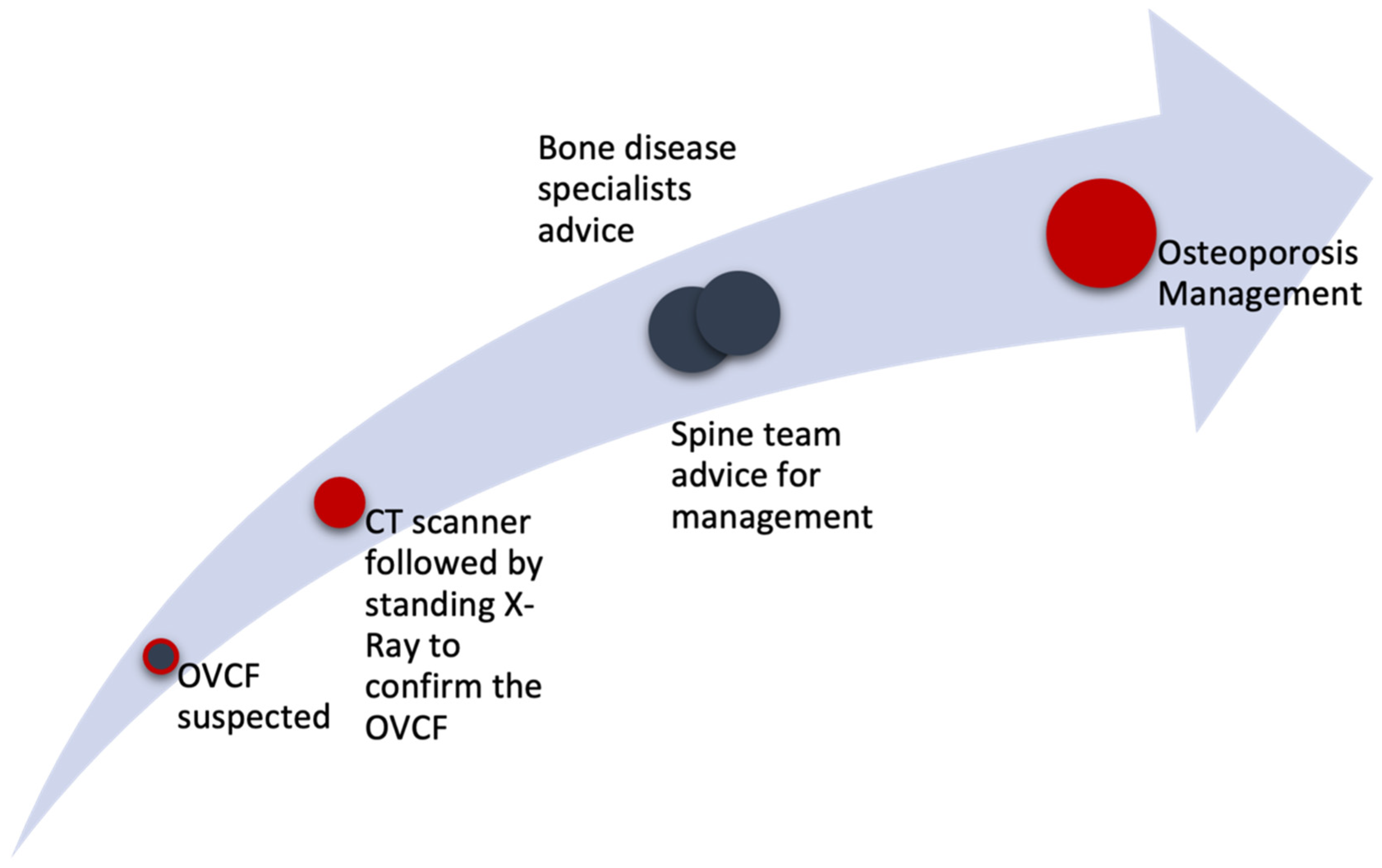
Multidisciplinary and Coordinated Management of Osteoporotic Vertebral Compression Fractures: Current State of the Art
Abstract
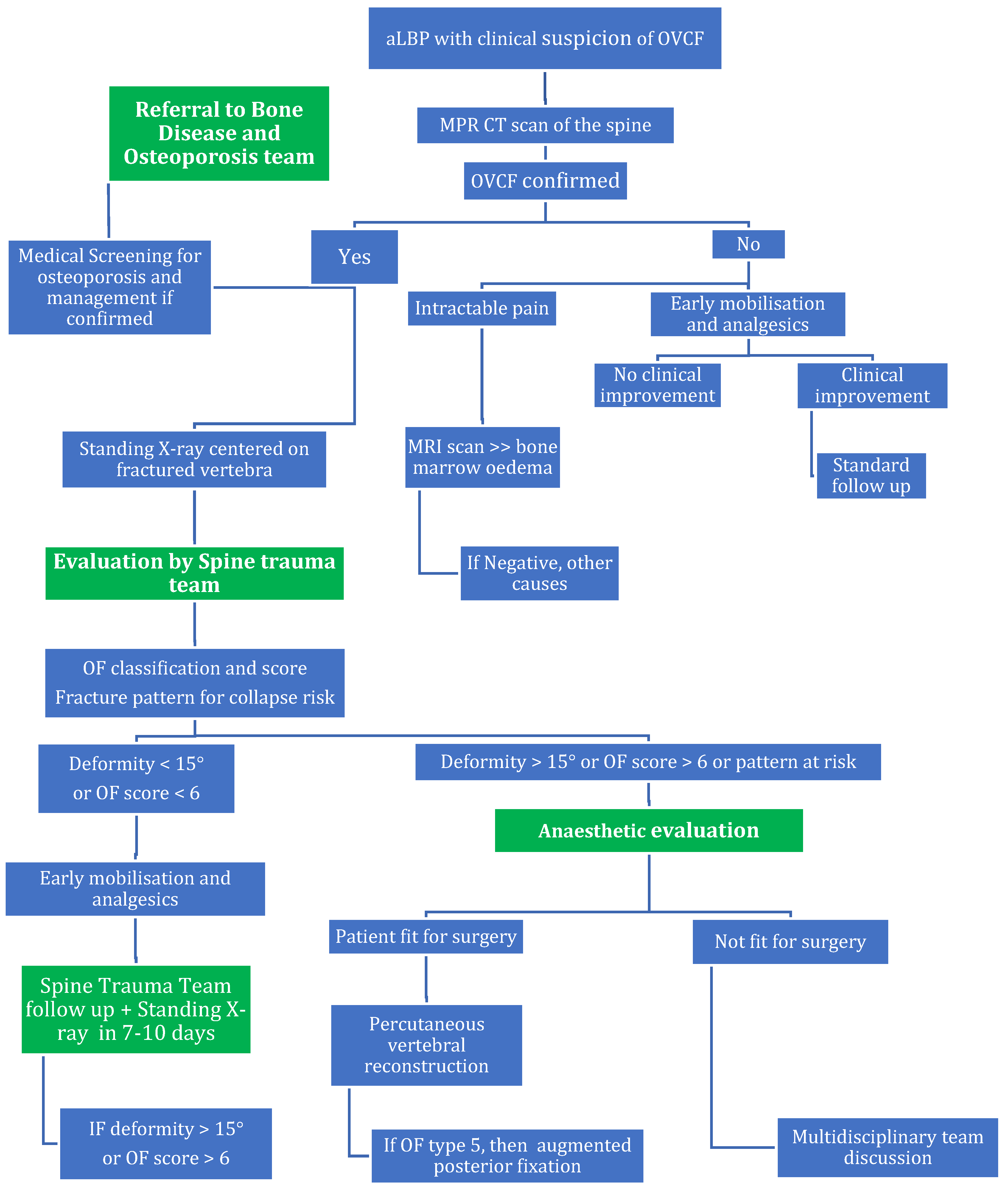
1. Background
2. Material and Methods
2.1. Who Needs Radiological Assessment?
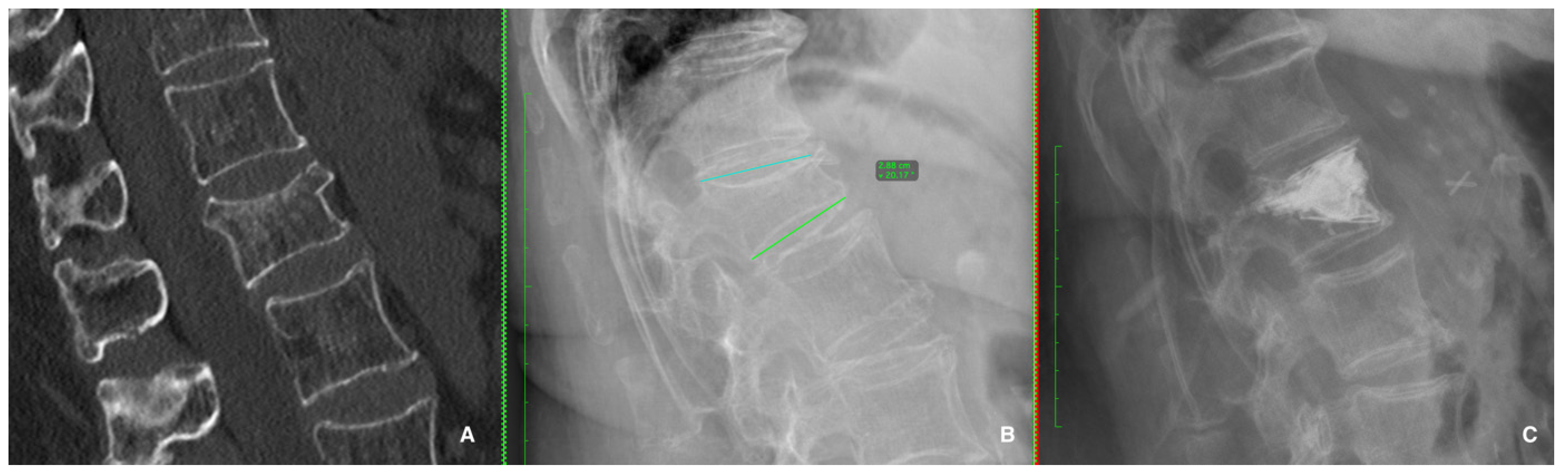
2.2. What Imaging Needs to Be Requested?
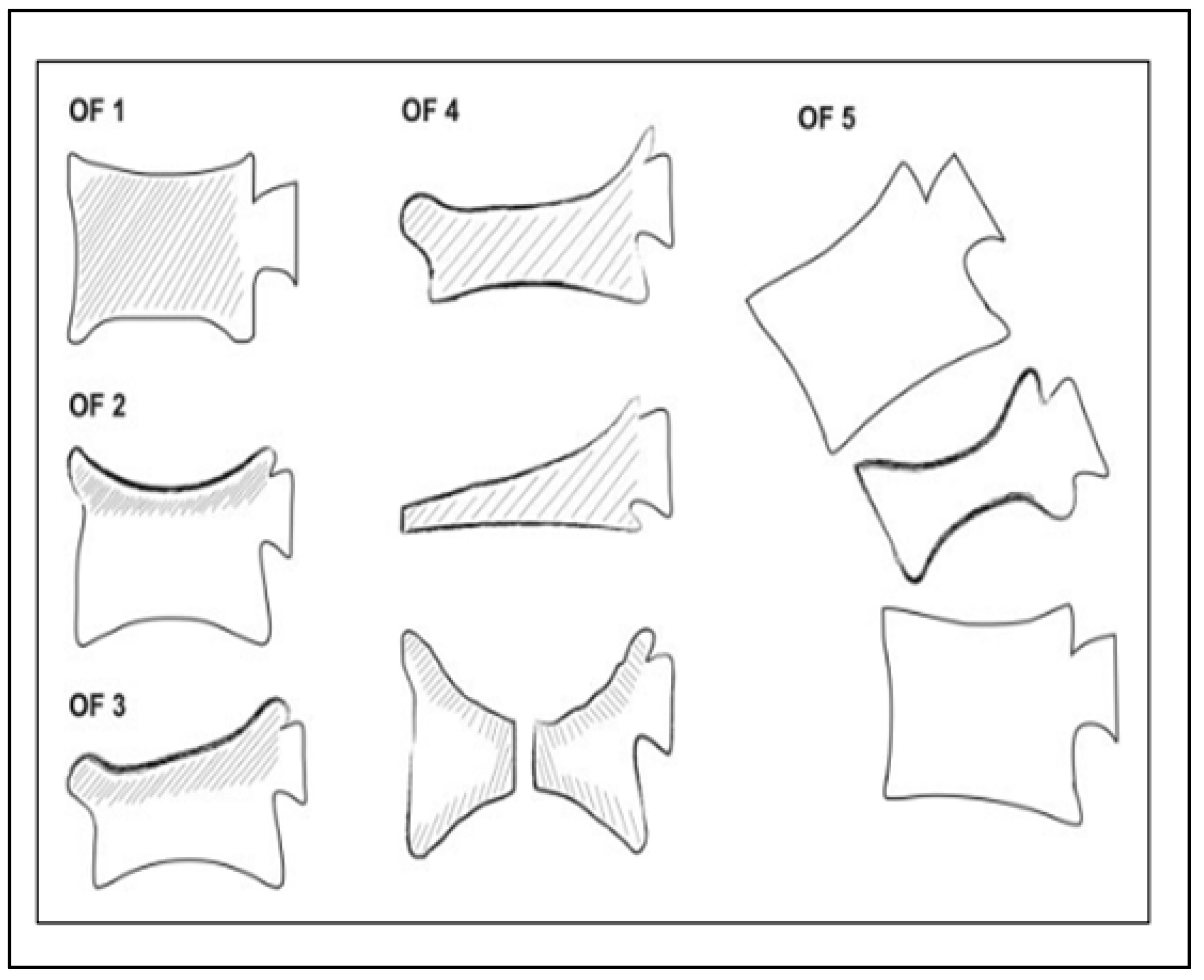
2.3. Is There a Specific Classification System for Osteoporotic Fractures?
2.4. Medical Management of Pain and Osteoporosis
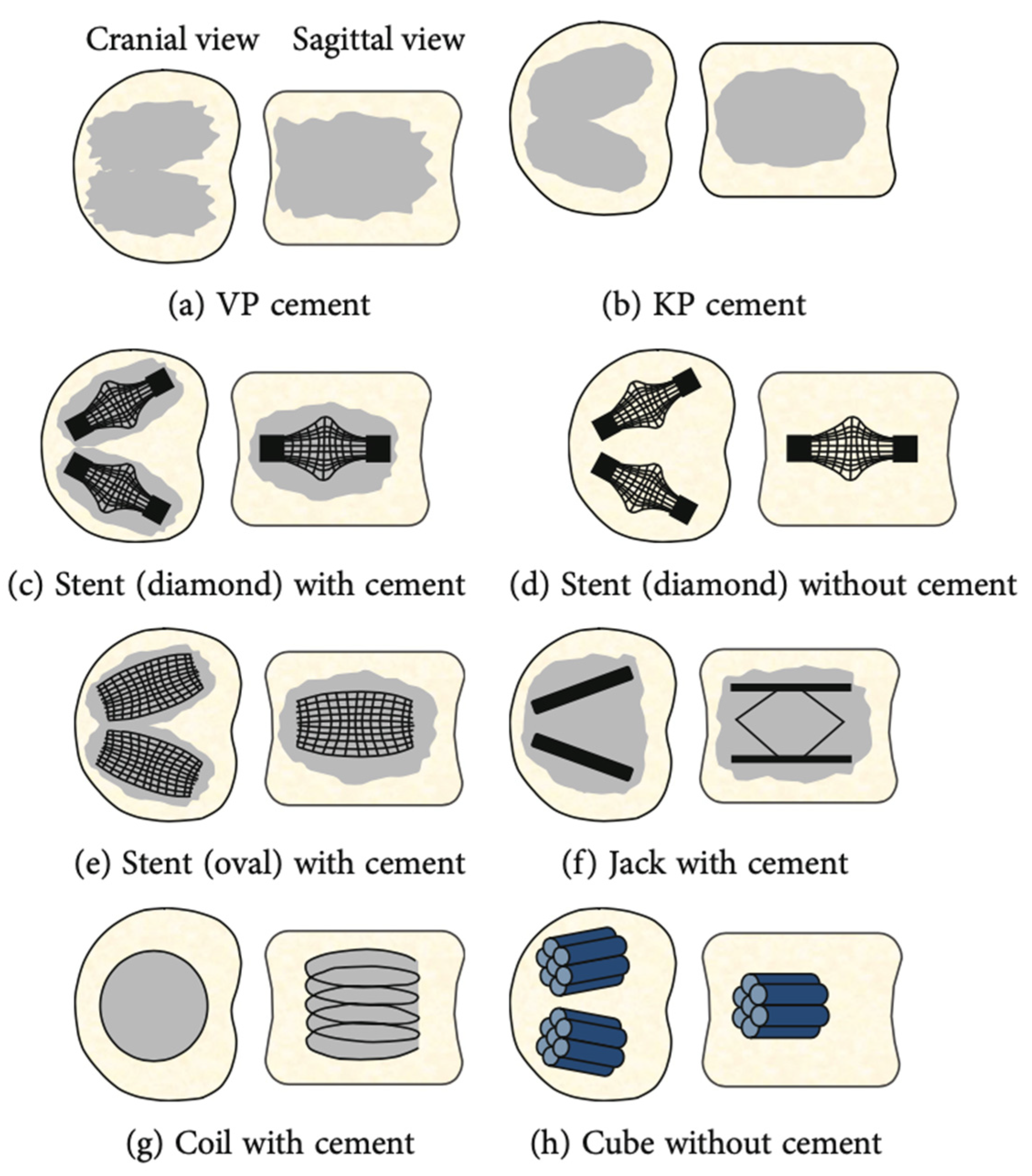
2.5. Conservative Therapy or Surgical Management for OVCFs?
3. Discussion
4. Conclusions
Funding
Conflicts of Interest
References
- Noriega, D.; Marcia, S.; Theumann, N.; Blondel, B.; Simon, A.; Hassel, F.; Maestretti, G.; Petit, A.; Weidle, P.A.; Mandly, A.G.; et al. A prospective, international, randomized, noninferiority study comparing an implantable titanium vertebral augmentation device versus balloon kyphoplasty in the reduction of vertebral compression fractures (SAKOS study). Spine J. 2019, 19, 1782–1795. [Google Scholar] [CrossRef] [PubMed]
- Ballane, G.; Cauley, J.A.; Luckey, M.M.; El-Hajj Fuleihan, G. Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos. Int. 2017, 28, 1531–1542. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, T.W.; Felsenberg, D.; Varlow, J.; Cooper, C.; Kanis, J.A.; Silman, A.J. The prevalence of vertebral deformity in european men and women: The European Vertebral Osteoporosis Study. J. Bone Miner. Res. 1996, 11, 1010–1018. [Google Scholar] [CrossRef] [PubMed]
- Long, Y.; Yi, W.; Yang, D. Advances in vertebral augmentation systems for osteoporotic vertebral compression fractures. Pain. Res. Manag. 2020, 2020, 3947368. [Google Scholar] [CrossRef] [PubMed]
- European Prospective Osteoporosis Study (EPOS) Group; Felsenberg, D.; Silman, A.J.; Lunt, M.; Armbrecht, G.; Ismail, A.A.; Finn, J.D.; Cockerill, W.C.; Banzer, D.; Benevolenskaya, L.I.; et al. Incidence of vertebral fracture in Europe: Results from the European Prospective Osteoporosis Study (EPOS). J. Bone Miner. Res. 2002, 17, 716–724. [Google Scholar] [CrossRef] [PubMed]
- Jalava, T.; Sarna, S.; Pylkkänen, L.; Mawer, B.; Kanis, J.A.; Selby, P.; Davies, M.; Adams, J.; Francis, R.M.; Robinson, J.; et al. Association between vertebral fracture and increased mortality in osteoporotic patients. J. Bone Miner. Res. 2003, 18, 1254–1260. [Google Scholar] [CrossRef]
- Son, H.J.; Park, S.J.; Kim, J.K.; Park, J.S. Mortality risk after the first occurrence of osteoporotic vertebral compression fractures in the general population: A nationwide cohort study. PLoS ONE 2023, 18, e0291561. [Google Scholar] [CrossRef]
- Parreira, P.; Maher, C.; Megale, R.; March, L.; Ferreira, M. An overview of clinical guidelines for the management of vertebral compression fracture: A systematic review. Spine J. 2017, 17, 1932–1938. [Google Scholar] [CrossRef]
- Depalma, M. Red flags of low back pain. JAAPA 2020, 33, 8–11. [Google Scholar] [CrossRef]
- Enthoven, W.; Geuze, J.; Scheele, J.; Bierma-Zeinstra, S.; Bueving, H.; Bohnen, A.; Peul, W.; Van Tulder, M.; Berger, M.; Koes, B.; et al. Prevalence and “red flags” regarding specified causes of back pain in older adults presenting in gen-eral practice. Phys. Ther. 2016, 96, 305–312. [Google Scholar] [CrossRef]
- Pedersen, V.; Lampart, A.; Bingisser, R.; Nickel, C.H. Accuracy of plain radiography in detecting fractures in older individuals after low-energy falls: Current evidence. Trauma. Surg. Acute Care Open 2020, 5, E000560. [Google Scholar] [CrossRef]
- Ruiz Santiago, F.; Láinez Ramos-Bossini, A.J.; Wáng, Y.X.J.; López Zúñiga, D. The role of radiography in the study of spinal disorders. Quant. Imaging Med. Surg. 2020, 10, 2322–2355. [Google Scholar] [CrossRef]
- Balasubramanian, A.; Zhang, J.; Chen, L.; Wenkert, D.; Daigle, S.G.; Grauer, A.; Curtis, J.R. Risk of subsequent fracture after prior fracture among older women. Osteoporos. Int. 2019, 30, 79–92. [Google Scholar] [CrossRef] [PubMed]
- Johansson, H.; Siggeirsdóttir, K.; Harvey, N.C.; Odén, A.; Gudnason, V.; Mccloskey, E.; Sigurdsson, G.; Kanis, J.A. Imminent risk of fracture after fracture. Osteoporos. Int. 2017, 28, 775–780. [Google Scholar] [CrossRef] [PubMed]
- Kanis, J.A.; Johansson, H.; Odén, A.; Harvey, N.C.; Gudnason, V.; Sanders, K.M.; Sigurdsson, G.; Siggeirsdottir, K.; Fitzpat-RICK, L.A.; Borgström, F.; et al. Characteristics of recurrent fractures. Osteoporos. Int. 2018, 29, 1747–1757. [Google Scholar] [CrossRef] [PubMed]
- Zvekic-Svorcan, J.; Aleksic, J.; Jankovic, T.; Filipovic, K.; Cvetkovic, M.; Vuksanovic, M.; Filipov, P. Capture the vertebral fracture: Risk factors as a prediction. J. Back. Musculoskelet. Rehabil. 2019, 32, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Vandenberg, J.; Cullison, K.; Fowler, S.A.; Parsons, M.S.; Mcandrew, C.M.; Carpenter, C.R. Blunt thoracolumbar-spine trauma evaluation in the emergency department: A meta-analysis of diagnostic accuracy for history, physical examination, and imaging. J. Emerg. Med. 2019, 56, 153–165. [Google Scholar] [CrossRef]
- Lampart, A.; Arnold, I.; Mäder, N.; Niedermeier, S.; Escher, A.; Stahl, R.; Trumm, C.; Kammerlander, C.; Böcker, W.; Nickel, C.; et al. Prevalence of fractures and diagnostic accuracy of emergency X-ray in older adults sus-taining a low-energy fall: A retrospective study. J. Clin. Med. 2020, 9, 97. [Google Scholar] [CrossRef]
- Ruiz Santiago, F.; Láinez Ramos-Bossini, A.J.; Wáng, Y.X.J.; Martínez Barbero, J.P.; García Espinosa, J.; Martínez Martínez, A. The value of magnetic resonance imaging and computed tomography in the study of spinal disorders. Quant. Imaging Med. Surg. 2022, 12, 3947–3986. [Google Scholar] [CrossRef]
- Diacinti, D.; Guglielmi, G. Vertebral morphometry. Radiol. Clin. N. Am. 2010, 48, 561–575. [Google Scholar] [CrossRef]
- Diacinti, D.; Pisani, D.; Del Fiacco, R.; Francucci, C.M.; Fiore, C.E.; Frediani, B.; Barone, A.; Bartalena, T.; Cattaruzza, M.S.; Guglielmi, G.; et al. Vertebral morphometry by X-ray absorptiometry: Which reference data for vertebral heights? Bone 2011, 49, 526–536. [Google Scholar] [CrossRef]
- Takahashi, S.; Hoshino, M.; Takayama, K.; Iseki, K.; Sasaoka, R.; Tsujio, T.; Yasuda, H.; Sasaki, T.; Kanematsu, F.; Kono, H.; et al. Time course of osteoporotic vertebral fractures by magnetic resonance imaging using a simple classification: A multicenter prospective cohort study. Osteoporos. Int. 2017, 28, 473–482. [Google Scholar] [CrossRef] [PubMed]
- Sugita, M.; Watanabe, N.; Mikami, Y.; Hase, H.; Kubo, T. Classification of vertebral compression fractures in the osteopo-rotic spine. J. Spinal Disord. Tech. 2005, 18, 376–381. [Google Scholar] [CrossRef] [PubMed]
- Genant, H.K.; Wu, C.Y.; Van Kuijk, C.; Nevitt, M.C. Vertebral fracture assessment using a semiquantitative technique. J. Bone Min. Res. 1993, 8, 1137–1148. [Google Scholar] [CrossRef]
- Schnake, K.J.; Blattert, T.R.; Hahn, P.; Franck, A.; Hartmann, F.; Ullrich, B.; Verheyden, A.; Mörk, S.; Zimmermann, V.; Gonschorek, O.; et al. Classification of osteoporotic thoracolumbar spine fractures: Recommendations of the spine section of the german society for orthopaedics and trauma (DGOU). Global Spine J. 2018, 8, 46S–49S. [Google Scholar] [CrossRef]
- Blattert, T.R.; Schnake, K.J.; Gonschorek, O.; Gercek, E.; Hartmann, F.; Katscher, S.; Mörk, S.; Morrison, R.; Müller, M.; Partenheimer, A.; et al. Nonsurgical and surgical management of osteoporotic vertebral body fractures: Recommendations of the spine section of the german society for orthopaedics and trauma (DGOU). Global Spine J. 2018, 8, 50S–55S. [Google Scholar] [CrossRef]
- Gold, D.T. The clinical impact of vertebral fractures: Quality of life in women with osteoporosis. Bone 1996, 18, S185–S189. [Google Scholar] [CrossRef] [PubMed]
- Scheyerer, M.J.; Spiegl, U.J.A.; Grueninger, S.; Hartmann, F.; Katscher, S.; Osterhoff, G.; Perl, M.; Pumberger, M.; Schmeiser, G.; Ullrich, B.W.; et al. Risk factors for failure in conservatively treated osteoporotic vertebral fractures: A systematic review. Glob. Spine J. 2022, 12, 289–297. [Google Scholar] [CrossRef]
- Zhang, J.N.; He, X.; Fan, Y.; Du, J.P.; Hao, D.J. Risk factors for conservative treatment failure in acute osteoporotic vertebral compression fractures (OVCFs). Arch. Osteoporos. 2019, 14, 24. [Google Scholar] [CrossRef]
- Lee, H.M.; Park, S.Y.; Lee, S.H.; Suh, S.W.; Hong, J.Y. Comparative analysis of clinical outcomes in patients with osteoporotic vertebral compression fractures (OVCFs): Conservative treatment versus balloon kyphoplasty. Spine J. 2012, 12, 998–1005. [Google Scholar] [CrossRef]
- Park, H.Y.; Ahn, J.H.; Ha, K.Y.; Kim, Y.H.; Kim, S.I.; Min, H.K.; Oh, I.S.; Seo, J.Y.; Park, S.H. Clinical and radiologic features of osteoporotic spine fracture with delayed neurologic compromises. World Neurosurg. 2018, 120, E1295–E1300. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, T.; Maeda, T.; Masuda, M.; Ueta, T.; Shiba, K. Morphology of the injured posterior wall causing spinal canal en-croachment in osteoporotic vertebral fractures. Spine J. 2016, 16, 946–950. [Google Scholar] [CrossRef]
- Hoshino, M.; Tsujio, T.; Terai, H.; Namikawa, T.; Kato, M.; Matsumura, A.; Suzuki, A.; Takayama, K.; Takaoka, K.; Nakamura, H. Impact of initial conservative treatment interventions on the outcomes of patients with osteoporotic vertebral fractures. Spine 2013, 38, E641–E648. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, S.; Smorgick, Y.; Mirovsky, Y.; Anekstein, Y.; Blecher, R.; Tal, S. Clinical and radiological factors affecting progressive collapse of acute osteoporotic compression spinal fractures. J. Clin. Neurosci. 2016, 31, 122–126. [Google Scholar] [CrossRef] [PubMed]
- Ha, K.Y.; Kim, Y.H. Risk factors affecting progressive collapse of acute osteoporotic spinal fractures. Osteoporos. Int. 2013, 24, 1207–1213. [Google Scholar] [CrossRef]
- Patil, S.; Nene, A.M. Predictors of kyphotic deformity in osteoporotic vertebral compression fractures: A radiological study. Eur. Spine J. 2014, 23, 2737–2742. [Google Scholar] [CrossRef]
- Nakamae, T.; Fujimoto, Y.; Yamada, K.; Hiramatsu, T.; Hashimoto, T.; Olmarker, K.; Adachi, N. Relationship between clini-cal symptoms of osteoporotic vertebral fracture with intravertebral cleft and radiographic findings. J. Orthop. Sci. 2017, 22, 201–206. [Google Scholar] [CrossRef]
- Ohnishi, T.; Iwata, A.; Kanayama, M.; Oha, F.; Hashimoto, T.; Iwasaki, N. Impact of spino-pelvic and global spinal alignment on the risk of osteoporotic vertebral collapse. Spine Surg. Relat. Res. 2018, 2, 72–76. [Google Scholar] [CrossRef]
- Iwata, A.; Kanayama, M.; Oha, F.; Hashimoto, T.; Iwasaki, N. Does spinopelvic alignment affect the union status in thoracolumbar osteoporotic vertebral compression fracture? Eur. J. Orthop. Surg. Traumatol. 2017, 27, 87–92. [Google Scholar] [CrossRef]
- Smorgick, Y.; Gefler, A.; Goldstein, S.; Mirovsky, Y.; Blecher, R.; Anekstein, Y. Determination of any correlation between sagittal spinopelvic configuration and progressive collapse of acute osteoporotic compression spine fractures: A retrospective radiological analysis. Asian Spine J. 2020, 14, 872–877. [Google Scholar] [CrossRef]
- Ha, K.Y.; Park, K.S.; Kim, S.I.; Kim, Y.H. Does bisphosphonate-based anti-osteoporosis medication affect osteoporotic spinal fracture healing? Osteoporos. Int. 2016, 27, 483–488. [Google Scholar] [CrossRef]
- Willers, C.; Norton, N.; Harvey, N.C.; Jacobson, T.; Johansson, H.; Lorentzon, M.; Mccloskey, E.V.; Borgström, F.; Kanis, J.A. Osteo-porosis in europe: A compendium of country-specific reports. Arch. Osteoporos. 2022, 17, 23. [Google Scholar] [CrossRef]
- Davis, S.; Simpson, E.; Hamilton, J.; James, M.M.; Rawdin, A.; Wong, R.; Goka, E.; Gittoes, N.; Selby, P. Denosumab, raloxifene, romosozumab and teriparatide to prevent osteoporotic fragility fractures: A systematic review and economic evaluation. Health Technol. Assess. 2020, 24, 1–314. [Google Scholar] [CrossRef]
- Reid, I.R.; Billington, E.O. Drug therapy for osteoporosis in older adults. Lancet 2022, 399, 1080–1092. [Google Scholar] [CrossRef]
- Händel, M.N.; Cardoso, I.; Von Bülow, C.; Rohde, J.F.; Ussing, A.; Nielsen, S.M.; Christensen, R.; Body, J.J.; Brandi, M.L.; Diez-Perez, A.; et al. Fracture risk reduction and safety by osteoporosis treatment compared with placebo or active comparator in postmenopausal women: Systematic review, network meta-analysis, and metaregression analysis of randomised clinical trials. BMJ 2023, 381, E068033. [Google Scholar] [CrossRef]
- Kendler, D.L.; Marin, F.; Zerbini, C.A.F.; Russo, L.A.; Greenspan, S.L.; Zikan, V.; Bagur, A.; Malouf-Sierra, J.; Lakatos, P.; Fahrleitner-Pammer, A.; et al. Effects of teri-paratide and risedronate on new fractures in post-menopausal women with severe osteoporosis (VERO): A multicentre, double-blind, double-dummy, randomised controlled trial. Lancet 2018, 391, 230–240. [Google Scholar] [CrossRef]
- Saag, K.G.; Petersen, J.; Brandi, M.L.; Karaplis, A.C.; Lorentzon, M.; Thomas, T.; Maddox, J.; Fan, M.; Meisner, P.D.; Grauer, A. Romosozumab or alendronate for fracture prevention in women with osteoporosis. N. Engl. J. Med. 2017, 377, 1417–1427. [Google Scholar] [CrossRef] [PubMed]
- Kanis, J.A.; Cooper, C.; Rizzoli, R.; Reginster, J.Y. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos. Int. 2019, 30, 3–44. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, S.; Lippuner, K.; Lamy, O.; Meier, C. 2020 recommendations for osteoporosis treatment according to fracture risk from the swiss association against osteoporosis (SVGO). Swiss Med. Wkly. 2020, 150, W20352. [Google Scholar] [CrossRef] [PubMed]
- Qaseem, A.; Hicks, L.A.; Etxeandia-Ikobaltzeta, I.; Shamliyan, T.; Cooney, T.G.; Cross, J.T., Jr.; Fitterman, N.; Lin, J.S.; Maro-To, M.; Obley, A.J.; et al. Pharmacologic treatment of primary osteoporosis or low bone mass to prevent fractures in adults: A living clinical guideline from the american college of physicians. Ann. Intern. Med. 2023, 176, 224–238. [Google Scholar] [CrossRef] [PubMed]
- Nevitt, M.C.; Chen, P.; Dore, R.K.; Reginster, J.Y.; Kiel, D.P.; Zanchetta, J.R.; Glass, E.V.; Krege, J.H. Reduced risk of back pain following teriparatide treatment: A meta-analysis. Osteoporos. Int. 2006, 17, 273–280. [Google Scholar] [CrossRef]
- Kim, G.H.; Cho, T.G. A comparative study on the treatment of osteoporotic vertebral compression fractures with early ambulation and at leat 1 week of absolute bed rest. Korean J. Neurotrauma 2022, 18, 56–63. [Google Scholar] [CrossRef]
- Ambrecht, G.; Belavy, D.L.; Backström, M.; Beller, G.; Alexandre, C.; Rizzoli, R.; Felsenberg, D. Trabecular and cortical bone density and architecture in women after 60 days of bed rest using high-resolution pQCT: WISE 2005. J Bone Miner Res. 2011, 26, 2399–2410. [Google Scholar] [CrossRef]
- Kehler, D.S.; Theou, O.; Rockwood, K. Bed rest and accelerated aging in relation to the musculoskeletal and cardiovascular systems and frailty biomarkers: A review. Exp. Gerontol. 2019, 124, 110643. [Google Scholar] [CrossRef]
- Petitt, J.C.; Desai, A.; Kashkoush, A.; Ahorukomeye, P.; Potter, T.O.; Stout, A.; Kelly, M.L. Failure of conservatively managed traumatic vertebral compression fractures: A systematic review. World Neurosurg. 2022, 165, 81–88. [Google Scholar] [CrossRef]
- Ozdemir, M.; Bayram, S.; Karalar, S.; Korkmaz, M.; Sulejmani, I.; Sivacioglu, S.; Akgul, T. investigation of possible reasons of failed treatment of conservative thoracolumbar osteoporotic vertebral fractures. Turk. Neurosurg. 2023, 33, 70–76. [Google Scholar] [CrossRef]
- Viswanathan, V.; Shetty, A.; Sindhiya, N.; Kanna, R.; Rajasekaran, S. Prospective study to identify the clinical and radiologic factors predictive of pseudarthrosis development in patients with osteoporotic vertebral fractures. World Neurosurg. 2022, 167, E350–E359. [Google Scholar] [CrossRef]
- Hofler, R.; Jones, G.A. Bracing for acute and subacute osteoporotic compression fracture: A systematic review of literature. World Neurosurg. 2020, 141, E453–E460. [Google Scholar] [CrossRef]
- Giangregorio, L.; Maclntyre, N.; Thabane, L.; Skidmore, C.; Papaioannou, A. Exercise for improving outcomes after osteoporotic vertebral fracture. Cochrane Database Syst. Rev. 2019, 7, CD008618. [Google Scholar] [CrossRef]
- Percutaneous Insertion of Craniocaudal Expandable Implants for Vertebral Compression Fracture Interventional Procedures Guidance [IPG568]. Available online: www.nice.org.uk/guidance/ipg568 (accessed on 23 November 2016).
- Kim, W.; Ma, S.; Shin, H.; Song, D.; Lee, J.; Chang, S.; Park, K.; Choy, W.; Oh, T. Correlation of sagittal imbalance and recollapse after percutaneous vertebroplasty for thoracolumbar osteoporotic vertebral compression fracture: A multivariate study of risk factors. Asian Spine J. 2021, 16, 231–240. [Google Scholar] [CrossRef]
- Zhai, G.; Li, A.; Liu, B.; Lv, D.; Zhang, J.; Sheng, W.; Yang, G.; Gao, Y. A meta-analysis of the secondary fractures for osteoporotic vertebral compression fractures after percutaneous vertebroplasty. Medecine 2021, 100, E25396. [Google Scholar] [CrossRef]
- Kutsal, F.Y.; Ergin Ergani, G.O. Vertebral compression fractures: Still an unpredictable aspect of osteoporosis. Turk. J. Med. Sci. 2021, 52, 393–399. [Google Scholar] [CrossRef]
- Rosen, H.N.; Walega, D.R. Osteoporotic Thoracolumbar Vertebral Compression Fractures: Clinical Manifestations and Treatment. Rosen, C.J., Mudler, J.E., Eds.; Uptodate 2020. Available online: https://www.uptodate.com/contents/osteoporotic-thoracolumbar-vertebral-compression-fractures-clinical-manifestations-and-treatment#! (accessed on 8 January 2024).
- Mccarthy, J.; Davis, A. Diagnosis and management of vertebral compression fractures. Am. Fam. Physician 2016, 94, 44–50. [Google Scholar]
- Momomura, R.; Shirmamura, Y.; Kaneko, K. Postopertative clinical outcomes of balloon kyphoplasty treatment: Would adherence to indication and contraindications prevent complications? Asian Spine J. 2019, 14, 198–203. [Google Scholar] [CrossRef]
- Hirsch, J.A.; Chandra, R.V.; Carter, N.S.; Beall, D.; Frohbergh, M.; Ong, K. Number needed to treat with vertebral augmentation to save a life. Ajnr Am. J. Neuroradiol. 2020, 41, 178–182. [Google Scholar] [CrossRef]
- Beall, D.; Lorio, M.P.; Yun, B.M.; Runa, M.J.; Ong, K.L.; Warner, C.B. Review of vertebral augmentation: An updated metaanalysis of the effectiveness. Int. J. Spine Surg. 2018, 12, 295–321. [Google Scholar] [CrossRef]
- Hoyt, D.; Urits, I.; Orhurhu, V.; Orhurhu, M.S.; Callan, J.; Powell, J.; Manchikanti, L.; Kaye, A.D.; Kaye, R.J.; Viswanath, O. Current concept in the management of vertebral compression fractures. Curr. Pain. Headache Rep. 2020, 24, 16. [Google Scholar] [CrossRef]
- Hinde, K.; Maingard, J.; Hirsch, J.A.; Phan, K.; Asadi, H.; Chandra, R.V. Mortality outcomes of vertebral augmentation (vertebroplasty and/or balloon kyphoplasty) for osteoporotic vertebral compression fractures: A systematic review and meta-analysis. Radiology 2020, 295, 96–103. [Google Scholar] [CrossRef]
- Noriega, D.; Maestretti, G.; Renaud, C.; Francaviglia, N.; Ould-Slimane, M.; Queinnec, S.; Ekkerlein, H.; Hassel, F.; Gum-Pert, R.; Sabatier, P.; et al. Clinical performance and safety of 108 spinejack implantations: 1-year results of a prospective multicenter single-arm registery study. Biomed. Res. Int. 2015, 2015, 173872. [Google Scholar] [CrossRef]
- Gajavelli, S.; Gee, A.; Bagheri, Z.S.; Schemitsch, E.H.; Bailey, C.S.; Rasoulinejad, P.; Zdero, R. A 20-year review of biomechanical experimental studies on spine implants used for percutaneous surgical repair of vertebral compression fractures. Biomed. Res. Int. 2022, 21, 6015067. [Google Scholar] [CrossRef]
- Capozzi, A.; Scambia, G.; Pedicelli, A.; Evangelista, M.; Sorge, R.; Lello, S. Clinical management of osteoporotic vertebral fracture treated with percutaneous vertebroplasty. Clin. Cases Miner. Bone Metab. 2017, 14, 161–166. [Google Scholar] [CrossRef]
- Skorupski, N.; Alexander, I.M. Multidisciplinary osteoporosis management of post low-energy trauma hip-fracture patients. J. Am. Assoc. Nurse Pract. 2013, 25, 3–10. [Google Scholar] [CrossRef]
- Osuna, P.M.; Ruppe, M.D.; Tabatabai, L.S. Fracture liaison services: Multidisciplinary approaches to secondary fracture prevention. Endocr. Pract. 2017, 23, 199–206. [Google Scholar] [CrossRef]

| Study | Related Complication | Risk Factors |
|---|---|---|
| Park H.Y. et al. (2018) [31] Hayashi T. et al. (2016) [32] | Vertebral collapse and spinal canal compromise and/or delayed neurological deficit | Posterior wall involvement, initial height loss, midportion-type fractures, swelled-front-type fractures, complex fracture morphology, intravertebral cleft development, fracture instability, fractures at the thoracolumbar junction and specific MRI changes |
| Sugita M. et al. (2005) [23] Hoshino M. et al. (2013) [33] | Poor clinical outcome | Bow-shaped type fractures, projecting type fractures, swelled-front-type fractures and posterior wall fractures |
| Goldstein S. et al. (2016) [34] Ha K.Y. et al. (2013) [35] Patil S. et al. (2014) [36] | Progressive vertebral collapse or progressive kyphotic deformity | Location at thoracolumbar junction, midportion-type fractures, intervertebral cleft development, specific fracture types, posterior wall fractures, superior endplate involvement, anterior wall fractures and previous adjacent level fractures |
| Nakamae T. et al. (2017) [37] | Symptomatic intravertebral cleft | Posterior wall fracture and vertebral instability |
| Ohnishi T. et al. (2018) [38] Iwata A. et al. (2017) [39] Smorgick Y. et al. (2020) [40] | Poor outcome (pain) and subsequent fracture | Values outside of specific ranges associated
|
| Zhang JN, He X, Fan Y et al. (2019) [29] Lee H.M., Park S.Y., Lee S.H. et al. (2012) [30] | Poor outcome (pain control) | age > 73 years, bone mineral density with a t-score < −2.95 SD, BMI < 23 kg/m2 and a modified frailty index > 2.5 |
| Basic Laboratory Tests for All Patients with Vertebral Fracture | Additional Laboratory Tests according to the Patient’s Clinical History, Physical Examination and Basic Laboratory Tests |
|---|---|
|
|
| Drug and Bone Mechanism of Action | Main Side Effects and/or Contraindications |
|---|---|
Inhibitors of bone resorption:
|
|
Activators of bone formation:
|
|
Mixed effect: Activators of bone formation and Inhibitors of bone resorption
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al Taha, K.; Lauper, N.; Bauer, D.E.; Tsoupras, A.; Tessitore, E.; Biver, E.; Dominguez, D.E. Multidisciplinary and Coordinated Management of Osteoporotic Vertebral Compression Fractures: Current State of the Art. J. Clin. Med. 2024, 13, 930. https://doi.org/10.3390/jcm13040930
Al Taha K, Lauper N, Bauer DE, Tsoupras A, Tessitore E, Biver E, Dominguez DE. Multidisciplinary and Coordinated Management of Osteoporotic Vertebral Compression Fractures: Current State of the Art. Journal of Clinical Medicine. 2024; 13(4):930. https://doi.org/10.3390/jcm13040930
Chicago/Turabian StyleAl Taha, Khalid, Nicolas Lauper, David E. Bauer, Andreas Tsoupras, Enrico Tessitore, Emmanuel Biver, and Dennis E. Dominguez. 2024. "Multidisciplinary and Coordinated Management of Osteoporotic Vertebral Compression Fractures: Current State of the Art" Journal of Clinical Medicine 13, no. 4: 930. https://doi.org/10.3390/jcm13040930
APA StyleAl Taha, K., Lauper, N., Bauer, D. E., Tsoupras, A., Tessitore, E., Biver, E., & Dominguez, D. E. (2024). Multidisciplinary and Coordinated Management of Osteoporotic Vertebral Compression Fractures: Current State of the Art. Journal of Clinical Medicine, 13(4), 930. https://doi.org/10.3390/jcm13040930







