The Treatment of Diabetic Retinal Edema with Intravitreal Steroids: How and When
Abstract
1. Introduction
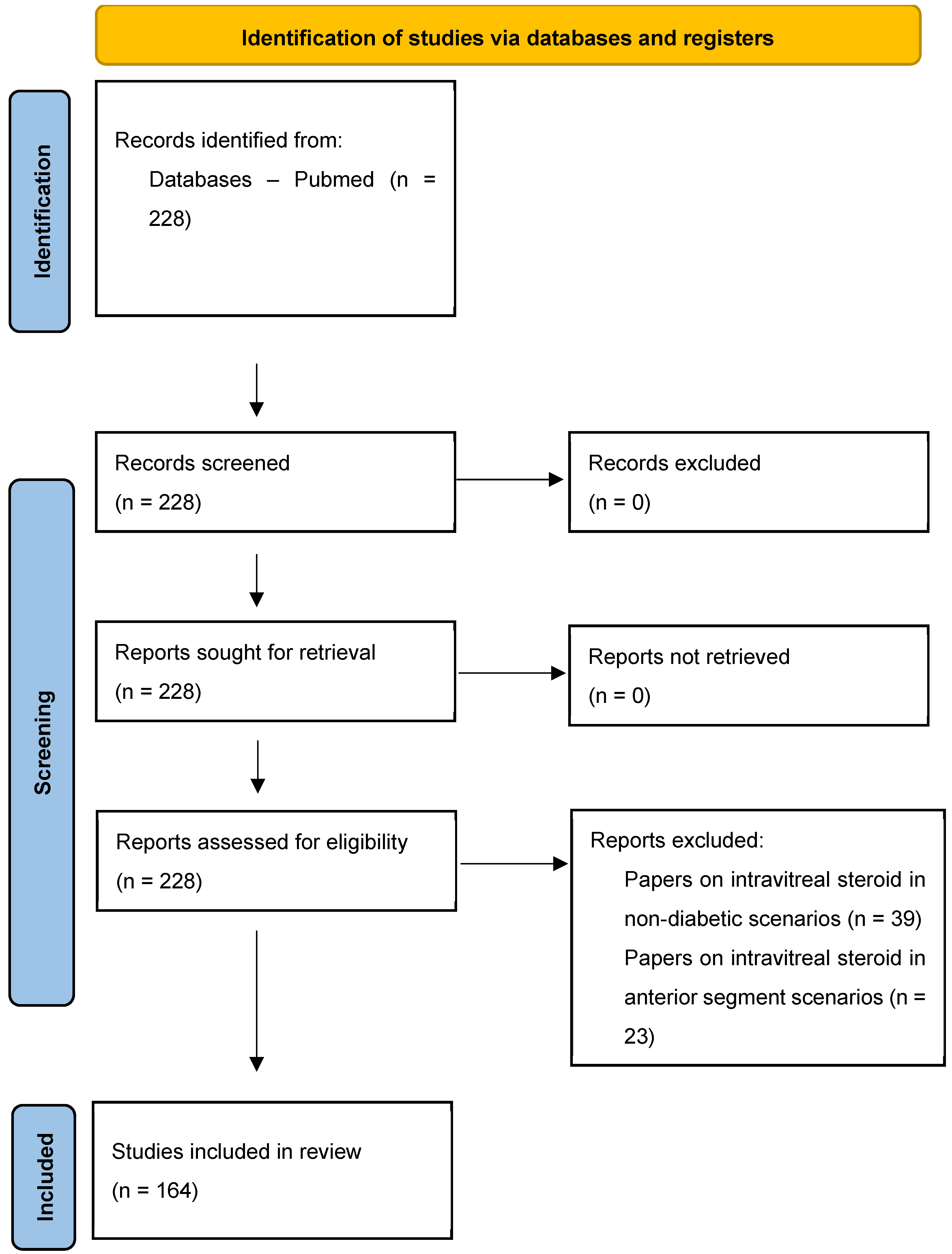
2. Methodology
3. Diabetic Macular Edema
3.1. Definition and Clinical Features of the Diabetic Macular Edema (DME)
- -
- retinal thickening with 500 µm of the center of the macula;
- -
- hard exudates within 500 µm of the center of the macula when associated with adjacent retina thickening;
- -
- retinal thickening of 1 disc area in size, any part of which is located within 1 disc area of the center of the macula.
3.2. Epidemiology and Natural History of DME
3.3. Diagnosis
- a
- Stereoscopic slit-lamp examination of the fundus using a Volk fundus lens: This is the most used method of diagnosing DME worldwide.
- b
- Color and stereo fundus photographs: These may be used to document clinical findings to stage DR and DME and identify their progression by comparing images longitudinally.
- c
- Fluorescein angiography (FA): Before the introduction of the OCT, FA has been the only method to assess and classify DME for several years [28]. FA retains fundamental importance in DME evaluation because it is the only imaging method able to detect vascular leakage and identify non-perfused areas and neovascularization in the retinal periphery [28], whose identification is mandatory to classify the DR severity and guide the treatment [4]. Non-perfused peripheral areas may indeed release inflammatory mediators that can sustain and explain a persistent DME, and the laser ablation of these ischemic areas may improve the central retinal morphology and function [29].
- d
- e
- OCT angiography (OCT-A): This provides high-reproducible and high-resolution images of the retinal vasculature, segmented in the different retinal layers that cannot be individually visualized on FA, without intravascular dye injection. OCT-A is able to show modification of the foveal avascular zone dimension, identify areas of capillary non-perfusion, and image the deep capillary plexus, which is not visible on FA, allowing a more accurate DR classification and providing useful data of the response to the different therapies [33].
3.4. Pathophysiology of DME as Rationale for Different Therapeutic Strategies
- a
- Retinal ischemia/hypoxia: This is considered to be the primum movens in DME pathogenesis. It is related to the retinal capillary and arterioles closure due to the pathological adhesion of altered leucocytes to a damaged vascular endothelium. This phenomenon, called leukostasis, seems to play an early and fundamental role in diabetic micro-vasculopathy development [8]. The most important consequence of retinal ischemia/hypoxia seems to be the up-regulation of many pro-inflammatory molecules [7], including the VEGF, which is considered to be the single most important mediator in DME pathogenesis [10,12]. VEGF causes inner BRB breakdown with consequent vascular hyper-permeability; it acts as a potent pro-inflammatory agent and may induce retinal neovascularization, it being a potent mitogen of the vascular endothelial cells [35].
- b
- Inner and outer blood-retinal barriers (BRBs) breakdown: In DME eyes, the long-standing hyperglycemia causes increased apoptosis of pericytes, vascular endothelial cells, EPR, and Mueller glial cells, along with diffuse damage of the intercellular tight-junction. The consequences are the breakdown of both inner and outer BRBs and the dysfunction of the active cellular transport of fluids out from the retina carried out by Mueller glial cells and RPE. The inner BRB breakdown seems to play a major role in DME pathogenesis [7,8].
- c
- d
- Increased retinal neurons degeneration and apoptosis: This has been demonstrated to occur early in DME eyes and to be independent of the microvascular alterations [36]. Several pieces of evidence suggest that retinal neurodegeneration may be a consequence of different factors, including chronic low-grade retinal inflammation, micro-environment alterations, glutamate accumulation, and oxidative stress. The damage and apoptosis of the retinal neurons cause a reduced retinal function and, if left untreated, will result in permanent visual loss [36].
3.5. Therapeutic Approaches in the Management of DME
- -
- Non-center involving DME (non-CIDME): As suggested by the ETDRS trial [23], the management approaches may include observation until the fluid involves the fovea or laser therapy in the presence of a considerable amount of edema/exudates located far from the fovea, i.e., >500 µm from the foveal avascular zone.
- -
- Center-involving macular edema (CIDME) with preserved VA (VA > 20/32): CIDME eyes with preserved vision are treated on the basis of the results of the DRCR.net Protocol V, an RCT that randomized eyes with CIDME and VA ≥ 20/25 to receive either prompt anti-VEGF, prompt macular laser or observation, and did not find differences amongst the three groups [26]. In these cases, observation, focal macular laser, IV injections of anti-VEGF or CSs, or a combination of these options are suggested.
- -
- Center-involving macular edema (CIDME) with visual loss (VA ≤ 20/32): CIDME eyes with visual loss were eligible for several RCTs that have demonstrated that the IV injections of anti-VEGF or CSs are significantly more effective than observation or laser for DME treatment, leading to the approval of the currently used IV pharmaceutic agents [40,41,42,43].
3.6. The Role of Metabolic Control, Laser Photocoagulation, Pars Plana Vitrectomy, and Intravitreal Anti-VEGF in DME Management
- a
- Metabolic control: The most important strategy for the prevention and treatment of DR and DME remains the control of the systemic risk factors favoring DME development and progression, including hyperglycemia, hyperlipidemia, systemic hypertension, anemia, and other hematological disorders, renal failure, sleep apnea, and carotid artery stenosis [4].
- b
- Laser photocoagulation: Focal photocoagulation of the leaking microaneurisms or grid laser photocoagulation of areas with diffuse leakage of the capillary bed has represented the gold standard in DME treatment from the mid-1980s for approximately 30 years [23] until the introduction of the intravitreal anti-VEGF therapy [41,43]. The mechanism of action of laser photocoagulation in the treatment of DME has not been fully elucidated. Focal photocoagulation laser likely works by destroying the sources of fluid leakage such as microaneurisms, but it probably may also improve the cytokine release from the RPE or Mueller cells and the RPE active pump of fluid toward the choroid. The grid laser increases the oxygenation of the inner retina by both decreasing the number of photoreceptors that are oxygen-consuming and favoring the diffusion of oxygen from the choroid to the inner retina.
- c
- Pars plana vitrectomy (PPV): Although still controversial, the vitreomacular traction seems to be a relevant factor in the development and maintenance of DME [10]. Animal and clinical studies have suggested that PPV may work by reducing vitreoretinal tractions, increasing vitreal and retinal oxygenation, and cleaning the vitreous from inflammatory mediators including VEGF, representing, therefore, a rational approach in DME eyes [49,50].
- d
- -
- Bevacizumab (Avastin, Genentech Inc., San Francisco, CA, USA) [52]: This is a full-length recombinant humanized monoclonal antibody binding the VEGF-A, approved for the treatment of several tumors, including metastatic colon, rectum, or breast cancer, that is used off-label in ophthalmology.
- -
- -
- -
- Brolucizumab (Beovue, Novartis): This is a new VEGF-A antagonist with a smaller molecular weight and a longer duration of action [55].
- -
- Faricimab (Vabysmo, Genentech/Roche): This is a new monoclonal antibody targeting both VEGF and Angiopoietin-2 [56].
- -
- -
- Anti-VEGF IV injections are characterized by short durations of action, with high rates of DME recurrence and pronounced CRT fluctuations [41,43,51,53,54,59,60,61], that have been demonstrated to be risk factors for irreversible retinal damage and visual loss [62,63]. Moreover, the need for frequent repeated IV injections leads to patients’ fatigue and lack of adherence; high costs for the public health service; and increased risk of side effects related to the intravitreal injections, such as infectious endophthalmitis, intraocular inflammation, iatrogen cataract, vitreal, and retinal hemorrhages [64].
- -
- -
- Anti-VEGF agents have been linked with the risk of persistent IOP rise requiring IOP-lowering treatment (5–10% of cases); with cataract development (0–15% of cases); and with the decrease of retinal ganglion cells layer thickness, which seems directly related with the number of IV anti-VEGF injections [66].
4. Corticosteroids for the Management of DME
4.1. The Corticosteroids
- a
- Definition
- b
- History of the CSs’ pharmacological use
- c
- Biological effects
- d
- Therapeutic effects
- e
- Side effects
- -
- Steroid-induced OHT and steroid-induced glaucoma (SIG) are the most frequent and dangerous side effects of the systemic and, most frequently, local use of CSs [74]. Subjects who respond to treatment with glucocorticoids with an IOP rise are referred to as “steroid-responders”, whose definition is not univocal and may include the following cases: IOP increase of >5 mmHg or >10 mmHg from baseline or IOP > 21 o 24 mmHg [74]. SIG can be considered to be a dangerous form of secondary open-angle glaucoma because it is frequently diagnosed late and is characterized by IOP levels that can be particularly high and lead to significant optic disc and perimetric damages within a short time [74].
- -
- Steroid-induced cataract: Prolonged use of high doses of CSs, especially if systemically administered, is a significant risk factor for the development of bilateral posterior subcapsular cataracts, with a higher incidence in children and susceptible subjects [73]. CSs are the fourth leading risk factor for cataract development, following diabetes, myopia, and glaucoma, and it has been calculated that approximately 4.7% of all cataracts are steroid-induced [73].
- -
- -
- Central serous chorioretinopathy (CSCR) development or recurrence: CSCR is an idiopathic retinal disease characterized by leakage of fluid through the RPE into the subretinal space, with serous detachments of the neurosensory retina and RPE, leading to central vision loss and metamorphopsia. Although still debated, the association between CRSC and CSs has been widely reported [71,72]. The proposed pathogenic mechanisms are a steroid-induced RPE active fluid pump impairment and an increase in the choroidal vessel permeability [71,72].
- f
- The rationale of the use of steroids in the pharmacological approach to DME
4.2. Intravitreal Corticosteroids Used for the Treatment of DME
- a
- Tiamcinolone acetonide (TA) [46]: This is commercially available as Kenalog-40 (Bristol-Myers Squibb, New York, NY, USA) or Tajoftal (Sooft Italia s.p.a. Montegiorgio, Udine, Italy), which is a crystalline powder available as an injectable suspension containing 40 mg/mL TA in isotonic saline solution and is delivered using a 30-gauge needle. TA is not approved for intraocular use, but it is used off-label to treat vitreoretinal diseases in a dose ranging between 1 and 4 mg [78], with functional and anatomical efficacy within 3–6 months post-injection [79]. Two other administration routes of TA tested in DME eyes, the posterior sub-tenon injection of 20 or 40 mg of TA [80] and the suprachoroidal injection of 2 or 4 mg of TA [81], have shown results comparable to those obtained with the IV TA injections, with less side effects. There is a preservative-free TA approved for intraocular use, though it is not for DME per se and not easily available, Triesence (Alcon Pharmaceuticals, Ft. Worth, TX, USA).
- b
- Dexamethasone (DEX) [42]: This is commercially available as a sustained-release biodegradable insert, the Ozurdex intravitreal implant (Allergan, Dublin, Ireland), which is a cylindrical tube (6 mm × 0.46 mm) composed of polylactic-co-glycolic acid polymers containing 0.7 mg of DEX, degrading into carbon dioxide and water as DEX is released into the vitreous body [82]. Ozurdex is delivered into the vitreous cavity using a single-use applicator with a 22-gauge needle for IV injection, and it was projected to endure a continuous IV release of micronized DEX over a period of ≤6 months. The peak of the functional and anatomical efficacy of the Ozurdex insert is typically reached at 2 months post-injection and has a duration of action of approximately 6 months [82].
- c
- Fluocinolone acetonide (FAc) [40]: This is commercially available as an IluvienTM IV implant (Alimera Sciences Inc., Alpharetta, GA, USA), which is a sustained-release non-biodegradable IV insert containing 0.19 mg of FAc. Iluvien is a cylindrical tube (3.5 mm × 0.37 mm) of polymer loaded with FAc that is inserted into the vitreous cavity through a 25-gauge needle and releases 0.2 µg/day of FAc. The FAMOUS study has demonstrated that the Iluvien IV implant is able to maintain a therapeutic concentration of FAc over a period of 36 months [83]. The peak of the functional and anatomical efficacy of the Iluvien IV insert has been observed between 6 and 11 months post-injection [84,85]. Being a non-biodegradable implant, floaters have been complained about by some patients after Iluvien implant [84,85].
4.3. Pharmacology of Intravitreal Corticosteroids Used for the Treatment of DME
- a
- Water solubility: DEX is the one that is the most water soluble, which implies increased bioavailability but rapid elimination. For these reasons, it is available commercially as a sustained-release biodegradable implant [21]. Fac is 50% less water soluble than DEX but still requires a sustained-release delivery system to maintain an efficient IV concentration of the drug over time. TA has low water solubility, and it is available as an IV injectable suspension [21]. Sustained IV inserts have the advantage of reducing the frequency of IV injections, with a subsequent decrease in complications related to repeated IV injection procedures, higher patient compliance, and lower healthcare costs [21].
- b
- Intravitreal pharmacokinetics: Human studies analyzing aqueous humor samplings have demonstrated that the 4 mg TA IV injection has a mean elimination half-time of 15.4 ±1.9 days [86].
4.4. Clinical Efficacy and Safety Profile of Intravitreal Corticosteroids Used in DME Treatment
- a
- Triamcinolone acetonide (TA)
- b
- Dexamethasone
- -
- -
- -
- comparative better results in naïve than in non-naïve eyes, whereas the outcomes in the two groups appear similar in anti-VEGF studies [105];
- -
- -
- better outcomes in real-life studies than in interventional studies [126]: the possibility of retreating at an earlier stage and the higher number of naïve (2/3 of treatment-naïve eyes in anti-VEGF studies vs. 1/5 in the Ozurdex studies), or short duration DME eyes with better baseline VA in the real-life studies, may explain these differences (on the other hand, systematic review and meta-analysis studies have demonstrated that IV anti-VEGF showed better anatomical and functional results in RCTs compared to the observational studies, likely because fewer injections are administered in the observation studies than those suggested by the RCTs [105,120,126], and VA gain seems to be strictly related to the number of the IV injections, at least during the first year of therapy [127,128]);
- -
- -
- lower number of required IV injections [105,107,108,120]: the comparison of the results of the MEAD study (Ozurdex pivotal study) [42] and RESTORE study (ranibizumab pivotal study) [129] showed that the VA gain observed in pseudophakic eyes receiving 0.7 mg DEX in the MEAD study (6 letters over 3 years with 4–5 implants) was comparable to that achieved in the RESTORE study by eyes receiving a mean of 7 ranibizumab injection/year
- -
- lower treatment costs, including medications, OCT, FA, and surgical procedures. The global cost of a 1-year therapy with Ozurdex is approximately one-half of that with anti-VEGF, which is mainly related to the significantly lower frequency of IV injections, even when the costs of the cataract and glaucoma surgeries are added [130].
- c
- Fluocinolone acetonide
4.5. When to Choose Intravitreal Corticosteroids for DME Treatment (Early Switch from Anti-VEGF or First-Line Therapy)
- a
- Patients unresponsive to anti-VEGF therapy: Previous RCTs [53,59,60,61] have demonstrated that approximately 40–65% of patients showed persistent DME despite adequate anti-VEGF therapy. It is important to note that the current literature does not provide a univocal definition of “poor-response” or “non-response” to treatment, so highly heterogeneous guidelines on when and how to switch or stop the different therapeutic approaches in DME have been proposed. The most commonly used definition of persistent or refractory DME after intravitreal pharmacotherapies is a VA gain of <5 letters and/or a CST reduction of <20% on OCT as compared to baseline [14,16].
- b
- Non-compliant patients or patients unable to maintain frequent follow-up visits: DME patients are often working, aging, or in poor health, requiring, therefore, frequent health care visits, and may thus have difficulties adhering to frequent office visits or monthly injection protocols. Approximately 60% of DME patients are poor or noncompliant with intravitreal therapy [153].
- c
- Patients with recent arterial thromboembolism (ATE) events: The relationship between IV anti-VEGF injections and the risk of ATEs is still debated [57], and it was not clarified by the majority of the RCTs in which patients with recent ATEs were excluded from the study [41,43,61]. On the other hand, real-world studies and systematic reviews have reported a link between anti-VEGF therapy and several systemic side effects, including deterioration of systemic hypertension, renal dysfunction, gastrointestinal perforation, stroke, myocardial infarction, and thromboembolic events [65,66].
- d
- Pregnant or breastfeeding women: DME can progress rapidly during pregnancy, especially in DM type 1 [1,2,4], so the management in pregnancy could be a challenge. The use of anti-VEGF in pregnancy is not recommended because of its potential negative effects on the angiogenesis of developing embryos or fetuses, and several case series have demonstrated a correlation between anti-VEGF IV injections given at the first five weeks of gestation and miscarriages or pre-eclampsia [155]. Although a close observation is suggested in the majority of cases, focal laser photocoagulation or intravitreal Ozurdex implant should be considered as the first-line treatment for DME in pregnancy, when therapy is considered to be necessary [13,14,15,16,17,18,19].
- e
- f
- Presence of hard exudates (HE) at the center of the fovea: This represents a major complication of DME because it can cause severe central visual loss and it is a negative predictive factor for visual outcomes [5,6]. A post-hoc analysis of the RCT Bevordex study comparing Ozurdex implants every 4 months and monthly bevacizumab injections showed that Ozurdex was associated with greater regression of the HE at 12 months [108]. These results suggest the preferential use of DEX over anti-VEGF in eyes with foveal hard exudates.
- g
- Associated OCT features of inflammation: Many OCT features, biomarkers of a high level of retinal inflammation and/or chronic DME, seem to be able to predict a poor or suboptimal responsiveness to anti-VEGF treatment, suggesting, therefore, the use of CSs as first-line therapy or an early switch to CS-therapy [32], which include the presence of large intra-retinal para-foveal cysts, a CRT > 410 µm, a large extension of the disorganization of the inner and outer retinal layers, a higher amount of hyper-reflective foci (HRFs), and the presence of a sub-foveal serous retinal detachment (SRD) [32]. In particular, a greater level of HRF seems to be one of the most important predictors for a better response to CS than to anti-VEGF [159]. OCT biomarkers in DME are proposed in order to identify in general good or poor responders to various treatments and to guide the decision to switch to other treatment options, allowing for a more personalized treatment with better visual outcomes [32,160].
- h
- Need for cataract surgery: DM patients are at higher risk of developing or deteriorating DME after cataract surgery and have a higher incidence of post-surgery macular edema, the so-called Irvine–Gass syndrome (IGS) [161]. Previous authors have reported that 22% of diabetic patients and 30% of patients with DR developed or worsened DME within 1 year after cataract surgery [161]. The results of the anti-VEGF therapy in cases of post-cataract surgery DME or of IGS are inconclusive [162], whereas IV CSs have shown promising outcomes.
- i
- Vitrectomized eyes: The vitreous body serves as a reservoir of IV-injected drugs. The study of the efficacy of the anti-VEGF agents in vitrectomized eyes has been proven to be time-limited [166], whereas TA [167,168], Ozurdex [169], and Iluvien [170] have been shown to be effective in vitrectomized eyes and can be considered the first choice in vitrectomized eyes in suitable cases.
4.6. When to Avoid Intravitreal Corticosteroids/Prefer Anti-VEGF Agents for DME Treatment
- a
- b
- Phakic patients with transparent crystalline: The intravitreal CS treatment has been associated with a high rate of cataract development or progression, particularly in the second year of treatment [40,42,46,59,87,110,117,141,142,143,144]. The incidence of cataract development or progression has been reported to range between 10% and 83% for TA [46,59,87], between 0% and 68% for DEX [42,110,117], and between 40% and 82% for FAc [40,141,142,143,144], whereas it was between 0 and 15.4% after anti-VEGF injections in real-life studies [66].
- c
- History of active or past ocular and periocular infections such as herpes or toxoplasmosis [16]. The CSs have a strong immunosuppressive action, so they can exacerbate all types of infections, and case reports of reactivation of ocular herpetic infection [70] or of acute retinal necrosis [75] after Ozurdex IV implant have been described.
- d
- Aphakia, absence or interruption of the posterior capsule, large iridectomy: All these conditions are associated with the risk of the implant migration into the anterior chamber, which has been described both for Ozurdex [172] and for Iluvien [173]. The migration of the implant into the anterior chamber can lead to localized or diffuse corneal edema due to endothelial cell loss, which may be related to the chemical toxicity of the implant components or to the mechanical trauma of the rigid device in contact with the cornea [172,173].
- e
- Presence of DME associated with advanced DR or with PDR: Previous studies have shown that both IV anti-VEGF (ranibizumab and aflibercept) [53,54] and IV CSs (TA, Ozurdex, and Iluvien) [46,174,175] used for the treatment of DME were able to simultaneously reduce the risk of DR progression and PDR development. The five-year outcomes of the Bevordex study showed that patients receiving anti-VEGF (bevacizumab) were less likely to develop PDR than those receiving Ozurdex [108], suggesting that anti-VEGF may be superior to CSs because of its greater anti-angiogenic effect. Anti-VEGF agents are currently considered the first-line treatment option in eyes with DME associated with PDR [13,14,15,16,17,18,19].
4.7. Summary of the Efficacy and Safety of the Intravitreal Corticosteroid in DME Management
- a
- Global efficacy and safety profile of intravitreal steroids: The Cochrane Library systematic review published in 2020, including 10 RCTs (4505 eyes) and evaluating the efficacy and safety of IV steroids (TA, DEX, and FAc) as monotherapy for the treatment of DME, concluded that “IV steroids probably are more effective than sham treatment or control, with levels of evidence higher for FAc, lower for DEX and lowest for TA, providing small VA gain (1 ≤ Snellen line) in most studies; they probably are less effective than anti-VEGF in improving BCVA; they are associated with increased risk of cataract development and progression (20% in the control groups and 50–60% in the steroid groups), and may be therefore indicated in pseudophakic eyes; they are associated with IOP elevation (5% in control groups and 30% in steroids groups), need of IOP-lowering medications (1% in control groups and 33% in steroids groups), and need of glaucoma surgery (<1% of controls and 2% in patients treated with steroids); the need of glaucoma surgery is probably higher with FAc)” [176].
- b
- Comparison of the efficacy profile amongst TA, DEX and FAc: A direct comparison amongst TA, DEX, and FA has not yet been performed either in RCTs nor in large real-life studies. Moreover, having a different pharmacokinetic, they should probably not simply be compared but instead utilized in different selected cases. TA and DEX can be considered as an attack treatment, because, once injected, they immediately release an important dose of drug into the vitreal cavity [21]. On the other hand, the FAc implant can be defined as a background therapy because it delivers low concentrations of FAc into the eye for approximately 36 months [21]. The FAc implant aims to stabilize DME and should be injected preferably in DME eyes that respond to steroid therapy [85].
- c
- Comparison of the safety profile amongst TA, DEX, and FAc: The risk for steroid-induced OHT or SIG seems to be higher for FA, lower for TA, and lowest for DEX [74]. Furthermore, Ozurdex [42] is associated with a lesser risk of cataract development as compared with IVTA [46] or Iluvien [40]. These differences may be related to their different gene regulation pattern at the level of the human trabecular meshwork cell lines; moreover, DEX is less lipophilic than TA and FA, with less accumulation in the trabecular meshwork and lens, explaining the reduced incidence of IOP elevation and cataract with Ozurdex [180].
- d
- e
- Rationale of the association of intravitreal steroids and anti-VEGF agents: These drugs have different mechanisms of action and could theoretically work well in combination. A systematic review and meta-analysis of the Cochrane Library published in 2018, which included 8 RCTs for a total of 817 eyes (the majority of which using bevacizumab plus TA), showed that the combination of IV anti-VEGF and steroids does not appear to provide additional visual benefit compared to monotherapy, exposing the patients to the potential side effects of both agents, such as cataract, glaucoma, stroke, and heart attack [183].
5. Guidelines for the Management of DME
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DM | diabetes mellitus |
| DR | diabetic retionopathy |
| DME | diabetic macular edema |
| CSc | corticosteroids |
| TA | triamcinolone acetonide |
| DEX | dexamethasone |
| FAc | fluocinolone acetonide |
| VEGF | vascular endothelial growth factors |
| PPV | pars plana vitrectomy |
| IOP | intraocular pressure |
| BRB | blood-retinal barriers |
| RPE | retinal pigment epithelium |
| CSME | Clinically Significant Macula Edema |
| RCT | randomized controlled trial |
| ETDRS | Early Treatment of Diabetic Retinopathy Study |
| CIDME | center-involved-DME |
| VA | visual acuity |
| BCVA | best corrected visual acuity |
| DRCR.net | Diabetic Retinopathy Clinical Research.Network |
| FAG | fluorescein angiography |
| OCT | optical coherence tomography |
| CRT | central retinal thickness |
Appendix A
| Authors | Treatments | Study Type | Population | Study Focus | Follow-Up | Efficacy | Side Effects | Others |
|---|---|---|---|---|---|---|---|---|
| Beck et al., 2009 (DRCR.net Protocol B) [46] | IVTA 1 mg and 4 mg; focal/gris macular laser | RCT | 840 CIDME eyes (BCVA 20/40–20/230) | Randomized treatment with 1 mg or 4 mg IVTA or focal/grid macular laser | 3 years | Higher VA gain with macular laser as compared to both IVTA groups | In laser, 1-mg and 4-mg IVTA groups, IOP rise (>10 mmHg) in 4%, 18%, and 33% of eyes; cataract surgery needed in 31%, 46%, and 83% of eyes, respectively | IVTA-treated eyes associated with lower rate of DR progression: laser linked with higher risk of macular laser scars and subretinal fibrosis |
| Gillies et al., 2009 [87] | IVTA 4 mg; IV sham | RCT | 69 CIDME eyes | Randomized treatment with 4 mg IVTA or sham, with adjunctive laser treatment where appropriate | 5 years | VA gain and CRT reduction slightly but not significantly higher with IVTA | 45% of the phakic eyes need cataract surgery in IVTA group | Comparable % of eyes requiring laser treatment in the two groups |
| Yilmaz et al., 2009 [79] | IVTA or sub-tenon TA | Systematic review of 6 RCTs | CIDME eyes refractory to laser | IVTA vs. no treatment or vs. TA sub-tenon injections | 6 months | Significant VA gain and CRT reduction with IVTA until month 3, but not at month 6 | Significantly higher IOP in both TA groups at month 3 and 6 | |
| Elman et al., 2010 (DRCR.net Protocol I) [59] | IVTA 4 mg; IV sham; macular laser; IV ranibizumab | RCT | 854 CIDME eyes (BCVA 20/32–20/320) | Randomized treatment with IV sham + prompt laser, 4 mg IVTA + prompt laser or IV ranibizumab + prompt or deferred laser | 5 years | VA gain higher in both ranibizumab groups, and comparable between ranibizumab and TA groups in pseudophakic eyes. CRT reduction similar in TA and ranibizumab groups, and lower in sham group. | As compared with the other groups, TA eyes had IOP elevation (IOP rise ≥ 10 mmHg or IOP > 30 mmHg) in 50% vs. 10%; cataract development in 60% vs. 14%. | |
| Soheilian et al., 2012 [96] | IVTA 4 mg or IV bevacizumab | RCT | 150 CIDME | Randomized treatment with IV bevacizumab or IV bevacizumab + IVTA or grid/focal laser every 3 months as needed | 2 years | Better VA gain in the bevacizumab group at 6 months, comparable results amongst the 3 groups at 2 years; similar CRT reduction | ||
| Kriechbaum et al., 2013 [95] | IVTA 8 mg | RCT | 30 CIDME treatment-naïve eyes | Randomized treatment with 1 IVTA or IV 3 monthly bevacizumab with re-treatment at need | 1 year | BCVA gain higher in the bevacizumab group; CRT reduction similar between groups | Higher cataract development in the TA group | |
| Zajac-Pytrus et al., 2017 [89] | IVTA 20 mg | Prospective interventional study | 110 CIDME eyes treatment-naïve or unresponsive to laser | Evaluation of efficacy and safety of IVTA | 6 months | Significant VA gain and CRT reduction until month 3, but not at month 6 | IOP rise at month 1 and 3 | |
| Arain et al., 2018 [98] | IVTA; IV bevacizumab | Prospective interventional study | 50 pseudophakic eyes with refractory CIDME | Evaluation of efficacy and safety of IVTA + IV bevacizumab | 3 months | Significant VA gain and CRT reduction until month 3 | ||
| Ogura et al., 2019 [80] | Sub-tenon 20 mg TA or 40 mg TA | RCT | 95 CIDME eyes | Evaluation of efficacy and safety of sub-tenon TA 20 mg or 40 mg | 3 months | Significant VA gain and CRT reduction in both groups until month 3 | At month 3, IOP rise in 9% and 13%, and cataract development in 6% and 10% of eyes in the 20-mg TA and 40-mg TA, respectively | |
| Rodrigues et al., 2020 [91] | IVTA 4 mg; IV bevacizumab | RCT | 65 CIDME unresppnsive to 6 monthly IV bevacizumab | Randomized treatment with IVTA 4 mg or IV bevacizumab at need | 1 year | BCVA stable in the bevacizumab group and reduced in the TA group; similar CRT reduction in both groups | Higher risk of IOP rise in TA group | |
| Abdel-Maboud 2021 [92] | IVTA; IV bevacizumab | Systematic review and meta-analysis of 17 RCTs | 1243 CIDME eyes | Randomized treatment with IVTA or IV bevacizumab | 12 months | Higher BCVA gain and CRT reduction with bevacizumab in comparison with TA or TA + bevacizumab | Higher risk of IOP rise with TA | |
| Barakat et al., 2021 [99] | Suprachoroidal TA; IV aflibercept | RCT | 71 treatment-naïve CIDME eyes | Randomized treatment with suprachoroidal TA + IV aflibercept every 3 months or monthly IV aflibercept intravitreal injections | 6 months | Similar VA gain, better CRT reduction in the combination group | Higher local side effect (IOP rise and cataract) in the combination group | Lower number of treatments in the combination group |
| Sorrentino et al., 2021 [90] | IVTA 4 mg | Prospective, interventional, non-comparative real-life | 49 CIDME eyes | Evaluation of efficacy and safety of IVTA | 6 months | Significant VA gain and CRT reduction until month 6 | Moderate IOP rise until month 3, with baseline values at 6 months | |
| Zhang et al., 2021 [97] | IVTA 4 mg; macular laser | Systematic review and meta-analysis of 8 studies (CRT and real-world studies) | 549 CIDME eyes | Comparison of IVTA, macular laser and TA + laser | 1 year | The early-term effect of IVTA + laser similar to IVTA alone but superior to laser alone; the long-term effect of IVTA + laser is similar to IVTA alone or laser alone | Higher risk of cataract and IOP rise associated with IVTA + laser o IVTA alone | Better effect if IVTA is administered before laser treatment |
| Nawar, 2022 [81] | Suprachoroidal TA 4 mg | Prospective nonrandomized interventional | 55 eyes with CIDME refractory to anti-VEGF | Evaluation of efficacy and safety of suprachoroidal TA | 12 months | Significant VA gain and CRT reduction until 12 months | Significant IOP increase at month 1, which returned to baseline values at month 3 | Baseline BCVA and OCT morphology of intra-retinal and outer-retinal layers are predictors of the final BCVA |
| Zhu et al., 2022 [93] | IVTA 4 mg | Prospective RCT | 102 CIDME eyes | Randomized treatment with IVTA or IV aflibercept | 6 months | Higher VA gain and CRT decrease in the aflibercept group | Higher risk of local side effects in the TA group | Humor aqueous level od VEGF and other inflammatory mediators lower in the aflibercept group |
| Authors | Treatments | Study Type | Population | Study Design | Follow-Up | Efficacy | Side Effects | Others |
|---|---|---|---|---|---|---|---|---|
| Callanan et al., 2013 (PLACID study) [100] | 0.7 mg DEX IV implant (Ozurdex) or macular laser | Multicenter RCT | 253 CIDME eyes | Randomized treatment with sham implant + laser or 0.7 mg DEX IV implant + laser | 1 year | higher VA gain at month 1 and 9 with DEX + laser, comparable between groups at 12 months; better morphological outcomes in the DEX + laser group. | 16% vs. 1.6% of eyes required IOP-lowering medication; amongst phakic eyes, 22% vs. 9.5% developed cataract in the DEX + laser and sham + laser groups, respectively. | |
| Boyer et al., 2014 (MEAD study, registration study of the 0.7 mg DEX intravitreal implant, Ozurdex) [42] | 0.35 mg or 0.7 mg DEX IV implant; sham IV injection | Multicenter RCT | 1048 CIDME with BCVA of 20/50–20/200 and CRT ≥ 300 µm 25% of eyes were treatment -naïve | randomized treatment with 0.7 mg or 0.35 mg DEX IV implant or sham procedure Re-treatment no more often than every 6 months | 3 years | Percentage of eyes with ≥15 letters BCVA gain of 22%, 18% and 12% respectively in DEX 0.7-mg, DEX 0.35-mg and sham group; significant CRT reduction in both DEX groups; severe systemic side effects <1% in both DEX and sham groups | IOP rise ≥ 10 mmHg in 28%, 25% and 4% respectively in DEX 0.7-mg, DEX 0.35-mg and sham group; glaucoma surgery in 1.5%, 0.9% and 0.3%; cataract development in 68%, 64% and 20% of phakic eyes, respectively | DEX groups were associated with significant decrease of aqueous inflammatory mediators; mean number of DEX re-treatment: 4/3 years |
| Lam et al., 2015 (CHROME study) [101] | 0.7 mg DEX IV implant (Ozurdex) | Multicentre retrospective observational real-life | 120 eyes with ME of at least 1 year (DME, RVO, uveitis) | Evaluation of efficacy and safety of 0.7 mg DEX IV implant | ≥3 months | Significant VA increase and CRT decrease | IOP rise ≥ 10 mmHg in 21% of eyes; glaucoma surgery in 1.7% of eyes; cataract surgery in 30% of phakic eyes | Re-injection interval time of 2.3–4.9 months |
| Cornish et al., 2016 (BEVORDEX study) [108] | 0.7 mg DEX IV implant (Ozurdex); bevacizumab IV injection | RCT | 68 CIDME eyes | Randomized treatment with Ozurdex implant every 4 months or monthy bevacizumab IV injections as needed | 2 years | Better functional results in bevacizumab group, similar between DEX and bevacizumab in pseudophakic eyes; similar anatomical outcomes | 22% of DEX eyes and 0% of eyes treated with bevacizumab needed IOP-lowering drugs; 37% of DEX group and 6% in the bevacizumab group underwent cataract surgery | Mean number of injections lower in DEX group (2.8 vs. 9.1) |
| Shah et al., 2016 [121] | 0.7 mg DEX IV implant (Ozurdex); bevacizumab IV injection | RCT | 50 eyes with persistent CIDME despite ≥ 3 IV anti-VEGF injections | Randomized treatment with 1 Ozurdex implant or 3 monthy bevacizumab IV injections | 7 months | Similar VA gain; greater CRT reduction in the Ozurdex group | Need of IOP-lowering medication greater in the Ozurdex group | |
| Heng et al., 2016 (OZLASE study) [102] | 0.7 mg DEX IV implant (Ozurdex); macular laser | RCT | 80 CIDME eyes | Randomized treatment with repeated Ozurdex + laser or macular laser | 1 year | VA gain only in the laser group; CRT decrease only in the Ozurdex + laser group | Need of IOP-lowering drugs in 20% of eyes in the Ozurdex + laser groups and 2.5% of eyes in the laser group; 33% of phakic eyes in the Ozurdex + laser group required cataract surgery | |
| Al-Khersan et al., 2017 [109] | 0.7 mg DEX IV implant (Ozurdex) | Multicentre retrospective review of real-life studies | 102 CIDME eyes | Comparison of long-term functional results between eyes with poor (VA gain < 5 letters) and robust response (VA gain ≥ 10 letters) at 3 months | ≥18 months | Early treatment functional response is directly correlated with the overall change in BCVA | n.a. | |
| Callanan et al., 2017 [107] | 0.7 mg DEX IV implant (Ozurdex); bevacizumab IV injection | Multicenter RCT | 163 persistent CIDME eyes with VA of 20/200 and 20/40 and CRT ≥ 300µm | Randomized treatment with Ozurdex implant every 5 months or monthy bevacizumab intravitreal injections as needed | 1 year | Higher VA gain in the bevacizumab group, similar between groups in pseudophakic eyes; better anatomical outcomes with Ozurdex; | IOP elevation respectively in 34.3% of eyes in the DEX group, and 1.6% in the ranibizumab group; cataract development in 9.4% in the DEX group, and 0% in the ranibizumab group. | Mean number of injections lower with Ozurdex (2.8 vs. 8.5 in a year) |
| Malcles et al., 2017 (Reldex study) [103] | 0.7 mg DEX IV implant (Ozurdex) | Prospective observational real-life | 128 DME eyes | Evaluation of efficacy and safety of 0.7 mg DEX IV implant | 3 years | Mean BCVA increase of +9.5 letters; significant CRT decrease | IOP ≥ 25 mmHg in 10% of eyes; cataract surgery in 47% of phakic eyes | mean of 3.6 DEX injections/3 years |
| Malcles et al., 2017 (SAFODEX study) [114] | 0.7 mg DEX IV implant (Ozurdex) | Retrospective observational real-life | 421 ME eyes (DME in 30% of cases, RVO, uveitis) | Evaluation of the safety profile (risk of IOP rise and glaucoma) of Ozurdex IV insert | 3–55 months | n.a. | IOP ≥ 25 mmHg in 20% of eyes; need of IOP-lowering medication in 30% of eyes; glaucoma surgery in 0.4% of cases; risk factors for IOP rise: pre-existing glaucoma treated with 2 or 3 hypotensive drugs | Glaucomatous patients treated with one, two or three hypotensive agents had respectively 37%, 50% and 100% of high responders (i.e IOP rise > 15 mmHg) |
| Sarao et al., 2017 [113] | 0.7 mg DEX IV implant (Ozurdex) | Multicenter RCT | 42 CIDME eyes | Randomized treatment with Ozurdex administration at need or single Ozurdex administration | 6 months | Better functional and anatomical results in the Ozurdex at need treatment group | Comparable safety profile between groups | Mean number of treatments: 1.6/6 months in the Ozurdex at need group |
| Bucolo et al., 2018 [110] | 0.7 mg DEX IV implant (Ozurdex) | Systematic review of real-world studies | 21 studies (831 DME eyes) | Comparison of Ozurdex IV implant every 6 months or at need | 5–23 months | Better functional and anatomical results with implant at need, with mean time of re-treatment of 4–5 months | IOP rise in 15–30% of eyes, no need of glaucoma surgery; cataract development in 10–50% of cases | 1/3 of the eyes were re-treated before six months from the first Ozurdex injection; mean re-treatment time of 5.3 ± 0.9 months; direct relationship between number of re-treatments and DME duration |
| Busch et al., 2018 [131] | 0.7 mg DEX IV implant (Ozurdex); anti-VEGF IV injection | Multicentre retrospective case-control | 110 eyes with DME unresponsive to anti-VEGF | Comparison of efficacy of the switch to Ozurdex after 3 monthly anti-VEGF injection or the prosecution of anti-VEGF therapy | 1 year | VA change of −0.4 letters in the anti-VEGF group and +6.1 letters in the DEX group; CRT change of +18 µm in the anti-VEGF eyes and −93 µm in the DEX eyes | n.a. | |
| He et al., 2018 [120] | 0.7 mg DEX IV implant (Ozurdex); anti-VEGF IV injection | Meta-analysis of RCTs | 4 RCTs (521 DME eyes) | Comparison of efficacy and safety of Ozurdex intravitreal implant vs. anti-VEGF intravitreal injections | 1 year | Ozurdex provided better anatomical outcomes despite significantly lower functional results (cataract development) | Ozurdex was associated with significantly fewer IV injections, higher risk of IOP elevation and cataract development, and lower risk of serious systemic adverse events | Treatment-naive eyes 17% in Ozurdex studies and 2/3 in anti-VEGF studies |
| Kodjikian et al., 2018 [105] | 0.7 mg DEX IV implant (Ozurdex); anti-VEGF IV injection | Systematic review and meta-analysis of real-life studies | 32 studies on anti-VEGF (6842 DME eyes) and 31 studies on Ozurdex IV implant (1703 eyes) | Evaluation of efficacy of Ozurdex IV implant and anti-VEGF IV injections | 6–48 months | Higher VA gain with Ozurdex (mean of +9.6 letters with Ozurdex and +4.4 with anti-VEGF) Better results in naïve eyes with Ozurdex, similar results in naïve and non-naïve with anti-VEGF | n.a. | Mean number of injections per year: 1.6 with Ozurdex and 5.8 with anti-VEGF |
| Maturi et al., 2018 (DRCR.net Protocol U) [115] | 0.7 mg DEX IV implant (Ozurdex); ranibizumab IV injections | RCT | 129 eyes with CIDME refractory to ranibizumab IV injections | Randomized treatment to Ozurdex + ranibizumab or sham + ranibizumab after 3 monthly ranibizumab injections | 2 years | Similar VA gain between groups; higher VA gain in the Ozurdex + ranibizumab in pseudophakic eyes; better morphological results in the Ozurdex + ranibizumab group | Need of IOP-lowering drugs in 30% of eyes in Ozurdex + ranibizumab group and in 0% in sham + ranibizumab group | |
| Castro-Navarro et al., 2019 [111] | 0.7 mg DEX IV implant (Ozurdex) | Retrospective observational real-life | 29 treatment-naïve and 55 non-naïve CIDME eyes | Comparison of efficacy of 0.7 mg DEX IV implant between naïve and refractory DME eyes | 6 months | Better functional results in naïve eyes | 35% of eyes required re-injection between months 3 and 6 post-op | |
| Martinez et al., 2019 [116] | 0.7 mg DEX IV implant (Ozurdex) | Retrospective observational real-life | 69 eyes with CIDME unresponsive to anti-VEGF | Comparison of the efficacy and safety of the switch to Ozurdex after 3 (early switch) or 6 monthly anti-VEGF injections (late switch) | 2 years | Better functional and anatomical results in the “early-switch” group | IOP rise in 10% and 26% of early- and late-switch groups respectively; 10% of phakic eyes required cataract extraction | Mean number of Ozurdex implants: 1.1/2 years in the early- and 1.7/2 years in the late-switch group |
| Rosenblatt et al., 2020 (European DME Registry Study) [104] | 0.7 mg DEX IV implant (Ozurdex) | Multicentre retrospective Observational real-life | 340 naïve-treatment and non-naïve DME eyes | Evaluation of efficacy and safety of 0.7 mg DEX intravitreal implant | 6 months | VA gain of ≥15 letters in 23%, VA gain of ≥10 letters in 38% and VA lost of ≥15 letters in 8% of eyes. Better functional results in naïve eyes, with less DME duration and better glycemic control | IOP rise of >25 mmHg in 8% of eyes | The peak of improvement was achieved 3 months after the injection and dissipated until 6 months |
| Rajesh et al., 2020 (International Ozurdex Study Group) [117] | 0.7 mg DEX IV implant (Ozurdex) | Multicenter retrospective observational real-life | 2736 ME eyes (DME in 52% of cases, RVO, uveitis) | Evaluation of the safety profile of Ozurdex insert | 6–102 months | n.a. | IOP > 25 mmHg in 26% of eyes; 0.5% required glaucoma surgery; cataract development in 47% of cases; 32.5% of eyes required cataract surgery; endophthalmitis, retinal detachment, and vitreous hemorrhages < 0.1% of eyes | |
| Zarranz-Ventura et al., 2020 [112] | 0.7 mg DEX IV implant (Ozurdex) | Retrospective observational real-life | 203 naïve-treatment and non-naïve DME eyes | Comparison of efficacy and safety of 0.7 mg DEX IV implant between treatment-naïve and non-naïve DME eyes | 2 years | Naïve eyes had better functional and anatomical results, with lower number of re-injections and longer time to re-treatment | ||
| Comet et al., 2021 (INVICTUS study) [122] | 0.7 mg DEX IV implant (Ozurdex); ranibizumab IV injection; aflibercept IV injection | Prospective non randomized observation real-life study | 70 treatment-naïve CIDME eyes | Comparison of efficacy of Ozurdex IV implant, ranibizumab or aflibercept IV injection | 1 year | Similar functional results amogst groups; better anatomical outcomes with Ozurdex | n.a. | |
| Veritti et al., 2021 [126] | 0.7 mg DEX IV implant (Ozurdex); anti-VDEGF IV injection | Systematic review and meta-analysis of RCTs and real-life studies | 72 studies (45,032 DME eyes) | Evaluation and comparison of efficacy and safety of Ozurdex IV implant vs. anti-VEGF IV injections | 12 months | VA gain obtained using anti-VEGF agents slightly but not significantly higher in RCTs than observational studies;Ozurdex implant showed significantly better results in observational studies than in RCTs. | With both RCTs and real-life studies, higher functional results with aflibercept as compared to Ozurdex and bevacizumab (similar to ranibizumab); with observational studies only, VA gain similar between anti-VEGF and Ozurdex | |
| Gascon 2022 (INVICOST study) [130] | 0.7 mg DEX IV implant (Ozurdex); ranibizumab IV injection; aflibercept IV injection | Prospective observational | 60 treatment-naïve DME eyes | Comparison of the costs of the treatment with Ozurdex, aflibercept and ranibizumab | 1 year | Ozurdex was significantly less expensive than that with anti-VEGF agents (approximately one half), mostly because of the lower frequency of intravitreal injections | n.a. | |
| Chi et al., 2023 [124] | 0.7 mg DEX IV implant (Ozurdex) | Systematic review and meta-analysis of RCTs and real-life studies | 30 studies (10 RCTs, 3 prospective real-world studies and 17 retrospective real-world studies) 2409 CIDME eyes | Comparison of efficacy and safety of Ozurdex IV implant vs. anti-VEGF IV injections | 1–12 months | Similar functional results in non-resistant or naïve DME eyes, and better results for Ozurdex in resistant DME eyes; anatomical results significantly better for Ozurdex in both resistant and non-resistant DME eyes; | Side effects were comparable between the two groups | |
| Kaya et al., 2023 [119] | 0.7 mg DEX IV implant (Ozurdex); ranibizumab IV injection | Prospective, consecutive clinical interventional | 68 treatment-naïve CIDME eyes with OCT inflammatory biomarkers | Randomized treatment to Ozurdex + ranibizumab or ranibizumab monotherapy | 2 years | VA gain ≥15 letters in 65% and 26% of Ozurdex + ranibizumab and ranibizumab groups respectively; greater CRT decrease in the combination group; | IOP rise ≥5 mmHg and cataract development in 38% and 27% of the combination group, and in 18% and 12% of the ranibizumab monotherapy group | |
| Patil et al., 2023 [123] | 0.7 mg DEX IV implant (Ozurdex); IVTA injection; anti-VEGF IV injection | Systematic review and meta-analysis of RCTs | 14 RCTs (827 DME eyes) | Comparison of efficacy and safety of intravitreal anti-VEGF and steroids (Ozurdex or TA) | 1 year | DEX and TA were associated with comparable functional results and significantly better anatomical outcomes | DEX and TA were associated with significantly higher risk of IOP elevation | |
| Ruiz-Moreno et al., 2023 [132] | 0.7 mg DEX IV implant (Ozurdex) | Multicentre retrospective cost analysis | 108 eyes with CIDME unresponsive to anti-VEGF | Evaluation of the cost-effectiveness of the switch to Ozurdex after 3 (early-switch) or >3 (late-switch) anti-VEGF injections | 1 year | Early switch to Ozurdex is more cost-effective than late-switch |
| Authors | Drug | Study Type | Population | Study Focus | Follow-Up | Efficacy | Side Effects | Others |
|---|---|---|---|---|---|---|---|---|
| Campochiaro et al., 2012 (FAME study, registration study of the 0.2 µg/d FAc IV implant (Iluvien) [40] | 0.2 µg/d or 0.5 µg/d FAc IV implant; IV sham | Multicenter RCT | 956 eyes with persistent CIDME despite macular laser with BCVA of 20/50–20/400 and CRT ≥ 250 µm | Randomized treatment with intravitreal inserts releasing 0.2 µg/day or 0.5 µg/day FAc or sham injection. | 3 years | VA gain ≥ 15 letters in 29%, 28% and 19% in the 0.5 µg/d, 0.2 µg/d and sham group; better results in chronic DME (3 years) | In the 0.5 µg/d FAc, 0.2 µg/d FAc and sham groups: IOP rise ≥ 10 mmHg in 37%, 34% and 10%; need of glaucoma surgery in 8.1%, 4.8% and 0.5%; cataract development in 89%, 82% and 27% of eyes. | Need of adjunctive therapies in 51%, 54% and 95% of the 0.5 µg/d FAc, 0.2 µg/d FAc and sham groups; mean number of re-treatments: 1.3/3 years; Need of glaucoma surgery only in steroid-responders |
| Peto 2017 (Iluvien Clinical Evidence Study (ICE-UK) [133] | 0.2 µg/d FAc IV implant (Iluvien) | Multicentre retrospective observational real-world | 233 eyes with chronic and refractory CIDME | Evaluation of efficacy and safety of Iluvien IV implant | 1 year | Mean VA gain of +3.8 letters; mean CRT decrease of −113 µm | 19% of eyes required IOP-lowering drugs; no need of glaucoma surgery | Significant VA gain only by eyes with baseline VA > 55 letters; eyes with CRT ≥ 400 µm at baseline were more likely to achieve e significant CRT reduction |
| Ch’ng et al., 2018 [147] | 0.2 µg/d FAc IV implant (Iluvien) | Retrospective cost analysis | 14 eyes with refractory CIDMEswitched from IV pharmacotherapy to Iluvien | Evaluation of costs before and after the switch to Iluvien | 3 years | Switch to Iluvien is a cost-saving procedure | n.a. | Switch to Iluvien is a time-saving procedure |
| Eaton et al., 2019 (the USER study) [134] | 0.2 µg/d FAc IV implant (Iluvien) | Retrospective chart review | 160 CIDME eyes (91% non-treatment-naïve) | Evaluation of efficacy and safety of Iluvien IV implant | 3 years | Stable VA for up to 3 years; CRT decrease; significant reduction of CRT fluctuation | IOP ≥ 25 mmHg in 31% of eyes; need of IOP-lowering medication in 24% of eyes; no need of glaucoma surgery | Reduction number of treatment (anti-VEGF or Ozurdex) from 1 every 2.9 months pre-FAc implant to 1 every 14.3 months after-FAc implant; non-steroid-responders to Ozurdex have a probability of 96% of being non-steroid responders to Iluvien |
| Rehak et al., 2019 [136] | 0.2 µg/d FAc IVimplant (Iluvien); 0.7 mg DEX IV implant (Ozurdex) | Retrospective chart review | 59 eyes with CIDME responsive to anti-VEGF and/or Ozurdex but recidivant after stopping treatment | Comparison between switching directly from anti-VEGF to Iluvien and indirectly via Ozurdex to Iluvien after >4 months | 3 years | Significant VA gain similar in both groups (+10.6 and +9.7 letters); significant CRT reduction after 3 months of Iluvien implant and maintained for up to 36 months | IOP rise > 10 mmHg in 26% of eyes; cataract development in 73% of phakic eyes | 37% of eyes required additional treatments |
| Augustin et al., 2020 (Retro-IDEAL study) [135] | 0.2 µg/d FAc IV implant (Iluvien) | Retrospective observational real-world | 81 CIDME eyes unresponsive to anti-VEGF | Evaluation of efficacy and safety of the switch from anti-VEGF to Iluvien IV implant | 3 years | VA gain of +5.5 letters from month 9 and maintained for 3 years; CRT decrease | IOP rise in 27% of eyes managed with IOP-lowering medications | |
| Fallico et al., 2021 [142] | 0.2 µg/d FAc IV implant (Iluvien) | Systematic review and meta-analysis of real-world studies | 9 real-world studies (7 retrospective and 2 prospective) (428 eyes) | Evaluation of efficacy and safety of Iluvien IV implant | 2 years | Significant VA gain and CRT decrease | Need of IOP-lowering drugs in 27% of eyes; need of glaucoma surgery in 3% of cases; cataract extraction in 39% of phakic eyes | Need of supplementary therapies in 39% of eyes |
| Kodjikian et al., 2021 [143] | 0.2 µg/d Fac IV implant (Iluvien) | Systematic review of real-world studies | 22 observational real-world studies (1880 DME eyes) | Evaluation of efficacy and safety of Iluvien IV implant | ≥1 year | mean peak of VA gain of +8.7 letters 1 year post-op; mean CRT decrease of 34% from baseline | IOP rise 20% of eyes; 0.6% required glaucoma surgery; cataract extraction in 43% of phakic eyes | Higher VA gain associated with lower BCVA at baseline and more recent DME |
| Bailey et al., 2022 (Medisof audit study) [138] | 0.2 µg/d FAc IV implant (Iluvien) | Multicenter retrospective observational real-world | 256 eyes with chronic and refractory CIDME (89% psedophakic) | Evaluation of the long-term efficacy and safety of the Iluvien IV implant | 4 years | VA gain ≥5, ≥10 letters and ≥15 letters in 46%, 25% and 17% of eyes respectively; stabilization of the retinal morphology for 4 years. | IOP increase ≥10 mmHg in 29%, use of IOP-lowering medications in 28% and glaucoma surgery in 2.7% of eyes | Mean number of FAc inserts: 1.1/4 years; need of IOP-lowering treatments in 50% of patients with prior history of OHT or glaucoma and 18% of those without |
| Baillif et al., 2022 [139] | 0.2 µg/d FAc IV implant (Iluvien) | Multicenter, retrospective observational | 113 CIDME responsive to Ozurdex without IOP rise | Evaluation of efficacy and safety of the switch from Ozurdex to Iluvien | 1 year | Significant VA gain and CRT decrease | No side effects, IOP ≤ 18 mmHg during the entire follow-up | Need of additional treatments in 33% of eyes; shorter time between last Ozurdex and Iluvien implant (≤8 weeks) associated with reduced CRT fluctuations and reduced need for additional treatments |
| Cicinelli et al., 2022 [137] | 0.2 µg/d FAc IV implant (Iluvien) | Retrospective observational real-life | 54 chronic DME pseudophakic eyes previously treated with Ozurdex | Evaluation of efficacy and safety of the switch from Ozurdex to Iluvien | 1 year | Significant VA gain and CRT reduction | >20-fold risk of IOP rise in eyes showing IOP-elevation post-Ozurdex | Direct correlation between morphological response to Ozurdex and Iluvien; absence of relationship between VA gain post-Ozurdex and post-Iluvien |
| Mathies et al., 2022 (REALFAc study) [140] | 0.2 µg/d FAc IV implant (Iluvien) | Prospective observational real-life | 62 eyes with chronic (mean DME duration of 60 months) refractory CIDME | Evaluation efficacy and safety of the Iluvien IV implant | 1 year | VA gain ≥5 letters in 50% of eyes; CRT decrease; | Need of IOP-lowering medications in 18% of cases | Need of additional treatment in 37% of cases |
| Singer et al., 2022 (PALADIN study) [141] | 0.2 µg/d FAc IV implant (Iluvien) | Prospective, multicentre, observational, non-randomized, open-label | 202 non-steroid-responders CIDME eyes | Evaluation of the long-term efficacy and safety of the Iluvien IV implant | 3 years | mean BCVA increase of +3.6 letters and mean CRT reduction of −60.7 µm, with reduced VA and CRT fluctuation for 3 years | IOP rise ≥10 mmHg in 27.7% of eyes; need of IOP-lowering drugs in 38% of eyes; glaucoma surgery in 1.5% of eyes; cataract surgery in 62% of phakic eyes | Eyes with IOP < 25 mmHg after local steroids had IOP < 25 mmHg after FAc in 97% of cases; need of additional therapy in 75% of eyes, with frequency decrease from 3.5/year before Iluvien to 1.7/year after Iluvien |
| Khoramnia et al., 2023 (ILUVIEN Registry Safety Study—IRISS) [144] | 0.2 µg/d FAc IV implant (Iluvien) | Multicenter, open-label, observational real-world registry study | 695 eyes with chronic CIDME | Evaluation of the long-term efficacy and safety of the Iluvien intravitreal implant | 4 years | Mean VA gain of +5 letters; VA gain ≥15 letters in 18% of eyes | IOP elevation ≥ 10 mmHg in 15% of eyes; need of IOP-lowering medications in 35%; glaucoma surgery in 4.3%; cataract extraction.in 65% of the phakic eyes | Mean number of FAc inserts: 1.1/4 years; need of supplementary therapies in 44% of eyes |
| Roth et al., 2023 [149] | 0.2 µg/d FAc IV implant (Iluvien) | Observational real-world study | 202 CIDME eyes after a successful prior IV steroid challenge | Evaluation of the safety profile of the Iluvien IV implant | 3 years | n.a. | IOP > 25 mmHg in 32% of eyes; IOP >30 mmHg in 16% of cases | Eyes with IOP < 25 mmHg after previous IV steroids had IOP < 25 mmHg after FAc in 78% of cases |
References
- Cloete, L. Diabetes mellitus: An overview of the types, symptoms, complications and management. Nurs. Stand. 2021, 37, 61–66. [Google Scholar] [CrossRef]
- Lovic, D.; Piperidou, A.; Zografou, I.; Grassos, H.; Pittaras, A.; Manolis, A. The Growing Epidemic of Diabetes Mellitus. Curr. Vasc. Pharmacol. 2020, 18, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Riddle, M.C.; Herman, W.H. The Cost of Diabetes Care—An Elephant in the Room. Diabetes Care 2018, 41, 929–932. [Google Scholar] [CrossRef] [PubMed]
- Lin, K.-Y.; Hsih, W.-H.; Lin, Y.-B.; Wen, C.-Y.; Chang, T.-J. Update in the epidemiology, risk factors, screening, and treatment of diabetic retinopathy. J. Diabetes Investig. 2021, 12, 1322–1325. [Google Scholar] [CrossRef] [PubMed]
- Holekamp, N.M. Overview of diabetic macular edema. Am. J. Manag. Care 2016, 22 (Suppl. S10), S284–S291. [Google Scholar] [PubMed]
- Bandello, F.; Battaglia Parodi, M.; Lanzetta, P.; Loewenstein, A.; Massin, P.; Menchini, F.; Veritti, D. Diabetic Macular Edema. Dev. Ophthalmol. 2017, 58, 102–138. [Google Scholar] [CrossRef]
- Yoshimura, T.; Sonoda, K.-H.; Sugahara, M.; Mochizuki, Y.; Enaida, H.; Oshima, Y.; Ueno, A.; Hata, Y.; Yoshida, H.; Ishibashi, T. Comprehensive analysis of inflammatory immune mediators in vitreoretinal diseases. PLoS ONE 2009, 4, e8158. [Google Scholar] [CrossRef] [PubMed]
- Klaassen, I.; Van Noorden, C.J.; Schlingemann, R.O. Molecular basis of the inner blood-retinal barrier and its breakdown in diabetic macular edema and other pathological conditions. Prog. Retin. Eye Res. 2013, 34, 19–48. [Google Scholar] [CrossRef]
- Romero-Aroca, P.; Baget-Bernaldiz, M.; Pareja-Rios, A.; Lopez-Galvez, M.; Navarro-Gil, R.; Verges, R. Diabetic Macular Edema Pathophysiology: Vasogenic versus Inflammatory. J. Diabetes Res. 2016, 2016, 2156273. [Google Scholar] [CrossRef]
- Daruich, A.; Matet, A.; Moulin, A.; Kowalczuk, L.; Nicolas, M.; Sellam, A.; Rothschild, P.-R.; Omri, S.; Gélizé, E.; Jonet, L.; et al. Mechanisms of macular edema: Beyond the surface. Prog. Retin. Eye Res. 2018, 63, 20–68. [Google Scholar] [CrossRef]
- Starace, V.; Battista, M.; Brambati, M.; Cavalleri, M.; Bertuzzi, F.; Amato, A.; Lattanzio, R.; Bandello, F.; Cicinelli, M.V. The role of inflammation and neurodegeneration in diabetic macular edema. Ther. Adv. Ophthalmol. 2021, 13, 25158414211055963. [Google Scholar] [CrossRef]
- Zhang, J.; Zhang, J.; Zhang, C.; Zhang, J.; Gu, L.; Luo, D.; Qiu, Q. Diabetic Macular Edema: Current Understanding, Molecular Mechanisms and Therapeutic Implications. Cells 2022, 11, 3362. [Google Scholar] [CrossRef]
- Puliafito, C.A.; Cousins, S.W.; Bacharach, J.; Gonzalez, V.H.; Holekamp, N.M.; Merrill, P.T.; Ohr, M.P.; Parrish, R.K., 2nd; Riemann, C.D. Forming a Consensus: Data and Guidance for Physicians Treating Diabetic Macular Edema. Ophthalmic Surg. Lasers Imaging Retin. 2016, 47 (Suppl. S4), S4–S15. [Google Scholar] [CrossRef]
- Schmidt-Erfurth, U.; Garcia-Arumi, J.; Bandello, F.; Berg, K.; Chakravarthy, U.; Gerendas, B.S.; Jonas, J.; Larsen, M.; Tadayoni, R.; Loewenstein, A. Guidelines for the Management of Diabetic Macular Edema by the European Society of Retina Specialists (EURETINA). Ophthalmologica 2017, 237, 185–222. [Google Scholar] [CrossRef]
- Browning, D.J.; Stewart, M.W.; Lee, C. Diabetic macular edema: Evidence-based management. Indian J. Ophthalmol. 2018, 66, 1736–1750. [Google Scholar] [CrossRef]
- Kodjikian, L.; Bellocq, D.; Bandello, F.; Loewenstein, A.; Chakravarthy, U.; Koh, A.; Augustin, A.; de Smet, M.D.; Chhablani, J.; Tufail, A.; et al. First-line treatment algorithm and guidelines in center-involving diabetic macular edema. Eur. J. Ophthalmol. 2019, 29, 573–584. [Google Scholar] [CrossRef] [PubMed]
- Amoaku, W.M.; Ghanchi, F.; Bailey, C.; Banerjee, S.; Banerjee, S.; Downey, L.; Gale, R.; Hamilton, R.; Khunti, K.; Posner, E.; et al. Diabetic retinopathy and diabetic macular oedema pathways and management: UK Consensus Working Group. Eye 2020, 34 (Suppl. S1), 1–51, Erratum in Eye 2020, 34, 1941–1942. [Google Scholar] [CrossRef]
- Chhablani, J.; Wong, K.M.; Tan, G.S.F.; Sudhalkar, A.M.; Laude, A.F.; Cheung, C.M.G.F.M.; Zhao, P.F.; Uy, H.; Lim, J.; Valero, S.M.; et al. Diabetic Macular Edema Management in Asian Population: Expert Panel Consensus Guidelines. Asia-Pac. J. Ophthalmol. 2020, 9, 426–434. [Google Scholar] [CrossRef]
- Giridhar, S.; Verma, L.; Rajendran, A.; Bhend, M.; Goyal, M.; Ramasamy, K.; Rajalakshmi; Padmaja, R.; Natarajan, S.; Palanivelu, M.S.; et al. Diabetic macular edema treatment guidelines in India: All India Ophthalmological Society Diabetic Retinopathy Task Force and Vitreoretinal Society of India consensus statement. Indian J. Ophthalmol. 2021, 69, 3076–3086. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Wang, N.; Schachat, A.P.; Bao, S.; Gillies, M. Glucocorticoids: Structure, signaling and molecular mechanisms in the treatment of diabetic retinopathy and diabetic macular edema. Curr. Mol. Med. 2014, 14, 376–384. [Google Scholar] [CrossRef] [PubMed]
- Whitcup, S.M.; Cidlowski, J.A.; Csaky, K.G.; Ambati, J. Pharmacology of Corticosteroids for Diabetic Macular Edema. Investig. Ophthalmol. Vis. Sci. 2018, 59, 1–12. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- Anonymous. Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Early Treatment Diabetic Retinopathy Study research group. Arch. Ophthalmol. 1985, 103, 1796–1806. [Google Scholar]
- Klein, R.; Klein, B.E.; Moss, S.E.; Cruickshanks, K.J. The Wisconsin Epidemiologic Study of Diabetic Retinopathy. XV. The long-term incidence of macular edema. Ophthalmology 1995, 102, 7–16. [Google Scholar] [CrossRef]
- Damaskos, C.; Garmpis, N.; Kollia, P.; Mitsiopoulos, G.; Barlampa, D.; Drosos, A.; Patsouras, A.; Gravvanis, N.; Antoniou, V.; Litos, A.; et al. Assessing Cardiovascular Risk in Patients with Diabetes: An Update. Curr. Cardiol. Rev. 2020, 16, 266–274. [Google Scholar] [CrossRef]
- Baker, C.W.; Glassman, A.R.; Beaulieu, W.T.; Antoszyk, A.N.; Browning, D.J.; Chalam, K.V.; Grover, S.; Jampol, L.M.; Jhaveri, C.D.; Melia, M.; et al. Effect of Initial Management With Aflibercept vs. Laser Photocoagulation vs. Observation on Vision Loss Among Patients With Diabetic Macular Edema Involving the Center of the Macula and Good Visual Acuity: A Randomized Clinical Trial. JAMA 2019, 321, 1880–1894. [Google Scholar] [CrossRef] [PubMed]
- Murakami, T.; Yoshimura, N. Structural changes in individual retinal layers in diabetic macular edema. J. Diabetes Res. 2013, 2013, 920713. [Google Scholar] [CrossRef]
- Acón, D.; Wu, L. Multimodal Imaging in Diabetic Macular Edema. Asia-Pac. J. Ophthalmol. 2018, 7, 22–27. [Google Scholar] [CrossRef]
- Huang, Z.; Qiu, K.; Yi, J.; Lin, H.; Zheng, D.; Huang, D.; Zhang, G.; Chen, H.; Zheng, J.; Wang, Y.; et al. Diabetic retinopathy with extensively large area of capillary non-perfusion: Characteristics and treatment outcomes. BMC Ophthalmol. 2022, 22, 293. [Google Scholar] [CrossRef] [PubMed]
- Virgili, G.; Menchini, F.; Casazza, G.; Hogg, R.; Das, R.R.; Wang, X.; Michelessi, M. Optical coherence tomography (OCT) for detection of macular oedema in patients with diabetic retinopathy. Cochrane Database Syst. Rev. 2015, 1, CD008081. [Google Scholar] [CrossRef]
- Im, J.H.; Jin, Y.-P.; Chow, R.; Yan, P. Prevalence of diabetic macular edema based on optical coherence tomography in people with diabetes: A systematic review and meta-analysis. Surv. Ophthalmol. 2022, 67, 1244–1251. [Google Scholar] [CrossRef]
- Munk, M.R.; Somfai, G.M.; de Smet, M.D.; Donati, G.; Menke, M.N.; Garweg, J.G.; Ceklic, L. The Role of Intravitreal Corticosteroids in the Treatment of DME: Predictive OCT Biomarkers. Int. J. Mol. Sci. 2022, 23, 7585. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Moon, B.G.; Cho, A.R.; Yoon, Y.H. Optical Coherence Tomography Angiography of DME and Its Association with Anti-VEGF Treatment Response. Ophthalmology 2016, 123, 2368–2375. [Google Scholar] [CrossRef] [PubMed]
- Tranos, P.G.; Wickremasinghe, S.S.; Stangos, N.T.; Topouzis, F.; Tsinopoulos, I.; Pavesio, C.E. Macular edema. Surv. Ophthalmol. 2004, 49, 470–490. [Google Scholar] [CrossRef]
- Apte, R.S.; Chen, D.S.; Ferrara, N. VEGF in Signaling and Disease: Beyond Discovery and Development. Cell 2019, 176, 1248–1264. [Google Scholar] [CrossRef] [PubMed]
- Sohn, E.H.; van Dijk, H.W.; Jiao, C.; Kok, P.H.B.; Jeong, W.; Demirkaya, N.; Garmager, A.; Wit, F.; Kucukevcilioglu, M.; van Velthoven, M.E.J.; et al. Retinal neurodegeneration may precede microvascular changes characteristic of diabetic retinopathy in diabetes mellitus. Proc. Natl. Acad. Sci. USA 2016, 113, E2655–E2664. [Google Scholar] [CrossRef] [PubMed]
- Gurreri, A.; Pazzaglia, A. Diabetic Macular Edema: State of Art and Intraocular Pharmacological Approaches. Adv. Exp. Med. Biol. 2021, 1307, 375–389. [Google Scholar] [CrossRef] [PubMed]
- Tatsumi, T. Current Treatments for Diabetic Macular Edema. Int. J. Mol. Sci. 2023, 24, 9591. [Google Scholar] [CrossRef] [PubMed]
- Dugel, P.U.; Hillenkamp, J.; Sivaprasad, S.; Vögeler, J.; Mousseau, M.-C.; Wenzel, A.; Margaron, P.; Hashmonay, R.; Massin, P. Baseline visual acuity strongly predicts visual acuity gain in patients with diabetic macular edema following anti-vascular endothelial growth factor treatment across trials. Clin. Ophthalmol. 2016, 10, 1103–1110. [Google Scholar] [CrossRef]
- Campochiaro, P.A.; Brown, D.M.; Pearson, A.; Chen, S.; Boyer, D.; Ruiz-Moreno, J.; Garretson, B.; Gupta, A.; Hariprasad, S.M.; Bailey, C.; et al. Sustained delivery fluocinolone acetonide vitreous inserts provide benefit for at least 3 years in patients with diabetic macular edema. Ophthalmology 2012, 119, 2125–2132. [Google Scholar] [CrossRef]
- Nguyen, Q.D.; Brown, D.M.; Marcus, D.M.; Boyer, D.S.; Patel, S.; Feiner, L.; Gibson, A.; Sy, J.; Rundle, A.C.; Hopkins, J.J.; et al. Ranibizumab for diabetic macular edema: Results from 2 phase III randomized trials: RISE and RIDE. Ophthalmology 2012, 119, 789–801. [Google Scholar] [CrossRef] [PubMed]
- Boyer, D.S.; Yoon, Y.H.; Belfort, R., Jr.; Bandello, F.; Maturi, R.K.; Augustin, A.J.; Li, X.-Y.; Cui, H.; Hashad, Y.; Whitcup, S.M.; et al. Three-Year, randomized, sham-controlled trial of dexamethasone intravitreal implant in patients with diabetic macular edema. Ophthalmology 2014, 121, 1904–1914. [Google Scholar] [CrossRef] [PubMed]
- Korobelnik, J.-F.; Do, D.V.; Schmidt-Erfurth, U.; Boyer, D.S.; Holz, F.G.; Heier, J.S.; Midena, E.; Kaiser, P.K.; Terasaki, H.; Marcus, D.M.; et al. Intravitreal aflibercept for diabetic macular edema. Ophthalmology 2014, 121, 2247–2254. [Google Scholar] [CrossRef] [PubMed]
- Diabetes Control and Complications Trial Research Group. Progression of retinopathy with intensive versus conventional treatment in the Diabetes Control and Complications Trial. Ophthalmology 1995, 102, 647–661. [Google Scholar] [CrossRef] [PubMed]
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998, 352, 837–853, Erratum in Lancet 1999, 354, 602. [Google Scholar]
- Diabetic Retinopathy Clinical Research Network (DRCR.net); Beck, R.W.; Edwards, A.R.; Aiello, L.P.; Bressler, N.M.; Ferris, F.; Glassman, A.R.; Hartnett, E.; Ip, M.S.; Kim, J.E.; et al. Three-year follow-up of a randomized trial comparing focal/grid photocoagulation and intravitreal triamcinolone for diabetic macular edema. Arch Ophthalmol. 2009, 127, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Sabal, B.; Teper, S.; Wylęgała, E. Subthreshold Micropulse Laser for Diabetic Macular Edema: A Review. J. Clin. Med. 2022, 12, 274. [Google Scholar] [CrossRef]
- Lois, N.; Campbell, C.; Waugh, N.; Azuara-Blanco, A.; Maredza, M.; Mistry, H.; McAuley, D.; Acharya, N.; Aslam, T.M.; Bailey, C.; et al. Diabetic Macular Edema and Diode Subthreshold Micropulse Laser: A Randomized Double-Masked Noninferiority Clinical Trial. Ophthalmology 2023, 130, 14–27. [Google Scholar] [CrossRef]
- Jackson, T.L.; Nicod, E.; Angelis, A.; Grimaccia, F.; Pringle, E.; Kanavos, P. Pars plana vitrectomy for diabetic macular edema: A Systematic Review, Meta-Analysis, and Synthesis of Safety Literature. Retina 2017, 37, 886–895. [Google Scholar] [CrossRef]
- Khattab, A.A.A.; Ahmed, M.M.; Hammed, A.H. Pars plana vitrectomy for tractional diabetic macular edema with or without internal limiting membrane peeling. Med. Hypothesis Discov. Innov. Ophthalmol. 2022, 11, 110–118. [Google Scholar] [CrossRef]
- Fogli, S.; Del Re, M.; Rofi, E.; Posarelli, C.; Figus, M.; Danesi, R. Clinical pharmacology of intravitreal anti-VEGF drugs. Eye 2018, 32, 1010–1020. [Google Scholar] [CrossRef]
- Rajendram, R.; Fraser-Bell, S.; Kaines, A.; Michaelides, M.; Hamilton, R.D.; Degli Esposti, S.; Peto, T.; Egan, C.; Bunce, C.; Leslie, R.D.; et al. A 2-year prospective randomized controlled trial of intravitreal bevacizumab or laser therapy (BOLT) in the management of diabetic macular edema: 24-month data: Report 3. Arch. Ophthalmol. 2012, 130, 972–979. [Google Scholar] [CrossRef] [PubMed]
- Reddy, R.K.; Pieramici, D.J.; Gune, S.; Ghanekar, A.; Lu, N.; Quezada-Ruiz, C.; Baumal, C.R. Efficacy of Ranibizumab in Eyes with Diabetic Macular Edema and Macular Nonperfusion in RIDE and RISE. Ophthalmology 2018, 125, 1568–1574. [Google Scholar] [CrossRef] [PubMed]
- Heier, J.S.; Korobelnik, J.-F.; Brown, D.M.; Schmidt-Erfurth, U.; Do, D.V.; Midena, E.; Boyer, D.S.; Terasaki, H.; Kaiser, P.K.; Marcus, D.M.; et al. Intravitreal Aflibercept for Diabetic Macular Edema: 148-Week Results from the VISTA and VIVID Studies. Ophthalmology 2016, 123, 2376–2385. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.P.; Barakat, M.R.; Ip, M.S.; Wykoff, C.C.; Eichenbaum, D.A.; Joshi, S.; Warrow, D.; Sheth, V.S.; Stefanickova, J.; Kim, Y.S.; et al. Efficacy and Safety of Brolucizumab for Diabetic Macular Edema: The KINGFISHER Randomized Clinical Trial. JAMA Ophthalmol. 2023, 141, 1152. [Google Scholar] [CrossRef] [PubMed]
- Wykoff, C.C.; Abreu, F.; Adamis, A.P.; Basu, K.; Eichenbaum, D.A.; Haskova, Z.; Lin, H.; Loewenstein, A.; Mohan, S.; Pearce, I.A.; et al. Efficacy, durability, and safety of intravitreal faricimab with extended dosing up to every 16 weeks in patients with diabetic macular oedema (YOSEMITE and RHINE): Two randomised, double-masked, phase 3 trials. Lancet 2022, 399, 741–755. [Google Scholar] [CrossRef] [PubMed]
- Virgili, G.; Parravano, M.; Evans, J.R.; Gordon, I.; Lucenteforte, E. Anti-vascular endothelial growth factor for diabetic macular oedema: A network meta-analysis. Cochrane Database Syst. Rev. 2017, 6, CD007419, Update in Cochrane Database Syst. Rev. 2018, 10, CD007419. [Google Scholar] [CrossRef]
- Gonzalez, V.H.; Campbell, J.; Holekamp, N.M.; Kiss, S.; Loewenstein, A.; Augustin, A.J.; Ma, J.; Ho, A.C.; Patel, V.; Whitcup, S.M.; et al. Early and Long-Term Responses to Anti–Vascular Endothelial Growth Factor Therapy in Diabetic Macular Edema: Analysis of Protocol I Data. Am. J. Ophthalmol. 2016, 172, 72–79. [Google Scholar] [CrossRef]
- Diabetic Retinopathy Clinical Research Network; Elman, M.J.; Aiello, L.P.; Beck, R.W.; Bressler, N.M.; Bressler, S.B.; Edwards, A.R.; Ferris, F.L., 3rd; Friedman, S.M.; Glassman, A.R.; et al. Randomized trial evaluating ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology 2010, 117, 1064–1077.e35. [Google Scholar] [CrossRef]
- Bressler, N.M.; Beaulieu, W.T.; Glassman, A.R.; Blinder, K.J.; Bressler, S.B.; Jampol, L.M.; Melia, M.; Wells, J.A., 3rd. Diabetic Retinopathy Clinical Research Network Persistent Macular Thickening Following Intravitreous Aflibercept, Bevacizumab, or Ranibizumab for Central-Involved Diabetic Macular Edema With Vision Impairment: A Secondary Analysis of a Randomized Clinical Trial. JAMA Ophthalmol. 2018, 136, 257–269, Erratum in JAMA Ophthalmol. 2018, 136, 601. [Google Scholar] [CrossRef] [PubMed]
- Glassman, A.R.; Wells, J.A., 3rd; Josic, K.; Maguire, M.G.; Antoszyk, A.N.; Baker, C.; Beaulieu, W.T.; Elman, M.J.; Jampol, L.M.; Sun, J.K. Five-Year Outcomes after Initial Aflibercept, Bevacizumab, or Ranibizumab Treatment for Diabetic Macular Edema (Protocol T Extension Study). Ophthalmology 2020, 127, 1201–1210. [Google Scholar] [CrossRef]
- Starr, M.R.; Salabati, M.; Mahmoudzadeh, R.; Patel, L.G.; Ammar, M.J.; Hsu, J.; Garg, S.; Ho, A.C.; Kuriyan, A.E. Fluctuations in Central Subfield Thickness Associated With Worse Visual Outcomes in Patients With Diabetic Macular Edema in Clinical Trial Setting. Am. J. Ophthalmol. 2021, 232, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Wang, V.Y.; Kuo, B.L.; Chen, A.X.; Wang, K.; Greenlee, T.E.; Conti, T.F.; Singh, R.P. Fluctuations in macular thickness in patients with diabetic macular oedema treated with anti-vascular endothelial growth factor agents. Eye 2022, 36, 1461–1467. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.; Patel, S.N.; Chaudhary, V.; Garg, S.J. Complications of intravitreal injections: 2022. Curr. Opin. Ophthalmol. 2022, 33, 137–146. [Google Scholar] [CrossRef] [PubMed]
- Porta, M.; Striglia, E. Intravitreal anti-VEGF agents and cardiovascular risk. Intern. Emerg. Med. 2020, 15, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Zehden, J.A.; Mortensen, X.M.; Reddy, A.; Zhang, A.Y. Systemic and Ocular Adverse Events with Intravitreal Anti-VEGF Therapy Used in the Treatment of Diabetic Retinopathy: A Review. Curr. Diabetes Rep. 2022, 22, 525–536. [Google Scholar] [CrossRef] [PubMed]
- Adcock, I.M.; Mumby, S. Glucocorticoids. Handb. Exp. Pharmacol. 2017, 237, 171–196. [Google Scholar] [CrossRef] [PubMed]
- Kapugi, M.; Cunningham, K. Corticosteroids. Orthop. Nurs. 2019, 38, 336–339. [Google Scholar] [CrossRef] [PubMed]
- Jonas, J.B.; Söfker, A. Intraocular injection of crystalline cortisone as adjunctive treatment of diabetic macular edema. Am. J. Ophthalmol. 2001, 132, 425–427. [Google Scholar] [CrossRef]
- Jusufbegovic, D.; Schaal, S. Quiescent herpes simplex keratitis reactivation after intravitreal injection of dexamethasone implant. Retin. Cases Brief Rep. 2017, 11, 296–297. [Google Scholar] [CrossRef]
- Nicholson, B.P.; Atchison, E.; Idris, A.A.; Bakri, S.J. Central serous chorioretinopathy and glucocorticoids: An update on evidence for association. Surv. Ophthalmol. 2018, 63, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Araki, T.; Ishikawa, H.; Iwahashi, C.; Niki, M.; Mitamura, Y.; Sugimoto, M.; Kondo, M.; Kinoshita, T.; Nishi, T.; Ueda, T.; et al. Central serous chorioretinopathy with and without steroids: A multicenter survey. PLoS ONE 2019, 14, e0213110. [Google Scholar] [CrossRef] [PubMed]
- Kačmar, J.; Cholevík, D. Corticosteroid Induced Posterior Subcapsular Cataract. Czech Slovak Ophthalmol. 2019, 74, 226–232. (In English) [Google Scholar] [CrossRef] [PubMed]
- Roberti, G.; Oddone, F.; Agnifili, L.; Katsanos, A.; Michelessi, M.; Mastropasqua, L.; Quaranta, L.; Riva, I.; Tanga, L.; Manni, G. Steroid-induced glaucoma: Epidemiology, pathophysiology, and clinical management. Surv. Ophthalmol. 2020, 65, 458–472. [Google Scholar] [CrossRef] [PubMed]
- Ulavíková, Z.; Anwarzai, J.; Krásnik, V. Acute retinal necrosis after intravitreal dexamethasone implant. A case report. Cesk. Slov. Oftalmol. 2022, 78, 144–148. (In English) [Google Scholar]
- Armaly, M.F.; Becker, B. Intraocular pressure response to topical corticosteroids. Fed. Proc. 1965, 24, 1274–1278. [Google Scholar] [PubMed]
- Sohn, H.J.; Han, D.H.; Kim, I.T.; Oh, I.K.; Kim, K.H.; Lee, D.Y.; Nam, D.H. Changes in aqueous concentrations of various cytokines after intravitreal triamcinolone versus bevacizumab for diabetic macular edema. Am. J. Ophthalmol. 2011, 152, 686–694. [Google Scholar] [CrossRef] [PubMed]
- Hauser, D.; Bukelman, A.; Pokroy, R.; Katz, H.; Len, A.; Thein, R.; Parness-Yossifon, R.; Pollack, A. Intravitreal triamcinolone for diabetic macular edema: Comparison of 1, 2, and 4 mg. Retina 2008, 28, 825–830. [Google Scholar] [CrossRef]
- Yilmaz, T.; Weaver, C.D.; Gallagher, M.J.; Cordero-Coma, M.; Cervantes-Castaneda, R.A.; Klisovic, D.; Lavaque, A.J.; Larson, R.J. Intravitreal triamcinolone acetonide injection for treatment of refractory diabetic macular edema: A systematic review. Ophthalmology 2009, 116, 902–911; quiz 912–913. [Google Scholar] [CrossRef]
- Ogura, Y.; Shimura, M.; Iida, T.; Sakamoto, T.; Yoshimura, N.; Yamada, M.; Ishibashi, T. Phase II/III Clinical Trial of Sub-Tenon Injection of Triamcinolone Acetonide (WP-0508ST) for Diabetic Macular Edema. Ophthalmologica 2019, 241, 161–169. [Google Scholar] [CrossRef]
- Nawar, A.E. Effectiveness of Suprachoroidal Injection of Triamcinolone Acetonide in Resistant Diabetic Macular Edema Using a Modified Microneedle. Clin. Ophthalmol. 2022, 16, 3821–3831. [Google Scholar] [CrossRef]
- Chang-Lin, J.-E.; Attar, M.; Acheampong, A.A.; Robinson, M.R.; Whitcup, S.M.; Kuppermann, B.D.; Welty, D. Pharmacokinetics and pharmacodynamics of a sustained-release dexamethasone intravitreal implant. Investig. Ophthalmol. Vis. Sci. 2011, 52, 80–86. [Google Scholar] [CrossRef]
- Campochiaro, P.A.; Nguyen, Q.D.; Hafiz, G.; Bloom, S.; Brown, D.M.; Busquets, M.; Ciulla, T.; Feiner, L.; Sabates, N.; Billman, K.; et al. Aqueous levels of fluocinolone acetonide after administration of fluocinolone acetonide inserts or fluocinolone acetonide implants. Ophthalmology 2013, 120, 583–587. [Google Scholar] [CrossRef]
- Fusi-Rubiano, W.; Blow, R.R.; Lane, M.; Morjaria, R.; Denniston, A.K. Iluvien™ (Fluocinolone Acetonide 0.19 mg Intravitreal Implant) in the Treatment of Diabetic Macular Edema: A Review. Ophthalmol. Ther. 2018, 7, 293–305, Erratum in Ophthalmol. Ther. 2020, 9, 205. [Google Scholar] [CrossRef] [PubMed]
- Kodjikian, L.; Bandello, F.; de Smet, M.; Dot, C.; Zarranz-Ventura, J.; Loewenstein, A.; Sudhalkar, A.; Bilgic, A.; Cunha-Vaz, J.; Dirven, W.; et al. Fluocinolone acetonide implant in diabetic macular edema: International experts’ panel consensus guidelines and treatment algorithm. Eur. J. Ophthalmol. 2022, 32, 1890–1899. [Google Scholar] [CrossRef] [PubMed]
- Audren, F.; Tod, M.; Massin, P.; Benosman, R.; Haouchine, B.; Erginay, A.; Caulin, C.; Gaudric, A.; Bergmann, J.-F. Pharmacokinetic–pharmacodynamic modeling of the effect of triamcinolone acetonide on central macular thickness in patients with diabetic macular edema. Investig. Ophthalmol. Vis. Sci. 2004, 45, 3435–3441. [Google Scholar] [CrossRef] [PubMed]
- Gillies, M.C.; Simpson, J.M.; Gaston, C.; Hunt, G.; Ali, H.; Zhu, M.; Sutter, F. Five-year results of a randomized trial with open-label extension of triamcinolone acetonide for refractory diabetic macular edema. Ophthalmology 2009, 116, 2182–2187. [Google Scholar] [CrossRef] [PubMed]
- Aceves-Franco, L.A.; Sanchez-Aguilar, O.E.; Barragan-Arias, A.R.; Ponce-Gallegos, M.A.; Navarro-Partida, J.; Santos, A. The Evolution of Triamcinolone Acetonide Therapeutic Use in Retinal Diseases: From Off-Label Intravitreal Injection to Advanced Nano-Drug Delivery Systems. Biomedicines 2023, 11, 1901. [Google Scholar] [CrossRef] [PubMed]
- Zając-Pytrus, H.M.; Kaczmarek, R.; Strońska-Lipowicz, D.; Pomorska, M.; Misiuk-Hojło, M. Theeffects and safety of intravitreal triamcinolone injections in the treatment of diabetic macular edema. Adv. Clin. Exp. Med. 2017, 26, 45–49. [Google Scholar] [CrossRef] [PubMed]
- Sorrentino, F.S.; Bonifazzi, C.; Parmeggiani, F. Diabetic macular edema: Safe and effective treatment with intravitreal triamcinolone acetonide (Taioftal). PLoS ONE 2021, 16, e0257695. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, M.W.; Cardillo, J.A.; Messias, A.; Siqueira, R.C.; Scott, I.U.; Jorge, R. Bevacizumab versus triamcinolone for persistent diabetic macular edema: A randomized clinical trial. Graefes Arch. Clin. Exp. Ophthalmol. 2020, 258, 479–490. [Google Scholar] [CrossRef]
- Abdel-Maboud, M.; Menshawy, E.; Bahbah, E.I.; Outani, O.; Menshawy, A. Intravitreal bevacizumab versus intravitreal triamcinolone for diabetic macular edema–Systematic review, meta-analysis and meta-regression. PLoS ONE 2021, 16, e0245010. [Google Scholar] [CrossRef]
- Zhu, Y.; Li, J.; Yu, S.; Mao, B.; Ying, J. Clinical Comparative Study of Intravitreal Injection of Triamcinolone Acetonide and Aflibercept in the Treatment of Diabetic Retinopathy Cystoid Macular Edema. Emerg. Med. Int. 2022, 2022, 1348855. [Google Scholar] [CrossRef]
- Jain, S.; Thompson, J.R.; Foot, B.; Tatham, A.; Eke, T. Severe intraocular pressure rise following intravitreal triamcinolone: A national survey to estimate incidence and describe case profiles. Eye 2014, 28, 399–401. [Google Scholar] [CrossRef]
- Kriechbaum, K.; Prager, S.; Mylonas, G.; Scholda, C.; Rainer, G.; Funk, M.; Kundi, M.; Schmidt-Erfurth, U.; Diabetic Retinopathy Research Group. Intravitreal bevacizumab (Avastin) versus triamcinolone (Volon A) for treatment of diabetic macular edema: One-year results. Eye 2014, 28, 9–15; quiz 16. [Google Scholar] [CrossRef] [PubMed]
- Soheilian, M.; Garfami, K.H.; Ramezani, A.; Yaseri, M.; Peyman, G.A. Two-year results of a randomized trial of intravitreal bevacizumab alone or combined with triamcinolone versus laser in diabetic macular edema. Retina 2012, 32, 314–321. [Google Scholar] [CrossRef]
- Zhang, L.; Chen, X. Efficacy and safety of triamcinolone acetonide injection combined with laser photocoagulation in the treatment of diabetic macular edema: A systematic review and meta-analysis. Ann. Palliat. Med. 2021, 10, 12467–12477. [Google Scholar] [CrossRef] [PubMed]
- Arain, M.A.; Muzaffar, W.; Farooq, O.; Azhar, M.N. Combined Intravitreal Triamcenolone Acetonide and Bevacizumab for Refractory Diabetic Macular Edema. J. Coll. Physicians Surg. Pak. 2018, 28, 603–606. [Google Scholar] [CrossRef] [PubMed]
- Barakat, M.R.; Wykoff, C.C.; Gonzalez, V.; Hu, A.; Marcus, D.; Zavaleta, E.; Ciulla, T.A. Suprachoroidal CLS-TA plus Intravitreal Aflibercept for Diabetic Macular Edema: A Randomized, Double-Masked, Parallel-Design, Controlled Study. Ophthalmol. Retin. 2021, 5, 60–70. [Google Scholar] [CrossRef]
- Callanan, D.G.; Gupta, S.; Boyer, D.S.; Ciulla, T.A.; Singer, M.A.; Kuppermann, B.D.; Liu, C.-C.; Li, X.-Y.; Hollander, D.A.; Schiffman, R.M.; et al. Dexamethasone intravitreal implant in combination with laser photocoagulation for the treatment of diffuse diabetic macular edema. Ophthalmology 2013, 120, 1843–1851. [Google Scholar] [CrossRef]
- Lam, W.-C.; Albiani, D.; Yoganathan, P.; Chen, J.C.; Kherani, A.; Maberley, D.; Oliver, A.; Rabinovitch, T.; Sheidow, T.G.; Tourville, E.; et al. Real-world assessment of intravitreal dexamethasone implant (0.7 mg) in patients with macular edema: The CHROME study. Clin. Ophthalmol. 2015, 9, 1255–1268. [Google Scholar] [CrossRef]
- Heng, L.Z.; Sivaprasad, S.; Crosby-Nwaobi, R.; Saihan, Z.; Karampelas, M.; Bunce, C.; Peto, T.; Hykin, P.G. A prospective randomised controlled clinical trial comparing a combination of repeated intravitreal Ozurdex and macular laser therapy versus macular laser only in centre-involving diabetic macular oedema (OZLASE study). Br. J. Ophthalmol. 2016, 100, 802–807. [Google Scholar] [CrossRef]
- Malclès, A.; Dot, C.; Voirin, N.; Agard, E.; Vié, A.-L.; Bellocq, D.; Denis, P.; Kodjikian, L. Real-life study in diabetic macular edema treated with dexamethasone implant: The reldex study. Retina 2017, 37, 753–760. [Google Scholar] [CrossRef]
- Rosenblatt, A.; Udaondo, P.; Cunha-Vaz, J.; Sivaprasad, S.; Bandello, F.; Lanzetta, P.; Kodjikian, L.; Goldstein, M.; Habot-Wilner, Z.; Loewenstein, A.; et al. A Collaborative Retrospective Study on the Efficacy and Safety of Intravitreal Dexamethasone Implant (Ozurdex) in Patients with Diabetic Macular Edema: The European DME Registry Study. Ophthalmology 2020, 127, 377–393. [Google Scholar] [CrossRef]
- Kodjikian, L.; Bellocq, D.; Mathis, T. Pharmacological Management of Diabetic Macular Edema in Real-Life Observational Studies. BioMed Res. Int. 2018, 2018, 8289253. [Google Scholar] [CrossRef] [PubMed]
- Mehta, H.; Nguyen, V.; Barthelmes, D.; Pershing, S.; Chi, G.C.; Dopart, P.; Gillies, M.C. Outcomes of Over 40,000 Eyes Treated for Diabetic Macula Edema in Routine Clinical Practice: A Systematic Review and Meta-analysis. Adv. Ther. 2022, 39, 5376–5390. [Google Scholar] [CrossRef] [PubMed]
- Callanan, D.G.; Loewenstein, A.; Patel, S.S.; Massin, P.; Corcóstegui, B.; Li, X.-Y.; Jiao, J.; Hashad, Y.; Whitcup, S.M. A multicenter, 12-month randomized study comparing dexamethasone intravitreal implant with ranibizumab in patients with diabetic macular edema. Graefes Arch. Clin. Exp. Ophthalmol. 2017, 255, 463–473. [Google Scholar] [CrossRef]
- Cornish, E.E.; Teo, K.Y.; Gillies, M.C.; Lim, L.L.; Nguyen, V.; Wickremasinghe, S.; Mehta, H.; McAllister, I.L.; Fraser-Bell, S. Five-year outcomes of eyes initially enrolled in the 2-year BEVORDEX trial of bevacizumab or dexamethasone implants for diabetic macular oedema. Br. J. Ophthalmol. 2022, 107, 79–83. [Google Scholar] [CrossRef] [PubMed]
- Al-Khersan, H.; Hariprasad, S.M.; Chhablani, J. Dex Implant Study Group. Early Response to Intravitreal Dexamethasone Implant Therapy in Diabetic Macular Edema May Predict Visual Outcome. Am. J. Ophthalmol. 2017, 184, 121–128. [Google Scholar] [CrossRef]
- Bucolo, C.; Gozzo, L.; Longo, L.; Mansueto, S.; Vitale, D.C.; Drago, F. Long-term efficacy and safety profile of multiple injections of intravitreal dexamethasone implant to manage diabetic macular edema: A systematic review of real-world studies. J. Pharmacol. Sci. 2018, 138, 219–232. [Google Scholar] [CrossRef] [PubMed]
- Castro-Navarro, V.; Cervera-Taulet, E.; Navarro-Palop, C.; Monferrer-Adsuara, C.; Hernández-Bel, L.; Montero-Hernández, J. Intravitreal dexamethasone implant Ozurdex® in naïve and refractory patients with different subtypes of diabetic macular edema. BMC Ophthalmol. 2019, 19, 15. [Google Scholar] [CrossRef]
- Zarranz-Ventura, J.; Romero-Núñez, B.; Bernal-Morales, C.; Velazquez-Villoria, D.; Sala-Puigdollers, A.; Figueras-Roca, M.; Copete, S.; Distefano, L.; Boixadera, A.; García-Arumi, J.; et al. Differential response to intravitreal dexamethasone implant in naïve and previously treated diabetic macular edema eyes. BMC Ophthalmol. 2020, 20, 443. [Google Scholar] [CrossRef]
- Sarao, V.; Veritti, D.; Furino, C.; Giancipoli, E.; Alessio, G.; Boscia, F.; Lanzetta, P. Dexamethasone implant with fixed or individualized regimen in the treatment of diabetic macular oedema: Six-month outcomes of the UDBASA study. Acta Ophthalmol. 2017, 95, e255–e260. [Google Scholar] [CrossRef]
- Malclès, A.; Dot, C.; Voirin, N.; Vié, A.-L.; Agard, E.; Bellocq, D.; Denis, P.; Kodjikian, L. Safety of intravitreal dexamethasone implant (ozurdex): The SAFODEX study. Incidence and Risk Factors of Ocular Hypertension. Retina 2017, 37, 1352–1359. [Google Scholar] [CrossRef]
- Maturi, R.K.; Glassman, A.R.; Liu, D.; Beck, R.W.; Bhavsar, A.R.; Bressler, N.M.; Jampol, L.M.; Melia, M.; Punjabi, O.S.; Salehi-Had, H.; et al. Effect of Adding Dexamethasone to Continued Ranibizumab Treatment in Patients With Persistent Diabetic Macular Edema: A DRCR Network Phase 2 Randomized Clinical Trial. JAMA Ophthalmol. 2018, 136, 29–38. [Google Scholar] [CrossRef]
- Martínez, A.H.; Delgado, E.P.; Silva, G.S.; Mateos, L.C.; Pascual, J.L.; Villa, J.L.; Vicente, P.G.; Almeida-González, C.-V. Early versus late switch: How long should we extend the anti-vascular endothelial growth factor therapy in unresponsive diabetic macular edema patients? Eur. J. Ophthalmol. 2020, 30, 1091–1098. [Google Scholar] [CrossRef]
- Rajesh, B.; Zarranz-Ventura, J.; Fung, A.T.; Busch, C.; Sahoo, N.K.; Rodriguez-Valdes, P.J.; Sarao, V.; Mishra, S.K.; Saatci, A.O.; Mirete, P.U.; et al. Safety of 6000 intravitreal dexamethasone implants. Br. J. Ophthalmol. 2020, 104, 39–46. [Google Scholar] [CrossRef]
- Pérez-Sarriegui, A.; Casas-Llera, P.; Díez-Álvarez, L.; Contreras, I.; Moreno-López, M.; Figueroa, M.; González-Martín-Moro, J.; Muñoz-Negrete, F.; Rebolleda, G. Phaco-non-penetrating deep sclerectomy in ocular hypertension secondary to dexamethasone intravitreal implant. Arch. Soc. Esp. Oftalmol. 2018, 93, 580–585. [Google Scholar] [CrossRef] [PubMed]
- Kaya, M.; Atas, F.; Kocak, N.; Ozturk, T.; Ayhan, Z.; Kaynak, S. Intravitreal Ranibizumab and Dexamethasone Implant Injections as Primary Treatment of Diabetic Macular Edema: The Month 24 Results from Simultaneously Double Protocol. Curr. Eye Res. 2023, 48, 498–505. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Ren, X.-J.; Hu, B.-J.; Lam, W.-C.; Li, X.-R. A meta-analysis of the effect of a dexamethasone intravitreal implant versus intravitreal anti-vascular endothelial growth factor treatment for diabetic macular edema. BMC Ophthalmol. 2018, 18, 121. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.U.; Harless, A.; Bleau, L.; Maturi, R.K. Prospective randomized subject-masked study of intravitreal bevacizumab monotherapy versus dexamethasone implant monotherapy in the treatment of persistent diabetic macular edema. Retina 2016, 36, 1986–1996. [Google Scholar] [CrossRef]
- Comet, A.; Gascon, P.; Ramtohul, P.; Donnadieu, B.; Denis, D.; Matonti, F. INVICTUS: Intravitreal anti-VEGF and dexamethasone implant comparison for the treatment of diabetic macular edema: A 12 months follow-up study. Eur. J. Ophthalmol. 2021, 31, 754–758, Erratum in Eur. J. Ophthalmol. 2020, 31, NP158. [Google Scholar] [CrossRef]
- Patil, N.S.; Mihalache, A.; Hatamnejad, A.; Popovic, M.M.; Kertes, P.J.; Muni, R.H. Intravitreal Steroids Compared with Anti-VEGF Treatment for Diabetic Macular Edema: A Meta-Analysis. Ophthalmol. Retin. 2023, 7, 289–299. [Google Scholar] [CrossRef]
- Chi, S.-C.; Kang, Y.-N.; Huang, Y.-M. Efficacy and safety profile of intravitreal dexamethasone implant versus antivascular endothelial growth factor treatment in diabetic macular edema: A systematic review and meta-analysis. Sci. Rep. 2023, 13, 7428. [Google Scholar] [CrossRef]
- Pacella, F.; Romano, M.R.; Turchetti, P.; Tarquini, G.; Carnovale, A.; Mollicone, A.; Mastromatteo, A.; Pacella, E. An eighteen-month follow-up study on the effects of Intravitreal Dexamethasone Implant in diabetic macular edema refractory to anti-VEGF therapy. Int. J. Ophthalmol. 2016, 9, 1427–1432. [Google Scholar] [CrossRef]
- Veritti, D.; Sarao, V.; Soppelsa, V.; Lanzetta, P. Managing Diabetic Macular Edema in Clinical Practice: Systematic Review and Meta-Analysis of Current Strategies and Treatment Options. Clin. Ophthalmol. 2021, 15, 375–385. [Google Scholar] [CrossRef] [PubMed]
- Holekamp, N.M.; Campbell, J.; Almony, A.; Ingraham, H.; Marks, S.; Chandwani, H.; Cole, A.L.; Kiss, S. Vision Outcomes Following Anti–Vascular Endothelial Growth Factor Treatment of Diabetic Macular Edema in Clinical Practice. Am. J. Ophthalmol. 2018, 191, 83–91, Erratum in Am. J. Ophthalmol. 2018, 194, 192. [Google Scholar] [CrossRef]
- Ciulla, T.A.; Pollack, J.S.; Williams, D.F. Visual acuity outcomes and anti-VEGF therapy intensity in diabetic macular oedema: A real-world analysis of 28 658 patient eyes. Br. J. Ophthalmol. 2021, 105, 216–221. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, P.; Bandello, F.; Schmidt-Erfurth, U.; Lang, G.E.; Massin, P.; Schlingemann, R.O.; Sutter, F.; Simader, C.; Burian, G.; Gerstner, O.; et al. The RESTORE study: Ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology 2011, 118, 615–625. [Google Scholar] [CrossRef] [PubMed]
- Gascon, P.; Borget, I.; Comet, A.; Carton, L.; Matonti, F.; Dupont-Benjamin, L. Costs comparison of treating diabetic macular edema with aflibercept, ranibizumab or dexamethasone at 1 year in France (INVICOST study). Eur. J. Ophthalmol. 2021, 32, 1702–1709. [Google Scholar] [CrossRef]
- Busch, C.; Zur, D.; Fraser-Bell, S.; Laíns, I.; Santos, A.R.; Lupidi, M.; Cagini, C.; Gabrielle, P.-H.; Couturier, A.; Mané-Tauty, V.; et al. Shall we stay, or shall we switch? Continued anti-VEGF therapy versus early switch to dexamethasone implant in refractory diabetic macular edema. Acta Diabetol. 2018, 55, 789–796. [Google Scholar] [CrossRef]
- Ruiz-Moreno, J.M.; Ruiz-Medrano, J. Early-switch versus late-switch in patients with diabetic macular edema: A cost-effectiveness study. Graefes Arch. Clin. Exp. Ophthalmol. 2023, 261, 941–949. [Google Scholar] [CrossRef]
- Peto, T. An overview of the clinical outcomes of the fluocinolone acetonide 190 µg intravitreal implant clinical evidence study in the United Kingdom (ICE-UK). Curr. Med. Res. Opin. 2017, 33 (Suppl. S2), 3–4. [Google Scholar] [CrossRef][Green Version]
- Eaton, A.; Koh, S.S.; Jimenez, J.; Riemann, C.D. The USER Study: A Chart Review of Patients Receiving a 0.2 µg/day Fluocinolone Acetonide Implant for Diabetic Macular Edema. Ophthalmol. Ther. 2019, 8, 51–62. [Google Scholar] [CrossRef]
- Augustin, A.J.; Bopp, S.; Fechner, M.; Holz, F.; Sandner, D.; Winkgen, A.-M.; Khoramnia, R.; Neuhann, T.; Warscher, M.; Spitzer, M.; et al. Three-year results from the Retro-IDEAL study: Real-world data from diabetic macular edema (DME) patients treated with ILUVIEN® (0.19 mg fluocinolone acetonide implant). Eur. J. Ophthalmol. 2020, 30, 382–391. [Google Scholar] [CrossRef]
- Rehak, M.; Busch, C.; Unterlauft, J.-D.; Jochmann, C.; Wiedemann, P. Outcomes in diabetic macular edema switched directly or after a dexamethasone implant to a fluocinolone acetonide intravitreal implant following anti-VEGF treatment. Acta Diabetol. 2020, 57, 469–478. [Google Scholar] [CrossRef]
- Cicinelli, M.V.; Rosenblatt, A.; Grosso, D.; Zollet, P.; Capone, L.; Rabiolo, A.; Lattanzio, R.; Loewenstein, A.; Bandello, F.; Nassisi, M.; et al. The outcome of fluocinolone acetonide intravitreal implant is predicted by the response to dexamethasone implant in diabetic macular oedema. Eye 2021, 35, 3232–3242, Erratum in Eye 2021, 35, 3459. [Google Scholar] [CrossRef] [PubMed]
- Bailey, C.; Chakravarthy, U.; Lotery, A.; Menon, G.; Talks, J. Medisoft Audit Group Extended real-world experience with the ILUVIEN® (fluocinolone acetonide) implant in the United Kingdom: 3-year results from the Medisoft® audit study. Eye 2022, 36, 1012–1018. [Google Scholar] [CrossRef] [PubMed]
- Baillif, S.; Staccini, P.; Weber, M.; Delyfer, M.-N.; Le Mer, Y.; Gualino, V.; Collot, L.; Merite, P.-Y.; Creuzot-Garcher, C.; Kodjikian, L.; et al. Management of Patients with Diabetic Macular Edema Switched from Dexamethasone Intravitreal Implant to Fluocinolone Acetonide Intravitreal Implant. Pharmaceutics 2022, 14, 2391. [Google Scholar] [CrossRef] [PubMed]
- Mathis, T.; Papegaey, M.; Ricard, C.; Rezkallah, A.; Matonti, F.; Sudhalkar, A.; Vartin, C.; Dot, C.; Kodjikian, L. Efficacy and Safety of Intravitreal Fluocinolone Acetonide Implant for Chronic Diabetic Macular Edema Previously Treated in Real-Life Practice: The REALFAc Study. Pharmaceutics 2022, 14, 723. [Google Scholar] [CrossRef] [PubMed]
- Singer, M.A.; Sheth, V.; Mansour, S.E.; Coughlin, B.; Gonzalez, V.H. Three-Year Safety and Efficacy of the 0.19-mg Fluocinolone Acetonide Intravitreal Implant for Diabetic Macular Edema: The PALADIN Study. Ophthalmology 2022, 129, 605–613. [Google Scholar] [CrossRef] [PubMed]
- Fallico, M.; Maugeri, A.; Lotery, A.; Longo, A.; Bonfiglio, V.; Russo, A.; Avitabile, T.; Furino, C.; Cennamo, G.; Barchitta, M.; et al. Fluocinolone acetonide vitreous insert for chronic diabetic macular oedema: A systematic review with meta-analysis of real-world experience. Sci. Rep. 2021, 11, 4800. [Google Scholar] [CrossRef] [PubMed]
- Kodjikian, L.; Baillif, S.; Creuzot-Garcher, C.; Delyfer, M.-N.; Matonti, F.; Weber, M.; Mathis, T. Real-World Efficacy and Safety of Fluocinolone Acetonide Implant for Diabetic Macular Edema: A Systematic Review. Pharmaceutics 2021, 13, 72. [Google Scholar] [CrossRef]
- Khoramnia, R.; Peto, T.; Koch, F.; Taylor, S.R.; de Sousa, J.P.C.; Hill, L.; Bailey, C.; Chakravarthy, U.; ILUVIEN Registry Safety Study (IRISS) Investigators Group. Safety and effectiveness of the fluocinolone acetonide intravitreal implant (ILUVIEN): 3-year results from the European IRISS registry study. Br. J. Ophthalmol. 2023, 107, 1502–1508. [Google Scholar] [CrossRef] [PubMed]
- Schmit-Eilenberger, V. A novel intravitreal fluocinolone acetonide implant (Iluvien®) in the treatment of patients with chronic diabetic macular edema that is insufficiently responsive to other medical treatment options: A case series. Clin. Ophthalmol. 2015, 9, 801–811. [Google Scholar] [CrossRef]
- McCluskey, J.D.; Kaufman, P.L.; Wynne, K.; Lewis, G. Early adoption of the fluocinolone acetonide (FAc) intravitreal implant in patients with persistent or recurrent diabetic macular edema (DME). Int. Med. Case Rep. J. 2019, 12, 93–102. [Google Scholar] [CrossRef]
- Ch’ng, S.W.; Brent, A.J.; Empeslidis, T.; Konidaris, V.; Banerjee, S. Real-World Cost Savings Demonstrated by Switching Patients with Refractory Diabetic Macular Edema to Intravitreal Fluocinolone Acetonide (Iluvien): A Retrospective Cost Analysis Study. Ophthalmol. Ther. 2018, 7, 75–82. [Google Scholar] [CrossRef]
- Parrish, R.K., 2nd; Campochiaro, P.A.; Pearson, P.A.; Green, K.; Traverso, C.E. FAME Study Group Characterization of Intraocular Pressure Increases and Management Strategies Following Treatment With Fluocinolone Acetonide Intravitreal Implants in the FAME Trials. Ophthalmic Surg. Lasers Imaging Retin. 2016, 47, 426–435. [Google Scholar] [CrossRef]
- Roth, D.B.; Eichenbaum, D.; Malik, D.; Radcliffe, N.M.; Cutino, A.; Small, K.W.; PALADIN Study Group. The 0.19-mg Fluocinolone Acetonide Intravitreal Implant for Diabetic Macular Edema: Intraocular Pressure-Related Effects over 36 Months. Ophthalmol. Retin. 2023, 8, 49–54. [Google Scholar] [CrossRef]
- El Rayes, E.N.; Leila, M. Visual function and retinal morphological changes after single suprachoroidal delivery of fluocinolone acetonide (Iluvien®) implant in eyes with chronic diabetic macular edema. Int. J. Retin. Vitr. 2023, 9, 20. [Google Scholar] [CrossRef]
- Bressler, S.B.; Odia, I.; Maguire, M.G.; Dhoot, D.S.; Glassman, A.R.; Jampol, L.M.; Marcus, D.M.; Solomon, S.D.; Sun, J.K.; Diabetic Retinopathy Clinical Research Network. Factors Associated With Visual Acuity and Central Subfield Thickness Changes When Treating Diabetic Macular Edema With Anti–Vascular Endothelial Growth Factor Therapy: An Exploratory Analysis of the Protocol T Randomized Clinical Trial. JAMA Ophthalmol. 2022, 137, 382–389, Erratum in JAMA Ophthalmol. 2022, 140, 1030. [Google Scholar] [CrossRef]
- Kwon, J.-W.; Jee, D. Aqueous humor cytokine levels in patients with diabetic macular edema refractory to anti-VEGF treatment. PLoS ONE 2018, 13, e0203408, Erratum in PLoS ONE 2018, 13, e0207902. [Google Scholar] [CrossRef]
- Ehlken, C.; Helms, M.; Böhringer, D.; Agostini, H.T.; Stahl, A. Association of treatment adherence with real-life VA outcomes in AMD, DME, and BRVO patients. Clin. Ophthalmol. 2017, 12, 13–20. [Google Scholar] [CrossRef]
- Uludag, G.; Hassan, M.; Matsumiya, W.; Pham, B.H.; Chea, S.; Trong Tuong Than, N.; Doan, H.L.; Akhavanrezayat, A.; Halim, M.S.; Do, D.V.; et al. Efficacy and safety of intravitreal anti-VEGF therapy in diabetic retinopathy: What we have learned and what should we learn further? Expert Opin. Biol. Ther. 2022, 22, 1275–1291. [Google Scholar] [CrossRef]
- Polizzi, S.; Mahajan, V.B. Intravitreal Anti-VEGF Injections in Pregnancy: Case Series and Review of Literature. J. Ocul. Pharmacol. Ther. 2015, 31, 605–610. [Google Scholar] [CrossRef]
- Fazelat, A.; Lashkari, K. Off-label use of intravitreal triamcinolone acetonide for diabetic macular edema in a pregnant patient. Clin. Ophthalmol. 2011, 5, 439–441. [Google Scholar] [CrossRef][Green Version]
- Concillado, M.; Lund-Andersen, H.; Mathiesen, E.R.; Larsen, M. Dexamethasone Intravitreal Implant for Diabetic Macular Edema During Pregnancy. Am. J. Ophthalmol. 2016, 165, 7–15. [Google Scholar] [CrossRef] [PubMed]
- Sophie, R.; Lu, N.; Campochiaro, P.A. Predictors of Functional and Anatomic Outcomes in Patients with Diabetic Macular Edema Treated with Ranibizumab. Ophthalmology 2015, 122, 1395–1401. [Google Scholar] [CrossRef] [PubMed]
- Terada, N.; Murakami, T.; Uji, A.; Dodo, Y.; Mori, Y.; Tsujikawa, A. Hyperreflective Walls in Foveal Cystoid Spaces as a Biomarker of Diabetic Macular Edema Refractory to Anti-VEGF Treatment. Sci. Rep. 2020, 10, 7299. [Google Scholar] [CrossRef] [PubMed]
- Vujosevic, S.; Simó, R. Local and Systemic Inflammatory Biomarkers of Diabetic Retinopathy: An Integrative Approach. Investig. Ophthalmol. Vis. Sci. 2017, 58, BIO68–BIO75. [Google Scholar] [CrossRef] [PubMed]
- Jeng, C.-J.; Hsieh, Y.-T.; Yang, C.-M.; Yang, C.-H.; Lin, C.-L.; Wang, I.-J. Development of diabetic retinopathy after cataract surgery. PLoS ONE 2018, 13, e0202347. [Google Scholar] [CrossRef]
- Khodabandeh, A.; Fadaifard, S.; Abdollahi, A.; Karkhaneh, R.; Roohipoor, R.; Abdi, F.; Ghasemi, H.; Habibollahi, S.; Mazloumi, M. Role of combined phacoemulsification and intravitreal injection of bevacizumab in prevention of postoperative macular edema in non-proliferative diabetic retinopathy. J. Curr. Ophthalmol. 2018, 30, 245–249. [Google Scholar] [CrossRef]
- Tatsumi, T.; Oshitari, T.; Ando, T.; Takatsuna, Y.; Arai, M.; Baba, T.; Sato, E.; Yamamoto, S. Comparison of the Efficacy of Sub-Tenon versus Intravitreal Triamcinolone Acetonide Injection during Cataract Surgery for Diabetic Macular Edema. Ophthalmologica 2018, 241, 17–23. [Google Scholar] [CrossRef]
- Fallico, M.; Avitabile, T.; Castellino, N.; Longo, A.; Russo, A.; Bonfiglio, V.; Parisi, F.; Furino, C.; Panozzo, G.; Scorcia, V.; et al. Intravitreal dexamethasone implant one month before versus concomitant with cataract surgery in patients with diabetic macular oedema: The dexcat study. Acta Ophthalmol. 2021, 99, E74–E80. [Google Scholar] [CrossRef]
- Furino, C.; Boscia, F.; Niro, A.; D’Addario, M.; Grassi, M.O.; Saglimbene, V.; Reibaldi, M.; Alessio, G. Diabetic macular edema and cataract surgery: Phacoemulsification Combined With Dexamethasone Intravitreal Implant Compared With Standard Phacoemulsification. Retina 2021, 41, 1102–1109. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.S.; Ghosn, C.; Yu, Z.; Zacharias, L.C.; Kao, H.; Lanni, C.; Abdelfattah, N.; Kuppermann, B.; Csaky, K.G.; D’Argenio, D.Z.; et al. Vitreous VEGF Clearance is increased after vitrectomy. Investig. Ophthalmol. Vis. Sci. 2010, 51, 2135–2138. [Google Scholar] [CrossRef]
- Costa, J.F.; Sousa, K.; Marques, J.P.; Marques, M.; Cachulo, M.L.; Silva, R.; Gomes, N.; Figueira, J. Efficacy and safety of postvitrectomy intravitreal triamcinolone therapy for diabetic macular edema. Eur. J. Ophthalmol. 2016, 26, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, A.; Tsuzuki, A.; Arai, K.; Gekka, T.; Kohzaki, K.; Tsuneoka, H. Efficacy of Intravitreal Triamcinolone Acetonide for Diabetic Macular Edema After Vitrectomy. J. Ocul. Pharmacol. Ther. 2016, 32, 38–43. [Google Scholar] [CrossRef]
- Rezkallah, A.; Malclès, A.; Dot, C.; Voirin, N.; Agard, É.; Vié, A.-L.; Denis, P.; Mathis, T.; Kodjikian, L. Evaluation of efficacy and safety of dexamethasone intravitreal implants before and after vitrectomy in a real-life study. Acta Ophthalmol. 2017, 96, e544–e546. [Google Scholar] [CrossRef] [PubMed]
- Pessoa, B.; Coelho, J.; Correia, N.; Ferreira, N.; Beirão, M.; Meireles, A. Fluocinolone Acetonide Intravitreal Implant 190 μg (ILUVIEN®) in Vitrectomized versus Nonvitrectomized Eyes for the Treatment of Chronic Diabetic Macular Edema. Ophthalmic Res. 2017, 59, 68–75. [Google Scholar] [CrossRef]
- Breusegem, C.; Vandewalle, E.; Van Calster, J.; Stalmans, I.; Zeyen, T. Predictive value of a topical dexamethasone provocative test before intravitreal triamcinolone acetonide injection. Investig. Ophthalmol. Vis. Sci. 2009, 50, 573–576. [Google Scholar] [CrossRef] [PubMed]
- Tsoutsanis, P.; Kapantais, D. Anterior migration of Ozurdex implant: A review on risk factors, complications, and management. Int. J. Retin. Vitr. 2023, 9, 74. [Google Scholar] [CrossRef] [PubMed]
- Rishi, P.; Majumder, P.D.; Biswas, J. Anterior Chamber Migration of Fluocinolone Acetonide Intravitreal Implant. JAMA Ophthalmol. 2019, 137, e185931. [Google Scholar] [CrossRef] [PubMed]
- Wykoff, C.C.; Chakravarthy, U.; Campochiaro, P.A.; Bailey, C.; Green, K.; Cunha-Vaz, J. Long-term Effects of Intravitreal 0.19 mg Fluocinolone Acetonide Implant on Progression and Regression of Diabetic Retinopathy. Ophthalmology 2017, 124, 440–449. [Google Scholar] [CrossRef] [PubMed]
- Iglicki, M.; Zur, D.; Busch, C.; Okada, M.; Loewenstein, A. Progression of diabetic retinopathy severity after treatment with dexamethasone implant: A 24-month cohort study the ‘DR-Pro-DEX Study’. Acta Diabetol. 2018, 55, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Rittiphairoj, T.; Mir, T.A.; Li, T.; Virgili, G. Intravitreal steroids for macular edema in diabetes. Cochrane Database Syst. Rev. 2020, 11, CD005656. [Google Scholar] [CrossRef] [PubMed]
- Zarranz-Ventura, J.; Mali, J.O. Effectiveness of 190 μg Fluocinolone Acetonide and 700 μg Dexamethasone Intravitreal Implants in Diabetic Macular Edema Using the Area-Under-the-Curve Method: The CONSTANT Analysis. Clin. Ophthalmol. 2020, 14, 1697–1704. [Google Scholar] [CrossRef] [PubMed]
- Kuley, B.; Storey, P.P.; Pancholy, M.; Wibbelsman, T.D.; Obeid, A.; Regillo, C.; Garg, S. Treatment of Eyes With Diabetic Macular Edema That Had a Suboptimal Response to Antivascular Endothelial Growth Factor Therapy: 2-mg Intravitreal Triamcinolone Acetonide vs. 0.7-mg Dexamethasone Implant. J. Vitr. Dis. 2020, 4, 372–376. [Google Scholar] [CrossRef]
- Augustin, A.J.; Kuppermann, B.D.; Lanzetta, P.; Loewenstein, A.; Li, X.-Y.; Cui, H.; Hashad, Y.; Whitcup, S.M.; Ozurdex MEAD Study Group. Dexamethasone intravitreal implant in previously treated patients with diabetic macular edema: Subgroup analysis of the MEAD study. BMC Ophthalmol. 2015, 15, 150. [Google Scholar] [CrossRef]
- Thakur, A.; Kadam, R.; Kompella, U.B. Trabecular Meshwork and Lens Partitioning of Corticosteroids: Implications for elevated intraocular pressure and cataracts. Arch. Ophthalmol. 2011, 129, 914–920. [Google Scholar] [CrossRef]
- Amoaku, W.M.K.; Saker, S.; Stewart, E.A. A review of therapies for diabetic macular oedema and rationale for combination therapy. Eye 2015, 29, 1115–1130. [Google Scholar] [CrossRef] [PubMed]
- Ehlers, J.P.; Yeh, S.; Maguire, M.G.; Smith, J.R.; Mruthyunjaya, P.; Jain, N.; Kim, L.A.; Weng, C.Y.; Flaxel, C.J.; Schoenberger, S.D.; et al. Intravitreal Pharmacotherapies for Diabetic Macular Edema: A Report by the American Academy of Ophthalmology. Ophthalmology 2021, 129, 88–99. [Google Scholar] [CrossRef] [PubMed]
- Mehta, H.; Hennings, C.; Gillies, M.C.; Nguyen, V.; Campain, A.; Fraser-Bell, S. Anti-vascular endothelial growth factor combined with intravitreal steroids for diabetic macular oedema. Cochrane Database Syst. Rev. 2018, 4, CD011599. [Google Scholar] [CrossRef] [PubMed]
- Weinberg, T.; Loewenstein, A. The role of steroids in treating diabetic macular oedema in the era of anti-VEGF. Eye 2020, 34, 1003–1005. [Google Scholar] [CrossRef]
- Mansour, S.E.; Browning, D.J.; Wong, K.; Flynn, H.W., Jr.; Bhavsar, A.R. The Evolving Treatment of Diabetic Retinopathy. Clin. Ophthalmol. 2020, 14, 653–678. [Google Scholar] [CrossRef]
| vascular endothelial growth factor (VEGF)-A |
| angiopoietin-2 (Ang-2) |
| tumor necrosis factor (TNF)-α |
| placental growth factor (PGF) |
| hepatocyte growth factor (HGF) |
| insulin-like growth factor (IGF) |
| platelet activation factor (PAF) |
| interleukines (IL) IL-1, IL-6, IL-8 |
| reactive oxygen species (ROS) |
| nitric oxide (NO) |
| protein kinase C (PKC) |
| advanced glycation products (AGEs) |
| monocyte chemoattractant protein-1 (MCP-1) |
| nitric oxide synthase (iNOS) |
| matrix metalloproteinases (MMPs) |
| intercellular adhesion molecule-1 (ICAM-1) |
| kallikrein-kinins (KKs) |
| chemokines |
| prostaglandins |
| leukotrienes |
| histamine |
| complement factors |
| activated retinal microglia |
| activated macrophages, lymphocytes, and neutrophyles |
| Down-regulation of VEGF-A by reducing the expression of the VEGF-A genes and by regulating the expression of the VEGF-A receptors |
| Down-regulation of several other pro-inflammatory mediators, including interleukin-6, intercellular adhesion molecule-1 (ICAM-1), P-selectine, nitric oxide (NO), prostaglandins, and leukotrienes |
| Inhibition of leukostasis, with significant reduction of the neutrophil, lymphocyte, and macrophage migration through the blood vessel walls to the inflammation tissue sites |
| Restoration of the structural integrity of the tight junctions of the blood-retinal barriers |
| Inhibition of the collagenase with reduction of the vascular permeability |
| Downregulation of the expression of the aquaporin-4 in the Mueller cells’ membrane, thus reducing the intracellular edema |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salvetat, M.L.; Pellegrini, F.; Spadea, L.; Salati, C.; Musa, M.; Gagliano, C.; Zeppieri, M. The Treatment of Diabetic Retinal Edema with Intravitreal Steroids: How and When. J. Clin. Med. 2024, 13, 1327. https://doi.org/10.3390/jcm13051327
Salvetat ML, Pellegrini F, Spadea L, Salati C, Musa M, Gagliano C, Zeppieri M. The Treatment of Diabetic Retinal Edema with Intravitreal Steroids: How and When. Journal of Clinical Medicine. 2024; 13(5):1327. https://doi.org/10.3390/jcm13051327
Chicago/Turabian StyleSalvetat, Maria Letizia, Francesco Pellegrini, Leopoldo Spadea, Carlo Salati, Mutali Musa, Caterina Gagliano, and Marco Zeppieri. 2024. "The Treatment of Diabetic Retinal Edema with Intravitreal Steroids: How and When" Journal of Clinical Medicine 13, no. 5: 1327. https://doi.org/10.3390/jcm13051327
APA StyleSalvetat, M. L., Pellegrini, F., Spadea, L., Salati, C., Musa, M., Gagliano, C., & Zeppieri, M. (2024). The Treatment of Diabetic Retinal Edema with Intravitreal Steroids: How and When. Journal of Clinical Medicine, 13(5), 1327. https://doi.org/10.3390/jcm13051327










