The Influence of Temporary Epiphysiodesis of the Proximal End of the Tibia on the Shape of the Knee Joint in Children Treated for Leg Length Discrepancy
Abstract
1. Introduction
2. Materials and Methods
2.1. Selection of Participants
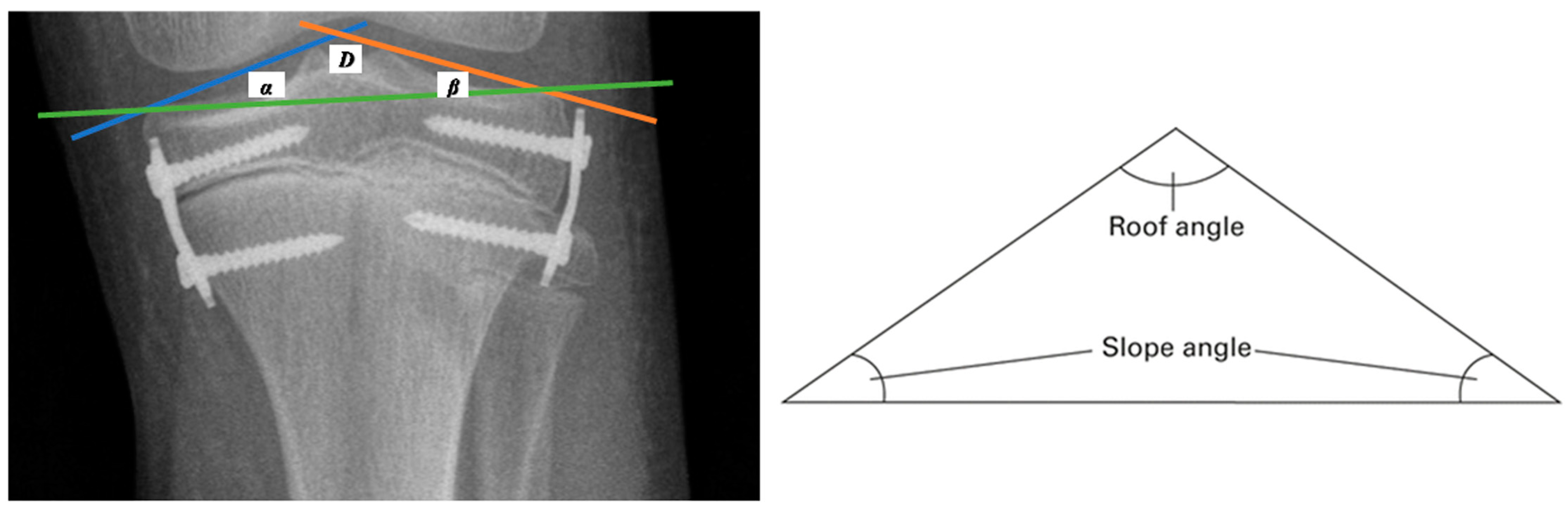
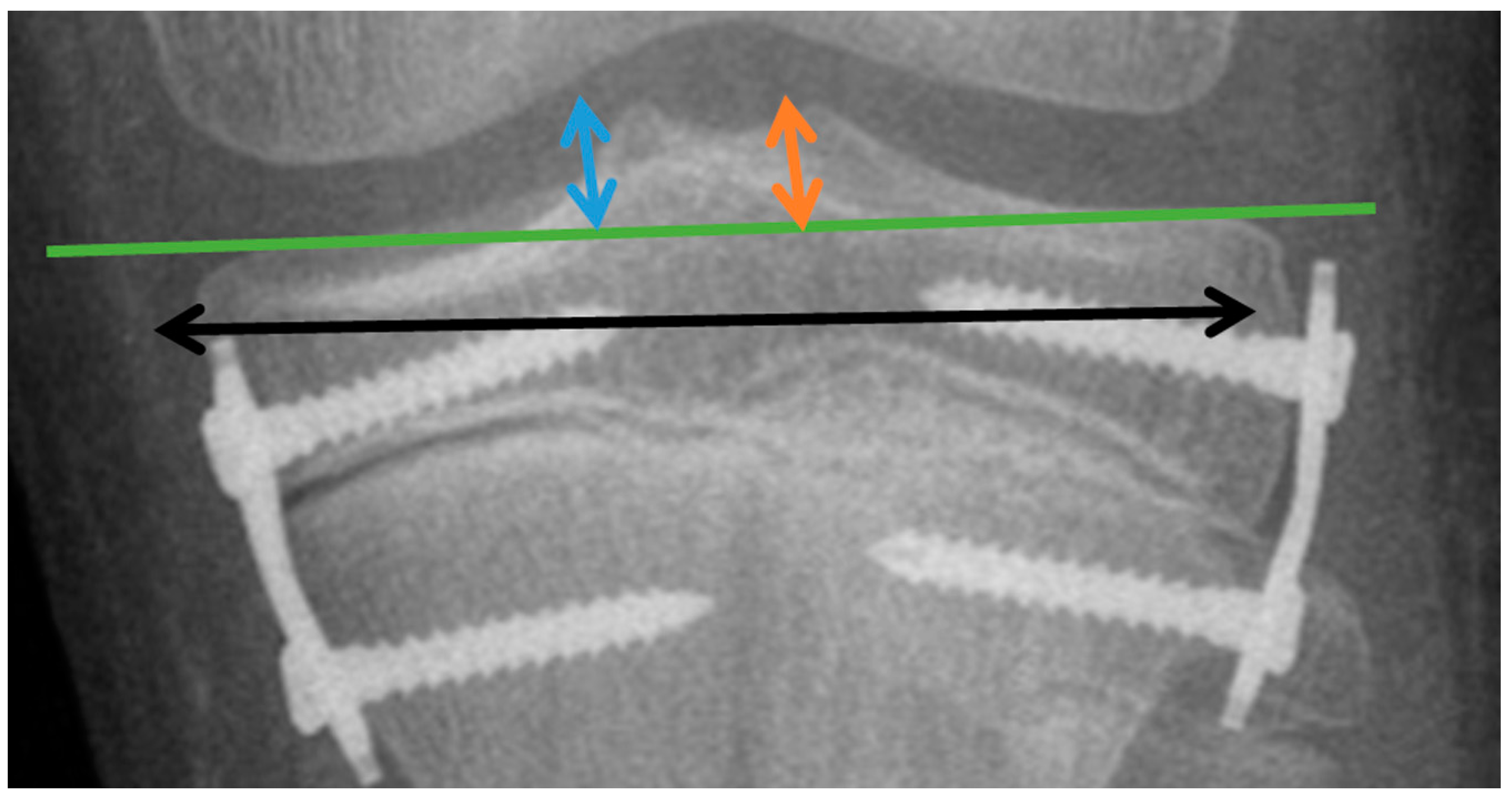
2.2. Study Design
2.3. Statistical Analysis
3. Results
3.1. Changes in the Investigated Parameters Evaluated after the Completion of the Treatment
3.2. Changes in the Investigated Parameters Evaluated Every Six Months during the Treatment
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Baylis, W.J.; Rzonca, E.C. Functional and Structural Limb Length Discrepancies: Evaluation and Treatment. Clin. Podiatr. Med. Surg. 1988, 5, 509–520. [Google Scholar] [CrossRef] [PubMed]
- Danbert, R.J. Clinical Assessment and Treatment of Leg Length Inequalities. J. Manip. Physiol. Ther. 1988, 11, 290–295. [Google Scholar]
- Walsh, M.; Connolly, P.; Jenkinson, A.; O’Brien, T. Leg Length Discrepancy—An Experimental Study of Compensatory Changes in Three Dimensions Using Gait Analysis. Gait Posture 2000, 12, 156–161. [Google Scholar] [CrossRef] [PubMed]
- Paley, J.; Talor, J.; Levin, A.; Bhave, A.; Paley, D.; Herzenberg, J.E. The Multiplier Method for Prediction of Adult Height. J. Pediatr. Orthop. 2004, 24, 732–737. [Google Scholar] [CrossRef]
- Birch, J.G.; Samchukov, M.L. Use of the Ilizarov Method to Correct Lower Limb Deformities in Children and Adolescents. J. Am. Acad. Orthop. Surg. 2004, 12, 144–154. [Google Scholar] [CrossRef]
- Stevens, P.M. Guided Growth for Angular Correction: A Preliminary Series Using a Tension Band Plate. J. Pediatr. Orthop. 2007, 27, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Sinha, R.; Weigl, D.; Mercado, E.; Becker, T.; Kedem, P.; Bar-On, E. Eight-Plate Epiphysiodesis: Are We Creating an Intra-Articular Deformity? Bone Jt. J. 2018, 100-B, 1112–1116. [Google Scholar] [CrossRef]
- Raab, P.; Wild, A.; Seller, K.; Krauspe, R. Correction of Length Discrepancies and Angular Deformities of the Leg by Blount’s Epiphyseal Stapling. Eur. J. Pediatr. 2001, 160, 668–674. [Google Scholar] [CrossRef]
- Courvoisier, A.; Eid, A.; Merloz, P. Epiphyseal Stapling of the Proximal Tibia for Idiopathic Genu Valgum. J. Child. Orthop. 2009, 3, 217–221. [Google Scholar] [CrossRef]
- Vogt, B.; Tretow, H.; Schuhknecht, B.; Horter, M.; Schiedel, F.; Rödl, R. Coronal and Sagittal Axis Deviation Following Temporary Epiphysiodesis Using Blount-Staple or Eight-Plate for Treatment of Leg Length Discrepancy. Arch. Orthop. Trauma. Surg. 2014, 134, 421–447. [Google Scholar]
- Blount, W.P.; Clarke, G.R. Control of Bone Growth by Epiphyseal Stapling; a Preliminary Report. J. Bone Joint Surg. Am. 1949, 31A, 464–478. [Google Scholar] [CrossRef]
- Gorman, T.M.; Vanderwerff, R.; Pond, M.; MacWilliams, B.; Santora, S.D. Mechanical Axis Following Staple Epiphysiodesis for Limb-Length Inequality. J. Bone Jt. Surg.-Am. Vol. 2009, 91, 2430–2439. [Google Scholar] [CrossRef]
- Schroerlucke, S.; Bertrand, S.; Clapp, J.; Bundy, J.; Gregg, F.O. Failure of Orthofix Eight-Plate for the Treatment of Blount Disease. J. Pediatr. Orthop. 2009, 29, 57–60. [Google Scholar] [CrossRef]
- Wiemann, J.M.; Tryon, C.; Szalay, E.A. Physeal Stapling Versus 8-Plate Hemiepiphysiodesis for Guided Correction of Angular Deformity about the Knee. J. Pediatr. Orthop. 2009, 29, 481–485. [Google Scholar] [CrossRef] [PubMed]
- Métaizeau, J.P.; Wong-Chung, J.; Bertrand, H.; Pasquier, P. Percutaneous Epiphysiodesis Using Transphyseal Screws (PETS). J. Pediatr. Orthop. 1998, 18, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Ballal, M.S.; Bruce, C.E.; Nayagam, S. Correcting Genu Varum and Genu Valgum in Children by Guided Growth: TEMPORARY HEMIEPIPHYSIODESIS USING TENSION BAND PLATES. J. Bone Jt. Surg. Br. 2010, 92-B, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Burghardt, R.D.; Herzenberg, J.E.; Standard, S.C.; Paley, D. Temporary Hemiepiphyseal Arrest Using a Screw and Plate Device to Treat Knee and Ankle Deformities in Children: A Preliminary Report. J. Child. Orthop. 2008, 2, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Gaumétou, E.; Mallet, C.; Souchet, P.; Mazda, K.; Ilharreborde, B. Poor Efficiency of Eight-Plates in the Treatment of Lower Limb Discrepancy. J. Pediatr. Orthop. 2016, 36, 715–719. [Google Scholar] [CrossRef]
- Gottliebsen, M.; Møller-Madsen, B.; Stødkilde-Jørgensen, H.; Rahbek, O. Controlled Longitudinal Bone Growth by Temporary Tension Band Plating: An Experimental Study. Bone Jt. J. 2013, 95-B, 855–860. [Google Scholar] [CrossRef] [PubMed]
- Lauge-Pedersen, H.; Hägglund, G. Eight Plate Should Not Be Used for Treating Leg Length Discrepancy. J. Child. Orthop. 2013, 7, 285–288. [Google Scholar] [CrossRef] [PubMed]
- Borbas, P.; Agten, C.A.; Rosskopf, A.B.; Hingsammer, A.; Eid, K.; Ramseier, L.E. Guided Growth with Tension Band Plate or Definitive Epiphysiodesis for Treatment of Limb Length Discrepancy? J. Orthop. Surg. 2019, 14, 99. [Google Scholar] [CrossRef]
- Karbowski, A.; Camps, L.; Matthia, H.H. Histopathological Features of Unilateral Stapling in Animal Experiments. Arch. Orthop. Trauma Surg. 1989, 108, 353–358. [Google Scholar] [CrossRef]
- Golightly, Y.M.; Allen, K.D.; Helmick, C.G.; Renner, J.B.; Jordan, J.M. Symptoms of the Knee and Hip in Individuals with and without Limb Length Inequality. Osteoarthr. Cartil. 2009, 17, 596–600. [Google Scholar] [CrossRef]
- Golightly, Y.M.; Allen, K.D.; Renner, J.B.; Helmick, C.G.; Salazar, A.; Jordan, J.M. Relationship of Limb Length Inequality with Radiographic Knee and Hip Osteoarthritis. Osteoarthr. Cartil. 2007, 15, 824–829. [Google Scholar] [CrossRef] [PubMed]
- Sanders, J.O.; Howell, J.; Qiu, X. Comparison of the Paley Method Using Chronological Age with Use of Skeletal Maturity for Predicting Mature Limb Length in Children. J. Bone Jt. Surg. 2011, 93, 1051–1056. [Google Scholar] [CrossRef]
- Gottliebsen, M.; Shiguetomi-Medina, J.M.; Rahbek, O.; Møller-Madsen, B. Guided Growth: Mechanism and Reversibility of Modulation. J. Child. Orthop. 2016, 10, 471–477. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.-C.; Kao, H.-K.; Yang, W.-E.; Chang, C.-H. Tension Band Plating Is Less Effective in Achieving Equalization of Leg Length. J. Child. Orthop. 2018, 12, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Bayhan, I.A.; Karatas, A.F.; Rogers, K.J.; Bowen, J.R.; Thacker, M.M. Comparing Percutaneous Physeal Epiphysiodesis and Eight-Plate Epiphysiodesis for the Treatment of Limb Length Discrepancy. J. Pediatr. Orthop. 2017, 37, 323–327. [Google Scholar] [CrossRef]




| Parameter | Group I | Group II | Group III |
|---|---|---|---|
| Duration of treatment (months) | 18 | 30 | 42 |
| Number/(boys/girls) | 24/(12/12) | 24/(18/6) | 12/(6/6) |
| Age y.m average/(range) | 13.2/(12.2–13.80) | 10.11/(10.2–11.11) | 9.0/(8.6–9.6) |
| Age y.m boys average/(range) | 13.0/(12.2–13.11) | 11.3/(10.7–11.11) | 9.2/(9.0–9.6) |
| Age y.m girls average/(range) | 13.3/(2.11–13.10) | 10.6/(10.2–10.11) | 8.11/(8.10–9.6) |
| LLD cm average/(range) | 2.0/(1.5–2.8) | 2.6/(1.4–3.6) | 2.4/(1.6–3.6) |
| LLD cm boys average/(range) | 2.1/(1.5–2.8) | 2.6/(1.5–2.8) | 2.5/(2.0–3.2) |
| LLD cm girls average/(range) | 2.0/(1.5–2.6) | 2.6/(1.4–3.6) | 2.4/(1.6–3.6) |
| Parameter | Group I (0–18 Months) | Group II (0–30 Months) | Group III (0–42 Months) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Girls | Boys | Total | Girls | Boys | Total | Girls | Boys | Total | |
| Δ D angle (degrees) | 6–16 (av. 9.5) | 1–15 (av. 8.9) | 1–16 (av. 9.1) | 8–9 (av. 8.3) | 9–15 (av. 12.0) | 8–15 (av. 10.2) | 8–9 (av. 8.6) | 6–14 (av. 10.3) | 8–14 (av. 9.4) |
| Δ α angle (degrees) | 1–8.9 (av. 4.9) | 5.1–6.8 (av. 7.3) | 1–8.9 (av. 5.1) | 1.9–2.2 (av. 2.0) | 6.3–9.6 (av. 8.3) | 1.9–9.6 (av. 5.15) | 2.8–7.4 (av. 4.3) | 5.7–8.9 (av. 7.3) | 2.8–7.4 (av. 5.8) |
| Δ β angle (degrees) | 1.5–16 (av. 6.25) | 0.5–2.7 (av. 1.9) | 0.5–16 (av. 4) | 3.2–3.6 (av. 3.4) | 1–7.1 (av. 3) | 1–7.1 (av. 3.2) | 6.1–8.8 (av. 7.9) | 3.9–6.1 (av. 5) | 3.9–8.8 (av. 6.45) |
| Δ MTH (mm) | 0.6–2.6 (av. 1.6) | 0.7–1.9 (av. 1.4) | 0.6–2.6 (av. 1.5) | 1.5–2.2 (av. 1.9) | 0.5–3.6 (av. 2.3) | 0.5–3.6 (av. 2.1) | 1.3–2.1 (av. 1.5) | 1.2–2.5 (av. 1.9) | 1.2–2.5 (av. 1.7) |
| Δ LTH (mm) | 2.4–4.7 (av. 2.4) | 0.7–1.7 (av. 1.2) | 0.7–4.7 (av. 3.6) | 2.6–3.8 (av. 3.4) | 0.3–3.8 (av. 2.4) | 0.3–3.8 (av. 2.9) | 0.3–2.1 (av. 0.9) | 2.1–3.6 (av. 2.8) | 0.3–3.6 (av. 1.8) |
| Δ TW (mm) | 0.3–17.7 (av. 6.6) | 1.8–13.3 (av. 9.4) | 0.3–17.7 (av. 8) | 0.9–1.1 (av. 1.0) | 1.4–5.7 (av. 1.8) | 0.9–5.7 (av. 1.4) | 1.6–9.9 (av. 4.3) | 9.9–12.2 (av. 11) | 1.6–12.2 (av. 7.6) |
| Parameter | G I (0–18 Months) | G II (0–30 Months) | G III (0–42 Months) | |||
|---|---|---|---|---|---|---|
| Girls | Boys | Girls | Boys | Girls | Boys | |
| D angle l | 0.0007 | 0.0102 | 0.0002 | 0.0001 | 0.0039 | 0.0039 |
| D angle k | 0.0004 | 0.0555 | 0.2709 | 0.6358 | 0.0277 | 0.5706 |
| α angle l | 0.2615 | 0.4079 | 0.5492 | 0.0001 | 0.4407 | 0.7419 |
| α angle k | 0.0011 | 0.4936 | 0.0795 | 0.6269 | 0.0609 | 0.6226 |
| β angle l | 0.0117 | 0.0776 | 0.6586 | 0.0007 | 0.0041 | 0.0206 |
| β angle k | 0.0005 | 0.6823 | 0.1617 | 0.0001 | 0.1311 | 0.9943 |
| MTH l | 0.0001 | 0.0001 | 0.0001 | 0.0001 | 0.00001 | 0.00001 |
| MTH k | 0.0103 | 0.4677 | 0.0245 | 0.0001 | 0.02707 | 0.2056 |
| LTH l | 0.0001 | 0.0001 | 0.0001 | 0.0001 | 0.0001 | 0.0001 |
| LTH k | 0.7839 | 0.5299 | 0.0291 | 0.0001 | 0.0001 | 0.8245 |
| TW l | 0.0001 | 0.0001 | 0.01231 | 0.0001 | 0.0001 | 0.0001 |
| TW k | 0.0001 | 0.0001 | 0.0001 | 0.0001 | 0.0001 | 0.0001 |
| Girls | Boys | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Period | D | α | β | MLH | LTH | TW | D | α | β | MLH | LTH | TW |
| 0–6 m | 0.0277 | 0.0281 | 0.9165 | 0.0125 | 0.0047 | 0.3078 | 0.4631 | 0.0022 | 0.0277 | 0.0022 | 0.0995 | 0.6379 |
| 6–12 m | 0.0277 | 0.0121 | 0.6002 | 0.0229 | 0.0229 | 0.0229 | 0.2489 | 0.0022 | 0.3454 | 0.6949 | 0.0281 | 0.1579 |
| 12–18 m | 0.0277 | 0.0121 | 0.4631 | 0.0022 | 0.0995 | 0.3078 | 0.0277 | 0.1579 | 0.6002 | 0.0229 | 0.0121 | 0.6379 |
| Girls | Boys | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Period | D | α | β | MLH | LTH | TW | D | α | β | MLH | LTH | TW |
| 0–6 m | 0.0678 | 0.1159 | 0.0277 | 0.9165 | 0.9165 | 0.0277 | 0.0707 | 0.0011 | 0.0096 | 0.0479 | 0.0002 | 0.0011 |
| 6–12 m | 0.0277 | 0.9165 | 0.0479 | 0.0277 | 0.0277 | 0.0277 | 0.0002 | 0.0096 | 0.0033 | 0.0018 | 0.7174 | 0.0151 |
| 12–18 m | 0.0277 | 0.0277 | 0.9165 | 0.0277 | 0.1158 | 0.9165 | 0.0011 | 0.6791 | 0.4204 | 0.0311 | 0.0014 | 0.4379 |
| 18–24 m | 0.0277 | 0.0277 | 0.1158 | 0.1797 | 0.0277 | 0.0277 | 0.2667 | 0.7771 | 0.0006 | 0.0049 | 0.0582 | 0.4459 |
| 24–30 m | 0.4652 | 0.0277 | 0.4631 | 0.0277 | 0.0277 | 0.0277 | 0.4459 | 0.0096 | 0.0057 | 0.0386 | 0.0084 | 0.0311 |
| Girls | Boys | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Period | D | α | β | MLH | LTH | TW | D | α | β | MLH | LTH | TW |
| 0–6 m | 0.1158 | 0.1158 | 0.0277 | 0.1158 | 0.0277 | 0.0277 | 0.1158 | 0.1158 | 0.9165 | 0.4631 | 0.4631 | 0.1158 |
| 6–12 m | 0.0678 | 0.0277 | 0.9165 | 0.0277 | 0.0277 | 0.0277 | 0.0678 | 0.9165 | 0.9165 | 0.4631 | 0.0277 | 0.9158 |
| 12–18 m | 0.0678 | 0.0277 | 0.0277 | 0.4631 | 0.9165 | 0.1158 | 0.0678 | 0.4631 | 0.0277 | 0.4631 | 0.4631 | 0.1158 |
| 18–24 m | 0.4652 | 0.0277 | 0.0277 | 0.0277 | 0.0277 | 0.9165 | 0.0678 | 0.9165 | 0.9165 | 0.0277 | 0.0277 | 0.1158 |
| 24–30 m | 0.0277 | 0.1158 | 0.0277 | 0.0277 | 0.0277 | 0.0277 | 0.1797 | 0.9165 | 0.9165 | 0.9165 | 0.4631 | 0.4631 |
| 30–36 m | 0.9165 | 0.9165 | 0.0277 | 0.0277 | 0.0277 | 0.0277 | 0.0277 | 0.9165 | 0.0277 | 0.4631 | 0.4631 | 0.1158 |
| 36–42 m | 0.1158 | 0.9165 | 0.0277 | 0.1158 | 0.1158 | 0.0277 | 0.1158 | 0.0277 | 0.9165 | 0.4652 | 0.1158 | 0.1277 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Starobrat, G.; Danielewicz, A.; Szponder, T.; Wójciak, M.; Sowa, I.; Różańska-Boczula, M.; Latalski, M. The Influence of Temporary Epiphysiodesis of the Proximal End of the Tibia on the Shape of the Knee Joint in Children Treated for Leg Length Discrepancy. J. Clin. Med. 2024, 13, 1458. https://doi.org/10.3390/jcm13051458
Starobrat G, Danielewicz A, Szponder T, Wójciak M, Sowa I, Różańska-Boczula M, Latalski M. The Influence of Temporary Epiphysiodesis of the Proximal End of the Tibia on the Shape of the Knee Joint in Children Treated for Leg Length Discrepancy. Journal of Clinical Medicine. 2024; 13(5):1458. https://doi.org/10.3390/jcm13051458
Chicago/Turabian StyleStarobrat, Grzegorz, Anna Danielewicz, Tomasz Szponder, Magdalena Wójciak, Ireneusz Sowa, Monika Różańska-Boczula, and Michał Latalski. 2024. "The Influence of Temporary Epiphysiodesis of the Proximal End of the Tibia on the Shape of the Knee Joint in Children Treated for Leg Length Discrepancy" Journal of Clinical Medicine 13, no. 5: 1458. https://doi.org/10.3390/jcm13051458
APA StyleStarobrat, G., Danielewicz, A., Szponder, T., Wójciak, M., Sowa, I., Różańska-Boczula, M., & Latalski, M. (2024). The Influence of Temporary Epiphysiodesis of the Proximal End of the Tibia on the Shape of the Knee Joint in Children Treated for Leg Length Discrepancy. Journal of Clinical Medicine, 13(5), 1458. https://doi.org/10.3390/jcm13051458








