A Novel Scoring System Predicting Red Blood Cell Transfusion Requirements in Patients Undergoing Invasive Spine Surgery
Abstract
1. Introduction
2. Materials and Methods
2.1. Source of Data
2.2. Outcome
2.3. Predictors
2.4. Score Development
- (i)
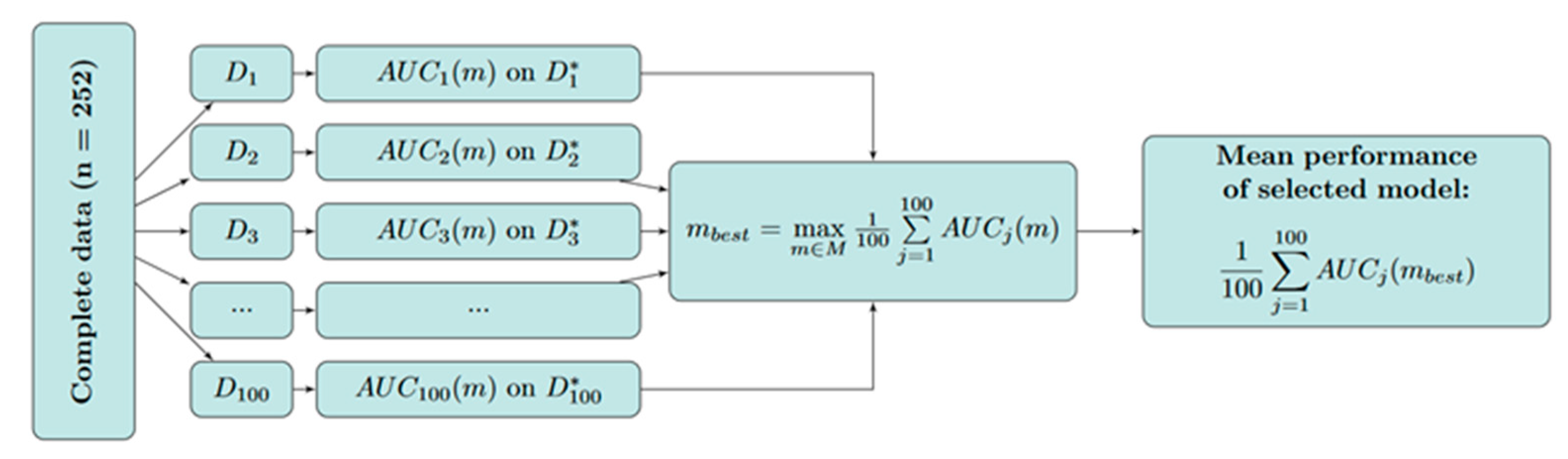
- The random division of the complete cohort (n = 252) into 100 training cohorts from to (each containing 80% of all observations, stratified by event/non-event) and 100 test cohorts from to (each containing the remaining 20% of observations) using random sampling.
- (ii)
- Each possible model was fitted to each training cohort and the AUC was calculated for each test cohort , denoted by .
- (iii)
- The best-performing model was derived by maximizing the mean AUC across all test cohorts.
2.5. Handling of Missing Data
3. Results
3.1. Participants
3.2. Prediction Model
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bundesärztekammer (Ed.) Querschnitts-Leitlinien zur Therapie mit Blutkomponenten und Plasmaderivaten: Gesamtnovelle 2020; Deutscher Ärzteverlag: Köln, Germany, 2021; 337p. [Google Scholar]
- Sixty-Third World Health Assembly, World Health Organization. WHO Guiding Principles on Human Cell, Tissue and Organ Transplantation. Cell Tissue Bank 2010, 11, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Judd, L.; Hof, L.; Beladdale, L.; Friederich, P.; Thoma, J.; Wittmann, M.; Zacharowski, K.; Meybohm, P.; Choorapoikayil, S. Prevalence of pre-operative anaemia in surgical patients: A retrospective, observational, multicentre study in Germany. Anaesthesia 2022, 77, 1209–1218. [Google Scholar] [CrossRef] [PubMed]
- Meybohm, P.; Schmitt, E.; Choorapoikayil, S.; Hof, L.; Old, O.; Baumhove, O.; Weenen, S.d.L.v.; Bayer, A.; Friederich, P.; Bräutigam, B.; et al. German Patient Blood Management Network: Effectiveness and safety analysis in 1.2 million patients. Br. J. Anaesth. 2023, 131, 472–481. [Google Scholar] [CrossRef] [PubMed]
- Delis, A.; Bautz, D.; Ehrentraut, H.; Doll, K.; Randau, T.M.; Strauss, A.C.; Habicht, I.; Güresir, E.; Bogatsch, H.; Kranke, P.; et al. Effects of Different Hemoglobin Levels on Near-Infrared Spectroscopy-Derived Cerebral Oxygen Saturation in Elderly Patients Undergoing Noncardiac Surgery. Transfus. Med. Hemotherapy 2023, 50, 270–276. [Google Scholar] [CrossRef] [PubMed]
- Meybohm, P.; Lindau, S.; Treskatsch, S.; Francis, R.; Spies, C.; Velten, M.; Wittmann, M.; Gueresir, E.; Stoppe, C.; Kowark, A.; et al. Liberal transfusion strategy to prevent mortality and anaemia-associated, ischaemic events in elderly non-cardiac surgical patients—The study design of the LIBERAL-Trial. Trials 2019, 20, 101. [Google Scholar] [CrossRef] [PubMed]
- Fiedler, S.A.; Henseler, O.; Hoffelner, M.; Doll, M.; Hutschenreuter, G.; Hoch, J.; Weinauer, F.; Humpe, A.; Funk, M.B.; Hilger, A. Monitoring Blood Supply in Germany: A Regulatory Perspective. Transfus. Med. Hemotherapy 2023, 50, 129–134. [Google Scholar] [CrossRef] [PubMed]
- Peduzzi, P.; Concato, J.; Kemper, E.; Holford, T.R.; Feinstein, A.R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 1996, 49, 1373–1379. [Google Scholar] [CrossRef] [PubMed]
- Bischl, B.; Mersmann, O.; Trautmann, H.; Weihs, C. Resampling methods for meta-model validation with recommendations for evolutionary computation. Evol. Comput. 2012, 20, 249–275. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, L.M.; Massaro, J.M.; D’Agostino, R.B. Presentation of multivariate data for clinical use: The Framingham Study risk score functions. Stat. Med. 2004, 23, 1631–1660. [Google Scholar] [CrossRef] [PubMed]
- Hayn, D.; Kreiner, K.; Ebner, H.; Kastner, P.; Breznik, N.; Rzepka, A.; Hofmann, A.; Gombotz, H.; Schreier, G. Development of Multivariable Models to Predict and Benchmark Transfusion in Elective Surgery Supporting Patient Blood Management. Appl. Clin. Inform. 2017, 8, 617–631. [Google Scholar] [CrossRef] [PubMed]
- Walczak, S.; Velanovich, V. Prediction of perioperative transfusions using an artificial neural network. PLoS ONE 2020, 15, e0229450. [Google Scholar] [CrossRef] [PubMed]
- Larocque, B.J.; Gilbert, K.; Brien, W.F. Prospective validation of a point score system for predicting blood transfusion following hip or knee replacement. Transfusion 1998, 38, 932–937. [Google Scholar] [CrossRef] [PubMed]
- Pulitanò, C.; Arru, M.; Bellio, L.; Rossini, S.; Ferla, G.; Aldrighetti, L. A risk score for predicting perioperative blood transfusion in liver surgery. Br. J. Surg. 2007, 94, 860–865. [Google Scholar] [CrossRef] [PubMed]
- Rashiq, S.; Shah, M.; Chow, A.K.; O’Connor, P.J.; Finegan, B.A. Predicting allogeneic blood transfusion use in total joint arthroplasty. Anesth. Analg. 2004, 99, 1239–1244. [Google Scholar] [CrossRef] [PubMed]
- Goudie, R.; Sterne, J.A.C.; Verheyden, V.; Bhabra, M.; Ranucci, M.; Murphy, G.J. Risk scores to facilitate preoperative prediction of transfusion and large volume blood transfusion associated with adult cardiac surgery. Br. J. Anaesth. 2015, 114, 757–766. [Google Scholar] [CrossRef] [PubMed]
- Klein, A.A.; Collier, T.; Yeates, J.; Miles, L.F.; Fletcher, S.N.; Evans, C.; Richards, T. The ACTA PORT-score for predicting perioperative risk of blood transfusion for adult cardiac surgery. Br. J. Anaesth. 2017, 119, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Shih, H.; Rajendran, S. Comparison of Time Series Methods and Machine Learning Algorithms for Forecasting Taiwan Blood Services Foundation’s Blood Supply. J. Healthc. Eng. 2019, 2019, 6123745. [Google Scholar] [CrossRef] [PubMed]


| Patient Characteristics | |||
|---|---|---|---|
| No RBC Package Received (N = 191) | One or More RBC Packages Received (N = 61) | Overall (N = 252) | |
| Sex | |||
| Male | 96 (50.3%) | 33 (54.1%) | 129 (51.2%) |
| Female | 95 (49.7%) | 28 (45.9%) | 123 (48.8%) |
| Age | |||
| Mean (SD) | 61.0 (17.0) | 67.3 (17.6) | 62.6 (17.3) |
| Median [Min, Max] | 65.0 [14.0, 89.0] | 69.0 [22.0, 89.0] | 66.5 [14.0, 89.0] |
| Height | |||
| Mean (SD) | 172 (9.76) | 172 (11.3) | 172 (10.1) |
| Median [Min, Max] | 170 [150, 198] | 172 [140, 196] | 172 [140, 198] |
| Missing | 5 (2.6%) | 2 (3.3%) | 7 (2.8%) |
| Weight | |||
| Mean (SD) | 80.3 (17.6) | 78.6 (20.6) | 79.9 (18.3) |
| Median [Min, Max] | 78.0 [43.0, 150] | 76.0 [38.0, 140] | 77.5 [38.0, 150] |
| Missing | 2 (1.0%) | 0 (0%) | 2 (0.8%) |
| ASA score | |||
| 1 | 19 (9.9%) | 4 (6.6%) | 23 (9.1%) |
| 2 | 111 (58.1%) | 20 (32.8%) | 131 (52.0%) |
| 3 | 44 (23.0%) | 28 (45.9%) | 72 (28.6%) |
| Missing | 17 (8.9%) | 9 (14.8%) | 26 (10.3%) |
| Premedication (anticoagulant) | |||
| No | 140 (73.3%) | 36 (59.0%) | 176 (69.8%) |
| Yes | 51 (26.7%) | 25 (41.0%) | 76 (30.2%) |
| Number of prior spine surgeries | |||
| No prior surgery | 171 (89.5%) | 43 (70.5%) | 214 (84.9%) |
| One prior surgery | 19 (9.9%) | 15 (24.6%) | 34 (13.5%) |
| Two prior surgeries | 1 (0.5%) | 3 (4.9%) | 4 (1.6%) |
| Pre-Operative Laboratory Measures | |||
|---|---|---|---|
| No RBC Package Received (N = 191) | One or More RBC Packages Received (N = 61) | Overall (N = 252) | |
| Hb (g/dL) | |||
| Mean (SD) | 13.3 (1.96) | 10.6 (2.14) | 12.7 (2.32) |
| Median [Min, Max] | 13.4 [7.70, 19.1] | 10.3 [7.00, 15.9] | 12.9 [7.00, 19.1] |
| Quick | |||
| Mean (SD) | 103 (14.7) | 96.1 (13.5) | 101 (14.7) |
| Median [Min, Max] | 105 [21.0, 130] | 97.0 [63.0, 126] | 103 [21.0, 130] |
| Missing | 1 (0.5%) | 0 (0%) | 1 (0.4%) |
| INR | |||
| Mean (SD) | 0.996 (0.161) | 1.02 (0.0809) | 1.00 (0.146) |
| Median [Min, Max] | 1.00 [0.800, 2.80] | 1.00 [0.900, 1.20] | 1.00 [0.800, 2.80] |
| Missing | 1 (0.5%) | 0 (0%) | 1 (0.4%) |
| PTT | |||
| Mean (SD) | 24.8 (3.69) | 26.1 (6.74) | 25.1 (4.62) |
| Median [Min, Max] | 24.0 [18.0, 53.0] | 25.0 [18.0, 65.0] | 24.0 [18.0, 65.0] |
| Missing | 1 (0.5%) | 2 (3.3%) | 3 (1.2%) |
| Thrombocytes | |||
| Mean (SD) | 278 (104) | 291 (105) | 281 (104) |
| Median [Min, Max] | 261 [84.0, 792] | 275 [94.0, 623] | 265 [84.0, 792] |
| Missing | 2 (1.0%) | 2 (3.3%) | 4 (1.6%) |
| Details of the Planned Surgery | |||
|---|---|---|---|
| No RBC Package Received (N = 191) | One or More RBC Packages Received (N = 61) | Overall (N = 252) | |
| Fracture | |||
| no | 141 (73.8%) | 38 (62.3%) | 179 (71.0%) |
| yes | 50 (26.2%) | 23 (37.7%) | 73 (29.0%) |
| Tumor | |||
| no | 162 (84.8%) | 48 (78.7%) | 210 (83.3%) |
| yes | 29 (15.2%) | 13 (21.3%) | 42 (16.7%) |
| Type of surgery | |||
| cervical spine | 59 (30.9%) | 12 (19.7%) | 71 (28.2%) |
| thoracic spine | 25 (13.1%) | 7 (11.5%) | 32 (12.7%) |
| lumbar spine | 82 (42.9%) | 23 (37.7%) | 105 (41.7%) |
| combination | 25 (13.1%) | 19 (31.1%) | 44 (17.5%) |
| Incision | |||
| dorsal incision | 145 (75.9%) | 54 (88.5%) | 199 (79.0%) |
| ventral incision | 46 (24.1%) | 7 (11.5%) | 53 (21.0%) |
| Vertebral body replacement | |||
| no vertebral body replacement | 175 (91.6%) | 47 (77.0%) | 222 (88.1%) |
| vertebral body replacement | 16 (8.4%) | 13 (21.3%) | 29 (11.5%) |
| missing | 0 (0%) | 1 (1.6%) | 1 (0.4%) |
| Stages | |||
| 0 | 93 (48.7%) | 11 (18.0%) | 104 (41.3%) |
| 1 | 28 (14.7%) | 4 (6.6%) | 32 (12.7%) |
| 2 | 38 (19.9%) | 19 (31.1%) | 57 (22.6%) |
| 3 | 14 (7.3%) | 10 (16.4%) | 24 (9.5%) |
| >3 | 18 (9.4%) | 17 (27.9%) | 35 (13.9%) |
| Risk Factor | Coefficient Estimate | Risk Points |
|---|---|---|
| Type of surgery | ||
| cervical spine | - | 0 |
| thoracic spine | 0.267 | 0 |
| lumbar spine | 1.099 | 1 |
| combination | 1.783 | 2 |
| Vertebral body replacement | ||
| no | - | 0 |
| yes | 0.841 | 1 |
| Stages | ||
| 0 | - | 0 |
| 1 | 0.593 | 1 |
| 2 | 1.805 | 2 |
| 3 | 2.260 | 3 |
| >3 | 2.122 | 3 |
| Hb (g/dL) | ||
| <8 | −0.665 | 7 |
| [8;12) | −0.665 | 5 |
| [12;16] | −0.665 | 2 |
| >16 | −0.665 | 0 |
| Score Value | Estimated Probability | Score Value | Estimated Probability |
|---|---|---|---|
| 0 | 0.13% | 7 | 31.13% |
| 1 | 0.29% | 8 | 51.16% |
| 2 | 0.67% | 9 | 70.82% |
| 3 | 1.54% | 10 | 84.91% |
| 4 | 3.5% | 11 | 92.88% |
| 5 | 7.76% | 12 | 96.8% |
| 6 | 16.32% | 13 | 98.59% |
| Patient | Risk Factor | Type of Surgery | Vetebral Body Replacement | Stages | Hb (g/dL) | Total Score Value | Estimated Probability |
|---|---|---|---|---|---|---|---|
| 1 | Risk category | lumbar spine | yes | 0 | 9.1 | 7 | 31.13% |
| Risk points | +1 | +1 | +0 | +5 | |||
| 2 | Risk category | combination | no | >3 | 11.7 | 10 | 84.91% |
| Risk points | +2 | +0 | +3 | +5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schenk, A.; Ende, J.; Hoch, J.; Güresir, E.; Grabert, J.; Coburn, M.; Schmid, M.; Velten, M. A Novel Scoring System Predicting Red Blood Cell Transfusion Requirements in Patients Undergoing Invasive Spine Surgery. J. Clin. Med. 2024, 13, 948. https://doi.org/10.3390/jcm13040948
Schenk A, Ende J, Hoch J, Güresir E, Grabert J, Coburn M, Schmid M, Velten M. A Novel Scoring System Predicting Red Blood Cell Transfusion Requirements in Patients Undergoing Invasive Spine Surgery. Journal of Clinical Medicine. 2024; 13(4):948. https://doi.org/10.3390/jcm13040948
Chicago/Turabian StyleSchenk, Alina, Jonas Ende, Jochen Hoch, Erdem Güresir, Josefin Grabert, Mark Coburn, Matthias Schmid, and Markus Velten. 2024. "A Novel Scoring System Predicting Red Blood Cell Transfusion Requirements in Patients Undergoing Invasive Spine Surgery" Journal of Clinical Medicine 13, no. 4: 948. https://doi.org/10.3390/jcm13040948
APA StyleSchenk, A., Ende, J., Hoch, J., Güresir, E., Grabert, J., Coburn, M., Schmid, M., & Velten, M. (2024). A Novel Scoring System Predicting Red Blood Cell Transfusion Requirements in Patients Undergoing Invasive Spine Surgery. Journal of Clinical Medicine, 13(4), 948. https://doi.org/10.3390/jcm13040948







