexual Risky Behaviors
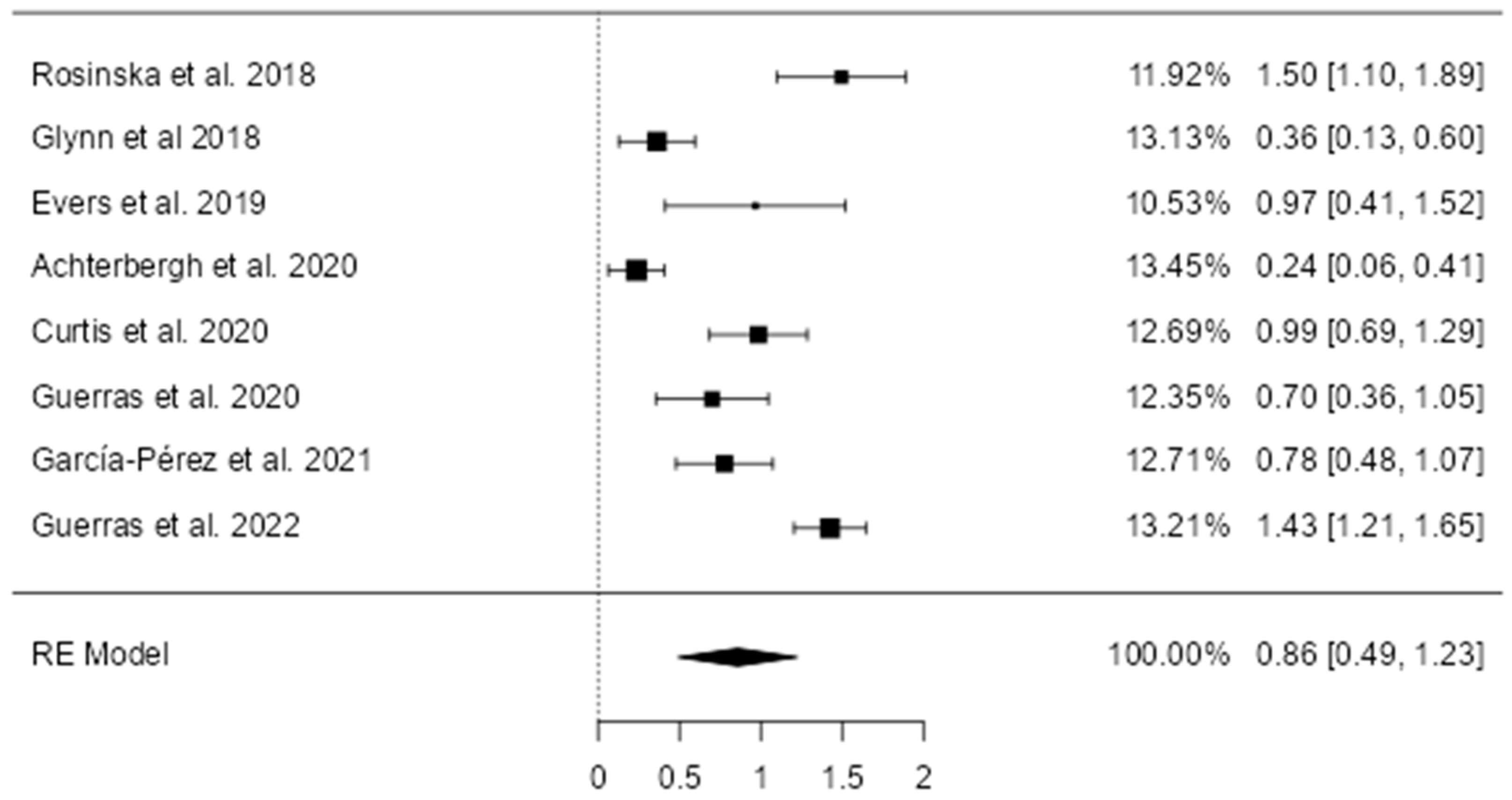
3.4. Sexually Transmitted Disease Risk
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kirby, T.; Thornber-Dunwell, M. High-Risk Drug Practices Tighten Grip on London Gay Scene. Lancet 2013, 381, 101–102. [Google Scholar] [CrossRef] [PubMed]
- Weatherburn, P.; Hickson, F.; Reid, D.; Torres-Rueda, S.; Bourne, A. Motivations and Values Associated with Combining Sex and Illicit Drugs (Chemsex) among Gay Men in South London: Findings from a Qualitative Study. Sex. Transm. Infect. 2017, 93, 203–206. [Google Scholar] [CrossRef] [PubMed]
- Bourne, A.; Reid, D.; Hickson, F.; Torres-Rueda, S.; Weatherburn, P. Illicit Drug Use in Sexual Settings (‘chemsex’) and HIV/STI Transmission Risk Behaviour among Gay Men in South London: Findings from a Qualitative Study. Sex. Transm. Infect. 2015, 91, 564–568. [Google Scholar] [CrossRef]
- PHE Public Health England. Substance Misuse Services for Men Who Have Sex with Men Involved in Chemsex. 2015, 1–11. Available online: https://assets.publishing.service.gov.uk/media/5a74bf61e5274a3f93b487db/Substance_misuse_services_for_men_who_have_sex_with_men_involved_in_chemsex.pdf (accessed on 22 February 2024).
- Tomkins, A.; George, R.; Kliner, M. Sexualised Drug Taking among Men Who Have Sex with Men: A Systematic Review. Perspect. Public Health 2019, 139, 23–33. [Google Scholar] [CrossRef]
- Maxwell, S.; Shahmanesh, M.; Gafos, M. Chemsex Behaviours among Men Who Have Sex with Men: A Systematic Review of the Literature. Int. J. Drug Policy 2019, 63, 74–89. [Google Scholar] [CrossRef]
- Carey, J.W.; Mejia, R.; Bingham, T.; Ciesielski, C.; Gelaude, D.; Herbst, J.H.; Sinunu, M.; Sey, E.; Prachand, N.; Jenkins, R.A.; et al. Drug Use, High-Risk Sex Behaviors, and Increased Risk for Recent HIV Infection among Men Who Have Sex with Men in Chicago and Los Angeles. AIDS Behav. 2009, 13, 1084–1096. [Google Scholar] [CrossRef] [PubMed]
- González-Baeza, A.; Dolengevich-Segal, H.; Pérez-Valero, I.; Cabello, A.; Téllez, M.J.; Sanz, J.; Pérez-Latorre, L.; Bernardino, J.I.; Troya, J.; De La Fuente, S.; et al. Sexualized Drug Use (Chemsex) Is Associated with High-Risk Sexual Behaviors and Sexually Transmitted Infections in HIV-Positive Men Who Have Sex with Men: Data from the U-SEX GESIDA 9416 Study. AIDS Patient Care STDS 2018, 32, 112–118. [Google Scholar] [CrossRef]
- Zhang, Y.; Bao, R.; Leuba, S.I.; Li, J.; Wang, H.; Zhang, J.; Chu, Z.; Geng, W.; Jiang, Y.; Xu, J. Association of Nitrite Inhalants Use and Unprotected Anal Intercourse and HIV/Syphilis Infection among MSM in China: A Systematic Review and Meta-Analysis. BMC Public Health 2020, 20, 1378. [Google Scholar] [CrossRef]
- Wong, N.S.; Kwan, T.H.; Lee, K.C.K.; Lau, J.Y.C.; Lee, S.S. Delineation of Chemsex Patterns of Men Who Have Sex with Men in Association with Their Sexual Networks and Linkage to HIV Prevention. Int. J. Drug Policy 2020, 75, 102591. [Google Scholar] [CrossRef]
- Chen, J.; Huang, Y.L.; Chen, H.L.; Xia, J. Nitrite Inhalants Use, Sexual Behaviors and HIV/Syphilis Infection among Men Who Have Sex with Men in Chongqing, China. Infect. Dis. Poverty 2020, 9, 127. [Google Scholar] [CrossRef]
- Spindler, H.H.; Scheer, S.; Chen, S.Y.; Klausner, J.D.; Katz, M.H.; Valleroy, L.A.; Schwarcz, S.K. Viagra, Methamphetamine, and HIV Risk: Results from a Probability Sample of MSM, San Francisco. Sex. Transm. Dis. 2007, 34, 586–591. [Google Scholar] [CrossRef]
- Hibbert, M.P.; Hillis, A.; Brett, C.E.; Porcellato, L.A.; Hope, V.D. A Narrative Systematic Review of Sexualised Drug Use and Sexual Health Outcomes among LGBT People. Int. J. Drug Policy 2021, 93, 103187. [Google Scholar] [CrossRef] [PubMed]
- Race, K.; Murphy, D.; Pienaar, K.; Lea, T. Injecting as a Sexual Practice: Cultural Formations of ‘Slamsex’. Sexualities 2023, 26, 620–637. [Google Scholar] [CrossRef]
- Guerra, F.M.; Salway, T.J.; Beckett, R.; Friedman, L.; Buchan, S.A. Review of Sexualized Drug Use Associated with Sexually Transmitted and Blood-Borne Infections in Gay, Bisexual and Other Men Who Have Sex with Men. Drug Alcohol Depend. 2020, 216, 108237. [Google Scholar] [CrossRef] [PubMed]
- Sewell, J.; Cambiano, V.; Miltz, A.; Speakman, A.; Lampe, F.C.; Phillips, A.; Stuart, D.; Gilson, R.; Asboe, D.; Nwokolo, N.; et al. Changes in Recreational Drug Use, Drug Use Associated with Chemsex, and HIV-Related Behaviours, among HIV-Negative Men Who Have Sex with Men in London and Brighton, 2013–2016. Sex. Transm. Infect. 2018, 94, 494–501. [Google Scholar] [CrossRef] [PubMed]
- Sewell, J.; Miltz, A.; Lampe, F.C.; Cambiano, V.; Speakman, A.; Phillips, A.N.; Stuart, D.; Gilson, R.; Asboe, D.; Nwokolo, N.; et al. Poly Drug Use, Chemsex Drug Use, and Associations with Sexual Risk Behaviour in HIV-Negative Men Who Have Sex with Men Attending Sexual Health Clinics. Int. J. Drug Policy 2017, 43, 33–43. [Google Scholar] [CrossRef]
- Ruiz-Robledillo, N.; Ferrer-Cascales, R.; Portilla-Tamarit, I.; Alcocer-Bruno, C.; Clement-Carbonell, V.; Portilla, J. Chemsex Practices and Health-Related Quality of Life in Spanish Men with Hiv Who Have Sex with Men. J. Clin. Med. 2021, 10, 1662. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- PROSPERO. Available online: https://www.crd.york.ac.uk/prospero/#guidancenotes (accessed on 27 December 2022).
- Risk of Bias Tools—Current Version of RoB 2. Available online: https://www.riskofbias.info/welcome/rob-2-0-tool/current-version-of-rob-2 (accessed on 18 August 2022).
- Vandenbroucke, J.P.; Von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. PLoS Med. 2007, 4, 1628–1654. [Google Scholar] [CrossRef]
- DerSimonian, R.; Laird, N. Meta-Analysis in Clinical Trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Cochran, W.G. Some Methods for Strengthening the Common χ2 Tests. Biometrics 1954, 10, 417. [Google Scholar] [CrossRef]
- The Jamovi Project 2023. Available online: https://www.jamovi.org (accessed on 20 September 2023).
- R Core Team. R: A Language and Environment for Statistical Computing; R Core Team: Vienna, Austria, 2021. [Google Scholar]
- Viechtbauer, W. Conducting Meta-Analyses in R with the Metafor Package. J. Stat. Softw. 2010, 36, 1–48. [Google Scholar] [CrossRef]
- Rosińska, M.; Gios, L.; Nöstlinger, C.; Vanden Berghe, W.; Marcus, U.; Schink, S.; Sherriff, N.; Jones, A.M.; Folch, C.; Dias, S.; et al. Prevalence of Drug Use during Sex amongst MSM in Europe: Results from a Multi-Site Bio-Behavioural Survey. Int. J. Drug Policy 2018, 55, 231–241. [Google Scholar] [CrossRef]
- Glynn, R.W.; Byrne, N.; O’Dea, S.; Shanley, A.; Codd, M.; Keenan, E.; Ward, M.; Igoe, D.; Clarke, S. Chemsex, Risk Behaviours and Sexually Transmitted Infections among Men Who Have Sex with Men in Dublin, Ireland. Int. J. Drug Policy 2018, 52, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Evers, Y.J.; Van Liere, G.A.F.S.; Hoebe, C.J.P.A.; Dukers-Muijrers, N.H.T.M. Chemsex among Men Who Have Sex with Men Living Outside Major Cities and Associations with Sexually Transmitted Infections: A Cross-Sectional Study in the Netherlands. PLoS ONE 2019, 14, e216732. [Google Scholar] [CrossRef] [PubMed]
- Achterbergh, R.C.A.; Drückler, S.; van Rooijen, M.S.; van Aar, F.; Slurink, I.A.L.; de Vries, H.J.C.; Boyd, A. Sex, Drugs, and Sexually Transmitted Infections: A Latent Class Analysis among Men Who Have Sex with Men in Amsterdam and Surrounding Urban Regions, the Netherlands. Drug Alcohol Depend. 2020, 206, 107526. [Google Scholar] [CrossRef] [PubMed]
- Curtis, T.J.; Rodger, A.J.; Burns, F.; Nardone, A.; Copas, A.; Wayal, S. Patterns of Sexualised Recreational Drug Use and Its Association with Risk Behaviours and Sexual Health Outcomes in Men Who Have Sex with Men in London, UK: A Comparison of Cross-Sectional Studies Conducted in 2013 and 2016. Sex. Transm. Infect. 2020, 96, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Guerras, J.M.; Hoyos Miller, J.; Agustí, C.; Chanos, S.; Pichon, F.; Kuske, M.; Cigan, B.; Fuertes, R.; Stefanescu, R.; Ooms, L.; et al. Association of Sexualized Drug Use Patterns with HIV/STI Transmission Risk in an Internet Sample of Men Who Have Sex with Men from Seven European Countries. Arch. Sex. Behav. 2021, 50, 461–477. [Google Scholar] [CrossRef] [PubMed]
- García-Pérez, J.N.; Cañas-Ruano, E.; Navarro, J.; Raventós, B.; López, L.; Broto, C.; Arando, M.; Barberá, M.J.; Descalzo, V.; Suanzes, P.; et al. Sexual Behavior and Drug Use Impact in Gay, Bisexual, and Other Men Who Have Sex with Men. Med. Clin. (Barc.) 2022, 159, 563–568. [Google Scholar] [CrossRef]
- Guerras, J.M.; Hoyos, J.; Agustí, C.; Casabona, J.; Sordo, L.; Pulido, J.; de la Fuente, L.; Belza, M.J. Substance Use in Sexual Context among Spanish Resident Men Who Have Sex with Men. Adicciones 2022, 34, 37–50. [Google Scholar] [CrossRef]
- Edmundson, C.; Heinsbroek, E.; Glass, R.; Hope, V.; Mohammed, H.; White, M.; Desai, M. Sexualised Drug Use in the United Kingdom (UK): A Review of the Literature. Int. J. Drug Policy 2018, 55, 131–148. [Google Scholar] [CrossRef] [PubMed]
- Schreck, B.; Victorri-Vigneau, C.; Guerlais, M.; Laforgue, E.; Grall-Bronnec, M. Slam Practice: A Review of the Literature. Eur. Addict. Res. 2021, 27, 161–178. [Google Scholar] [CrossRef] [PubMed]
- European Drug Report 2022: Trends and Developments|Www.Emcdda.Europa.Eu. Available online: https://www.emcdda.europa.eu/publications/edr/trends-developments/2022_en (accessed on 22 February 2024).
- Closson, E.F.; Mitty, J.A.; Malone, J.; Mayer, K.H.; Mimiaga, M.J. Exploring Strategies for PrEP Adherence and Dosing Preferences in the Context of Sexualized Recreational Drug Use among MSM: A Qualitative Study. AIDS Care—Psychol. Socio-Medical Asp. AIDS/HIV 2018, 30, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Hegazi, A.; Lee, M.J.; Whittaker, W.; Green, S.; Simms, R.; Cutts, R.; Nagington, M.; Nathan, B.; Pakianathan, M.R. Chemsex and the City: Sexualised Substance Use in Gay Bisexual and Other Men Who Have Sex with Men Attending Sexual Health Clinics. Int. J. STD AIDS 2017, 28, 362–366. [Google Scholar] [CrossRef] [PubMed]
- Pakianathan, M.; Whittaker, W.; Lee, M.J.; Avery, J.; Green, S.; Nathan, B.; Hegazi, A. Chemsex and New HIV Diagnosis in Gay, Bisexual and Other Men Who Have Sex with Men Attending Sexual Health Clinics. HIV Med. 2018, 19, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Drückler, S.; Van Rooijen, M.S.; De Vries, H.J.C. Chemsex among Men Who Have Sex with Men: A Sexualized Drug Use Survey among Clients of the Sexually Transmitted Infection Outpatient Clinic and Users of a Gay Dating App in Amsterdam, the Netherlands. Sex. Transm. Dis. 2018, 45, 325–331. [Google Scholar] [CrossRef]

| Study | N Sample Size | GHB/GBL | Ketamine | Mephedrone | Crystal Meth | Other Drugs * |
|---|---|---|---|---|---|---|
| Rosinska et al., 2018 [28] | 4266 | ● | ● | ● | ● | |
| Glynn et al., 2018 [29] | 486 | ● | ● | ● | ● | α |
| Evers et al., 2019 [30] | 250 | ● | ● | ● | ● | β |
| Achterbergh et al., 2020 [31] | 4461 | ● | ● | ● | ● | γ |
| Curtis et al., 2020 [32] | 1644 | ● | ● | ● | ||
| Guerras et al., 2020 [33] | 9407 | ● | ● | ● | ||
| García-Pérez et al., 2022 [34] | 514 | ● | ● | ● | ● | δ |
| Guerras et al., 2022 [35] | 2883 | ● | ● | ● |
| Rosinska et al., 2018 [28] | Glynn et al., 2018 [29] | Evers et al., 2019 [30] | Achterbergh et al., 2020 [31] | Curtis et al., 2020 [32] | Guerras et al., 2020 [33] | García-Pérez et al., 2022 [34] | Guerras et al., 2022 [35] | |
|---|---|---|---|---|---|---|---|---|
| PS | OR. 1.8 | aPR 3.5 | ||||||
| CAI | OR 1.55 | 52% | 66.8% | aPR 1.11 | OR 6.5 | 46% | aPR1.7 | |
| CAR | 56% | |||||||
| HNP | OR 7.4 | OR 2.4 | OR 2.92 | Median 8 vs. 5 | aPR 2.11 | OR 1.6 | Median 33 vs. 15 | aPR1.5 |
| SG | 32% | OR. 9.8 | ||||||
| CS | 19% | aPR 1.43 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Coronado-Muñoz, M.; García-Cabrera, E.; Quintero-Flórez, A.; Román, E.; Vilches-Arenas, Á. Sexualized Drug Use and Chemsex among Men Who Have Sex with Men in Europe: A Systematic Review and Meta-Analysis. J. Clin. Med. 2024, 13, 1812. https://doi.org/10.3390/jcm13061812
Coronado-Muñoz M, García-Cabrera E, Quintero-Flórez A, Román E, Vilches-Arenas Á. Sexualized Drug Use and Chemsex among Men Who Have Sex with Men in Europe: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2024; 13(6):1812. https://doi.org/10.3390/jcm13061812
Chicago/Turabian StyleCoronado-Muñoz, Marina, Emilio García-Cabrera, Angélica Quintero-Flórez, Encarnación Román, and Ángel Vilches-Arenas. 2024. "Sexualized Drug Use and Chemsex among Men Who Have Sex with Men in Europe: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 13, no. 6: 1812. https://doi.org/10.3390/jcm13061812
APA StyleCoronado-Muñoz, M., García-Cabrera, E., Quintero-Flórez, A., Román, E., & Vilches-Arenas, Á. (2024). Sexualized Drug Use and Chemsex among Men Who Have Sex with Men in Europe: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 13(6), 1812. https://doi.org/10.3390/jcm13061812