Hydrotherapy after Rotator Cuff Repair Improves Short-Term Functional Results Compared with Land-Based Rehabilitation When the Immobilization Period Is Longer
Abstract
1. Introduction
2. Materials and Methods
2.1. Pre- and Post-Operative Clinical Assessment
2.2. Surgical Procedure
2.3. Rehabilitation Protocol
2.4. Statistical Analyses
3. Results
Post-Operative Outcomes
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Luime, J.J.; Koes, B.W.; Hendriksen, I.J.; Burdorf, A.; Verhagen, A.P.; Miedema, H.S.; Verhaar, J.A. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand. J. Rheumatol. 2004, 33, 73–81. [Google Scholar] [CrossRef]
- Bunker, T. Rotator cuff disease. Curr. Orthop. 2002, 3, 223–233. [Google Scholar] [CrossRef]
- Hashimoto, T.; Nobuhara, K.; Hamada, T. Pathologic evidence of degeneration as a primary cause of rotator cuff tear. Clin. Orthop. Relat. Res. 2003, 415, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Codding, J.L.; Keener, J.D. Natural History of Degenerative Rotator Cuff Tears. Curr. Rev. Musculoskelet. Med. 2018, 11, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Karjalainen, T.V.; Jain, N.B.; Heikkinen, J.; Johnston, R.V.; Page, C.M.; Buchbinder, R. Surgery for rotator cuff tears. Cochrane Database Syst. Rev. 2019, 12, CD013502. [Google Scholar] [CrossRef] [PubMed]
- Teunis, T.; Lubberts, B.; Reilly, B.T.; Ring, D. A systematic review and pooled analysis of the prevalence of rotator cuff disease with increasing age. J. Shoulder Elb. Surg. 2014, 23, 1913–1921. [Google Scholar] [CrossRef] [PubMed]
- Vidal, C.; Lira, M.J.; de Marinis, R.; Liendo, R.; Contreras, J.J. Increasing incidence of rotator cuff surgery: A nationwide registry study in Chile. BMC Musculoskelet. Disord. 2021, 22, 1052. [Google Scholar] [CrossRef] [PubMed]
- Yanik, E.L.; Chamberlain, A.M.; Keener, J.D. Trends in rotator cuff repair rates and comorbidity burden among commercially insured patients younger than the age of 65 years, United States 2007–2016. JSES Rev. Rep. Tech. 2021, 1, 309–316. [Google Scholar] [CrossRef]
- Paloneva, J.; Lepola, V.; Aarimaa, V.; Joukainen, A.; Ylinen, J.; Mattila, V.M. Increasing incidence of rotator cuff repairs–A nationwide registry study in Finland. BMC Musculoskelet. Disord. 2015, 16, 189. [Google Scholar] [CrossRef]
- Littlewood, C.M.S.; Walters, S. Epidemiology of Rotator Cuff Tendinopathy: A Systematic Review. Shoulder Elb. 2013, 5, 256–265. [Google Scholar] [CrossRef]
- McCabe, R.A.; Nicholas, S.J.; Montgomery, K.D.; Finneran, J.J.; McHugh, M.P. The effect of rotator cuff tear size on shoulder strength and range of motion. J. Orthop. Sports Phys. Ther. 2005, 35, 130–135. [Google Scholar] [CrossRef]
- Parikh, N.; Martinez, D.J.; Winer, I.; Costa, L.; Dua, D.; Trueman, P. Direct and indirect economic burden associated with rotator cuff tears and repairs in the US. Curr. Med. Res. Opin. 2021, 37, 1199–1211. [Google Scholar] [CrossRef]
- Paraskevopoulos, E.; Plakoutsis, G.; Chronopoulos, E.; Maria, P. Effectiveness of Combined Program of Manual Therapy and Exercise Vs Exercise Only in Patients With Rotator Cuff-related Shoulder Pain: A Systematic Review and Meta-analysis. Sports Health 2023, 15, 727–735. [Google Scholar] [CrossRef]
- Longo, U.G.; Rizzello, G.; Petrillo, S.; Loppini, M.; Maffulli, N.; Denaro, V. Conservative Rehabilitation Provides Superior Clinical Results Compared to Early Aggressive Rehabilitation for Rotator Cuff Repair: A Retrospective Comparative Study. Medicina 2019, 55, 402. [Google Scholar] [CrossRef]
- Moosmayer, S.; Gartner, A.V.; Tariq, R. The natural course of nonoperatively treated rotator cuff tears: An 8.8-year follow-up of tear anatomy and clinical outcome in 49 patients. J. Shoulder Elb. Surg. 2017, 26, 627–634. [Google Scholar] [CrossRef]
- Chalmers, P.N.; Ross, H.; Granger, E.; Presson, A.P.; Zhang, C.; Tashjian, R.Z. The Effect of Rotator Cuff Repair on Natural History: A Systematic Review of Intermediate to Long-Term Outcomes. JB JS Open Access 2018, 3, e0043. [Google Scholar] [CrossRef]
- Colvin, A.C.; Egorova, N.; Harrison, A.K.; Moskowitz, A.; Flatow, E.L. National trends in rotator cuff repair. J. Bone Joint Surg. Am. 2012, 94, 227–233. [Google Scholar] [CrossRef] [PubMed]
- Tauro, J.C. Arthroscopic rotator cuff repair: Analysis of technique and results at 2- and 3-year follow-up. Arthroscopy 1998, 14, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Aleem, A.W.; Brophy, R.H. Outcomes of rotator cuff surgery: What does the evidence tell us? Clin. Sports Med. 2012, 31, 665–674. [Google Scholar] [CrossRef]
- Namdari, S.; Green, A. Range of motion limitation after rotator cuff repair. J. Shoulder Elb. Surg. 2010, 19, 290–296. [Google Scholar] [CrossRef] [PubMed]
- Cikes, A.; Kadri, F.; van Rooij, F.; Ladermann, A. Aquatic therapy following arthroscopic rotator cuff repair enables faster improvement of Constant score than land-based therapy or self-rehabilitation therapy. J. Exp. Orthop. 2023, 10, 2. [Google Scholar] [CrossRef]
- Bouche, P.A.; Gaujac, N.; Descamps, J.; Conso, C. Assessment of several postoperative protocols after rotator cuff repair: A network meta-analysis. Orthop. Traumatol. Surg. Res. 2022, 108, 103418. [Google Scholar] [CrossRef]
- Keener, J.D.; Galatz, L.M.; Stobbs-Cucchi, G.; Patton, R.; Yamaguchi, K. Rehabilitation following arthroscopic rotator cuff repair: A prospective randomized trial of immobilization compared with early motion. J. Bone Joint Surg. Am. 2014, 96, 11–19. [Google Scholar] [CrossRef]
- Nabergoj, M.; Bagheri, N.; Bonnevialle, N.; Gallinet, D.; Barth, J.; Labattut, L.; Metais, P.; Godeneche, A.; Garret, J.; Clavert, P.; et al. Arthroscopic rotator cuff repair: Is healing enough? Orthop. Traumatol. Surg. Res. 2021, 107, 103100. [Google Scholar] [CrossRef]
- Cuff, D.J.; Pupello, D.R. Prospective randomized study of arthroscopic rotator cuff repair using an early versus delayed postoperative physical therapy protocol. J. Shoulder Elb. Surg. 2012, 21, 1450–1455. [Google Scholar] [CrossRef]
- Gallagher, B.P.; Bishop, M.E.; Tjoumakaris, F.P.; Freedman, K.B. Early versus delayed rehabilitation following arthroscopic rotator cuff repair: A systematic review. Phys. Sportsmed. 2015, 43, 178–187. [Google Scholar] [CrossRef]
- Mazuquin, B.; Moffatt, M.; Gill, P.; Selfe, J.; Rees, J.; Drew, S.; Littlewood, C. Effectiveness of early versus delayed rehabilitation following rotator cuff repair: Systematic review and meta-analyses. PLoS ONE 2021, 16, e0252137. [Google Scholar] [CrossRef] [PubMed]
- Sheps, D.M.; Silveira, A.; Beaupre, L.; Styles-Tripp, F.; Balyk, R.; Lalani, A.; Glasgow, R.; Bergman, J.; Bouliane, M.; Shoulder; et al. Early Active Motion Versus Sling Immobilization After Arthroscopic Rotator Cuff Repair: A Randomized Controlled Trial. Arthroscopy 2019, 35, 749–760.e742. [Google Scholar] [CrossRef] [PubMed]
- Houck, D.A.; Kraeutler, M.J.; Schuette, H.B.; McCarty, E.C.; Bravman, J.T. Early Versus Delayed Motion After Rotator Cuff Repair: A Systematic Review of Overlapping Meta-analyses. Am. J. Sports Med. 2017, 45, 2911–2915. [Google Scholar] [CrossRef] [PubMed]
- Speer, K.P.; Cavanaugh, J.T.; Warren, R.F.; Day, L.; Wickiewicz, T.L. A role for hydrotherapy in shoulder rehabilitation. Am. J. Sports Med. 1993, 21, 850–853. [Google Scholar] [CrossRef] [PubMed]
- Levin, S. Early Mobilization Speeds Recovery. Phys. Sportsmed. 1993, 21, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Brady, B.; Redfern, J.; MacDougal, G.; Williams, J. The addition of aquatic therapy to rehabilitation following surgical rotator cuff repair: A feasibility study. Physiother. Res. Int. 2008, 13, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Burmaster, C.; Eckenrode, B.J.; Stiebel, M. Early Incorporation of an Evidence-Based Aquatic-Assisted Approach to Arthroscopic Rotator Cuff Repair Rehabilitation: Prospective Case Study. Phys. Ther. 2016, 96, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Dufournet, A.; Chong, X.L.; Schwitzguebel, A.; Bernimoulin, C.; Carvalho, M.; Bothorel, H.; Ladermann, A. Aquatic Therapy versus Standard Rehabilitation after Surgical Rotator Cuff Repair: A Randomized Prospective Study. Biology 2022, 11, 610. [Google Scholar] [CrossRef] [PubMed]
- Ladermann, A.; Burkhart, S.S.; Hoffmeyer, P.; Neyton, L.; Collin, P.; Yates, E.; Denard, P.J. Classification of full-thickness rotator cuff lesions: A review. EFORT Open Rev. 2016, 1, 420–430. [Google Scholar] [CrossRef] [PubMed]
- Patte, D. Classification of rotator cuff lesions. Clin. Orthop. Relat. Res. 1990, 254, 81–86. [Google Scholar] [CrossRef]
- Goutallier, D.; Postel, J.M.; Bernageau, J.; Lavau, L.; Voisin, M.C. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin. Orthop. Relat. Res. 1994, 304, 78–83. [Google Scholar] [CrossRef]
- Abrassart, S.; Kolo, F.; Piotton, S.; Chih-Hao Chiu, J.; Stirling, P.; Hoffmeyer, P.; Ladermann, A. ‘Frozen shoulder’ is ill-defined. How can it be described better? EFORT Open Rev. 2020, 5, 273–279. [Google Scholar] [CrossRef]
- Constant, C.R.; Murley, A.H. A clinical method of functional assessment of the shoulder. Clin. Orthop. Relat. Res. 1987, 214, 160–164. [Google Scholar] [CrossRef]
- Ladermann, A.; Chague, S.; Preissmann, D.; Kolo, F.C.; Zbinden, O.; Kevelham, B.; Bothorel, H.; Charbonnier, C. Acromioplasty during repair of rotator cuff tears removes only half of the impinging acromial bone. JSES Int. 2020, 4, 592–600. [Google Scholar] [CrossRef]
- Collin, P.; McCoubrey, G.; Ladermann, A. Posterosuperior rotator cuff repair by an independent double-row technique. Technical note and radiological and clinical results. Orthop. Traumatol. Surg. Res. 2016, 102, 405–408. [Google Scholar] [CrossRef]
- Barth, J.; Andrieu, K.; Fotiadis, E.; Hannink, G.; Barthelemy, R.; Saffarini, M. Critical period and risk factors for retear following arthroscopic repair of the rotator cuff. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 2196–2204. [Google Scholar] [CrossRef] [PubMed]
- Kukkonen, J.; Kauko, T.; Vahlberg, T.; Joukainen, A.; Aarimaa, V. Investigating minimal clinically important difference for Constant score in patients undergoing rotator cuff surgery. J. Shoulder Elb. Surg. 2013, 22, 1650–1655. [Google Scholar] [CrossRef]
- Killian, M.L.; Cavinatto, L.; Galatz, L.M.; Thomopoulos, S. The role of mechanobiology in tendon healing. J. Shoulder Elb. Surg. 2012, 21, 228–237. [Google Scholar] [CrossRef] [PubMed]
- Sarver, J.J.; Peltz, C.D.; Dourte, L.; Reddy, S.; Williams, G.R.; Soslowsky, L.J. After rotator cuff repair, stiffness--but not the loss in range of motion--increased transiently for immobilized shoulders in a rat model. J. Shoulder Elb. Surg. 2008, 17, 108S–113S. [Google Scholar] [CrossRef] [PubMed]
- Sekome, K.; Maddocks, S. The short-term effects of hydrotherapy on pain and self-perceived functional status in individuals living with osteoarthritis of the knee joint. S. Afr. J. Physiother. 2019, 75, 476. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Chung, S.W.; Kim, J.Y.; Ok, J.H.; Park, I.; Oh, J.H. Is early passive motion exercise necessary after arthroscopic rotator cuff repair? Am. J. Sports Med. 2012, 40, 815–821. [Google Scholar] [CrossRef] [PubMed]
- Thomson, S.; Jukes, C.; Lewis, J. Rehabilitation following surgical repair of the rotator cuff: A systematic review. Physiotherapy 2016, 102, 20–28. [Google Scholar] [CrossRef]
- Yi, A.; Villacis, D.; Yalamanchili, R.; Hatch, G.F., 3rd. A Comparison of Rehabilitation Methods After Arthroscopic Rotator Cuff Repair: A Systematic Review. Sports Health 2015, 7, 326–334. [Google Scholar] [CrossRef]

| Land-Based Therapy (n = 92) | Hydrotherapy (n = 93) | p-Value LB vs. H | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Early (n = 29) | Late (n = 63) | Early (n = 33) | Late (n = 60) | |||||||||
| Mean ± SD | (Min–Max) | Mean ± SD | (Min–Max) | p-Value | Mean ± SD | (Min–Max) | Mean ± SD | (Min–Max) | p-Value | Early | Late | |
| n (%) | n (%) | n (%) | n (%) | |||||||||
| Male gender | 16 (55%) | 36 (57%) | 1.000 | 19 (58%) | 33 (55%) | 0.983 | 1.000 | 0.954 | ||||
| Dominant side | 20 (69%) | 33 (52%) | 0.205 | 25 (76%) | 35 (58%) | 0.146 | 0.754 | 0.630 | ||||
| Age at surgery | 56.0 ± 7.5 | (45.0–75.0) | 56.8 ± 5.4 | (47.0–67.0) | 0.624 | 52.8 ± 9.5 | (37.0–69.0) | 56.2 ± 5.2 | (46.0–67.0) | 0.063 | 0.146 | 0.811 |
| Score | ||||||||||||
| Constant | 55.9 ± 15.9 | (21.0–88.0) | 50.4 ± 3.3 | (44.0–57.0) | 0.125 | 58.0 ± 16.7 | (30.0–87.5) | 50.6 ± 3.2 | (44.0–57.0) | 0.009 | 1.000 | 1.000 |
| Land-Based Therapy (n = 92) | Hydrotherapy (n = 93) | p-Value LB vs. H | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Early (n = 29) | Late (n = 63) | Early (n = 33) | Late (n = 60) | |||||||||
| Mean ± SD | (Min–Max) | Mean ± SD | (Min–Max) | p-Value | Mean ± SD | (Min–Max) | Mean ± SD | (Min–Max) | p-Value | Early | Late | |
| Constant | ||||||||||||
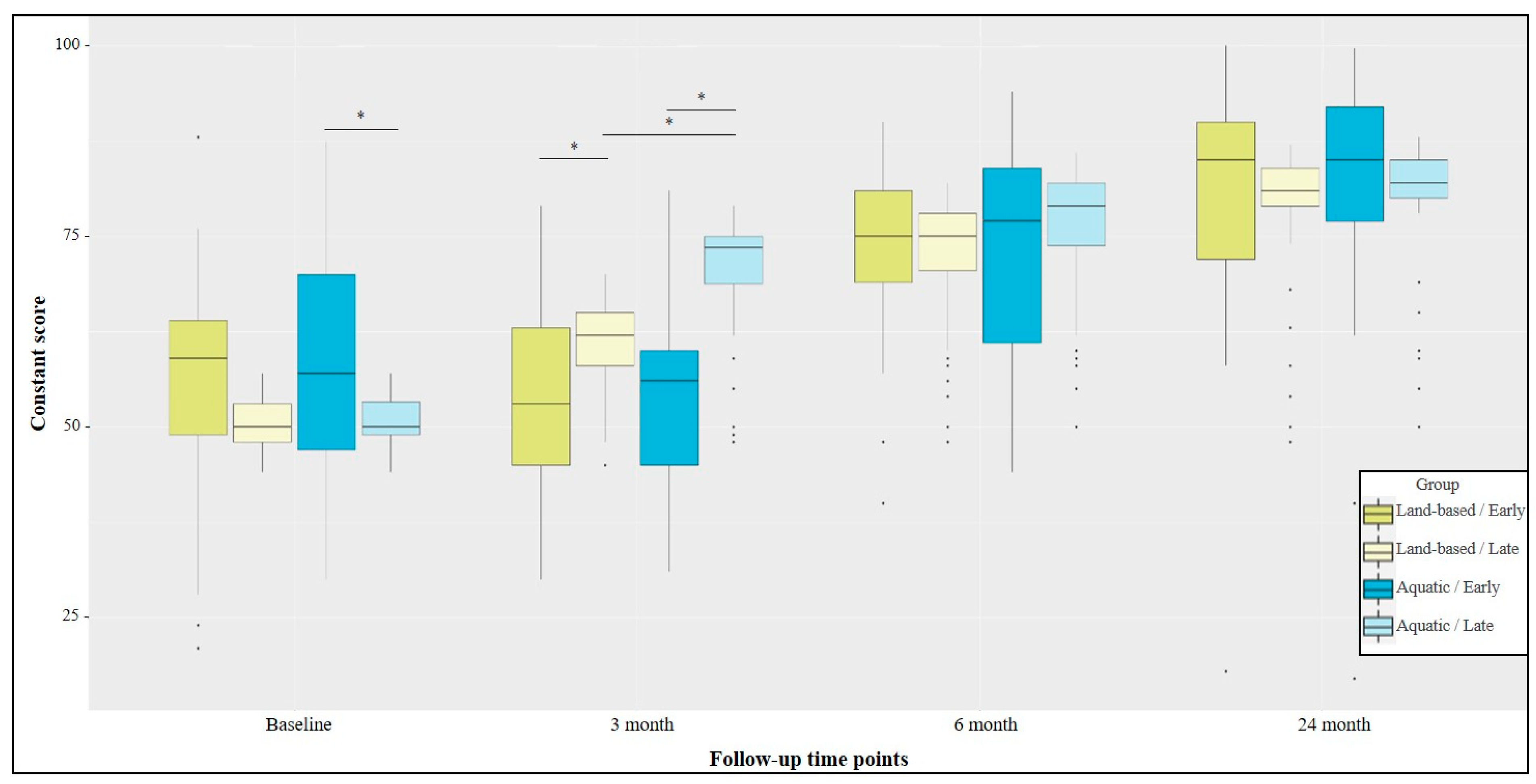
| 3 months | 54.6 ± 13.3 | (30.0–79.0) | 61.0 ± 5.7 | (45.0–70.0) * | 0.042 | 55.4 ± 12.8 | (31.0–81.0) | 70.3 ± 8.2 | (48.0–79.0) * | <0.001 | 1.000 | <0.001 |
| 6 months | 72.6 ± 12.3 | (40.0–90.0) * | 72.2 ± 8.6 | (48.0–82.0) * | 1.000 | 73.7 ± 13.7 | (44.0–94.0) * | 75.5 ± 9.5 | (50.0–86.0) * | 1.000 | 1.000 | 0.478 |
| 24 months | 79.8 ± 16.2 | (18.0–100.0) | 78.8 ± 9.0 | (48.0–87.0) * | 1.000 | 79.8 ± 18.0 | (17.0–100.0) | 80.3 ± 8.6 | (50.0–88.0) | 1.000 | 1.000 | 1.000 |
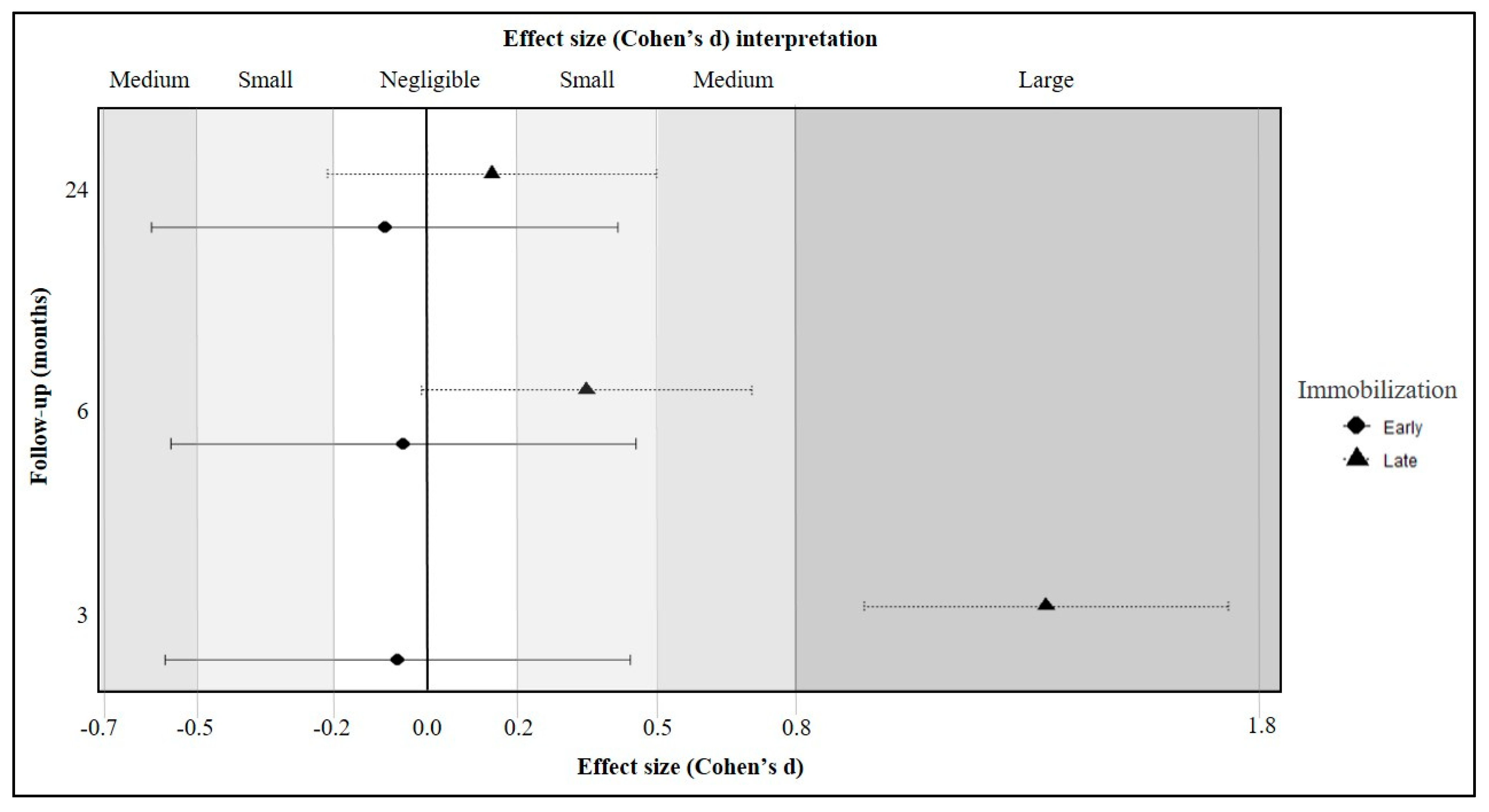
| Follow-Up | Effect | DFn | DFd | F | p-Value | Ges |
|---|---|---|---|---|---|---|
| 3 month | Rehabilitation | 1 | 181 | 11.786 | 0.001 | 0.061 |
| Immobilization | 1 | 181 | 52.562 | <0.001 | 0.225 | |
| Rehabilitation × Immobilization | 1 | 181 | 8.372 | 0.004 | 0.044 | |
| 6 month | Rehabilitation | 1 | 181 | 1.808 | 0.180 | 0.010 |
| Immobilization | 1 | 181 | 0.2 | 0.655 | 0.001 | |
| Rehabilitation × Immobilization | 1 | 181 | 0.471 | 0.493 | 0.003 | |
| 24 month | Rehabilitation | 1 | 181 | 0.158 | 0.692 | 0.001 |
| Immobilization | 1 | 181 | 0.017 | 0.895 | 0.000 | |
| Rehabilitation × Immobilization | 1 | 181 | 0.16 | 0.690 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lädermann, A.; Cikes, A.; Zbinden, J.; Martinho, T.; Pernoud, A.; Bothorel, H. Hydrotherapy after Rotator Cuff Repair Improves Short-Term Functional Results Compared with Land-Based Rehabilitation When the Immobilization Period Is Longer. J. Clin. Med. 2024, 13, 954. https://doi.org/10.3390/jcm13040954
Lädermann A, Cikes A, Zbinden J, Martinho T, Pernoud A, Bothorel H. Hydrotherapy after Rotator Cuff Repair Improves Short-Term Functional Results Compared with Land-Based Rehabilitation When the Immobilization Period Is Longer. Journal of Clinical Medicine. 2024; 13(4):954. https://doi.org/10.3390/jcm13040954
Chicago/Turabian StyleLädermann, Alexandre, Alec Cikes, Jeanni Zbinden, Tiago Martinho, Anthony Pernoud, and Hugo Bothorel. 2024. "Hydrotherapy after Rotator Cuff Repair Improves Short-Term Functional Results Compared with Land-Based Rehabilitation When the Immobilization Period Is Longer" Journal of Clinical Medicine 13, no. 4: 954. https://doi.org/10.3390/jcm13040954
APA StyleLädermann, A., Cikes, A., Zbinden, J., Martinho, T., Pernoud, A., & Bothorel, H. (2024). Hydrotherapy after Rotator Cuff Repair Improves Short-Term Functional Results Compared with Land-Based Rehabilitation When the Immobilization Period Is Longer. Journal of Clinical Medicine, 13(4), 954. https://doi.org/10.3390/jcm13040954






