Comparison of In-Hospital Outcomes between Early and Late Catheter-Directed Thrombolysis in Acute Pulmonary Embolism: A Retrospective Observational Study
Abstract
1. Introduction
2. Methodology
2.1. Database
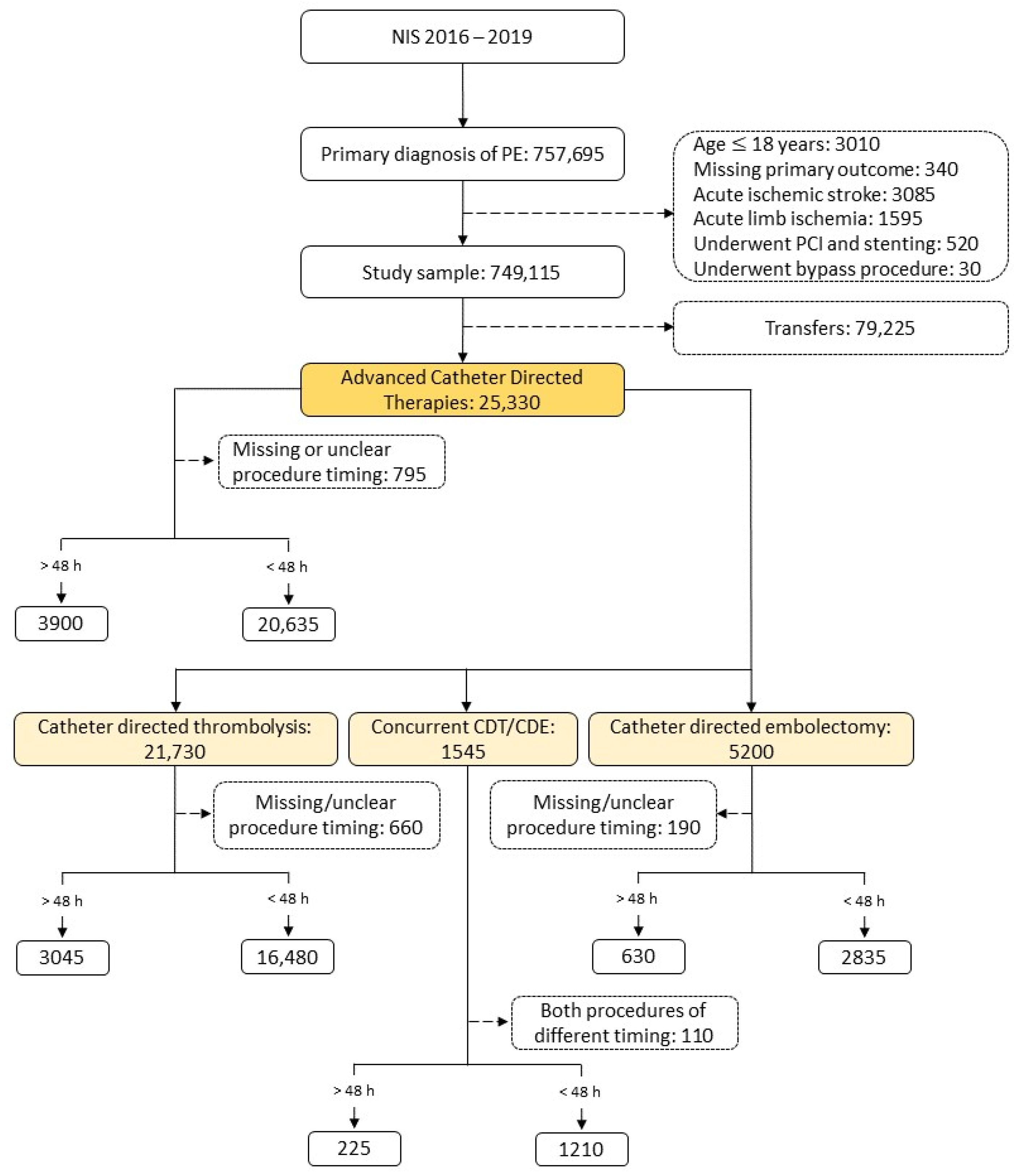
2.2. Sample Extraction
2.3. Comorbidities Identification
2.4. Exposure and Outcomes
2.5. Statistical Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACBT | advanced catheter-based therapies |
| aOR | adjusted odds ratio |
| CAD | coronary artery disease |
| CDE | catheter-directed embolectomy |
| CDT | catheter-directed thrombolysis |
| CCI | Charlson’s comorbidity index |
| COPD | chronic obstructive pulmonary disease |
| DM | diabetes mellitus |
| ECMO | extracorporeal membrane oxygenation |
| HLD | hyperlipidemia |
| HTN | hypertension |
| ICD | international classification of disease |
| PE | pulmonary embolism |
| PVD | peripheral vascular disease |
| US-CDT | ultrasound facilitated catheter-directed thrombolysis |
References
- Tsao, C.W.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Beaton, A.Z.; Boehme, A.K.; Buxton, A.E.; et al. Heart Disease and Stroke Statistics-2023 Update: A Report from the American Heart Association. Circulation 2023, 147, e93–e621. [Google Scholar] [CrossRef]
- Martin, S.S.; Aday, A.W.; Almarzooq, Z.I.; Anderson, C.A.M.; Arora, P.; Avery, C.L.; Baker-Smith, C.M.; Barone Gibbs, B.; Beaton, A.Z.; Boehme, A.K.; et al. 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data from the American Heart Association. Circulation 2024. [Google Scholar] [CrossRef] [PubMed]
- Zghouzi, M.; Mwansa, H.; Shore, S.; Hyder, S.N.; Kamdar, N.; Moles, V.M.; Barnes, G.D.; Froehlich, J.; McLaughlin, V.V.; Paul, T.K.; et al. Sex, Racial, and Geographic Disparities in Pulmonary Embolism-related Mortality Nationwide. Ann. Am. Thorac. Soc. 2023, 20, 1571–1577. [Google Scholar] [CrossRef] [PubMed]
- Fu, X.; Zhong, Y.; Xu, W.; Ju, J.; Yu, M.; Ge, M.; Gu, X.; Chen, Q.; Sun, Y.; Huang, H.; et al. The prevalence and clinical features of pulmonary embolism in patients with AE-COPD: A meta-analysis and systematic review. PLoS ONE 2021, 16, e0256480. [Google Scholar] [CrossRef]
- Kearon, C.; Akl, E.A.; Ornelas, J.; Blaivas, A.; Jimenez, D.; Bounameaux, H.; Huisman, M.; King, C.S.; Morris, T.A.; Sood, N.; et al. Antithrombotic Therapy for VTE Disease: CHEST Guideline and Expert Panel Report. Chest 2016, 149, 315–352. [Google Scholar] [CrossRef] [PubMed]
- Zuin, M.; Rigatelli, G.; Zuliani, G.; Zonzin, P.; Ramesh, D.; Roncon, L. Thrombolysis in hemodynamically unstable patients: Still underused: A review based on multicenter prospective registries on acute pulmonary embolism. J. Thromb. Thrombolysis 2019, 48, 323–330. [Google Scholar] [CrossRef] [PubMed]
- Meyer, G.; Vicaut, E.; Danays, T.; Agnelli, G.; Becattini, C.; Beyer-Westendorf, J.; Bluhmki, E.; Bouvaist, H.; Brenner, B.; Couturaud, F.; et al. Fibrinolysis for Patients with Intermediate-Risk Pulmonary Embolism. N. Engl. J. Med. 2014, 370, 1402–1411. [Google Scholar] [CrossRef]
- Kerrigan, J.; Morse, M.; Haddad, E.; Willers, E.; Ramaiah, C. Advances in Percutaneous Management of Pulmonary Embolism. Int. J. Angiol. 2022, 31, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Giri, J.; Sista, A.K.; Weinberg, I.; Kearon, C.; Kumbhani, D.J.; Desai, N.D.; Piazza, G.; Gladwin, M.T.; Chatterjee, S.; Kobayashi, T.; et al. Interventional Therapies for Acute Pulmonary Embolism: Current Status and Principles for the Development of Novel Evidence: A Scientific Statement From the American Heart Association. Circulation 2019, 140, e774–e801. [Google Scholar] [CrossRef]
- Kucher, N.; Boekstegers, P.; Müller, O.J.; Kupatt, C.; Beyer-Westendorf, J.; Heitzer, T.; Tebbe, U.; Horstkotte, J.; Müller, R.; Blessing, E.; et al. Randomized, controlled trial of ultrasound-assisted catheter-directed thrombolysis for acute intermediate-risk pulmonary embolism. Circulation 2014, 129, 479–486. [Google Scholar] [CrossRef]
- Piazza, G.; Hohlfelder, B.; Jaff, M.R.; Ouriel, K.; Engelhardt, T.C.; Sterling, K.M.; Jones, N.J.; Gurley, J.C.; Bhatheja, R.; Kennedy, R.J.; et al. A Prospective, Single-Arm, Multicenter Trial of Ultrasound-Facilitated, Catheter-Directed, Low-Dose Fibrinolysis for Acute Massive and Submassive Pulmonary Embolism: The SEATTLE II Study. JACC Cardiovasc. Interv. 2015, 8, 1382–1392. [Google Scholar] [CrossRef]
- Porres-Aguilar, M.; Anaya-Ayala, J.E.; Heresi, G.A.; Rivera-Lebron, B.N. Pulmonary Embolism Response Teams: A Novel Approach for the Care of Complex Patients With Pulmonary Embolism. Clin. Appl. Thromb. Hemost. 2018, 24, 48s–55s. [Google Scholar] [CrossRef] [PubMed]
- HCUP Databases. Healthcare Cost and Utilization Project (HCUP). 2006–2019. Agency for Healthcare Research and Quality, Rockville, MD, USA. Available online: www.hcup-us.ahrq.gov/databases.jsp (accessed on 20 August 2023).
- Sedhom, R.; Elbadawi, A.; Megaly, M.; Jaber, W.A.; Cameron, S.J.; Weinberg, I.; Mamas, M.A.; Elgendy, I.Y. Hospital procedural volume and outcomes with catheter-directed intervention for pulmonary embolism: A nationwide analysis. Eur. Heart J. Acute Cardiovasc. Care 2022, 11, 684–692. [Google Scholar] [CrossRef] [PubMed]
- Elgendy, I.Y.; Mahmoud, A.N.; Mansoor, H.; Bavry, A.A. Early Invasive Versus Initial Conservative Strategies for Women with Non-ST-Elevation Acute Coronary Syndromes: A Nationwide Analysis. Am. J. Med. 2017, 130, 1059–1067. [Google Scholar] [CrossRef] [PubMed]
- Quan, H.; Sundararajan, V.; Halfon, P.; Fong, A.; Burnand, B.; Luthi, J.C.; Saunders, L.D.; Beck, C.A.; Feasby, T.E.; Ghali, W.A. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med. Care 2005, 43, 1130–1139. [Google Scholar] [CrossRef] [PubMed]
- Goldhaber, S.Z.; Markis, J.E.; Kessler, C.M.; Meyerovitz, M.F.; Kim, D.; Vauchan, D.E.; Selwyn, A.P.; Loscalzo, J.; Dawley, D.L.; Sharma, G.V.; et al. Perspectives on treatment of acute pulmonary embolism with tissue plasminogen activator. Semin. Thromb. Hemost. 1987, 13, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Goldhaber, S.Z.; Vaughan, D.E.; Markis, J.E.; Selwyn, A.P.; Meyerovitz, M.F.; Loscalzo, J.; Kim, D.S.; Kessler, C.M.; Dawley, D.L.; Sharma, G.V.; et al. Acute pulmonary embolism treated with tissue plasminogen activator. Lancet 1986, 2, 886–889. [Google Scholar] [CrossRef] [PubMed]
- Pal, S.; Gangu, K.; Garg, I.; Shuja, H.; Bobba, A.; Chourasia, P.; Shekhar, R.; Sheikh, A.B. Gender and Race-Based Health Disparities in COVID-19 Outcomes among Hospitalized Patients in the United States: A Retrospective Analysis of a National Sample. Vaccines 2022, 10, 2036. [Google Scholar] [CrossRef]
- Goldhaber, S.Z.; Meyerovitz, M.F.; Markis, J.E.; Kim, D.; Kessler, C.M.; Sharma, G.V.; Vaughan, D.E.; Selwyn, A.P.; Dawley, D.L.; Loscalzo, J.; et al. Thrombolytic therapy of acute pulmonary embolism: Current status and future potential. J. Am. Coll. Cardiol. 1987, 10, 96b–104b. [Google Scholar] [CrossRef]
- Daniels, L.B.; Parker, J.A.; Patel, S.R.; Grodstein, F.; Goldhaber, S.Z. Relation of duration of symptoms with response to thrombolytic therapy in pulmonary embolism. Am. J. Cardiol. 1997, 80, 184–188. [Google Scholar] [CrossRef]
- Keskin, M.; Dogan, S.; Kaya, A.; Tenekecioğlu, E.; Ocal, L.; Cersit, S.; Seker, M.; Yavuz, S.; Orhan, A.L. The prognostic value of time from symptom onset to thrombolysis in patients with pulmonary embolism. Int. J. Cardiol. 2022, 352, 131–136. [Google Scholar] [CrossRef]
- Klok, F.A.; Piazza, G.; Sharp, A.S.P.; Ainle, F.N.; Jaff, M.R.; Chauhan, N.; Patel, B.; Barco, S.; Goldhaber, S.Z.; Kucher, N.; et al. Ultrasound-facilitated, catheter-directed thrombolysis vs anticoagulation alone for acute intermediate-high-risk pulmonary embolism: Rationale and design of the HI-PEITHO study. Am. Heart J. 2022, 251, 43–53. [Google Scholar] [CrossRef]
- Edla, S.; Rosman, H.; Neupane, S.; Boshara, A.; Szpunar, S.; Daher, E.; Rodriguez, D.; LaLonde, T.; Yamasaki, H.; Mehta, R.H.; et al. Early Versus Delayed Use of Ultrasound-Assisted Catheter-Directed Thrombolysis in Patients With Acute Submassive Pulmonary Embolism. J. Invasive Cardiol. 2018, 30, 157–162. [Google Scholar] [PubMed]
- Voore, P.; Suarez, J.; Reddy, D.R.; Guntupalli, K. 167: Optimal timing of catheter-directed thrombolysis in treatment of submassive pulmonary embolism. Crit. Care Med. 2018, 46, 66. [Google Scholar] [CrossRef]
- Alhuarrat, M.A.D.; Barssoum, K.; Helft, M.; Singh, P.; Grushko, M.; Faillace, R.; Sokol, S.I. C-35|Predictors of Early vs Late Catheter Directed Embolectomy Intervention for Pulmonary Embolism. J. Soc. Cardiovasc. Angiogr. Interv. 2023, 2, 100823. [Google Scholar] [CrossRef]
- Alhuarrat, M.A.D.; Pargaonkar, S.; Rahgozar, K.; Safiriyu, I.; Zhang, X.; Faillace, R.T.; Di Biase, L. Comparison of in-hospital outcomes and complications of left atrial appendage closure with the Watchman device between males and females. Europace 2023, 25, euad228. [Google Scholar] [CrossRef] [PubMed]
- Mohamed, M.O.; Volgman, A.S.; Contractor, T.; Sharma, P.S.; Kwok, C.S.; Rashid, M.; Martin, G.P.; Barker, D.; Patwala, A.; Mamas, M.A. Trends of Sex Differences in Outcomes of Cardiac Electronic Device Implantations in the United States. Can. J. Cardiol. 2020, 36, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Amgai, B.; Chakraborty, S.; Bandyopadhyay, D.; Gupta, M.; Patel, N.; Hajra, A.; Dey, A.K.; Koirala, S.; Ghosh, R.K.; Aronow, W.S.; et al. Sex Differences in In-Hospital Outcomes of Transcatheter Aortic Valve Replacement. Curr. Probl. Cardiol. 2021, 46, 100694. [Google Scholar] [CrossRef] [PubMed]
- Weze, K.O.; Obisesan, O.H.; Dardari, Z.A.; Cainzos-Achirica, M.; Dzaye, O.; Graham, G.; Miedema, M.D.; Yeboah, J.; DeFilippis, A.P.; Nasir, K.; et al. The Interplay of Race/Ethnicity and Obesity on the Incidence of Venous Thromboembolism. Am. J. Prev. Med. 2022, 63, e11–e20. [Google Scholar] [CrossRef]
- Martin, K.A.; McCabe, M.E.; Feinglass, J.; Khan, S.S. Racial Disparities Exist Across Age Groups in Illinois for Pulmonary Embolism Hospitalizations. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 2338–2340. [Google Scholar] [CrossRef]
- Phillips, A.R.; Reitz, K.M.; Myers, S.; Thoma, F.; Andraska, E.A.; Jano, A.; Sridharan, N.; Smith, R.E.; Mulukutla, S.R.; Chaer, R. Association Between Black Race, Clinical Severity, and Management of Acute Pulmonary Embolism: A Retrospective Cohort Study. J. Am. Heart Assoc. 2021, 10, e021818. [Google Scholar] [CrossRef] [PubMed]
- Dronamraju, V.H.; Lio, K.U.; Badlani, R.; Cheng, K.; Rali, P. PERT era, race-based healthcare disparities in a large urban safety net hospital. Pulm. Circ. 2023, 13, e12318. [Google Scholar] [CrossRef] [PubMed]
- Snyder, D.J.; Zilinyi, R.S.; Madhavan, M.V.; Alsaloum, M.; Saleem, D.; Buyske, J.J.; Healy, E.W.; McGredy, M.J.; Da Silva, B.T.; Rosenzweig, E.B.; et al. Association between Hispanic or Latino ethnicity and pulmonary embolism severity, management, and in-hospital outcomes. Vasc. Med. 2023, 28, 222–232. [Google Scholar] [CrossRef] [PubMed]

| Variable | Overall | Before Propensity Matching | After Propensity Matching | Standardized Mean Difference | |||||
|---|---|---|---|---|---|---|---|---|---|
| Catheter-Directed Thrombolysis | p Value | Catheter-Directed Thrombolysis | p Value | ||||||
| <48 h | >48 h | <48 h | >48 h | ||||||
| Population | 19,525 | 16,480 (84%) | 3045 (16%) | 2970 (50%) | 2970 (50%) | ||||
| Age | 60.7 ± 14.6 | 60.4 ± 14.5 | 62.5 ± 14.7 | <0.001 | 63.0 ± 14.0 | 62.6 ± 14.6 | 0.265 | −0.029 | |
| Gender | Male | 10,180 (52%) | 8690 (53%) | 1490 (49%) | <0.001 | 1405 (47%) | 1465 (49%) | 0.119 | −0.040 |
| Female | 9335 (48%) | 7790 (47%) | 1545 (51%) | 1565 (53%) | 1505 (51%) | ||||
| Race | White | 13,675 (72%) | 11,640 (72%) | 2035 (68%) | <0.001 | 2045 (69%) | 2030 (68%) | 0.548 | 0.020 |
| Black | 3795 (20%) | 3155 (20%) | 640 (21%) | 645 (22%) | 635 (21%) | ||||
| Others | 1590 (8%) | 1285 (8%) | 305 (10%) | 280 (9%) | 305 (10%) | ||||
| Hospital location and teaching status | Rural | 815 (4%) | 670 (4%) | 145 (5%) | 0.001 | 145 (5%) | 140 (5%) | <0.001 | −0.082 |
| Urban non-teaching | 4050 (21%) | 3355 (20%) | 695 (23%) | 545 (18%) | 690 (23%) | ||||
| Urban teaching | 14,660 (75%) | 12,455 (76%) | 2205 (72%) | 2280 (77%) | 2140 (72%) | ||||
| Hospital bed size | Small | 2970 (15%) | 2605 (16%) | 365 (12%) | <0.001 | 360 (12%) | 360 (12%) | 0.694 | −0.014 |
| Medium | 6215 (32%) | 5190 (31%) | 1025 (34%) | 980 (33%) | 1010 (34%) | ||||
| Large | 10,340 (53%) | 8685 (53%) | 1655 (54%) | 1630 (55%) | 1600 (54%) | ||||
| Charlson index | No comorbidities | 7005 (36%) | 6225 (38%) | 780 (26%) | <0.001 | 725 (24%) | 770 (26%) | 0.395 | −0.030 |
| Low | 8655 (44%) | 7175 (44%) | 1480 (49%) | 1490 (50%) | 1455 (49%) | ||||
| Moderate | 2345 (12%) | 1885 (11%) | 460 (15%) | 410 (14%) | 425 (14%) | ||||
| High | 1520 (8%) | 1195 (7%) | 325 (11%) | 345 (12%) | 320 (11%) | ||||
| Comorbidities | Diabetes | 5240 (27%) | 4345 (26%) | 895 (29%) | 0.001 | 880 (30%) | 860 (29%) | 0.569 | −0.015 |
| Chronic ischemic heart disease | 2510 (13%) | 2050 (12%) | 460 (15%) | <0.001 | 385 (13%) | 445 (15%) | 0.025 | 0.058 | |
| Peripheral vascular disease | 740 (4%) | 550 (3%) | 190 (6%) | <0.001 | 165 (6%) | 185 (6%) | 0.490 | 0.029 | |
| COPD | 3825 (20%) | 3075 (19%) | 750 (25%) | <0.001 | 775 (26%) | 745 (25%) | 0.372 | −0.023 | |
| HTN | 12,565 (64%) | 10,520 (64%) | 2045 (67%) | <0.001 | 1990 (67%) | 2010 (68%) | 0.580 | 0.014 | |
| Obesity | 7925 (41%) | 6660 (40%) | 1265 (42%) | 0.243 | 1280 (43%) | 1220 (41%) | 0.115 | −0.041 | |
| Renal failure | 2175 (11%) | 1715 (10%) | 460 (15%) | <0.001 | 405 (14%) | 435 (15%) | 0.264 | 0.029 | |
| Heart failure | 3120 (16%) | 2510 (15%) | 610 (20%) | <0.001 | 640 (22%) | 595 (20%) | 0.150 | −0.037 | |
| Smoking (current/former) | 6920 (35%) | 5765 (35%) | 1155 (38%) | 0.002 | 1035 (35%) | 1120 (38%) | 0.022 | 0.060 | |
| Hyperlipidemia | 7345 (38%) | 6095 (37%) | 1250 (41%) | <0.001 | 1230 (41%) | 1230 (41%) | 1.0 | 0 | |
| Primary Outcome | Overall (%) | Catheter-Directed Thrombolysis | Multivariate Regression Pre-Match (OR [CI]) | p Value | Multivariate Regression Post-Match (OR [CI]) | p Value | ||
|---|---|---|---|---|---|---|---|---|
| <48 h (%) | >48 h (%) | |||||||
| Mortality | 3.35 | 3.37 | 3.28 | 0.88 [0.71–1.10] | 0.269 | 0.83 [0.63–1.10] | 0.190 | |
| Vasopressor use | 1.20 | 1.21 | 1.15 | 0.85 [0.59–1.23] | 0.380 | 0.88 [0.55–1.41] | 0.598 | |
| ECMO use | 0.28 | 0.21 | 0.66 | 3.63 [1.96–6.73] | <0.001 | 9.03 [2.35–34.69] | 0.001 | |
| Need for blood transfusion | 3.15 | 2.76 | 5.25 | 1.73 [1.43–2.09] | <0.001 | 1.84 [1.41–2.40] | <0.001 | |
| Need for systemic thrombolysis | 2.18 | 1.88 | 3.78 | 1.96 [1.57–2.45] | <0.001 | 3.21 [2.18–4.74] | <0.001 | |
| Acute kidney injury | 19.1 | 17.7 | 26.8 | 1.57 [1.42–1.73] | <0.001 | 1.42 [1.25–1.61] | <0.001 | |
| Intracranial hemorrhage | 0.46 | 0.46 | 0.49 | 0.97 [0.55–1.72] | 0.930 | 2.14 [0.91–5.06] | 0.081 | |
| Cardiac arrest | 2.48 | 2.52 | 2.30 | 0.83 [0.64–1.08] | 0.167 | 0.81 [0.59–1.13] | 0.213 | |
| Cardiogenic shock | 3.69 | 3.76 | 3.28 | 0.79 [0.64–0.99] | 0.040 | 1.23 [0.91–1.66] | 0.176 | |
| Mechanical ventilation | Overall need | 4.79 | 4.67 | 5.42 | 1.07 [0.89–1.27] | 0.469 | 1.33 [1.05–1.70] | 0.020 |
| For <24 h | 2.0 | 2.12 | 1.31 | 0.61 [0.42–0.87] | 0.006 | 0.66 [0.42–1.02] | 0.060 | |
| For 24–96 h | 2.30 | 2.28 | 2.46 | 1.05 [0.80–1.38] | 0.728 | 1.73 [1.16–2.59] | 0.007 | |
| For >96 h | 1.25 | 1.0 | 2.63 | 2.87 [2.06–4.0] | <0.001 | 4.65 [2.59–8.34] | <0.001 | |
| Facility discharge | 13.6 | 12.6 | 18.9 | 1.35 [1.20–1.51] | <0.001 | 1.32 [1.14–1.53] | <0.001 | |
| Multivariate Regression * (Linear: Beta [CI]) | p Value | Days to CDT | |
|---|---|---|---|
 | |||
| Mortality | −0.09 [−0.19–0.01] | 0.08 | 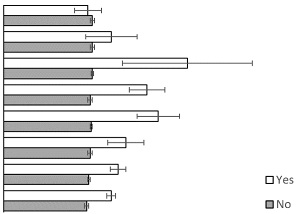 |
| Vasopressor use | 0.11 [−0.04–0.27] | 0.16 | |
| ECMO use | 0.95 [0.6–1.3] | <0.01 | |
| Blood transfusion | 0.43 [0.33–0.53] | <0.01 | |
| Systemic thrombolysis | 0.58 [0.46–0.7] | <0.01 | |
| Intubations | 0.28 [0.2–0.37] | <0.01 | |
| Facility discharges | 0.19 [0.14–0.25] | <0.01 | |
| Weekend admission | 0.25 [0.21–0.29] | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alhuarrat, M.A.D.; Barssoum, K.; Chowdhury, M.; Mathai, S.V.; Helft, M.; Grushko, M.; Singh, P.; Jneid, H.; Motiwala, A.; Faillace, R.T.; et al. Comparison of In-Hospital Outcomes between Early and Late Catheter-Directed Thrombolysis in Acute Pulmonary Embolism: A Retrospective Observational Study. J. Clin. Med. 2024, 13, 1093. https://doi.org/10.3390/jcm13041093
Alhuarrat MAD, Barssoum K, Chowdhury M, Mathai SV, Helft M, Grushko M, Singh P, Jneid H, Motiwala A, Faillace RT, et al. Comparison of In-Hospital Outcomes between Early and Late Catheter-Directed Thrombolysis in Acute Pulmonary Embolism: A Retrospective Observational Study. Journal of Clinical Medicine. 2024; 13(4):1093. https://doi.org/10.3390/jcm13041093
Chicago/Turabian StyleAlhuarrat, Majd Al Deen, Kirolos Barssoum, Medhat Chowdhury, Sheetal Vasundara Mathai, Miriam Helft, Michael Grushko, Prabhjot Singh, Hani Jneid, Afaq Motiwala, Robert T. Faillace, and et al. 2024. "Comparison of In-Hospital Outcomes between Early and Late Catheter-Directed Thrombolysis in Acute Pulmonary Embolism: A Retrospective Observational Study" Journal of Clinical Medicine 13, no. 4: 1093. https://doi.org/10.3390/jcm13041093
APA StyleAlhuarrat, M. A. D., Barssoum, K., Chowdhury, M., Mathai, S. V., Helft, M., Grushko, M., Singh, P., Jneid, H., Motiwala, A., Faillace, R. T., & Sokol, S. I. (2024). Comparison of In-Hospital Outcomes between Early and Late Catheter-Directed Thrombolysis in Acute Pulmonary Embolism: A Retrospective Observational Study. Journal of Clinical Medicine, 13(4), 1093. https://doi.org/10.3390/jcm13041093





