Effectiveness of Topical Oxygen Therapy in Gingivitis and Periodontitis: Clinical Case Reports and Review of the Literature
Abstract
1. Introduction
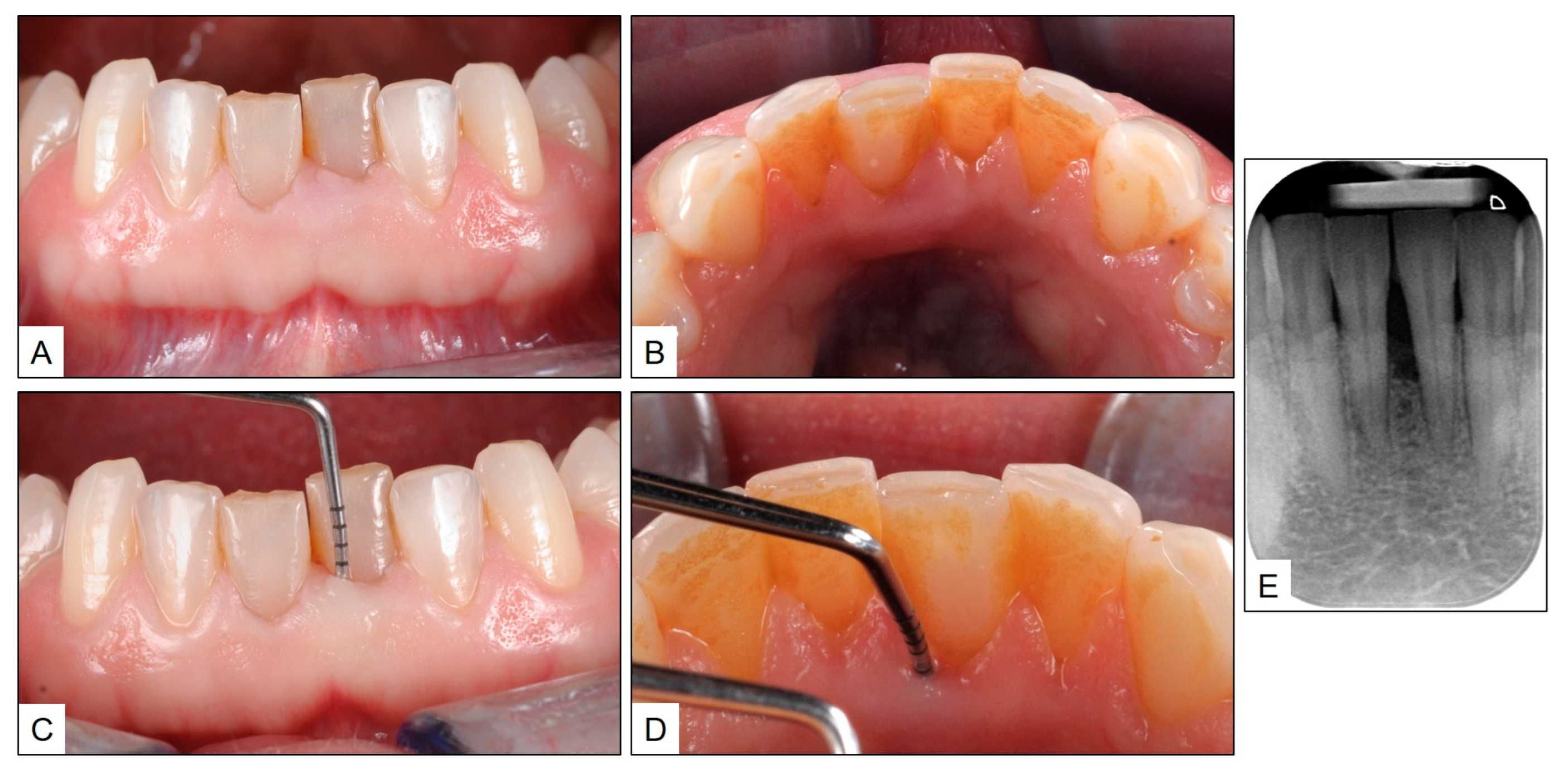
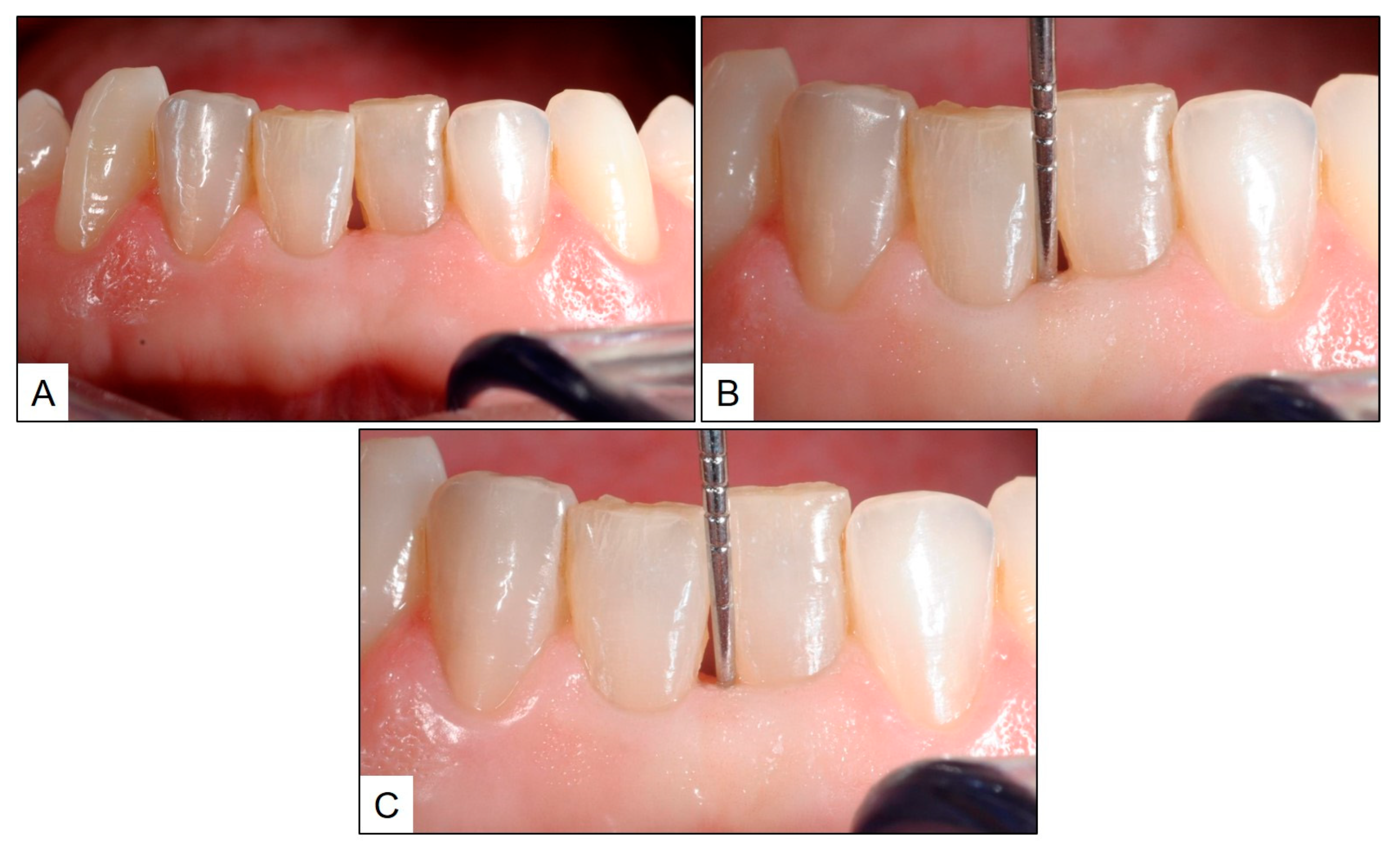
2. Clinical Case Report 1—Topical Oxygen Therapy (blue®m) in the Treatment of Gingivitis
3. Clinical Case Report 2—Topical Oxygen Therapy (blue®m) in the Treatment of Periodontitis
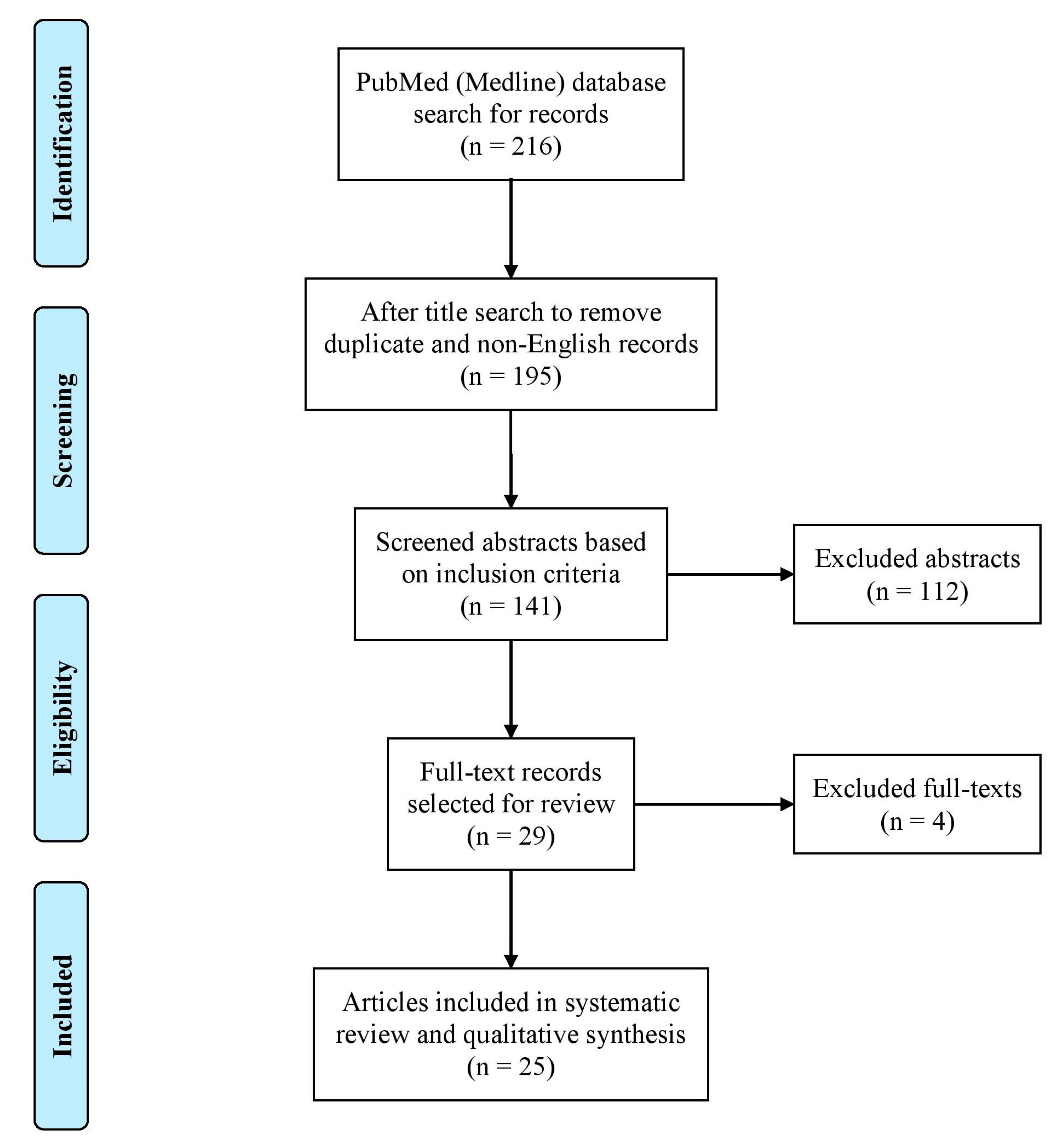
4. Systematic Review of the Literature—Methodology and Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Correction Statement
References
- Pradeep, A.R.; Kumari, M.; Priyanka, N.; Naik, S.B. Efficacy of chlorhexidine, metronidazole and combination gel in the treatment of gingivitis—A randomized clinical trial. J. Int. Acad. Periodontol. 2012, 14, 91–96. [Google Scholar] [PubMed]
- Martin, B.J.; Campbell, P.M.; Rees, T.D.; Buschang, P.H. A randomized controlled trial evaluating antioxidant-essential oil gel as a treatment for gingivitis in orthodontic patients. Angle Orthod. 2016, 86, 407–412. [Google Scholar] [CrossRef]
- Bergamaschi, C.C.; Santamaria, M.P.; Berto, L.A.; Cogo-Müller, K.; Motta, R.H.; Salum, E.A.; Nociti Júnior, F.H.; Goodson, J.M.; Groppo, F.C. Full mouth periodontal debridement with or without adjunctive metronidazole gel in smoking patients with chronic periodontitis: A pilot study. J. Periodontal Res. 2016, 51, 50–59. [Google Scholar] [CrossRef]
- Gomes, E.W.B.; Casarin, M.; Martins, T.M.; da Silva, A.F. Local delivery therapies as adjuvants to non-surgical periodontal treatment of periodontitis grade c: A systematic review. Clin. Oral Investig. 2020, 24, 4213–4224. [Google Scholar] [CrossRef] [PubMed]
- Pałka, Ł.; Nowakowska-Toporowska, A.; Dalewski, B. Is chlorhexidine in dentistry an ally or a foe? A narrative review. Healthcare 2022, 10, 764. [Google Scholar] [CrossRef]
- Agarwal, E.; Pradeep, A.R.; Bajaj, P.; Naik, S.B. Efficacy of local drug delivery of 0.5% clarithromycin gel as an adjunct to non-surgical periodontal therapy in the treatment of current smokers with chronic periodontitis: A randomized controlled clinical trial. J. Periodontol. 2012, 83, 1155–1163. [Google Scholar] [CrossRef] [PubMed]
- Cunha, E.J.; Auersvald, C.M.; Deliberador, T.M.; Gonzaga, C.C.; Esteban Florez, F.L.; Correr, G.M.; Storrer, C.L.M. Effects of active oxygen toothpaste in supragingival biofilm reduction: A randomized controlled clinical trial. Int. J. Dent. 2019, 2019, 3938214. [Google Scholar] [CrossRef]
- Plemmenos, G.; Piperi, C. Pathogenic molecular mechanisms in periodontitis and peri-implantitis: Role of advanced glycation end products. Life 2022, 12, 218. [Google Scholar] [CrossRef]
- Ramalingam, S.; Sundar, C.; Jansen, J.A.; Alghamdi, H. Chapter 1—Alveolar bone science: Structural characteristics and pathological changes. In Dental Implants and Bone Grafts; Alghamdi, H., Jansen, J., Eds.; Woodhead Publishing: Cambridge, UK, 2020; pp. 1–22. [Google Scholar]
- Ramalingam, S.; Alfotawi, R. Clinical applications of bone substitute materials and bone regeneration. In Bone Regeneration in the Maxillofacial Region, 1st ed.; Alfotawi, R., Ed.; Cambridge Scholars Publishing: Cambridge, UK, 2023; pp. 36–67. [Google Scholar]
- Pradeep, A.R.; Rao, N.S.; Naik, S.B.; Kumari, M. Efficacy of varying concentrations of subgingivally delivered metformin in the treatment of chronic periodontitis: A randomized controlled clinical trial. J. Periodontol. 2013, 84, 212–220. [Google Scholar] [CrossRef]
- Zanatta, F.B.; Antoniazzi, R.P.; Rösing, C.K. Staining and calculus formation after 0.12% chlorhexidine rinses in plaque-free and plaque covered surfaces: A randomized trial. J. Appl. Oral Sci. Rev. FOB 2010, 18, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.X.; Werner, J.; Kirsch, T.; Zuckerman, J.D.; Virk, M.S. Cytotoxicity evaluation of chlorhexidine gluconate on human fibroblasts, myoblasts, and osteoblasts. J. Bone Jt. Infect. 2018, 3, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Chiewchalermsri, C.; Sompornrattanaphan, M.; Wongsa, C.; Thongngarm, T. Chlorhexidine allergy: Current challenges and future prospects. J. Asthma Allergy 2020, 13, 127–133. [Google Scholar] [CrossRef] [PubMed]
- Passarelli, P.C.; Netti, A.; Lopez, M.A.; Giaquinto, E.F.; De Rosa, G.; Aureli, G.; Bodnarenko, A.; Papi, P.; Starzyńska, A.; Pompa, G.; et al. Local/topical antibiotics for peri-implantitis treatment: A systematic review. Antibiotics 2021, 10, 1298. [Google Scholar] [CrossRef] [PubMed]
- Frykberg, R.G. Topical wound oxygen therapy in the treatment of chronic diabetic foot ulcers. Medicina 2021, 57, 917. [Google Scholar] [CrossRef] [PubMed]
- Ngeow, W.C.; Tan, C.C.; Goh, Y.C.; Deliberador, T.M.; Cheah, C.W. A narrative review on means to promote oxygenation and angiogenesis in oral wound healing. Bioengineering 2022, 9, 636. [Google Scholar] [CrossRef] [PubMed]
- Cláudio, M.M.; Garcia, V.G.; Freitas, R.M.; Rodrigues, J.V.S.; Wainwright, M.; Casarin, R.C.V.; Duque, C.; Theodoro, L.H. Association of active oxygen-releasing gel and photodynamic therapy in the treatment of residual periodontal pockets in type 2 diabetic patients: A randomized controlled clinical study. J. Periodontol. 2023. Epub ahead of print. [Google Scholar] [CrossRef]
- Deliberador, T.M.; Weiss, S.G.; Rychuv, F.; Cordeiro, G.; Cate, M.t.; Leonardi, L.; Brancher, J.A.; Scariot, R. Comparative analysis in vitro of the application of blue®m oral gel versus chlorhexidine on porphyromonas gingivalis: A pilot study. Adv. Microbiol. 2020, 10, 194–201. [Google Scholar] [CrossRef]
- Grootveld, M.; Lynch, E.; Page, G.; Chan, W.; Percival, B.; Anagnostaki, E.; Mylona, V.; Bordin-Aykroyd, S.; Grootveld, K.L. Potential advantages of peroxoborates and their ester adducts over hydrogen peroxide as therapeutic agents in oral healthcare products: Chemical/biochemical reactivity considerations in vitro, ex vivo and in vivo. Dent. J. 2020, 8, 89. [Google Scholar] [CrossRef]
- Mattei, B.M.; Imanishi, S.A.W.; de Oliveira Ramos, G.; de Campos, P.S.; Weiss, S.G.; Deliberador, T.M. Mouthwash with active oxygen (blue®m) reduces postoperative inflammation and pain. Case Rep. Dent. 2021, 2021, 5535807. [Google Scholar] [CrossRef]
- Caton, J.G.; Armitage, G.; Berglundh, T.; Chapple, I.L.C.; Jepsen, S.; Kornman, K.S.; Mealey, B.L.; Papapanou, P.N.; Sanz, M.; Tonetti, M.S. A new classification scheme for periodontal and peri-implant diseases and conditions—Introduction and key changes from the 1999 classification. J. Clin. Periodontol. 2018, 45 (Suppl. S20), S1–S8. [Google Scholar] [CrossRef]
- Chapple, I.L.C.; Mealey, B.L.; Van Dyke, T.E.; Bartold, P.M.; Dommisch, H.; Eickholz, P.; Geisinger, M.L.; Genco, R.J.; Glogauer, M.; Goldstein, M.; et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. J. Clin. Periodontol. 2018, 45 (Suppl. S20), S68–S77. [Google Scholar] [CrossRef] [PubMed]
- Chibinski, A.C.; Pochapski, M.T.; Farago, P.V.; Santos, F.A.; Czlusniak, G.D. Clinical evaluation of chlorhexidine for the control of dental biofilm in children with special needs. Community Dent. Health 2011, 28, 222–226. [Google Scholar]
- Niazi, F.H.; Noushad, M.; Tanvir, S.B.; Ali, S.; Al-Khalifa, K.S.; Qamar, Z.; Al-Sheikh, R. Antimicrobial efficacy of indocyanine green-mediated photodynamic therapy compared with salvadora persica gel application in the treatment of moderate and deep pockets in periodontitis. Photodiagnosis Photodyn. Ther. 2020, 29, 101665. [Google Scholar] [CrossRef] [PubMed]
- Qamar, Z.; Almohana, S.A.; Khalid Alanazi, A.; Khalid Alanazi, A.; Almohana, A.A.; Zeeshan, T. Clinical evaluation of the effects of topical indocyanine-green mediated photosensitiser vs aloe vera gel as adjunct therapy to scaling and root planing in chronic periodontitis patients. Oral Health Prev. Dent. 2021, 19, 489–494. [Google Scholar] [PubMed]
- Yakout, B.K.; Kamel, F.R.; Khadr, M.; Heikal, L.A.H.; El-Kimary, G.I. Efficacy of hyaluronic acid gel and photobiomodulation therapy on wound healing after surgical gingivectomy: A randomized controlled clinical trial. BMC Oral Health 2023, 23, 805. [Google Scholar] [CrossRef] [PubMed]
- Pradeep, A.R.; Thorat, M.S. Clinical effect of subgingivally delivered simvastatin in the treatment of patients with chronic periodontitis: A randomized clinical trial. J. Periodontol. 2010, 81, 214–222. [Google Scholar] [CrossRef] [PubMed]
- Guarnelli, M.E.; Farina, R.; Cucchi, A.; Trombelli, L. Clinical and microbiological effects of mechanical instrumentation and local antimicrobials during periodontal supportive therapy in aggressive periodontitis patients: Smoker versus non-smoker patients. J. Clin. Periodontol. 2010, 37, 998–1004. [Google Scholar] [CrossRef] [PubMed]
- Flemmig, T.F.; Petersilka, G.; Völp, A.; Gravemeier, M.; Zilly, M.; Mross, D.; Prior, K.; Yamamoto, J.; Beikler, T. Efficacy and safety of adjunctive local moxifloxacin delivery in the treatment of periodontitis. J. Periodontol. 2011, 82, 96–105. [Google Scholar] [CrossRef]
- Sapna, N.; Vandana, K.L. Evaluation of hyaluronan gel (gengigel®) as a topical applicant in the treatment of gingivitis. J. Investig. Clin. Dent. 2011, 2, 162–170. [Google Scholar] [CrossRef]
- Sharma, A.; Pradeep, A.R. Clinical efficacy of 1% alendronate gel in adjunct to mechanotherapy in the treatment of aggressive periodontitis: A randomized controlled clinical trial. J. Periodontol. 2012, 83, 19–26. [Google Scholar] [CrossRef]
- Funosas, E.; Feser, G.; Escovich, L.; Maestri, L. Alteration of hemostasis in patients treated with subgingival nsaids during periodontal therapy. Acta Odontol. Latinoam. AOL 2012, 25, 103–108. [Google Scholar] [PubMed]
- Tonetti, M.S.; Lang, N.P.; Cortellini, P.; Suvan, J.E.; Eickholz, P.; Fourmousis, I.; Topoll, H.; Vangsted, T.; Wallkamm, B. Effects of a single topical doxycycline administration adjunctive to mechanical debridement in patients with persistent/recurrent periodontitis but acceptable oral hygiene during supportive periodontal therapy. J. Clin. Periodontol. 2012, 39, 475–482. [Google Scholar] [CrossRef] [PubMed]
- Chandra, R.V.; Sandhya, Y.P.; Nagarajan, S.; Reddy, B.H.; Naveen, A.; Murthy, K.R. Efficacy of lycopene as a locally delivered gel in the treatment of chronic periodontitis: Smokers vs nonsmokers. Quintessence Int. 2012, 43, 401–411. [Google Scholar] [PubMed]
- Madlena, M.; Banoczy, J.; Gotz, G.; Marton, S.; Kaan, M., Jr.; Nagy, G. Effects of amine and stannous fluorides on plaque accumulation and gingival health in orthodontic patients treated with fixed appliances: A pilot study. Oral Health Dent. Manag. 2012, 11, 57–61. [Google Scholar] [PubMed]
- Fawzy El-Sayed, K.M.; Dahaba, M.A.; Aboul-Ela, S.; Darhous, M.S. Local application of hyaluronan gel in conjunction with periodontal surgery: A randomized controlled trial. Clin. Oral Investig. 2012, 16, 1229–1236. [Google Scholar] [CrossRef]
- Patel, P.V.; Patel, A.; Kumar, S.; Holmes, J.C. Effect of subgingival application of topical ozonated olive oil in the treatment of chronic periodontitis: A randomized, controlled, double blind, clinical and microbiological study. Minerva Stomatol. 2012, 61, 381–398. [Google Scholar]
- Chava, V.K.; Vedula, B.D. Thermo-reversible green tea catechin gel for local application in chronic periodontitis: A 4-week clinical trial. J. Periodontol. 2013, 84, 1290–1296. [Google Scholar] [CrossRef]
- Anitha, V.; Rajesh, P.; Shanmugam, M.; Priya, B.M.; Prabhu, S.; Shivakumar, V. Comparative evaluation of natural curcumin and synthetic chlorhexidine in the management of chronic periodontitis as a local drug delivery: A clinical and microbiological study. Indian J. Dent. Res. Off. Publ. Indian Soc. Dent. Res. 2015, 26, 53–56. [Google Scholar] [CrossRef]
- Priyanka, N.; Kalra, N.; Saquib, S.; Malgaonkar, N.; Tarakji, B.; Varsha, J.; Pradeep, A.R. Efficacy of subgingivally delivered satranidazole in the treatment of type 2 diabetes subjects with chronic periodontitis: A randomized controlled clinical trial. J. Int. Acad. Periodontol. 2015, 17, 42–48. [Google Scholar]
- Pradeep, A.R.; Karvekar, S.; Nagpal, K.; Patnaik, K.; Guruprasad, C.N.; Kumaraswamy, K.M. Efficacy of locally delivered 1.2% rosuvastatin gel to non-surgical treatment of patients with chronic periodontitis: A randomized, placebo-controlled clinical trial. J. Periodontol. 2015, 86, 738–745. [Google Scholar] [CrossRef] [PubMed]
- Pulikkotil, S.J.; Nath, S. Effects of curcumin on crevicular levels of il-1β and ccl28 in experimental gingivitis. Aust. Dent. J. 2015, 60, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Kharaeva, Z.F.; Zhanimova, L.R.; Mustafaev, M.; De Luca, C.; Mayer, W.; Chung Sheun Thai, J.; Tiew Siok Tuan, R.; Korkina, L.G. Effects of standardised fermented papaya gel on clinical symptoms, inflammatory cytokines, and nitric oxide metabolites in patients with chronic periodontitis: An open randomised clinical study. Mediat. Inflamm. 2016, 2016, 9379840. [Google Scholar] [CrossRef]
- Rayyan, M.; Terkawi, T.; Abdo, H.; Abdel Azim, D.; Khalaf, A.; AlKhouli, Z.; Meziad, M.; Alshamma’a, M.; Abu Naim, H. Efficacy of grape seed extract gel in the treatment of chronic periodontitis: A randomized clinical study. J. Investig. Clin. Dent. 2018, 9, e12318. [Google Scholar] [CrossRef] [PubMed]
- Al-Shammari, N.M.; Shafshak, S.M.; Ali, M.S. Effect of 0.8% hyaluronic acid in conventional treatment of moderate to severe chronic periodontitis. J. Contemp. Dent. Pract. 2018, 19, 527–534. [Google Scholar] [CrossRef]
- Aslroosta, H.; Yaghobee, S.; Akbari, S.; Kanounisabet, N. The effects of topical erythropoietin on non-surgical treatment of periodontitis: A preliminary study. BMC Oral Health 2021, 21, 240. [Google Scholar] [CrossRef]
- Sanz, M.; Herrera, D.; Kebschull, M.; Chapple, I.; Jepsen, S.; Beglundh, T.; Sculean, A.; Tonetti, M.S.; EFP Workshop Participants and Methodological Consultants. Treatment of stage i-iii periodontitis-the efp s3 level clinical practice guideline. J. Clin. Periodontol. 2020, 47 (Suppl. S22), 4–60. [Google Scholar] [CrossRef]
- Veerachamy, S.; Yarlagadda, T.; Manivasagam, G.; Yarlagadda, P.K. Bacterial adherence and biofilm formation on medical implants: A review. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2014, 228, 1083–1099. [Google Scholar] [CrossRef] [PubMed]
- Sundar, C.; Ramalingam, S.; Mohan, V.; Pradeepa, R.; Ramakrishnan, M.J. Periodontal therapy as an adjunctive modality for hba1c reduction in type-2 diabetic patients. J. Educ. Health Promot. 2018, 7, 152. [Google Scholar] [PubMed]



| Author | Topical/Local Therapy Based on | Post Treatment Clinical Parameters | Outcomes/Conclusions |
|---|---|---|---|
| Pradeep et al. [28] | Simvastatin gel | Decrease in GBI—2.33 ± 0.80/Reduction in PPD—4.26 ± 1.59 mm/CAL gain—4.36 ± 1.92 mm | After 6 months, SRP with locally administered simvastatin gel gave significantly better clinical outcomes than SRP alone. |
| Guarnelli et al. [29] | Amine fluoride/Stannous fluoride (toothpaste and mouthrinse) | Decrease in PI *—Smoker (1.2)/Non-smoker (0.7)/Decrease in GI *—Smoker (0.2)/Non-smoker (0.3)/Reduction in PPD *—Smoker (0.5 mm)/Non-smoker (0.5 mm) | After 3 months, topical amine fluoride/stannous fluoride combination increased the efficacy of clinical outcomes compared with mechanical plaque control alone. |
| Flemmig et al. [30] | Moxifloxacin gel (0.125%, 0.4% and 1.25%) | Reduction in PPD—0.4% gel (1.5 ± 0.6 mm)/1.25% gel (1.2 ± 0.4 mm)/0.125% gel (1.1 ± 1.1 mm) | After 3 months, subgingival moxifloxacin 0.4% gel significantly reduced PPD compared with SRP alone. |
| Sapna and Vandana [31] | Hyaluronic acid gel (Gengigel® applied topical and intrasulcular) | Decrease in PI—0.72 ± 0.38/Decrease in GI—0.83 ± 0.32/Decrease in GBI—5.53 ± 1.91 | After 21 days, combined topical and intrasulcular hyaluronic acid gel administration significantly improved clinical outcomes and was equivalent to that of scaling alone. |
| Sharma and Pradeep [32] | Alendronate (1%) gel | Reduction in PPD—3.88 ± 1.39 mm/CAL gain—3.27 ± 1.11 | After 6 months, alendronate 1% gel when used as an adjunct to SRP significantly improves clinical periodontal outcomes and results in better bone fill in areas of bone destruction due to aggressive periodontitis. |
| Funosas et al. [33] | NSAID gel (aspirin 1%, ketoprofen 1%, ketoprofen 2%) | Decrease in PI—aspirin 1% (1.04 ± 0.84)/ketoprofen 1% (0.93 ± 0.80)/ketoprofen 2% (1.09 ± 0.74)/Decrease in GI—aspirin 1% (1.42 ± 0.76)/ketoprofen 1% (1.21 ± 0.83)/ketoprofen 2% (1.23 ± 0.77)/Reduction in PPD—aspirin 1% (1.26 ± 0.13 mm)/ketoprofen 1% (1.02 ± 0.21 mm)/ketoprofen 2% (1.08 ± 0.28 mm) | After 30 days, aspirin 1% gel administered subgingivally after SRP was the most effective NSAID gel in improving clinical outcomes. |
| Tonetti et al. [34] | Doxycycline gel (slow release formulation) | Reduction in PPD—0.11 ± 0.03 mm | After 3 months, subgingival scaling and administration of doxycycline gel resulted in significant reduction of PPD compared with scaling alone. |
| Chandra et al. [35] | Lycopene gel | After 3 months, locally administered lycopene gel significantly reduced gingival bleeding and PPD, and increased CAL. | |
| Madlena et al. [36] | Amine fluoride/Stannous fluoride (toothpaste and mouthrinse) | Decrease in PI—0.89 ± 0.15/Decrease in GI—1.05 ± 0.19 | After 4 weeks, use of amine fluoride/stannous fluoride as a chemical adjunct to mechanical plaque control was significantly beneficial in patients with orthodontic braces. |
| El-Sayed et al. [37] | Hyaluronic acid gel (Gengigel®) | Decrease in BOP *—0.50/Reduction in PPD *—3.0 mm/CAL gain *—3.5 mm | After 6 months, locally delivered hyaluronic acid gel significantly improves clinical outcomes of periodontal surgery. |
| Agarwal et al. [6] | Clarithromycin (0.5%) gel | Decrease in PI—1.47 ± 0.18/Decrease in GI—0.74 ± 0.08/Decrease in GBI—0.91 ± 0.10/Reduction in PPD—2.53 ± 0.16 mm/CAL gain—1.52 ± 0.15 | After 6 months, subgingival administration of clarithromycin 0.5% gel with SRP resulted in significantly enhanced clinical outcomes. |
| Patel et al. [38] | Ozonated olive oil | Decrease in PI—2.76 ± 0.16/Decrease in GI—2.17 ± 0.12/Decrease in GBI—4.15 ± 0.12 | After 8 weeks, SRP in combination with topically applied ozonated olive oil improves clinical periodontal outcomes, similar to results of chlorhexidine. |
| Pradeep et al. [1] | Chlorhexidine gel + Metronidazole gel | Decrease in PI—2.41 ± 0.10/Decrease in GI—1.36 ± 0.08/Decrease in bacterial population—26.6 ± 0.34 (×104 colonies) | After 6 months, topical application of a combination of chlorhexidine and metronidazole gel significantly improved clinical outcomes in gingivitis. |
| Pradeep et al. [11] | Metformin gel (0.5%, 1% and 1.5%) | Reduction in PPD—0.5% gel (2.97 ± 0.93 mm)/1% gel (4.0 ± 1.05 mm)/1.5% gel (3.8 ± 1.13 mm)/CAL gain—0.5% gel (2.23 ± 0.73 mm)/1% gel (3.83 ± 0.95 mm)/1.5% gel (3.6 ± 0.81 mm) | After 6 months, locally administered metformin gel (in differing concentrations) used as an adjunct with SRP significantly enhances periodontal clinical outcomes. |
| Chava and Vedula [39] | Green tea catechin gel | Decrease in GI—1.91 ± 0.20/Reduction in PPD—2.06 ± 0.07/CAL gain—2.1 ± 0.21 | After 4 weeks, use of locally administered green tea catechin gel as an adjunct to SRP significantly enhances clinical periodontal outcomes. |
| Anitha et al. [40] | Curcumin extract | Reduction in PPD—2.97 ± 0.12/CAL gain—2.79 ± 0.21 | After 30 days, locally administered curcumin extract as an adjunct to SRP significantly enhances clinical outcomes in comparison to chlorhexidine gel. |
| Priyanka et al. [41] | Satranidazole (3%) gel | Decrease in PI—0.18 ± 0.04/Decrease in GI—1.21 ± 0.06/Reduction in PPD—4.73 ± 0.33 mm/CAL gain—3.92 ± 0.29 mm | After 6 months, subgingivally administered satranidazole 3% gel as an adjunct with SRP significantly enhances periodontal clinical outcomes, in patients with type-2 diabetes. |
| Pradeep et al. [42] | Rosuvastatin (1.2%) gel | Decrease in GBI—3.71 ± 0.24/Reduction in PPD—4.04 ± 0.34 mm/CAL gain—4.2 ± 0.17 mm | After 6 months, subgingival delivery of rosuvastatin 1.2% gel as an adjunct with SRP resulted in significantly better clinical outcomes than SRP alone. |
| Pulikkotil and Nath [43] | Curcumin gel | Decrease in PI—0.42 ± 0.16/Decrease in GI—0.45 ± 0.31/Reduction in PPD—0.29 ± 0.67 mm | After 2 months, topically applied curcumin gel on gingivitis sites significantly improved clinical outcomes, equivalent to a combination of chlorhexidine and metronidazole gel, and better than application of chlorhexidine gel alone. |
| Kharaeva et al. [44] | Standardized fermented papaya gel | After 45 days, intragingival administration of papaya gel modulated the periodontal microenvironment resulting in synergistic antibacterial action with polymorphonuclear neutrophils, mediated through normalization of pro and anti-inflammatory cytokines. | |
| Bergamaschi et al. [3] | Metronidazole (15%) gel | Reduction in PPD *—1.8 mm/CAL gain *—1.9 mm | After 6 months, topically applied metronidazole (15%) gel as an adjunct to periodontal debridement was equally effective as orally administered metronidazole (750 mg) and better than periodontal debridement alone. |
| Martin et al. [2] | Essential oil gel (with antioxidants phloretin + ferulic acid) | Decrease in PI—0.08 ± 0.07/Decrease in GI—0.14 ± 0.04/Reduction in PPD—0.04 ± 0.03 mm | After 5 weeks, although there was no statistically significant improvement in clinical parameters, topical antioxidant gel application on the gingiva helped reduce inflammation among orthodontic patients. |
| Rayyan et al. [45] | Grape seed extract gel | Decrease in PI—0.75 ± 0.71/Decrease in GI—0.85 ± 0.77/Reduction in PPD—0.65 ± 0.98 mm | After 6 months, subgingivally administered grape seed extract gel, as an adjunct to SRP for periodontitis, significantly improved gingival parameters only. |
| Al-Shammari et al. [46] | Hyaluronic acid gel (Gengigel® applied subgingival) | Decrease in PI *—4.12/Decrease in GI *—4.11/Decrease in GBI *—4.04 | After 12 weeks, subgingival administration of hyaluronic acid gel as an adjunct to SRP results in significant improvement of clinical parameters. |
| Aslroosta et al. [47] | Erythropoietin gel | Decrease in PI—1.42 ± 0.22/Decrease in GI—1.62 ± 0.17/Decrease in GBI—1.87 ± 0.15/Reduction in PPD—1.77 ± 0.19 mm/CAL gain—1.70 ± 0.89 mm | After 3 months, locally administered erythropoietin gel as an adjunct to SRP results in significant improvement of gingival and periodontal clinical parameters except PI. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Basudan, A.M.; Abas, I.; Shaheen, M.Y.; Alghamdi, H.S. Effectiveness of Topical Oxygen Therapy in Gingivitis and Periodontitis: Clinical Case Reports and Review of the Literature. J. Clin. Med. 2024, 13, 1451. https://doi.org/10.3390/jcm13051451
Basudan AM, Abas I, Shaheen MY, Alghamdi HS. Effectiveness of Topical Oxygen Therapy in Gingivitis and Periodontitis: Clinical Case Reports and Review of the Literature. Journal of Clinical Medicine. 2024; 13(5):1451. https://doi.org/10.3390/jcm13051451
Chicago/Turabian StyleBasudan, Amani M., Irfan Abas, Marwa Y. Shaheen, and Hamdan S. Alghamdi. 2024. "Effectiveness of Topical Oxygen Therapy in Gingivitis and Periodontitis: Clinical Case Reports and Review of the Literature" Journal of Clinical Medicine 13, no. 5: 1451. https://doi.org/10.3390/jcm13051451
APA StyleBasudan, A. M., Abas, I., Shaheen, M. Y., & Alghamdi, H. S. (2024). Effectiveness of Topical Oxygen Therapy in Gingivitis and Periodontitis: Clinical Case Reports and Review of the Literature. Journal of Clinical Medicine, 13(5), 1451. https://doi.org/10.3390/jcm13051451










