The Complete Anatomy of the Anterior Ethmoidal Artery: A Meta-Analysis with Implications for Sinus and Skull Base Surgery
Abstract
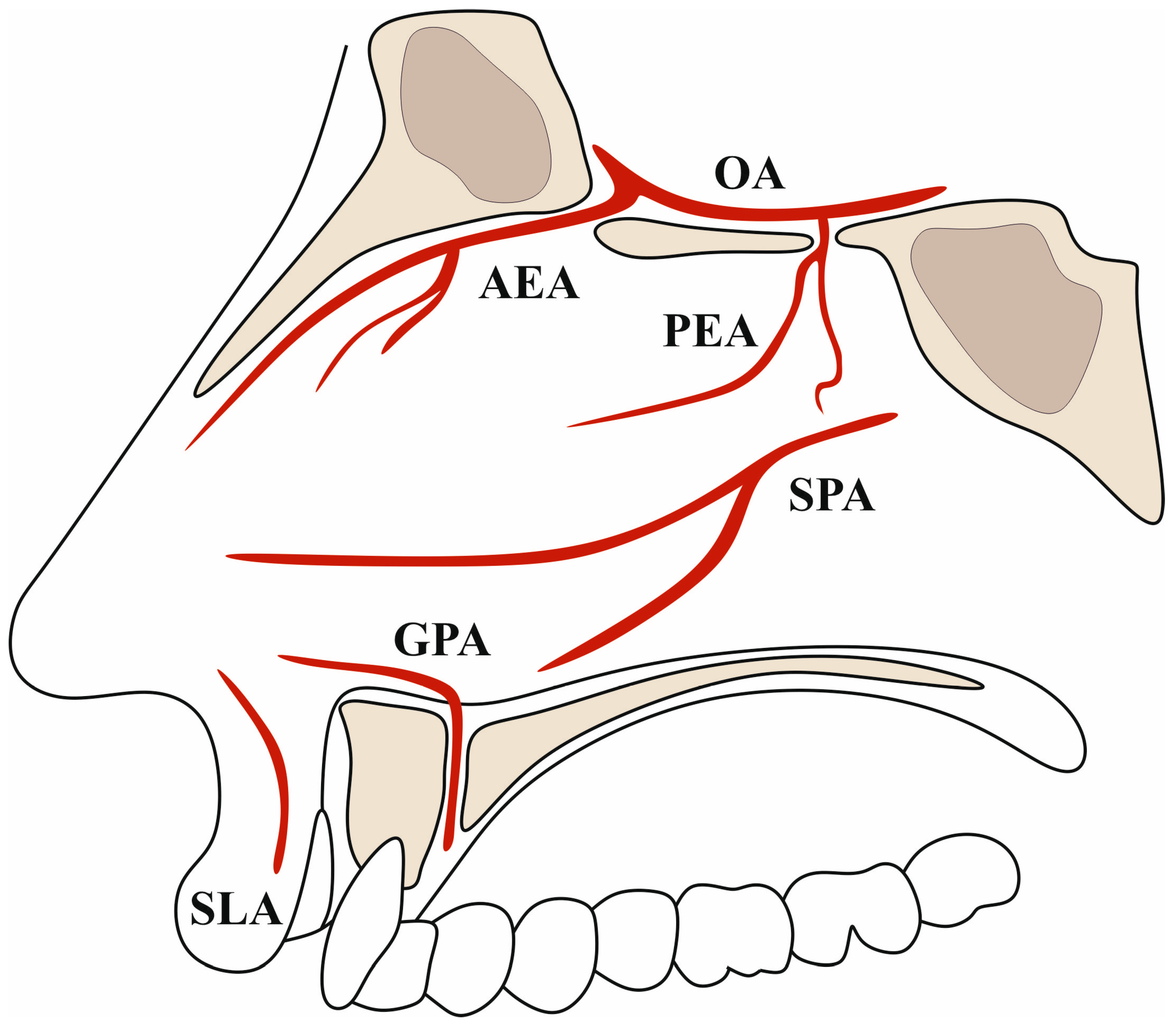
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Assessment and Data Extraction
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pollock, J.A.; Newton, T.H. The Anterior Falx Artery: Normal and Pathologic Anatomy. Radiology 1968, 91, 1089–1095. [Google Scholar] [CrossRef]
- Pamir, M.N.; Black, P.M.; Fahlbusch, R. Meningiomas; Elsevier: Amsterdam, The Netherlands, 2010. [Google Scholar]
- Mpolokeng, K.S.; Louw, G.J. An Unusual Arrangement of the Neurovascular Structures in One Ethmoidal Foramen of the Human Orbit. Transl. Res. Anat. 2020, 18, 100058. [Google Scholar] [CrossRef]
- El-Anwar, M.W.; Khazbak, A.O.; Eldib, D.B.; Algazzar, H.Y. Anterior Ethmoidal Artery: A Computed Tomography Analysis and New Classifications. J. Neurol. Surg. B Skull Base 2021, 82, e259–e267. [Google Scholar] [CrossRef]
- Ko, Y.-B.; Kim, M.-G.; Jung, Y.G. The Anatomical Relationship between the Anterior Ethmoid Artery, Frontal Sinus, and Intervening Air Cells; Can the Artery Be Useful Landmark? Korean J. Otorhinolaryngol.-Head Neck Surg. 2014, 57, 687–691. [Google Scholar]
- Lannoy-Penisson, L.; Schultz, P.; Riehm, S.; Atallah, I.; Veillon, F.; Debry, C. The Anterior Ethmoidal Artery: Radio-Anatomical Comparison and Its Application in Endonasal Surgery. Acta Otolaryngol. 2007, 127, 618–622. [Google Scholar] [CrossRef]
- Abdullah, B.; Lim, E.H.; Mohamad, H.; Husain, S.; Aziz, M.E.; Snidvongs, K.; Wang, D.Y.; Musa, K.I. Anatomical Variations of Anterior Ethmoidal Artery at the Ethmoidal Roof and Anterior Skull Base in Asians. Surg. Radiol. Anat. 2019, 41, 543–550. [Google Scholar] [CrossRef]
- Filho, B.C.A.; Weber, R.; Neto, C.D.P.; Lessa, M.M.; Voegels, R.L.; Butugan, O. Endoscopic Anatomy of the Anterior Ethmoidal Artery: A Cadaveric Dissection Study. Braz. J. Otorhinolaryngol. 2006, 72, 303–308. [Google Scholar] [CrossRef]
- Başak, S.; Karaman, C.Z.; Akdilli, A.; Mutlu, C.; Odabaşi, O.; Erpek, G. Evaluation of Some Important Anatomical Variations and Dangerous Areas of the Paranasal Sinuses by CT for Safer Endonasal Surgery. Rhinology 1998, 36, 162–167. [Google Scholar] [PubMed]
- Simmen, D.; Raghavan, U.; Briner, H.; Manestar, M.; Schuknecht, B.; Groscurth, P.; Jones, N. The Surgeon’s View of the Anterior Ethmoid Artery. Clin. Otolaryngol. 2006, 31, 187–191. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Lu, Q.; Liao, J.; Dang, R. Morphological Characteristics of the Anterior Ethmoidal Artery in Ethmoid Roof and Endoscopic Localization. Skull Base 2009, 19, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Monjas-Cánovas, I.; García-Garrigós, E.; Arenas-Jiménez, J.J.; Abarca-Olivas, J.; Sánchez-Del Campo, F.; Gras-Albert, J.R. Anatomía Radiológica de Las Arterias Etmoidales: Estudio Por TC En Cadáver. Acta Otorrinolaringol. Esp. 2011, 62, 367–374. [Google Scholar] [CrossRef]
- Han, J.K.; Becker, S.S.; Bomeli, S.R.; Gross, C.W. Endoscopic Localization of the Anterior and Posterior Ethmoid Arteries. Ann. Otol. Rhinol. Laryngol. 2008, 117, 931–935. [Google Scholar] [CrossRef]
- Patel, T.A.; Lubbe, D. How We Do It: Using the Nasion as a Landmark for Identifying the Anterior Ethmoidal Artery. J. Laryngol. Otol. 2023, 137, 1054–1057. [Google Scholar] [CrossRef]
- Yaprak, F.; Coban, I.; Ozer, M.A.; Govsa, F. The Tortuous Coursea of the Anterior Ethmoidal Artery in the Orbit: A Cadaveric Study. Acta Otorrinolaringol. 2024. [Google Scholar] [CrossRef]
- Gupta, A.; Ghosh, S.; Roychoudhury, A. Radiological and Clinical Correlations of the Anterior Ethmoidal Artery in Functional Endoscopic Sinus Surgery. J. Laryngol. Otol. 2022, 136, 154–157. [Google Scholar] [CrossRef] [PubMed]
- D’Antoni, A.V.; Tubbs, R.S.; Patti, A.C.; Higgins, Q.M.; Tiburzi, H.; Battaglia, F. The Critical Appraisal Tool for Anatomical Meta-analysis: A Framework for Critically Appraising Anatomical Meta-analyses. Clin. Anat. 2022, 35, 323–331. [Google Scholar] [CrossRef] [PubMed]
- Tomaszewski, K.A.; Henry, B.M.; Kumar Ramakrishnan, P.; Roy, J.; Vikse, J.; Loukas, M.; Tubbs, R.S.; Walocha, J.A. Development of the Anatomical Quality Assurance (AQUA) Checklist: Guidelines for Reporting Original Anatomical Studies. Clin. Anat. 2017, 30, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Henry, B.M.; Tomaszewski, K.A.; Walocha, J.A. Methods of Evidence-Based Anatomy: A Guide to Conducting Systematic Reviews and Meta-Analysis of Anatomical Studies. Ann. Anat.-Anat. Anz. 2016, 205, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Joshi, A.A.; Shah, K.D.; Bradoo, R.A. Radiological Correlation between the Anterior Ethmoidal Artery and the Supraorbital Ethmoid Cell. Indian J. Otolaryngol. Head Neck Surg. 2010, 62, 299–303. [Google Scholar] [CrossRef] [PubMed]
- McDonald, S.E.; Robinson, P.J.; Nunez, D.A. Radiological Anatomy of the Anterior Ethmoidal Artery for Functional Endoscopic Sinus Surgery. J. Laryngol. Otol. 2008, 122, 264–267. [Google Scholar] [CrossRef]
- Moon, H.; Kim, H.; Lee, J.; Chung, I.H.; Yoon, J. Surgical Anatomy of the Anterior Ethmoidal Canal in Ethmoid Roof. Laryngoscope 2001, 111, 900–904. [Google Scholar] [CrossRef] [PubMed]
- Cankal, F.; Apaydin, N.; Acar, H.I.; Elhan, A.; Tekdemir, I.; Yurdakul, M.; Kaya, M.; Esmer, A.F. Evaluation of the Anterior and Posterior Ethmoidal Canal by Computed Tomography. Clin. Radiol. 2004, 59, 1034–1040. [Google Scholar] [CrossRef] [PubMed]
- Naidu, L.; Sibiya, L.A.; Aladeyelu, O.S.; Rennie, C.O. Anatomical Landmarks for Localisation of the Anterior Ethmoidal Artery: A Combined Radiological and Cadaveric (Endoscopic) Study. Surg. Radiol. Anat. 2023, 45, 545–554. [Google Scholar] [CrossRef] [PubMed]
- Zong, Y.; Li, X.; Jiang, Y.; Xu, J.; Li, J. Transnasal Approach to the Anterior Skull Base. J. Craniofacial Surg. 2014, 25, 1041–1043. [Google Scholar] [CrossRef] [PubMed]
- Umar, N.F.; Aziz, M.E.; Mat Lazim, N.; Abdullah, B. The Effects of Suprabullar Pneumatization on the Orientation of Its Surrounding Anatomical Structures Relevant to the Frontal Drainage Pathway. Diagnostics 2021, 12, 52. [Google Scholar] [CrossRef] [PubMed]
- Takeda, T.; Kajiwara, R.; Omura, K.; Otori, N.; Wada, K. Analysis of Anatomical Variation of the Inclination of Lamellas Attached to the Skull Base and Its Correlation with the Anterior Ethmoidal Artery Floating in the Ethmoid Sinus for Use in Endoscopic Sinus Surgery. Surg. Radiol. Anat. 2020, 42, 995–1002. [Google Scholar] [CrossRef] [PubMed]
- Taha, M.A.; Hall, C.A.; Zylicz, H.E.; Westbrook, M.B.; Barham, W.T.; Stevenson, M.M.; Zito, B.A.; Barham, H.P. Variability of the Anterior Ethmoid Artery in Endoscopic Sinus Surgery. Ear Nose Throat J. 2022, 101, 268–273. [Google Scholar] [CrossRef]
- Song, M.; Zong, X.; Wang, X.; Pei, A.; Zhao, P.; Gui, S.; Yan, Y.; Zhang, Y. Anatomic Study of the Anterior Skull Base via an Endoscopic Transnasal Approach. Clin. Neurol. Neurosurg. 2011, 113, 281–284. [Google Scholar] [CrossRef]
- Solares, C.A.; Luong, A.; Batra, P.S. Technical Feasibility of Transnasal Endoscopic Anterior Ethmoid Artery Ligation: Assessment with Intraoperative Ct Imaging. Am. J. Rhinol. Allergy 2009, 23, 619–621. [Google Scholar] [CrossRef]
- Pernas, F.G.; Coughlin, A.M.; Hughes, S.E.; Riascos, R.; Maeso, P.A. A Novel Use of a Landmark to Avoid Injury of the Anterior Ethmoidal Artery during Endoscopic Sinus Surgery. Am. J. Rhinol. Allergy 2011, 25, 54–57. [Google Scholar] [CrossRef]
- Mason, E.; Solares, C.; Carrau, R.; Figueroa, R. Computed Tomographic Exploration of the Middle Ethmoidal Artery. J. Neurol. Surg. B Skull Base 2015, 76, 372–378. [Google Scholar] [CrossRef]
- Bortoli, V.; Martins, R.; Negri, K. Study of Anthropometric Measurements of the Anterior Ethmoidal Artery Using Three-Dimensional Scanning on 300 Patients. Int. Arch. Otorhinolaryngol. 2017, 21, 115–121. [Google Scholar] [CrossRef] [PubMed]
- Lemos-Rodriguez, A.M.; Farzal, Z.; Overton, L.J.; Rawal, R.B.; Eftekhari, K.; Sasaki-Adams, D.; Ewend, M.; Thorp, B.D.; Ebert, C.S.; Zanation, A.M. Analysis of Anterior and Posterior Maneuvers to Enhance Intraconal Exposure. Int. Forum Allergy Rhinol. 2019, 9, 556–561. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.C.; Ming Ku, P.K.; van Hasselt, C.A. New Guidelines for Endoscopic Localization of the Anterior Ethmoidal Artery: A Cadaveric Study. Laryngoscope 2000, 110, 1173–1178. [Google Scholar] [CrossRef] [PubMed]
- Kirchner, J.A.; Yanagisawa, E.; Crelin, E.S. Surgical Anatomy of the Ethmoidal Arteries: A Laboratory Study of 150 Orbits. Arch. Otolaryngol.-Head Neck Surg. 1961, 74, 382–386. [Google Scholar] [CrossRef]
- Kilinc, M.C.; Basak, H.; Çoruh, A.G.; Mutlu, M.; Guler, T.M.; Beton, S.; Comert, A.; Kahilogullari, G. Endoscopic Anatomy and a Safe Surgical Corridor to the Anterior Skull Base. World Neurosurg. 2021, 145, e83–e89. [Google Scholar] [CrossRef]
- Kho, J.P.Y.; Tang, I.P.; Tan, K.S.; Koa, A.J.; Prepageran, N.; Rajagopalan, R. Radiological Study of the Ethmoidal Arteries in the Nasal Cavity and Its Pertinence to the Endoscopic Surgeon. Indian J. Otolaryngol. Head Neck Surg. 2019, 71, 1994–1999. [Google Scholar] [CrossRef] [PubMed]
- Jang, D.W.; Lachanas, V.A.; White, L.C.; Kountakis, S.E. Supraorbital Ethmoid Cell: A Consistent Landmark for Endoscopic Identification of the Anterior Ethmoidal Artery. Otolaryngol.-Head Neck Surg. 2014, 151, 1073–1077. [Google Scholar] [CrossRef]
- Hamour, A.F.; Kus, L.; Monteiro, E.; Scheffler, P.; Lee, J.; Vescan, A. Radiological Anatomy of the Olfactory Fossa: Is Skull Base Anatomy Really Ever “Safe”? J. Neurol. Surg. B Skull Base 2022, 83, 053–058. [Google Scholar] [CrossRef]
- Güldner, C.; Diogo, I.; Windfuhr, J.; Bien, S.; Teymoortash, A.; Werner, J.A.; Bremke, M. Analysis of the Fossa Olfactoria Using Cone Beam Tomography (CBT). Acta Otolaryngol. 2011, 131, 72–78. [Google Scholar] [CrossRef]
- Floreani, S.R.; Nair, S.B.; Switajewski, M.C.; Wormald, P. Endoscopic Anterior Ethmoidal Artery Ligation: A Cadaver Study. Laryngoscope 2006, 116, 1263–1267. [Google Scholar] [CrossRef]
- Ferrari, M.; Pianta, L.; Borghesi, A.; Schreiber, A.; Ravanelli, M.; Mattavelli, D.; Rampinelli, V.; Belotti, F.; Rodella, L.F.; Maroldi, R.; et al. The Ethmoidal Arteries: A Cadaveric Study Based on Cone Beam Computed Tomography and Endoscopic Dissection. Surg. Radiol. Anat. 2017, 39, 991–998. [Google Scholar] [CrossRef]
- Fadda, G.L.; Petrelli, A.; Martino, F.; Succo, G.; Castelnuovo, P.; Bignami, M.; Cavallo, G. Anatomic Variations of Ethmoid Roof and Risk of Skull Base Injury in Endoscopic Sinus Surgery: Statistical Correlations. Am. J. Rhinol. Allergy 2021, 35, 871–878. [Google Scholar] [CrossRef] [PubMed]
- Eren, E.; Altay, C.; Arslanoğlu, S.; Erdoğan, N.K.; Uluç, M.E.; Önal, K.; Katılmiş, H. Searching for the Cheese: Does Ethmoid Pneumatization Affect the Location of the Anterior Ethmoid Artery? Eur. Arch. Oto-Rhino-Laryngol. 2014, 271, 281–285. [Google Scholar] [CrossRef]
- Erdogmus, S.; Govsa, F. The Anatomic Landmarks of Ethmoidal Arteries for the Surgical Approaches. J. Craniofacial Surg. 2006, 17, 280–285. [Google Scholar] [CrossRef]
- Ducasse, A.; Delattre, J.F.; Segal, A.; Desphieux, J.L.; Flament, J.B. Anatomical Basis of the Surgical Approach to the Medial Wall of the Orbit. Anat. Clin. 1985, 7, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Caklili, M.; Emengen, A.; Cabuk, B.; Anik, I.; Ceylan, S. Endoscopic Transorbital Approach to the Cavernous Sinus Lateral Compartment (Anatomical Cadaver Study). Turk. Neurosurg. 2021, 31, 813–819. [Google Scholar] [CrossRef]
- Abuzayed, B.; Tanriover, N.; Gazioglu, N.; Sanus, G.Z.; Ozlen, F.; Biceroglu, H.; Kafadar, A.M.; Eraslan, B.S.; Akar, Z. Endoscopic Endonasal Anatomy and Approaches to the Anterior Skull Base. J. Craniofacial Surg. 2010, 21, 529–537. [Google Scholar] [CrossRef] [PubMed]
- Henry, B.M.; Vikse, J.; Pekala, P.; Loukas, M.; Tubbs, R.S.; Walocha, J.A.; Jones, D.G.; Tomaszewski, K.A. Consensus Guidelines for the Uniform Reporting of Study Ethics in Anatomical Research within the Framework of the Anatomical Quality Assurance (AQUA) Checklist. Clin. Anat. 2018, 31, 521–524. [Google Scholar] [CrossRef]
- Abdullah, B.; Lim, E.H.; Husain, S.; Snidvongs, K.; Wang, D.Y. Anatomical Variations of Anterior Ethmoidal Artery and Their Significance in Endoscopic Sinus Surgery: A Systematic Review. Surg. Radiol. Anat. 2019, 41, 491–499. [Google Scholar] [CrossRef]
- Aytaç, I.; Tunç, O.; Yazici, A.; Başaran, A.; Gönüldaş, B.; Mumbuç, L.S. Anterior Skull Base Surgery via Endoscopic Endonasal Approach: Outcomes and Analysis. J. Craniofacial Surg. 2021, 32, 1664–1667. [Google Scholar] [CrossRef]
- Cecchini, G. Anterior and Posterior Ethmoidal Artery Ligation in Anterior Skull Base Meningiomas: A Review on Microsurgical Approaches. World Neurosurg. 2015, 84, 1161–1165. [Google Scholar] [CrossRef]
- Aref, M.; Kunigelis, K.E.; Yang, A.; Subramanian, P.S.; Ramakrishnan, V.R.; Youssef, A.S. The Effect of Preoperative Direct Ligation of Ethmoidal Arteries on the Perioperative Outcomes of Large Anterior Skull Base Meningiomas Surgery: A Clinical Study. World Neurosurg. 2018, 120, e776–e782. [Google Scholar] [CrossRef]
- Snyderman, C.H.; Carrau, R.L. Epistaxis. In Operative Otolaryngology: Head and Neck Surgery; Elsevier: Amsterdam, The Netherlands, 2008; pp. 7–16. [Google Scholar]
- Wysiadecki, G.; Varga, I.; Klejbor, I.; Balawender, K.; Ghosh, S.K.; Clarke, E.; Koziej, M.; Bonczar, M.; Ostrowski, P.; Żytkowski, A. Reporting Anatomical Variations: Should Unified Standards and Protocol (Checklist) for Anatomical Studies and Case Reports Be Established? Transl. Res. Anat. 2024, 35, 100284. [Google Scholar] [CrossRef]



| First Author | Year of Publication | Continent | Country | Method | Arteries Studied |
|---|---|---|---|---|---|
| Livashin Naidu [24] | 2023 | Africa | South Africa | CT + Cadavers | 126 |
| Nikma Fadlati Umar [26] | 2022 | Asia | Malaysia | CT | 370 |
| Melih Caklili [48] | 2021 | Asia | Turkey | Cadavers | 6 |
| Gian Luca Fadda [44] | 2021 | Europe | Italy | CT | 440 |
| Amr F. Hamour [40] | 2020 | North America | Canada | CT | 60 |
| Mustafa Cemil Kilinc [37] | 2020 | Asia | Turkey | Cadavers + CT | 14 |
| Mohamed A. Taha [28] | 2020 | North America | USA | CT | 100 |
| Teppei Takeda [27] | 2020 | Asia | Japan | CT | 366 |
| Mohammad Waheed El-Anwar [4] | 2019 | Africa/Asia | Egypt | CT | 300 |
| Baharudin Abdullah [51] | 2018 | Asia | Malaysia | CT | 252 |
| Jasmine P. Y. Kho [38] | 2018 | Asia | Malaysia | CT | 108 |
| Ana M. Lemos-Rodriguez [34] | 2018 | North America | USA | Cadavers | 8 |
| Marco Ferrari [43] | 2017 | Europe | Italy | Cadavers | 28 |
| Vinicius Tomadon Bortoli [33] | 2017 | South America | Brazil | CT | 600 |
| Eric Mason [32] | 2015 | North America | USA | CT | 100 |
| David W. Jang [39] | 2014 | North America | USA | CT | 78 |
| Young-Bum Ko [5] | 2014 | Asia | South Korea | CT | 119 |
| Yu Zong [25] | 2014 | Asia | China | Cadavers | 16 |
| Erdem Eren [45] | 2013 | Asia | Turkey | CT | 298 |
| Christian Güldner [41] | 2011 | Europe | Germany | CT | 282 |
| Francisco G. Pernas [31] | 2011 | North America | USA | CT | 138 |
| Ming Song [29] | 2011 | Asia | China | Cadavers | 20 |
| Anagha A. Joshi [20] | 2010 | Asia | India | CT | 100 |
| Bashar Abuzayed [49] | 2009 | Asia | Turkey | Cadavers | 24 |
| C. Arturo Solares [30] | 2009 | North America | USA | CT | 8 |
| You-xiong Yang [11] | 2009 | Asia | China | Cadavers | 28 |
| S. E. McDonald [21] | 2008 | Europe | United Kingdom | CT | 42 |
| Senem Erdogmus [46] | 2006 | Asia | Turkey | Cadavers | 37 |
| Bernardo Cunha Araujo Filho [8] | 2006 | South America | Brazil | Cadavers | 48 |
| Stephen R. Floreani [42] | 2006 | Australia | Australia | CT | 44 |
| D. Simmen [10] | 2006 | Europe | Switzerland | Cadavers | 34 |
| L. Lannoy-Penisson [6] | 2006 | Europe | France | Cadavers + CT | 18 |
| Cankal F. [23] | 2004 | Europe | Turkey | CT | 150 |
| Hyoung-Jin Moon [22] | 2001 | Asia | Korea | Cadavers + CT | 70 |
| Wai Chung Lee [35] | 2000 | Asia | China | Cadavers | 56 |
| Sema Basak [9] | 1998 | Asia | Turkey | CT | 222 |
| A Ducasse [47] | 1985 | Europe | France | Cadavers | 70 |
| John A. Kirchner [36] | 1961 | North America | USA | Cadavers | 70 |
| Category | Mean | Standard Error | Variance | Lower Limit | Upper Limit | Z-Value | p-Value |
|---|---|---|---|---|---|---|---|
| Diameter | |||||||
| Mean diameter of the AEA in the intraorbital part [mm] | 0.94 | 0.05 | 0.00 | 0.85 | 1.04 | 19.52 | 0.00 |
| Mean diameter of AEA in the intracranial part [mm] | 0.76 | 0.03 | 0.00 | 0.70 | 0.81 | 28.44 | 0.00 |
| Length | |||||||
| Mean length of the AEA [mm] | 4.64 | 1.18 | 1.40 | 2.32 | 6.96 | 3.91 | 0.00 |
| Category | Pooled Prevalence | LCI | HCI | Q | I2 |
|---|---|---|---|---|---|
| Type of AEA according to its relationship with the anterior skull base | |||||
| AEA embedded within the skull base/AEA at the level of the skull base producing a bony protrusion (Type A/B) [Overall] | 56.91% | 43.55% | 69.80% | 217.47 | 94.94 |
| AEA coursing freely in the ethmoid sinus within a bony anterior ethmoidal canal while connected to the skull base by a thin bony mesentery (Type C) [Overall] | 43.09% | 30.20% | 56.45% | 217.47 | 94.94 |
| AEA embedded within the skull base/AEA at the level of the skull base producing a bony protrusion (Type A/B) [Computed Tomography] | 52.23% | 36.43% | 67.81% | 140.28 | 95.72 |
| AEA coursing freely in the ethmoid sinus within a bony anterior ethmoidal canal while connected to the skull base by a thin bony mesentery (Type C) [Computed Tomography] | 47.77% | 32.19% | 63.57% | 140.28 | 95.72 |
| AEA embedded within the skull base/AEA at the level of the skull base producing a bony protrusion (Type A/B) [Cadavers] | 64.35% | 37.00% | 87.85% | 53.84 | 92.57 |
| AEA coursing freely in the ethmoid sinus within a bony anterior ethmoidal canal while connected to the skull base by a thin bony mesentery (Type C) [Cadavers] | 35.65% | 12.15% | 63.00% | 53.84 | 92.57 |
| Category | Pooled Prevalence | LCI | HCI | Q | I2 | ||
|---|---|---|---|---|---|---|---|
| Localization of the AEA | |||||||
| AEA between the second and third lamellae | 65.82% | 55.39% | 75.56% | 7.70 | 87.01 | ||
| AEA between the first and second lamellae | 14.87% | 0.00% | 38.08% | 53.17 | 98.12 | ||
| AEA in the second lamella | 4.95% | 0.00% | 30.07% | 100.78 | 99.01 | ||
| AEA in the third lamella | 4.09% | 0.00% | 24.31% | 80.51 | 98.76 | ||
| AEA beyond the third lamella | 1.74% | 0.49% | 3.64% | 2.31 | 56.78 | ||
| AEA within the posterior margin of the frontal sinus ostium | 1.25% | 0.00% | 3.35% | 4.45 | 77.52 | ||
| Category | Mean | Standard Error | Variance | Lower Limit | Upper Limit | Z-Value | p-Value |
| Distance between the AEA and nearby anatomical landmarks | |||||||
| Distance between AEA and skull base [mm] | 1.76 | 0.17 | 0.03 | 1.43 | 2.09 | 10.42 | 0.00 |
| Distance between AEA and inferior turbinate [mm] | 30.86 | 0.75 | 0.56 | 29.39 | 32.33 | 41.14 | 0.00 |
| Distance between AEA and middle turbinate [mm] | 20.98 | 0.27 | 0.07 | 20.45 | 21.50 | 78.50 | 0.00 |
| Distance between AEA and columella [mm] | 63.56 | 0.41 | 0.17 | 62.76 | 64.36 | 155.14 | 0.00 |
| Distance between AEA and nasofrontal beak [mm] | 11.60 | 5.26 | 27.68 | 1.29 | 21.91 | 2.20 | 0.03 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Szczepanek, E.; Toppich, J.; Ostrowski, P.; Bonczar, M.; Nasser, A.; Dziedzic, M.; Walocha, J.; Koziej, M. The Complete Anatomy of the Anterior Ethmoidal Artery: A Meta-Analysis with Implications for Sinus and Skull Base Surgery. J. Clin. Med. 2024, 13, 1695. https://doi.org/10.3390/jcm13061695
Szczepanek E, Toppich J, Ostrowski P, Bonczar M, Nasser A, Dziedzic M, Walocha J, Koziej M. The Complete Anatomy of the Anterior Ethmoidal Artery: A Meta-Analysis with Implications for Sinus and Skull Base Surgery. Journal of Clinical Medicine. 2024; 13(6):1695. https://doi.org/10.3390/jcm13061695
Chicago/Turabian StyleSzczepanek, Elżbieta, Julia Toppich, Patryk Ostrowski, Michał Bonczar, Ameen Nasser, Martyna Dziedzic, Jerzy Walocha, and Mateusz Koziej. 2024. "The Complete Anatomy of the Anterior Ethmoidal Artery: A Meta-Analysis with Implications for Sinus and Skull Base Surgery" Journal of Clinical Medicine 13, no. 6: 1695. https://doi.org/10.3390/jcm13061695
APA StyleSzczepanek, E., Toppich, J., Ostrowski, P., Bonczar, M., Nasser, A., Dziedzic, M., Walocha, J., & Koziej, M. (2024). The Complete Anatomy of the Anterior Ethmoidal Artery: A Meta-Analysis with Implications for Sinus and Skull Base Surgery. Journal of Clinical Medicine, 13(6), 1695. https://doi.org/10.3390/jcm13061695






