Epidural Spinal Cord Stimulation for Spinal Cord Injury in Humans: A Systematic Review
Abstract
1. Introduction
2. Epidural Spinal Cord Stimulation
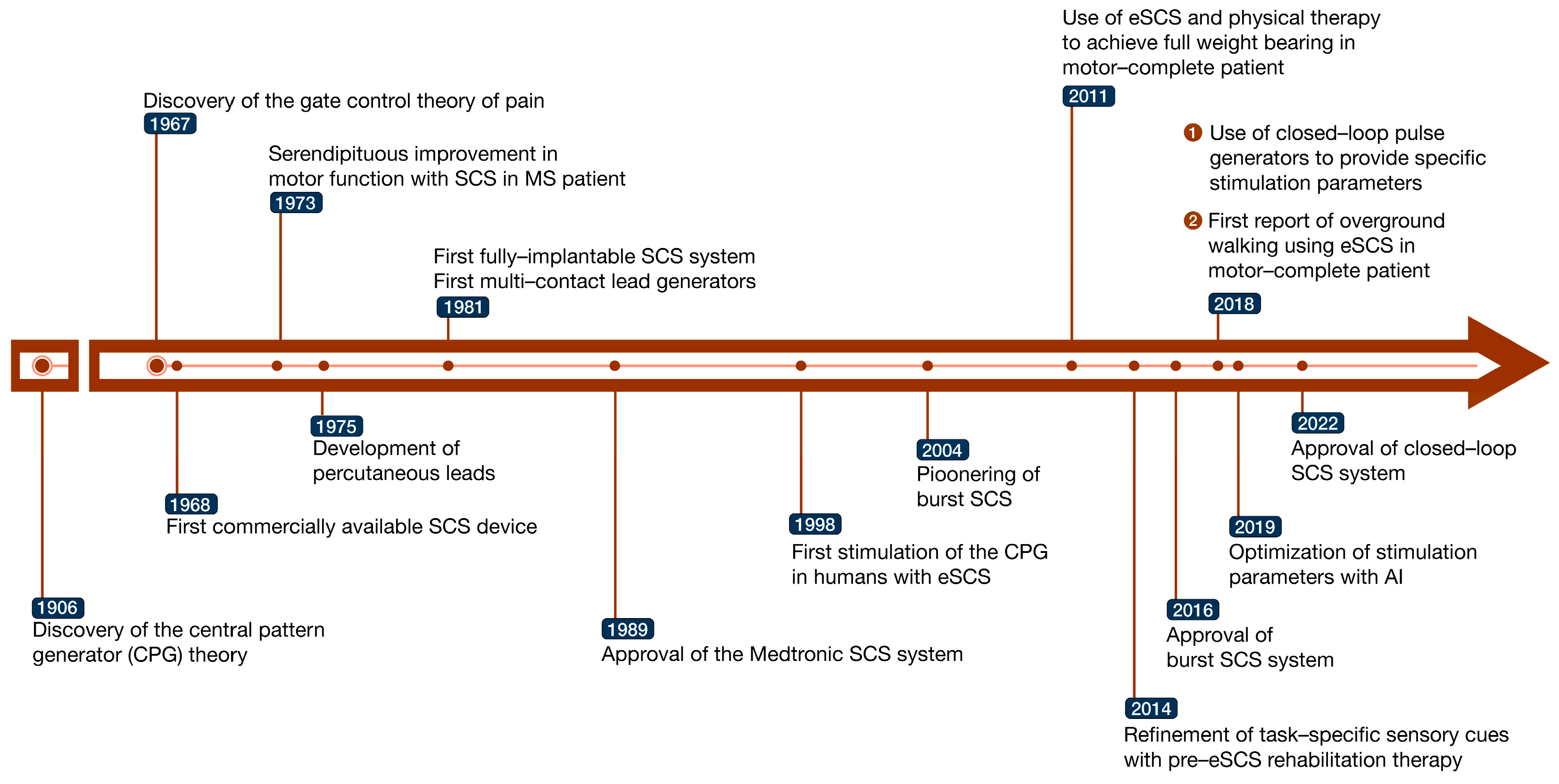
2.1. History and Evolution of eSCS
2.2. eSCS Implantation Approaches
2.3. Mechanisms of eSCS in Locomotor Control
2.3.1. Spinal Networks and Reflex Pathways
2.3.2. Sensory and Proprioceptive Inputs
2.3.3. Central Pattern Generators (CPGs)
2.4. Mechanisms of eSCS in Autonomic Control
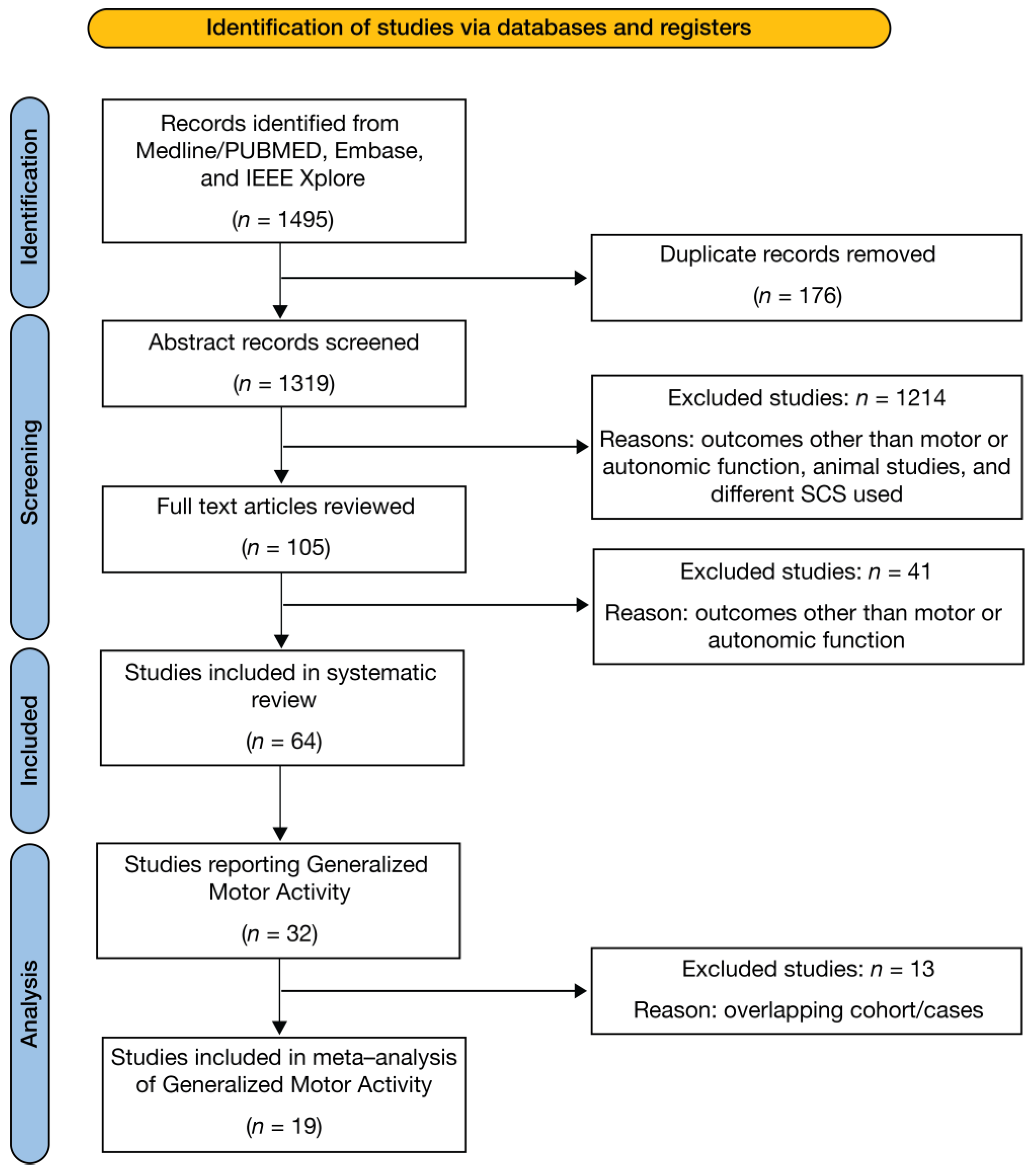
3. Methods
3.1. Search Strategy
3.2. Study Selection Criteria
3.3. Data Extraction
3.4. Analysis of Locomotor Outcomes
3.5. Bias Assessment
4. Results
4.1. Study Selection
4.2. Study and Participant Characteristics
4.3. Stimulator Parameters, Optimization, and Physical Rehabilitation
4.4. Outcomes Measured
4.5. Methodological Quality
4.6. Adverse Effects
5. Discussion
5.1. Efficacy of eSCS in Improving Locomotor Function
5.2. Efficacy of eSCS in Improving Autonomic Function
5.3. Efficacy of eSCS in Improving Combined Locomotor and Autonomic Function: AIS Scores
5.4. Safety of eSCS in SCI
| Author (Year) | Country | Subjects (Sex) | Age Range | Injury Level | Years Since Injury | ASIA Score | |
|---|---|---|---|---|---|---|---|
| 1 | Barolat (1986) [107] | USA | 1 (M) | 22 | C5 | 0.75 | C |
| 2 | Katz (1991) [119] | USA | 33 (31M, 2F) | 24–66 | C4–C10 | 0.58–31.5 | A–D |
| 3 | Dimitrijevic (1998) [30] | Austria | 6 (3M, 3F) | 18–58 | C5–T8 | 1–5 | A |
| 4 | Herman (2002) [32] | USA | 1 (M) | 43 | C5–C6 | 3.5 | C |
| 5 | Cahart (2004) [31] | USA | 1 (M) | 43 | C5–C6 | 3.5 | C |
| 6 | Jilge (2004) [134] | Austria | 5 (2M, 3F) | 24–34 | C4–T10 | 2–8 | 4A, 1B |
| 7 | Minassian (2004) [34] | Austria | 10 (7M, 3F) | 18–58 | C4–T10 | 2–8 | 8A, 2B |
| 8 | Ganley (2005) [135] | USA | 2 (M) | 43–48 | C6–T8 | 3.5–8 | C |
| 9 | DiMarco (2006) [99] | USA | 1 (M) | 52 | C5–C6 | 7 | C |
| 10 | Huang (2006) [33] | USA | 2 (M) | 43–48 | C5–T8 | 3.5–8 | C |
| 11 | Minassian (2007) [136] | Austria | 15 | – | – | – | A |
| 12 | DiMarco (2009) [100] | USA | 9 (8M, 1F) | 23–52 | C3–C6 | 1–34 | – |
| 13 | Harkema (2011) [22] | USA | 1 (M) | 23 | C7–T1 | 3.4 | B |
| 14 | Monshonkina (2012) [116] | Russia | 4 (1M, 3F) | 22–58 | C5–L1 | – | 2 A/B, 1B, 1 B/C |
| 15 | Minassian (2013) [118] | Austria | 7 | – | – | – | – |
| 16 | Angeli (2014) [35] | USA | 4 (M) | 23–32 | C6–T6 | 2.2–4.2 | 2A, 2B |
| 17 | Sayenko (2014) [62] | USA | 3 (M) | 23–32 | C7–T4 | 2.2–4.2 | 1A, 2B |
| 18 | Danner (2015) [137] | Austria | 10 (7M, 3F) | 18–58 | C4–T10 | 2–8 | 6A, 4B |
| 19 | Hoefstoetter (2015) [138] | Austria | 8 (6M, 2F) | 18–33 | C5–T6 | 1–13 | 6A, 2B |
| 20 | Rejc (2015) [36] | USA | 4 (M) | 24–33 | C7–T4 | 2.2–4.2 | 2A, 2B |
| 21 | Lu (2016) [117] | USA | 2 (M) | 18–20 | C5–C6 | 2–2.5 | B |
| 22 | Grahn (2017) [139] | USA | 1 (M) | 26 | T6 | 3 | A |
| 23 | Rejc (2017) A [37] | USA | 1 (M) | 32 | C7 | 4.2 | B |
| 24 | Rejc (2017) B [38] | USA | 4 (M) | 24–33 | C7–T4 | 2.2–4.2 | 2A, 2B |
| 25 | Angeli (2018) [39] | USA | 4 (3M, 1F) | 22–32 | C5–T4 | 2.5–3.3 | 2A, 2B |
| 26 | Aslan (2018) [140] | USA | 7 (M) | – | C5–T4 | 2.0–3.5 | 4A, 3B |
| 27 | DiMarco (2018) [101] | USA | 1 (M) | 50 | C4 | 2 | – |
| 28 | Formento (2018) [40] | Switzerland | 3 (M) | 28–47 | C4–C7 | 4–6 | 2C, 1D |
| 29 | Gill (2018) [41] | USA | 1 (M) | 26 | T6 | 3 | A |
| 30 | Harkema (2018) A [78] | USA | 4 (3M, 1F) | 24–35 | C4 | 3.8–8 | 3A, 1B |
| 31 | Harkema (2018) B [131] | USA | 4 (3M, 1F) | 24–35 | C4 | 3.8–8 | 3A, 1B |
| 32 | Herrity (2018) [129] | USA | 1 (M) | (31) | C5 | –3.3 | B |
| 33 | Wagner (2018) [42] | Switzerland | 3 (M) | 28–47 | C4–C8 | 4–6 | 2C, 1D |
| 34 | Walter (2018) [125] | Canada | 1 (M) | 32 | C5 | 4 | B |
| 35 | West (2018) [78] | Canada | 1 (M) | Early 30s | C5 | – | B |
| 36 | Calvert (2019) [43] | USA | 2 (M) | 26–37 | T3–T6 | 3–6 | A |
| Author (Year) | Stimulator Type | Lead Placement | No. of Leads | Lead Levels | Stimulation Parameters | Stimulation Optimization | Rehabilitation | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Frequency | Pulse Width (μs) | Amplitude | Pre–Op | Post–Op | |||||||
| 1 | Barolat (1986) [107] | Clinical Technology Corporation | PC | 1 | T1–T2 | 75 Hz | 250 | – | Stimulation parameters optimised for paraesthesia. Frequencies of 30–100 Hz were tested | No | No |
| 2 | Katz (1991) [119] | Medtronic | Paddle | 4 | – | – | – | – | Parameters optimized for spasticity | No | No |
| 3 | Dimitrijevic (1998) [30] | Medtronic | – | T11–L1 | 25–50 Hz | 200–500 | 5–9 V | Muscle twitches were tested using 3 cathode leads, followed by testing frequencies of 1–120 Hz and amplitude 1–10 V | No | No | |
| 4 | Herman (2002) [32] | Medtronic | PC | 4 | LS enlarge–ment | – | – | – | A variety of electrical parameters were tested for efficacy in promoting gait | ||
| 5 | Cahart (2004) [31] | Medtronic | PC | 4 | T10–T12 | 40–60 Hz | 800 | Midpoint between sensory and motor thresholds | A wide range of parameters were tested, with selection of pulse widths > 500 μs and frequencies of 40–60 Hz | Yes | Yes |
| 6 | Jilge (2004) [134] | Medtronic | PC | 4 | T12–L1 | 5–60 Hz | 210–450 | 1–10 V | Muscle twitches were elicited using a single electrode, with the stimulation amplitude being increased to the point of eliciting brief muscle contractions | No | No |
| 7 | Minassian (2004) [34] | Medtronic | PC | 4 | T10–L1 | 2.2–50 Hz | – | 1–10 V | Optimized for spasticity by applying strengths of 1–10 V at frequencies 2.2–100 Hz using different contact combinations of electrodes | No | No |
| 8 | Ganley (2005) [135] | – | PC | 4 | T10–T12 | 20–60 Hz | 800 | Between sensory and motor thresholds in S1 and at motor threshold in S2 | Parameters adjusted on an individual basis | Yes | No |
| 9 | DiMarco (2006) [109] | Neuro–Control Corp | PC | 1 | T9, T11, L1 | 53 Hz | 150 –200 μs | 40 V | Pulse width of 150 μs at T9, and 200 μs at T11 and L1. | No | No |
| 10 | Huang (2006) [33] | Medtronic | PC | 4 | T10–L2 | 20–40 Hz | 800 | 3–8.5 V | Stimulation intensity was set between sensory threshold and motor threshold but closer to motor threshold, during gait training sessions | ||
| 11 | Minassian (2007) [136] | Medtronic | PC | 4 | T10–L1 | 2.2–50 Hz | 210 | 1–10 V | – | No | No |
| 12 | DiMarco (2009) [100] | Neuro–Control Corp | PC | 1 | T9, T11, L1 | 30–40 Hz | 150–200 | 30–40 V | – | No | No |
| 13 | Harkema (2011) [22] | Medtronic | Paddle | 16 | L1–S1 | 5–40 Hz | 210 or 450 | 0.5–10 V | Variable combinations were tested to optimize standing and stepping. 15 Hz, 8V of the caudal level (L5–S1) was used for standing caudal; 30–40 Hz and sensory cues for manually facilitated stepping | Yes | Yes |
| 14 | Monshonkina (2012) [116] | Cooner Wire Co. | PC | 2–4 | L2–L4, S2 | 1–12 Hz | – | – | Therapeutic mono/bipolar (stimulation frequency of 1–12 Hz) 2 times for 30 min in addition to routine pharmacotherapy | Yes | No |
| 15 | Minassian (2013) [118] | Medtronic | PC | 4 | Lumbar spinal cord | 2–42 Hz | – | – | – | No | No |
| 16 | Angeli (2014) [35] | Medtronic | Paddle | 16 | L1–S1 | 25–30 | – | – | Stimulation parameters optimized for each leg and joint movement, with optimal frequency set at either 25 or 30 Hz | Yes | Yes |
| 17 | Sayenko (2014) [62] | Medtronic | Paddle | 16 | L1–S2 | 2 Hz | 210 | 0.5–10 V | Bilateral-evoked potentials from leg muscles were collected and evaluated by spatial, temporal, and amplitude characteristics to optimize location and symmetry of electrode placement | No | No |
| 18 | Danner (2015) [137] | Medtronic | PC | 4 | T11–L1 | 2–130 Hz | 210 | 0–10.5 V | – | No | No |
| 19 | Hoefstoetter (2015) [138] | Medtronic | PC | 4 | T11–L1 | 2–130 Hz | 210 | 0–10.5 V | – | No | No |
| 20 | Rejc (2015) [36] | Medtronic | Paddle | 16 | L1–S1 | 25–60 Hz | – | 1.0–9.0 V | For standing, a sub–motor threshold of 25 Hz was used followed by adjustments to activate specific motor neuron pools | Yes | Yes |
| 21 | Lu (2016) [117] | Boston Scientific | Paddle | 16 | C4/C5–T1 | 2–40 Hz | 210 | 0.1–10.0 mA | Different bipolar electrode configurations were tested to identify electrode pairs with greatest hand motor responses | No | Yes |
| 22 | Grahn (2017) [139] | Medtronic | Paddle | 16 | Lumbar enlarge–ment | 15–40 Hz | 210 | 0–6 | Tested wide–field vs. local–field electrode configurations using a pre–selected algorithm. Frequencies used were 25 and 40 Hz (for volitional control and stepping) and 15 Hz (for standing) | Yes | Yes |
| 23 | Rejc (2017) A [37] | Medtronic | Paddle | 16 | L1–S1 | 30–65 Hz | – | 0.4–3.5 V | The following electrode configurations were used for the following activities: (1) standing: combination of 40–60 Hz and 0.6–1V at T1–T2 and T3–T8; (2) stepping: 30–55 Hz and 0.7–3.5 V at T2–T3, T5–T6 and T7–T9; and (3) voluntary movement: 30–65 Hz and 0.4–2.2 V at T1–T3 | Yes | Yes |
| 24 | Rejc (2017) B [38] | Medtronic | Paddle | 16 | L1–S1 | 15–60 Hz | – | 1.2–10 V | Parameters were optimized to generate continuous EMG patterns for standing after stand training. | Yes | Yes |
| 25 | Angeli (2018) [39] | Medtronic | Paddle | 16 | L1–S1/S2 | 5–50 | – | 1–10 V | Simulation parameters were optimized for each individual to achieve the best motor performance task. Both standing and stepping configurations were modified every 2–4 weeks | Yes | Yes |
| 26 | Aslan (2018) [140] | Medtronic | Paddle | 16 | T11–L1 | 2–35 | – | 0–10 V | Unique electrode configurations for each subject were used. For EMG and cardiovascular response to rostral and caudal configuration of the electrode, a constant frequency of 2 Hz was used while amplitude increased from 0–10 V | No | No |
| 27 | DiMarco (2018) [101] | – | PC | 2 | T9–T11 | 50 | 200 | 40 V | – | No | No |
| 28 | Formento (2018) [40] | Medtronic | Paddle | 16 | Lumbo–sacral | 40 | – | 3–9 mA | Different frequencies and amplitudes were tested in random order to characterise the ability of eSCS to modulate motor output | No | No |
| 29 | Gill (2018) [41] | Medtronic | Paddle | 16 | T11–L1 | 20–25 | 210 | 3.3–6 V | Initial frequency based on prior literature. Subsequently, parameters and configurations were modified to enable voluntary control | Yes | Yes |
| 30 | Harkema (2018) A [77] | Medtronic | Paddle | 16 | T11–L1 | – | 450 | – | Configurations were optimized to maintain a target SBP of 110–120 mmHg or 105–115 mmHg and then adjusted as needed | No | No |
| 31 | Harkema (2018) B [131] | Medtronic | Paddle | 16 | T11–L1 | – | 450 | – | Configurations were optimized to maintain a target SBP of 110–120 mmHg or 105–115 mmHg and then adjusted as needed | No | No |
| 32 | Herrity (2018) [129] | Medtronic | Paddle | 16 | L1–S1 | 5–30 | 450 | Increased in steps of 0.1 V | Stimulation parameters were initiated using a global configuration that satisfied 4 rules, including the use of a fixed frequency (from 5 Hz) and pulse width (450 μs), with voltage ramped up slowly (0.1 V increments | Yes | Yes |
| 33 | Wagner (2018) [42] | Medtronic | Paddle | 16 | T11–L1 | 20–129 | – | 0.6–8 mA | Configurations were tested as monopolar pulses in EMG with selected configurations further tested for joint torque production. | No | Yes |
| 34 | Walter (2018) [125] | Medtronic | Paddle | 16 | T11–L1 | 25–45 | 300–450 | 4–7 V | The frequency and pulse width were pre–set, but the participant can use the stimulator as needed | No | No |
| 35 | West (2018) [78] | Medtronic | Paddle | 16 | T11–L1 | 35 | 300 | 3.5 V | A series of tests was conducted over 2 weeks to determine optimum stimulation parameters to increase blood pressure | No | No |
| 36 | Calvert (2019) [43] | Medtronic | Paddle | 16 | T11–L1 | 40 | 210 | 0–10 V | Electrode configurations from previous literature were used to assess volitional activity | Yes | No |
| 37 | Cheng (2019) [44] | Medtronic | Paddle | 16 | L1–S1 | 25 | 200 | – | The choice of stimulating electrodes was modified using a machine learning algorithm to search for optimal stimulation patterns | Yes | No |
| 38 | Darrow (2019) [45] | Abbott | Paddle | 16 | L2–S2 | 16–400 | 200–500 | 2–15 mA | Tested eSCS settings at each visit were chosen as the best by the participant’s experience over each month from an objectively determined setting list provided by a Bayesian optimization | No | No |
| 39 | Nightingale (2019) [130] | Medtronic | Paddle | 16 | T11–L1 | 35–40 | 300–420 | 3.5–6.0 V | Abdominal settings: 40 Hz, 420 μs, 3.5–6.0 V; Cardiorespiratory settings: 35 Hz, 300 μs, 3.5–6.0 V; | No | No |
| 40 | Terson de Paleville (2019) [122] | Medtronic | Paddle | 16 | L1–S1 | 10–45 | – | – | Stimulation configurations were specific for each individual, with specific configurations selected to enable the specific motor task. Standing configuration ranged from 10–40 Hz, and stepping 25–45 Hz | Yes | Yes |
| 41 | DiMarco (2020) [102] | – | PC | 2 | T9–T11 | 50 | 200 | 30–40 V | Stimulus parameters were set based on previous studies, which resulted in near maximal positive airway pressure generation | No | No |
| 42 | Gorgey (2020) [46] | Medtronic | Paddle | 16 | T12–S2 | 40 | 420 | 6–7 V | Parameters were modified based on patient performance | No | Yes |
| 43 | Penã Pino (2020) [47] | Abbott | Paddle | 16 | L2–S2 | – | – | – | Participants were provided with a programmer and allowed to adjust specific stimulation settings for specific tasks such as volitional movements, spasticity control, core strength, and autonomic functions | No | No |
| 44 | Beck (2021) [120] | Medtronic | Paddle | 16 | T12–L1 | – | – | – | An optimization period of 3 weeks was used to determine task–specific parameters, which were adjusted throughout a 12–month period | Yes | Yes |
| 45 | Calvert (2021) [48] | Medtronic | Paddle | 16 | T11–L1 | 0.2–2 | 210 | 0–10 V | Electrode configurations were defined empirically based on the motor output of each patient that enabled specific motor activation | Yes | Yes |
| 46 | DiMarco (2021) [123] | Ardiem Medical | PC | 2 | T9–T11 | 50 | 200 | 20–30 V | Each subject self–selected the number of stimulations and voltages applied. Typically, 2–3 applications of SCS (20–30 V, 50 Hz, 0.2 pulse width) were applied every 2–7 min and repeated several times | No | No |
| 47 | Gill (2021) [141] | Medtronic | Paddle | 16 | 20–30 | 200–450 | 2.0–4.1 V | Stimulation parameters were adjusted incrementally during initial sessions of stimulation–enabled task–specific training, and refined during BWST training sessions | Yes | Yes | |
| 48 | Herrity (2021) [121] | Medtronic | Paddle | 16 | L1–S1 | – | – | – | – | No | Yes |
| 49 | Ibánēz (2021) [49] | Medtronic | Paddle | 16 | T11–L1 | 10–40 | 450–1000 | 1.8–8.6 mA; 8 V | Parameters were optimized based on individualized maps of motor pools activation, previous evidence of lower limb extension pattern generation, and topographical organization of the activation pattern | No | No |
| 50 | Linde (2021) [50] | Medtronic | Paddle | 16 | Lumbo-sacral | – | – | – | Stimulation parameters optimized for movement were determined by participants | Yes | Yes |
| 51 | Mesbah (2021) [51] | Medtronic | Paddle | 16 | T12–L2 | 2 or 30 | 450 or 1000 | Increased from 0.1 V–0.5 V with 0.1 V | Stimulation parameters were further optimized for individual joint movement | No | No |
| 52 | Squair (2021) [98] | Medtronic | Paddle | 16 | T10–L1 | 120 | 450 | 0–7.5 mV | Parameters were optimized to recruit lower spinal segments and to increased blood pressure | No | No |
| 53 | Gorgey (2022) [52] | Medtronic | PC | 8 | T11–T12 | 2–40 | 150–210 | 0–10 V | Stimulation parameters were initially set at 2 Hz, 150 μs and 0–10 V. They were subsequently optimized to 20–30 Hz and 210 μs to ensure target achievements of functional movements in the supine position | No | No |
| 54 | Herrity (2022) [142] | Medtronic | Paddle | 16 | L1–S1 | 15–90 | 300–1000 | 0–12 mA | Bladder storage and voiding parameters were optimization tested and refined to build cohorts for multisystem stimulation. Parameters were: (1) bladder compliance: 60 Hz, 0–5 mA, 450 μs; and (2) voiding: 30 Hz, 4 mA, 1000 μs | No | No |
| 55 | Kandhari (2022) A [114] | Medtronic | PC | 8 | T1–T5 | 40 | 210 | 0–3.5 V | Different stimulation settings were tested over a period of 2 weeks | No | No |
| 56 | Kandhari (2022) B [143] | Medtronic | Paddle | 16 | T11–L1 | 15–60 | 210–400 | 1–6 V | A self–training program was implemented with sub–threshold stimulation levels at 60 Hz, 1–1.5 V and 270 μs to maintain the excitability of spinal neural networks | Yes | Yes |
| 57 | Rowald (2022) [53] | Medtronic | Paddle | 16 | T12–S2 | 20 or 100 | 500 | 0.5 V | Stimulation parameters were optimized based on responses elicited by eSCS, which where then optimized for each participant. These parameters were further fine–tuned through a stimulation scheduler software. | No | Yes |
| 58 | Smith (2022) [115] | Medtronic | Paddle | 16 | Lumbo-sacral | – | – | – | Individualized maps of motor pools activation were generated followed by selection of stimulation parameters based on guidelines | No | No |
| 59 | Boakye (2023) [108] | Medtronic | Paddle | 16 | T11–L1 | 2 | 450 | Increased from 0.1–0.5 V with 0.1 V | Initial testing of rostral and caudal electrode configurations was done to assess activation sequence of lower extremity muscles. Re–testing of these configurations allowed optimization of rostral muscles | No | Yes |
| 60 | Gorgey (2023) A [109] | Medtronic | PC | 2–8 | T10–L2 | 2–40 | 250–1000 | 1–10 mA | Spinal mapping was done daily after temporary (1 week) and permanent (2 weeks) implantation, as well after the first 6 months of the study (4 weeks) to identify optimal configurations to enable multiple functions and movements without inducing unwanted activity | No | Yes |
| 61 | Gorgey (2023) B [110] | Medtronic | PC | 2–8 | Lumbo-sacral enlarge-ment | 2–25 | 250–1000 | 1–10 mA | Configurations were tested at 2 Hz at three pulse widths (250 μs, 500 μs and 1,000 μs) at current 1–10 mA. For exoskeleton–assisted walking, configuration was optimized at 25 Hz, 250 μs, and 3 mA | No | Yes |
| 62 | Gupta (2023) [111] | – | – | 16 | Lumbo-sacral | 14–90 | 210–350 | – | – | No | No |
| 63 | Hoover (2023) [112] | Abbott | Paddle | – | – | – | – | – | – | No | Yes |
| 64 | Samijema (2023) [113] | Medtronic | Paddle | 16 | Lumbo-sacral | 17–35 | 300–500 | 4–6.8 V | – | No | No |
| Author (Year) | A/I | BWS | EMG | GA | GMA | IWS | OGW | Prop | SoE | Spas | STS | TSW | Key Findings | Complications | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Barolat (1986) [107] | – | – | • | – | • | – | – | – | • | – | – | – | Voluntary motor control of the left quadriceps and spasm abolition occurred with eSCS | None reported |
| 2 | Dimitrijevic (1998) [30] | – | – | • | – | – | – | – | – | – | – | – | – | Rhythmic locomotor–like activity and stepping movement was recruited at frequencies of 25–100 Hz | None reported |
| 3 | Herman (2002) [32] | – | • | – | • | • | • | • | – | • | • | – | • | Immediate improvement in gait rhythm; speed, endurance, and metabolic responses gradually converged with/without eSCS at short distances, although performance with eSCS was superior at long distances | None reported |
| 4 | Cahart (2004) [31] | – | • | • | • | – | • | – | – | • | – | – | • | Reduction in sense of effort for OGW and doubling of walking speed initially. Walking speeds reached 0.35 m/s, with increased ambulation distance > 325m after several weeks of ground training. | High–frequency stimulation (100 Hz) produced discomfort. |
| 5 | Jilge (2004) [134] | – | – | • | – | – | – | – | – | – | – | – | – | eSCS at the lumbosacral region at 5–15 Hz initiates and sustains lower limb extension | None reported |
| 6 | Minassian (2004) [34] | – | – | • | – | – | – | – | – | – | – | – | – | Segmental selective recruitment of lower limb muscles, which is characteristic of posterior root stimulation. A 2.2 Hz stimulation recruited short–latency compound muscle action potentials, whilst 5–15 and 25–50 Hz stimulation elicited sustained tonic extension and rhythmic activity, respectively. | None reported |
| 7 | Ganley (2005) [135] | – | • | • | • | • | • | • | – | • | – | – | • | eSCS enabled patients to walk faster and further | None reported |
| 8 | Huang (2006) [33] | – | • | • | • | • | • | • | – | • | – | – | • | eSCS activates neural structures in the dorsal aspect of the spinal cord and facilitates gait–related muscle recruitment; eSCS improved walking speed, endurance, and reduced SoE | None recorded |
| 9 | Minassian (2007) [136] | – | – | • | – | – | – | – | – | – | – | – | – | 5–15 Hz stimulation initiates lower limb extension; 25–50 Hz elicits alternating lower limb flexion/extension in supine individuals; and eSCS combined with assisted treadmill stepping increases excitability of lumbar cord networks and enhances stepping–like functional motor outputs | None reported |
| 10 | Harkema (2011) [22] | • | • | • | • | • | – | – | • | – | – | – | – | 15 Hz stimulation was optimized for standing, and 30–40 Hz for stepping. Recovery of supraspinal control of some leg movements occurred after 7 months, but only during eSCS | None reported |
| 11 | Monshonkina (2012) [116] | • | • | • | • | – | – | – | – | – | – | Combination of eSCS with locomotor training led to stepping patterns characteristic of normal walking and tonic activity of muscles needed for body balance maintenance. With bipolar stimulation, thresholds of muscle responses were significantly lower than thresholds determined with monopolar stimulation. | None reported | ||
| 12 | Minassian (2013) [118] | • | • | • | – | – | – | – | – | – | – | – | – | eSCS produces rhythmic EMG activities without step–related sensory feedback. eSCS also immediately augmented EMG activities as generated by passive stepping alone, in addition to activating muscles that did not respond otherwise. | None reported |
| 13 | Angeli (2014) [35] | – | • | • | • | • | – | – | – | – | – | – | • | eSCS enables patients with complete paralysis process conceptual, auditory and visual input to regain relatively fine voluntary motor control of paralyzed muscles | None reported |
| 14 | Sayenko (2014) [62] | – | • | • | – | • | – | – | – | – | – | – | – | eSCS of rostral and caudal areas of the lumbar spinal cord led to selective topographical recruitment of proximal and distal leg muscles | None reported |
| 15 | Danner (2015) [137] | – | – | • | – | – | – | – | – | – | – | – | – | Rhythmic activity was generated in 7/10 subjects after stimulation; these rhythms demonstrated flexion and extension phases similar to those needed for locomotion | None reported |
| 16 | Hoefstoetter (2015) [138] | – | – | • | – | – | – | – | – | – | – | – | – | Repeated epidural stimulation of the lumbosacral spinal cord can generate rhythmic burst–like activity at 20–60 Hz | None reported |
| 17 | Rejc (2015) [36] | • | • | • | – | • | – | – | – | – | – | – | – | 2 clinically sensory and motor complete participants could overground weight–bearing stand without external assistance; 2 clinically motor complete, sensory incomplete achieved hip extension with minimal assistance; caudal stimulation at higher frequencies (25–60 Hz) led to improve standing | Discomfort from abdominal contractions |
| 18 | Lu (2016) [117] | – | – | • | – | • | – | – | – | – | – | – | – | Cervical cord neuromodulation improves volitional hand motor function (grip and control) in individuals with chronic tetraplegia | None reported |
| 19 | Grahn (2017) [139] | • | • | • | – | • | – | – | – | – | – | – | – | eSCS with activity–specific training enabled (1) volitional control of task–specific muscle activity; (2) volitional control of rhythmic muscle activity to produce step–like movements while side–lying; (3) independent standing; and (4) voluntary control of step–like movements and rhythmic activity while in a vertical position with body weight partially supported | None noted |
| 20 | Rejc (2017) A [37] | • | • | – | • | – | – | – | – | – | • | – | eSCS with motor training led to ongoing neural adaptations that enabled a refined, task–specific activation pattern and movement duration in the absence of stimulation; re–emergence of muscle activation patterns sufficient for standing with independent knee and hip extension | None noted | |
| 21 | Rejc (2017) B [38] | • | • | • | • | – | – | – | – | – | • | – | Standing improved in all participants after stand training, however, step training worsened standing ability in 3/4 participants | None noted | |
| 22 | Angeli (2018) [39] | • | • | • | • | • | • | • | – | – | – | – | • | Intense locomotor treadmill training with body support and simultaneous eSCS led to independent walking and trunk stability in patients with complete spinal cord injury | Hip fracture during training (1); ankle oedema (1); drainage from surgery site (1) |
| 23 | Formento (2018) [40] | • | • | • | – | • | – | – | • | – | – | – | • | Proprioceptive information facilitates walking with eSCS. Thus, eSCS stimulation parameters that cancel proprioceptive information (continuous stimulation) prevent the modulation of reciprocal inhibitory networks involved in locomotion and reduces or abolishes the conscious perception of leg position | None reported |
| 24 | Gill (2018) [41] | • | • | • | • | • | – | • | • | – | • | – | • | Individuals with complete SCI have greater independence during body weight supported treadmill stepping if proprioceptive inputs are optimized through body weight support | None reported |
| 25 | Wagner (2018) [42] | – | • | • | • | • | • | • | • | – | – | • | • | eSCS re-established adaptive control of paralyzed muscles during overground walking within one week; spatiotemporal stimulation led to volitional control over walking and cycling. | None reported |
| 26 | Calvert (2019) [43] | – | – | • | – | • | – | – | – | – | – | – | – | eSCS–evoked motor responses guide intraoperative electrode placement to enable motor functions. Intentional control of step–like activity was achieved within first 5 days | None reported |
| 27 | Cheng (2019) [44] | – | – | • | – | – | – | – | – | – | – | – | – | During standing, eSCS activates an additional neural circuit, which is critical to, and improves, standing in SCI | None reported |
| 28 | Darrow (2019) [45] | – | – | • | – | • | – | – | – | – | – | – | – | Immediate restoration of volitional motor control with significant improvement in surface EMG during volitional control task with eSCS on | None noted |
| 29 | Gorgey (2020) [46] | • | – | • | – | • | • | • | – | – | – | – | – | After 24 sessions (12 weeks) of exoskeleton–assisted walking with eSCS, swing assistance decreased from 100% to 35%, accompanied by 573 unassisted steps (50% of total steps) | None noted |
| 30 | Penã Pino (2020) [47] | – | – | • | – | – | – | – | – | – | – | – | – | After eSCS, sustained volitional movement was achieved in 4/7 subjects even in the absence of stimulation; volitional power significantly increased with the ability to cycle without stimulation | None noted |
| 31 | Calvert (2021) [48] | – | – | – | – | • | – | – | – | – | – | – | – | eSCS combined with descending commands activate inhibitory inter–neuronal circuitry within spinal sensorimotor networks in SCI | None noted |
| 32 | Gill (2021) [141] | • | • | • | • | • | – | – | • | – | – | – | – | During eSCS–enabled BWST stepping, the knee extensors exhibited an increase in motor activation during trials in which stepping was passive compared to active or during trials in which 60% BWS was provided compared to 20% BWS | None noted |
| 33 | Ibánēz (2021) [49] | • | – | • | – | • | – | – | – | – | – | • | – | eSCS promotes both orderly (according to neuron size) and inverse trends of motor neuron recruitment, with the spinal networks involved in the generation of rhythmic activating favoring orderly recruitment trends | None noted |
| 34 | Linde (2021) [50] | – | – | – | • | • | – | – | – | – | – | – | • | eSCS (both on and off) combined with rehabilitation improved independence in stepping | None noted |
| 35 | Mesbah (2021) [51] | – | – | • | – | • | – | – | – | – | – | – | – | The region and position of lumbosacral enlargement covered by eSCS electrodes significantly correlates with the number of joints moved volitionally. All participants achieved lower extremity volitional motor control post eSCS and prior to any locomotor training | None noted |
| 36 | Gorgey (2022) [52] | • | • | – | – | – | – | – | – | – | – | – | Lumbosacral eSCS restored trunk control and maintained full standing in a person with complete paraplegia | Complete migration of left (outside the epidural space) and right ((from T11–12 to T12–L1) leads | |
| 37 | Kandhari (2022) B [143] | • | • | – | – | • | – | – | – | – | – | – | • | AIS scores changed from A–C for 8 patients and A–D for 2 patients after 8 weeks, with 6 patients improving their functional level of injury by ≥1 segment. Significant improvement in lower extremity muscles were seen in all patients. Independence and comfort were seen during walking post–therapy | None reported |
| 38 | Rowald (2022) [53] | • | • | • | • | • | • | • | • | – | – | • | • | Activity–specific eSCS enabled standing, swimming, cycling, walking and control of trunk movements within 1 day; gait improvement and volitional motor control also occurred after 1 week post eSCS. Neurorehabilitation mediated the restoration of these locomotor activities in community settings | None reported |
| 39 | Smith (2022) [115] | • | – | • | – | • | – | – | – | – | – | • | – | Measures of spared spinal cord tissue significantly relate to standing outcomes with eSCS –– 7/11 subjects with spared spinal cord tissue achieved some knee independence | None reported |
| 40 | Boakye (2023) [108] | • | • | • | – | • | • | – | – | – | – | – | • | All participants achieved voluntary movement in the lower extremities after eSCS. There was a correlation between quality of life with training, functional improvement, and complications | Ileus (2); seroma (2); pain with stimulation (2); dehiscence (2); incision site erythema (1), drainage (1), and cellulitis (1); device infection (1); neurostimulator malposition requiring correction (1); and electrode malfunction (1) |
| 41 | Gorgey (2023) A [109] | • | – | • | • | • | • | • | – | – | – | • | – | eSCS enabled voluntary increased muscle activation and movement below the level of injury and promoted independence during exoskeleton–assisted walking. In one individual, eSCS enabled motor control (below the injury level), and independent standing and stepping | None reported |
| 42 | Gupta (2023) [111] | – | – | – | – | • | – | – | – | – | • | – | – | The patient could perform seated knee extension and hip flexion 2 days post–eSCS implantation. Leg spams and other unwanted movements were abolished following longer–term (3–4 times/week) stimulation | None reported |
| 43 | Hoover (2023) [112] | – | – | • | – | • | – | – | – | – | – | – | – | Following eSCS and conscious effort, all participants were able to pedal without motor assist; eSCS and effort were significantly correlated with maximum power production and distance pedaled. No association was found between volitional movement and patient factors (age, time since injury, and spinal cord atrophy) | None reported |
| # Author (Year) | Age | Years Since Injury | ASIA Score | Level | N | A/I | BWS | GMA | IWS | OGW | STS | TSW | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Barolat (1986) [107] | 22 | 0.75 | C | C5 | 1 | – | – | 1/7 | – | – | – | – |
| 8 | Huang (2006) [33] | 43–48 | 3.5–8 | C | C5–T8 | 2 | – | 0.6 | 2/2 | 2/2 | 2/2 | – | • |
| 11 | Monshonkina (2012) [116] | 22–58 | 2A, 1B, 1B/C | C5–L1 | 4 | – | – | 2/4 | 2/4 | – | – | – | |
| 12 | Minassian (2013) [118] | – | 7A/B | 7 | 0/2 | 0.6 | – | – | – | – | – | ||
| 18 | Lu (2016) [117] | 18–20 | 2–2.5 | B | C5–C6 | 2 | – | – | 2/2 | – | – | – | – |
| 25 | Wagner (2018) [42] | 28–47 | 4–6 | 2C, 1D | C4–T8 | 3 | – | 0 | 3/3 | 3/3 | 2/3 | • | • |
| 26 | Calvert (2019) [43] | 26–37 | 3–6 | A | T3, T6 | 2 | – | – | 2/2 | – | – | – | – |
| 28 | Darrow (2019) [45] | 48–52 | 5–10 | A | T4, T8 | 2 | – | – | 2/2 | – | – | – | – |
| 29 | Gorgey (2020) [46] | 26 | 2 | C | C5 | 1 | 0/1 | – | 1/1 | 1/1 | • | – | – |
| 31 | Calvert (2021) [48] | 26–36 | 3–6 | A | T3, T6 | 2 | – | – | 2/2 | – | – | – | – |
| 34 | Linde (2021) [50] | 26–37 | 3–6 | A | T3, T6 | 2 | – | – | 2/2 | – | – | – | • |
| 36 | Gorgey (2022) [52] | 25 | 3 | A | T3 | 1 | 1/1 | – | – | – | – | – | |
| 37 | Kandhari (2022) [143] | 21–51 | 0.3–2 | A | T2–T12 | 10 | 10/10 | – | 10/10 | – | – | – | • |
| 38 | Rowald (2022) [53] | 29–41 | 1–9 | 2A, 1B | T3–T7 | 3 | 3/3 | 0 | 3/3 | 3/3 | 3/3 | • | • |
| 39 | Smith (2022) [115] | 21–45 | 2–9 | 6A, 5B | C2–T1 | 11 | 1/11 | – | 1/11 | – | – | • | – |
| 40 | Boakye (2023) [108] | 19–60 | 2–17 | 16A, 9B | C2–T5 | 25 | 8/25 | • | 25/25 | 2/8 | – | – | • |
| 41 | Gorgey (2023) A [109] | – | 6–9 | 1A, 1B | C8, T11 | 2 | 1/2 | – | 2/2 | 2/2 | 1/2 | • | – |
| 42 | Gupta (2023) [111] | 25 | 5 | T6 | 1 | – | – | 1/1 | – | – | – | – | |
| 43 | Hoover (2023) [112] | 26–58 | 3–17 | 6A, 1B | T4–T8 | 7 | – | – | 7/7 | – | – | – | – |
| Author (Year) | Cardiovascular | Pulmonary | GI & Genitourinary | Key Findings | Complications | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BP | Orth | HR | CF | Pleth | PAW | PEFR | SPIR | Bowel | B/I | S&V | UD | ||||
| 1 | Katz (1991) [120] | – | – | – | – | – | – | – | – | – | – | – | • | Postoperative changes in the lower urinary tract function were noted in 6 patients. Urodynamic parameters did not change significantly following implantation in the remaining 17 patients | None reported |
| 2 | DiMarco (2006) [100] | – | – | – | – | – | • | • | – | – | – | – | – | Combined T9 + L1 stimulation led to airway pressure and expiratory flow rates observed with a normal subject: airway pressure increased to 90 cm H2O (T9), 82 cm H2O (L1) and 132 cm H2O (T9 + L1); peak expiratory flow rate also increased to 6.4 L/s (T9), 5.0 L/s (L1), and 7.4 L/s (T9 + L1). | None reported |
| 3 | DiMarco (2009) [101] | – | – | – | – | – | • | • | – | – | – | – | – | Supramaximal SCS led to increases in both mean maximum peak airflow rates, from mean 1.86 ± 0.17 L/s at baseline to 8.6 ± 1.8 L/s (mean ± SE), and airway pressure from 22.4 ± 1.18 cm H2O at baseline to 137 ± 30 cm H2O (mean ± SE). | One non–functional lead (9); breakdown and infection (1); temporary asymptomatic AD (3) |
| 4 | Harkema (2011) [22] | – | – | – | – | – | – | – | – | – | – | • | – | eSCS with training led to functional gains in bladder and sexual function–the patient was able to voluntarily void with minimal residual volume of urine after previously having no voluntary bladder contraction. | None reported |
| 5 | Aslan (2018) [141] | • | • | • | – | • | – | – | – | – | – | – | – | eSCS applied while supine and standing resulted in increased arterial BP in individuals with SCI–induced cardiovascular deficits | None reported |
| 6 | DiMarco (2018) [102] | – | – | – | – | – | • | • | – | – | – | – | – | Spontaneous maximum airway pressure increased from 20 cm H2O to 61 and 86 cmH2O for FRC and TLC, respectively (monopolar stimulation, T9) and to 84 and 103 cmH2O for FRC and TLC, respectively (bipolar stimulation, T9 + T11); the subject also experienced greater sense in raising secretions with eSCS and no longer required other methods of secretion management | Temporary asymptomatic AD that resolved after 5–6 weeks |
| 7 | Harkema (2018) A [78] | • | • | • | – | • | – | – | – | – | – | – | – | Dorsal lumbosacral eSCS can effectively and safely activate mechanisms to elevate BP to normal ranges from a chronic hypotensive state in humans with severe SCI with individual–specific cardiovascular eSCS | None reported |
| 8 | Harkema (2018) B [132] | • | • | • | – | • | – | – | – | – | – | – | – | Orthostatic hypotension resolved with cardiovascular eSCS and after daily eSCS training without stimulation | None reported |
| 9 | Herrity (2018) [130] | – | – | – | – | – | – | – | – | – | – | • | • | Optimized parameters yielded lowest post–void residual volume and also improved reflexive voiding efficiency | None reported |
| 10 | Walter (2018) [126] | – | – | – | – | – | – | – | – | – | – | – | • | eSCS significantly reduced the time needed for bowel management and modulated detrusor pressure and external sphincter/pelvic floor muscle tone. | None reported |
| 11 | West (2018) [79] | • | • | • | • | – | – | – | – | – | – | – | The stimulation resolved orthostatic hypotension and related symptoms through action on preventing reduced MCA blood flow; eSCS also improved cardiac function | None reported | |
| 12 | Darrow (2019) [45] | • | • | • | • | – | – | – | – | • | • | • | – | eSCS led to restoration of cardiovascular function, orgasm, volitional urination, and improved surface EMG power during a volitional control task with eSCS on | None reported |
| 13 | Nightingale (2019) [130] | • | • | – | • | – | – | – | – | – | – | – | – | eSCS parameters optimized to facilitate motor function can also modulate cardiovascular function (increasing or maintaining arterial BP at rest or in response to an orthostatic challenge, respectively) | None reported |
| 14 | Terson de Paleville (2019) [122] | • | – | • | – | – | – | – | – | – | – | – | – | Combined eSCS and task–specific training improves cardiovascular fitness and body composition (reduces percentage fat, particularly android fat and android/gynoid ratio) | None reported |
| 15 | DiMarco (2020) [102] | – | – | – | – | – | • | • | – | – | – | – | – | SCS improved both expiratory muscle function (maximum expiratory pressure and cough restoration) and inspiratory muscle function (inspiratory capacity and maximum inspiratory pressure) after 20 weeks following daily stimulation | None reported |
| 16 | Beck (2021) [120] | – | – | – | – | – | – | – | – | – | • | • | • | eSCS optimized for locomotion negatively impacted neurogenic bladder functionality, leading to increase in episodes of urinary incontinence with worsening bladder compliance and pressures. One participant showed increase in lean body mass | None reported |
| 17 | DiMarco (2021) [123] | – | – | – | – | – | • | • | • | • | – | – | – | Optimized eSCS parameters for maximum airway pressure generation improves bowel movements and quality of life | None reported |
| 18 | Herrity (2021) [121] | • | – | • | – | • | – | – | – | – | • | • | Bladder storage parameters were significantly improved at post–training and at follow–up. Elevated BP during bladder extension, which is characteristic of AD, was however not attenuated | None reported | |
| 19 | Kandhari (2022) A [114] | – | – | – | – | – | • | – | • | – | – | – | – | eSCS at T2–T5 improved pulmonary function by increasing inspired volume, and promoting pulmonary dependence from mechanical ventilation to pressure support | None reported |
| 20 | Squair (2021) [98] | • | • | • | – | • | – | – | – | – | – | – | – | eSCS activates the sympathetic circuitry by increasing sympathetic nerve activity and normalizing circulating NE levels. Real–time hemodynamic stabilization during orthostatic challenges was seen with eSCS, which reduces the burden of orthostatic hypotension with long–term use | None reported |
| 21 | Herrity (2022) [142] | • | – | • | – | – | – | – | – | – | • | • | • | eSCS reduces incidences of urinary incontinence and provides a means for mitigating AD associated with bladder distension | None reported |
| 22 | Boakye (2023) [108] | • | – | – | – | – | – | – | – | – | – | – | – | All participants achieved SBP regulation within 110–120 mmHg and were able to integrate the eSCS into their daily lives; no worsening of bladder function was seen | Same as reported for motor outcomes |
| 23 | Gorgey (2023) B [110] | • | • | • | – | – | – | – | – | – | – | – | – | Post eSCS implantation cardiovascular autonomic control was enhanced during transitions from a supine position to a 45–degree head–up–tilt (orthostatic challenge) | None reported |
| 24 | Samijema (2023) [113] | • | – | • | – | – | – | – | – | – | – | – | – | Lumbosacral eSCS reduces elevation in BP during bowel procedures, preventing AD | None reported |
5.5. Limitations and Future Perspectives
5.6. Recommendations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- National Spinal Cord Injury Statistical Center. Facts and Figures at a Glance; University of Alabama at Birmingham: Birmingham, AL, USA, 2020. [Google Scholar]
- Lo, J.; Chan, L.; Flynn, S. A Systematic Review of the Incidence, Prevalence, Costs, and Activity and Work Limitations of Amputation, Osteoarthritis, Rheumatoid Arthritis, Back Pain, Multiple Sclerosis, Spinal Cord Injury, Stroke, and Traumatic Brain Injury in the United States: A 2019 Update. Arch. Phys. Med. Rehabil. 2021, 102, 115–131. [Google Scholar]
- Roberts, T.T.; Leonard, G.R.; Cepela, D.J. Classifications in Brief: American Spinal Injury Association (ASIA) Impairment Scale. Clin. Orthop. Relat. Res. 2017, 475, 1499–1504. [Google Scholar] [CrossRef]
- Sezer, N.; Akkuş, S.; Uğurlu, F.G. Chronic complications of spinal cord injury. World J. Orthop. 2015, 18, 24–33. [Google Scholar] [CrossRef]
- Hachem, L.D.; Ahuja, C.S.; Fehlings, M.G. Assessment and management of acute spinal cord injury: From point of injury to rehabilitation. J. Spinal Cord Med. 2017, 40, 665–675. [Google Scholar] [CrossRef] [PubMed]
- Russo, G.S.; Mangan, J.J.; Galetta, M.S.; Boody, B.; Bronson, W.; Segar, A.; Kepler, C.K.; Kurd, M.F.; Hilibrand, A.S.; Vaccaro, A.R.; et al. Update on Spinal Cord Injury Management. Clin. Spine Surg. 2020, 33, 258–264. [Google Scholar] [CrossRef] [PubMed]
- Truchon, C.; Fallah, N.; Santos, A.; Vachon, J.; Noonan, V.K.; Cheng, C.L. Impact of Therapy on Recovery during Rehabilitation in Patients with Traumatic Spinal Cord Injury. J. Neurotrauma 2017, 34, 2901–2909. [Google Scholar] [CrossRef] [PubMed]
- Arazpour, M.; Bani, M.A.; Hutchins, S.W.; Jones, R.K. The physiological cost index of walking with mechanical and powered gait orthosis in patients with spinal cord injury. Spinal Cord 2013, 51, 356–359. [Google Scholar] [CrossRef] [PubMed]
- Mekki, M.; Delgado, A.D.; Fry, A.; Putrino, D.; Huang, V. Robotic Rehabilitation and Spinal Cord Injury: A Narrative Review. Neurotherapeutics 2018, 15, 604–617. [Google Scholar] [CrossRef] [PubMed]
- Shinozaki, M.; Nagoshi, N.; Nakamura, M.; Okano, H. Mechanisms of Stem Cell Therapy in Spinal Cord Injuries. Cells 2021, 10, 2676. [Google Scholar] [CrossRef] [PubMed]
- Guo, J.S.; Qian, C.H.; Ling, E.A.; Zeng, Y.S. Nanofiber scaffolds for treatment of spinal cord injury. Curr. Med. Chem. 2014, 21, 4282–4289. [Google Scholar] [CrossRef]
- Li, X.; Liu, D.; Xiao, Z.; Zhao, Y.; Han, S.; Chen, B.; Dai, J. Scaffold-facilitated locomotor improvement post complete spinal cord injury: Motor axon regeneration versus endogenous neuronal relay formation. Biomaterials 2019, 197, 20–31. [Google Scholar] [CrossRef] [PubMed]
- Zou, Y. Targeting axon guidance cues for neural circuit repair after spinal cord injury. J. Cereb. Blood Flow Metab. 2021, 41, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Ladenbauer, J.; Minassian, K.; Hofstoetter, U.S.; Dimitrijevic, M.R.; Rattay, F. Stimulation of the human lumbar spinal cord with implanted and surface electrodes: A computer simulation study. IEEE Trans. Neural Syst. Rehabil. Eng. 2010, 18, 637–645. [Google Scholar] [CrossRef] [PubMed]
- Capogrosso, M.; Wenger, N.; Raspopovic, S.; Musienko, P.; Beauparlant, J.; Bassi Luciani, L.; Courtine, G.; Micera, S. A computational model for epidural electrical stimulation of spinal sensorimotor circuits. J. Neurosci. 2013, 33, 19326–19340. [Google Scholar] [CrossRef] [PubMed]
- Van den Brand, R.; Heutschi, J.; Barraud, Q.; DiGiovanna, J.; Bartholdi, K.; Huerlimann, M.; Friedli, L.; Vollenweider, I.; Moraud, E.M.; Duis, S.; et al. Restoring voluntary control of locomotion after paralyzing spinal cord injury. Science 2012, 336, 1182–1185. [Google Scholar] [CrossRef] [PubMed]
- Shah, P.K.; Sureddi, S.; Alam, M.; Zhong, H.; Roy, R.R.; Edgerton, V.R.; Gerasimenko, Y. Unique Spatiotemporal Neuromodulation of the Lumbosacral Circuitry Shapes Locomotor Success after Spinal Cord Injury. J. Neurotrauma 2016, 33, 1709–1723. [Google Scholar] [CrossRef]
- Melzack, R.; Wall, P. Pain mechanisms: A new theory. Science 1965, 150, 971–979. [Google Scholar] [CrossRef]
- Wall, P.D.; Sweet, W.H. Temporary abolition of pain in man. Science 1967, 155, 108–109. [Google Scholar] [CrossRef]
- Shealy, C.N.; Taslitz, N.; Mortimer, J.T.; Becker, D.P. Electrical inhibition of pain: Experimental evaluation. Anesth. Analg. 1967, 46, 299–305. [Google Scholar] [CrossRef]
- Cook, A.W.; Weinstein, S.P. Chronic dorsal column stimulation in multiple sclerosis. Prelim. Rep. N. Y. State J. Med. 1973, 73, 2868–2872. [Google Scholar]
- Harkema, S.; Gerasimenko, Y.; Hodes, J.; Burdick, J.; Angeli, C.; Chen, Y.; Ferreira, C.; Willhite, A.; Rejc, E.; Grossman, R.G.; et al. Effect of epidural stimulation of the lumbosacral spinal cord on voluntary movement, standing, and assisted stepping after motor complete paraplegia: A case study. Lancet 2011, 377, 1938–1947. [Google Scholar] [CrossRef] [PubMed]
- Siegfried, J.; Lazorthes, Y.; Broggi, G. Electrical spinal cord stimulation for spastic movement disorders. Appl. Neurophysiol. 1981, 44, 77–92. [Google Scholar] [CrossRef] [PubMed]
- Richardson, R.R.; McLone, D.G. Percutaneous epidural neurostimulation for paraplegic spasticity. Surg. Neurol. 1978, 9, 153–155. [Google Scholar] [PubMed]
- Dimitrijevic, M.M.; Dimitrijevic, M.R.; Illis, L.S.; Nakajima, K.; Sharkey, P.C.; Sherwood, A.M. Spinal cord stimulation for the control of spasticity in patients with chronic spinal cord injury: I. Clinical observations. Cent. Nerv. Syst. Trauma 1986, 3, 129–144. [Google Scholar] [CrossRef] [PubMed]
- Pinter, M.M.; Gerstenbrand, F.; Dimitrijevic, M.R. Epidural electrical stimulation of posterior structures of the human lumbosacral cord: 3. Control of spasticity. Spinal Cord 2000, 38, 524–531. [Google Scholar] [CrossRef]
- Sherrington, C.S. Observations on the scratch-reflex in the spinal dog. J. Physiol. 1906, 34, 1–50. [Google Scholar] [CrossRef]
- Grillner, S.; Zangger, P. How detailed is the central pattern generation for locomotion? Brain Res. 1975, 88, 367–371. [Google Scholar] [CrossRef]
- Bussel, B.; Roby-Brami, A.; Néris, O.R.; Yakovleff, A. Evidence for a spinal stepping generator in man. Paraplegia 1996, 34, 91–92. [Google Scholar] [CrossRef]
- Dimitrijevic, M.R.; Gerasimenko, Y.; Pinter, M.M. Evidence for a spinal central pattern generator in humans. Ann. N. Y. Acad. Sci. 1998, 860, 360–376. [Google Scholar] [CrossRef]
- Carhart, M.R.; He, J.; Herman, R.; D’Luzansky, S.; Willis, W.T. Epidural spinal-cord stimulation facilitates recovery of functional walking following incomplete spinal-cord injury. IEEE Trans. Neural Syst. Rehabil. Eng. 2004, 12, 32–42. [Google Scholar] [CrossRef] [PubMed]
- Herman, R.; He, J.; D’Luzansky, S.; Willis, W.; Dilli, S. Spinal cord stimulation facilitates functional walking in a chronic, incomplete spinal cord injured. Spinal Cord 2002, 40, 65–68. [Google Scholar] [CrossRef]
- Huang, H.; He, J.; Herman, R.; Carhart, M.R. Modulation effects of epidural spinal cord stimulation on muscle activities during walking. IEEE Trans. Neural Syst. Rehabil. Eng. 2006, 14, 14–23. [Google Scholar] [CrossRef]
- Minassian, K.; Jilge, B.; Rattay, F.; Pinter, M.M.; Binder, H.; Gerstenbrand, F.; Dimitrijevic, M.R. Stepping-like movements in humans with complete spinal cord injury induced by epidural stimulation of the lumbar cord: Electromyographic study of compound muscle action potentials. Spinal Cord 2004, 42, 401–416. [Google Scholar] [CrossRef]
- Angeli, C.A.; Edgerton, V.R.; Gerasimenko, Y.P.; Harkema, S.J. Altering spinal cord excitability enables voluntary movements after chronic complete paralysis in humans. Brain 2014, 137 Pt 5, 1394–1409. [Google Scholar] [CrossRef]
- Rejc, E.; Angeli, C.; Harkema, S. Effects of Lumbosacral Spinal Cord Epidural Stimulation for Standing after Chronic Complete Paralysis in Humans. PLoS ONE 2015, 10, e0133998. [Google Scholar] [CrossRef]
- Rejc, E.; Angeli, C.A.; Atkinson, D.; Harkema, S.J. Motor recovery after activity-based training with spinal cord epidural stimulation in a chronic motor complete paraplegic. Sci. Rep. 2017, 7, 13476. [Google Scholar] [CrossRef] [PubMed]
- Rejc, E.; Angeli, C.A.; Bryant, N.; Harkema, S.J. Effects of Stand and Step Training with Epidural Stimulation on Motor Function for Standing in Chronic Complete Paraplegics. J. Neurotrauma 2017, 34, 1787–1802. [Google Scholar] [CrossRef] [PubMed]
- Angeli, C.A.; Boakye, M.; Morton, R.A.; Vogt, J.; Benton, K.; Chen, Y.; Ferreira, C.K.; Harkema, S.J. Recovery of over-Ground Walking after Chronic Motor Complete Spinal Cord Injury. N. Engl. J. Med. 2018, 379, 1244–1250. [Google Scholar] [CrossRef] [PubMed]
- Formento, E.; Minassian, K.; Wagner, F.; Mignardot, J.B.; Le Goff-Mignardot, C.G.; Rowald, A.; Bloch, J.; Micera, S.; Capogrosso, M.; Courtine, G. Electrical spinal cord stimulation must preserve proprioception to enable locomotion in humans with spinal cord injury. Nat. Neurosci. 2018, 21, 1728–1741. [Google Scholar] [CrossRef] [PubMed]
- Gill, M.L.; Grahn, P.J.; Calvert, J.S.; Linde, M.B.; Lavrov, I.A.; Strommen, J.A.; Beck, L.A.; Sayenko, D.G.; Van Straaten, M.G.; Drubach, D.I.; et al. Neuromodulation of lumbosacral spinal networks enables independent stepping after complete paraplegia. Nat. Med. 2018, 24, 1677–1682. [Google Scholar] [CrossRef] [PubMed]
- Wagner, F.B.; Mignardot, J.B.; Le Goff-Mignardot, C.G.; Demesmaeker, R.; Komi, S.; Capogrosso, M.; Rowald, A.; Seáñez, I.; Caban, M.; Pirondini, E.; et al. Targeted neurotechnology restores walking in humans with spinal cord injury. Nature 2018, 563, 65–71. [Google Scholar] [CrossRef] [PubMed]
- Calvert, J.S.; Grahn, P.J.; Strommen, J.A.; Lavrov, I.A.; Beck, L.A.; Gill, M.L.; Linde, M.B.; Brown, D.A.; Van Straaten, M.G.; Veith, D.D.; et al. Electrophysiological Guidance of Epidural Electrode Array Implantation over the Human Lumbosacral Spinal Cord to Enable Motor Function after Chronic Paralysis. J. Neurotrauma 2019, 36, 1451–1460. [Google Scholar] [CrossRef] [PubMed]
- Cheng, R.; Sui, Y.; Sayenko, D.; Burdick, J.W. Motor Control after Human SCI through Activation of Muscle Synergies under Spinal Cord Stimulation. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 1331–1340. [Google Scholar] [CrossRef] [PubMed]
- Darrow, D.; Balser, D.; Netoff, T.I.; Krassioukov, A.; Phillips, A.; Parr, A.; Samadani, U. Epidural Spinal Cord Stimulation Facilitates Immediate Restoration of Dormant Motor and Autonomic Supraspinal Pathways after Chronic Neurologically Complete Spinal Cord Injury. J. Neurotrauma 2019, 36, 2325–2336. [Google Scholar] [CrossRef] [PubMed]
- Gorgey, A.S.; Gill, S.; Holman, M.E.; Davis, J.C.; Atri, R.; Bai, O.; Goetz, L.; Lester, D.L.; Trainer, R.; Lavis, T.D. The feasibility of using exoskeletal-assisted walking with epidural stimulation: A case report study. Ann. Clin. Transl. Neurol. 2020, 7, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Peña Pino, I.; Hoover, C.; Venkatesh, S.; Ahmadi, A.; Sturtevant, D.; Patrick, N.; Freeman, D.; Parr, A.; Samadani, U.; Balser, D.; et al. Long-Term Spinal Cord Stimulation after Chronic Complete Spinal Cord Injury Enables Volitional Movement in the Absence of Stimulation. Front. Syst. Neurosci. 2020, 14, 35. [Google Scholar] [CrossRef] [PubMed]
- Calvert, J.S.; Gill, M.L.; Linde, M.B.; Veith, D.D.; Thoreson, A.R.; Lopez, C.; Lee, K.H.; Gerasimenko, Y.P.; Edgerton, V.R.; Lavrov, I.A.; et al. Voluntary Modulation of Evoked Responses Generated by Epidural and Transcutaneous Spinal Stimulation in Humans with Spinal Cord Injury. J. Clin. Med. 2021, 10, 4898. [Google Scholar] [CrossRef]
- Ibáñez, J.; Angeli, C.A.; Harkema, S.J.; Farina, D.; Rejc, E. Recruitment order of motor neurons promoted by epidural stimulation in individuals with spinal cord injury. J. Appl. Physiol. 2021, 131, 1100–1110. [Google Scholar] [CrossRef]
- Linde, M.B.; Thoreson, A.R.; Lopez, C.; Gill, M.L.; Veith, D.D.; Hale, R.F.; Calvert, J.S.; Grahn, P.J.; Fautsch, K.J.; Sayenko, D.G.; et al. Quantitative Assessment of Clinician Assistance during Dynamic Rehabilitation Using Force Sensitive Resistors. Front. Rehabil. Sci. 2021, 2, 757828. [Google Scholar] [CrossRef]
- Mesbah, S.; Ball, T.; Angeli, C.; Rejc, E.; Dietz, N.; Ugiliweneza, B.; Harkema, S.; Boakye, M. Predictors of volitional motor recovery with epidural stimulation in individuals with chronic spinal cord injury. Brain 2021, 144, 420–433. [Google Scholar] [CrossRef]
- Gorgey, A.S.; Gouda, J.J. Single Lead Epidural Spinal Cord Stimulation Targeted Trunk Control and Standing in Complete Paraplegia. J. Clin. Med. 2022, 11, 5120. [Google Scholar] [CrossRef] [PubMed]
- Rowald, A.; Komi, S.; Demesmaeker, R.; Baaklini, E.; Hernandez-Charpak, S.D.; Paoles, E.; Montanaro, H.; Cassara, A.; Becce, F.; Lloyd, B.; et al. Activity-dependent spinal cord neuromodulation rapidly restores trunk and leg motor functions after complete paralysis. Nat. Med. 2022, 28, 260–271. [Google Scholar] [CrossRef] [PubMed]
- Logé, D.; De Coster, O.; Washburn, S. Technological innovation in spinal cord stimulation: Use of a newly developed delivery device for introduction of spinal cord stimulation leads. Neuromodulation 2012, 15, 392–401. [Google Scholar] [CrossRef] [PubMed]
- Pahapill, P.A. Surgical paddle-lead placement for screening trials of spinal cord stimulation. Neuromodulation 2014, 17, 346–348, discussion 348. [Google Scholar] [CrossRef]
- Lacroix-Ouellette, P.; Dubuc, R. Brainstem neural mechanisms controlling locomotion with special reference to basal vertebrates. Front. Neural Circuits 2023, 17, 910207. [Google Scholar] [CrossRef]
- Kiehn, O. Locomotor circuits in the mammalian spinal cord. Annu. Rev. Neurosci. 2006, 29, 279–306. [Google Scholar] [CrossRef]
- Chalif, J.I.; Martínez-Silva, M.L.; Pagiazitis, J.G.; Murray, A.J.; Mentis, G.Z. Control of mammalian locomotion by ventral spinocerebellar tract neurons. Cell 2022, 185, 328–344.e26. [Google Scholar] [CrossRef]
- Whelan, P.; Bonnot, A.; O’Donovan, M.J. Properties of rhythmic activity generated by the isolated spinal cord of the neonatal mouse. J. Neurophysiol. 2000, 84, 2821–2833. [Google Scholar] [CrossRef]
- Laliberte, A.M.; Goltash, S.; Lalonde, N.R.; Bui, T.V. Propriospinal Neurons: Essential Elements of Locomotor Control in the Intact and Possibly the Injured Spinal Cord. Front. Cell. Neurosci. 2019, 13, 512. [Google Scholar] [CrossRef]
- Courtine, G.; Gerasimenko, Y.; van den Brand, R.; Yew, A.; Musienko, P.; Zhong, H.; Song, B.; Ao, Y.; Ichiyama, R.M.; Lavrov, I.; et al. Transformation of nonfunctional spinal circuits into functional states after the loss of brain input. Nat. Neurosci. 2009, 12, 1333–1342. [Google Scholar] [CrossRef]
- Sayenko, D.G.; Angeli, C.; Harkema, S.J.; Edgerton, V.R.; Gerasimenko, Y.P. Neuromodulation of evoked muscle potentials induced by epidural spinal-cord stimulation in paralyzed individuals. J. Neurophysiol. 2014, 111, 1088–1099. [Google Scholar] [CrossRef]
- Guertin, P.; Angel, M.J.; Perreault, M.C.; McCrea, D.A. Ankle extensor group I afferents excite extensors throughout the hindlimb during fictive locomotion in the cat. J. Physiol. 1995, 487, 197–209. [Google Scholar] [CrossRef]
- Stein, R.B.; Capaday, C. The modulation of human reflexes during functional motor tasks. Trends Neurosci. 1988, 11, 328–332. [Google Scholar] [CrossRef] [PubMed]
- Harkema, S.J.; Hurley, S.L.; Patel, U.K.; Requejo, P.S.; Dobkin, B.H.; Edgerton, V.R. Human lumbosacral spinal cord interprets loading during stepping. J. Neurophysiol. 1997, 77, 797–811. [Google Scholar] [CrossRef] [PubMed]
- Cappellini, G.; Ivanenko, Y.P.; Dominici, N.; Poppele, R.E.; Lacquaniti, F. Migration of motor pool activity in the spinal cord reflects body mechanics in human locomotion. J. Neurophysiol. 2010, 104, 3064–3073. [Google Scholar] [CrossRef] [PubMed]
- Courtine, G.; Song, B.; Roy, R.R.; Zhong, H.; Herrmann, J.E.; Ao, Y.; Qi, J.; Edgerton, V.R.; Sofroniew, M.V. Recovery of supraspinal control of stepping via indirect propriospinal relay connections after spinal cord injury. Nat. Med. 2008, 14, 69–74. [Google Scholar] [CrossRef] [PubMed]
- Martinez, M.; Delivet-Mongrain, H.; Leblond, H.; Rossignol, S. Effect of locomotor training in completely spinalized cats previously submitted to a spinal hemisection. J. Neurosci. 2012, 32, 10961–10970. [Google Scholar] [CrossRef] [PubMed]
- Lavrov, I.; Courtine, G.; Dy, C.J.; van den Brand, R.; Fong, A.J.; Gerasimenko, Y.; Zhong, H.; Roy, R.R.; Edgerton, V.R. Facilitation of stepping with epidural stimulation in spinal rats: Role of sensory input. J. Neurosci. 2008, 28, 7774–7780. [Google Scholar] [CrossRef] [PubMed]
- Lavrov, I.; Gerasimenko, Y.; Burdick, J.; Zhong, H.; Roy, R.R.; Edgerton, V.R. Integrating multiple sensory systems to modulate neural networks controlling posture. J. Neurophysiol. 2015, 114, 3306–3314. [Google Scholar] [CrossRef] [PubMed]
- Takeoka, A.; Vollenweider, I.; Courtine, G.; Arber, S. Muscle spindle feedback directs locomotor recovery and circuit reorganization after spinal cord injury. Cell 2014, 159, 1626–1639. [Google Scholar] [CrossRef]
- Takeoka, A.; Arber, S. Functional Local Proprioceptive Feedback Circuits Initiate and Maintain Locomotor Recovery after Spinal Cord Injury. Cell Rep. 2019, 27, 71–85.e3. [Google Scholar] [CrossRef]
- Forssberg, H.; Grillner, S.; Halbertsma, J. The locomotion of the low spinal cat. I. Coordination within a hindlimb. Acta Physiol. Scand. 1980, 108, 269–281. [Google Scholar] [CrossRef] [PubMed]
- Baumbauer, K.M.; Hoy, K.C., Jr.; Huie, J.R.; Hughes, A.J.; Woller, S.A.; Puga, D.A.; Setlow, B.; Grau, J.W. Timing in the absence of supraspinal input I: Variable, but not fixed, spaced stimulation of the sciatic nerve undermines spinally-mediated instrumental learning. Neuroscience 2008, 155, 1030–1047. [Google Scholar] [CrossRef] [PubMed]
- Grillner, S.; El Manira, A. Current Principles of Motor Control, with Special Reference to Vertebrate Locomotion. Physiol. Rev. 2020, 100, 271–320. [Google Scholar] [CrossRef] [PubMed]
- Tesio, L.; Scarano, S. Ground Walking in Chronic Complete Spinal Cord Injury: Does Epidural Stimulation Allow “Awakening” of Corticospinal Circuits? A Wide-Ranging Epistemic Criticism. Am. J. Phys. Med. Rehabil. 2021, 100, e43–e47. [Google Scholar] [CrossRef]
- Harkema, S.J.; Wang, S.; Angeli, C.A.; Chen, Y.; Boakye, M.; Ugiliweneza, B.; Hirsch, G.A. Normalization of Blood Pressure with Spinal Cord Epidural Stimulation after Severe Spinal Cord Injury. Front. Hum. Neurosci. 2018, 12, 83. [Google Scholar] [CrossRef]
- West, C.R.; Phillips, A.A.; Squair, J.W.; Williams, A.M.; Walter, M.; Lam, T.; Krassioukov, A.V. Association of Epidural Stimulation with Cardiovascular Function in an Individual with Spinal Cord Injury. JAMA Neurol. 2018, 75, 630–632. [Google Scholar] [CrossRef] [PubMed]
- Collins, H.L.; DiCarlo, S.E. TENS attenuates response to colon distension in paraplegic and quadriplegic rats. Am. J. Physiol. Heart Circ. Physiol. 2002, 283, H1734–H1739. [Google Scholar] [CrossRef] [PubMed]
- Sachdeva, R.; Nightingale, T.E.; Pawar, K.; Kalimullina, T.; Mesa, A.; Marwaha, A.; Williams, A.M.M.; Lam, T.; Krassioukov, A.V. Noninvasive Neuroprosthesis Promotes Cardiovascular Recovery after Spinal Cord Injury. Neurotherapeutics 2021, 18, 1244–1256. [Google Scholar] [CrossRef]
- Legg Ditterline, B.E.; Aslan, S.C.; Wang, S.; Ugiliweneza, B.; Hirsch, G.A.; Wecht, J.M.; Harkema, S. Restoration of autonomic cardiovascular regulation in spinal cord injury with epidural stimulation: A case series. Clin. Auton. Res. 2021, 31, 317–320. [Google Scholar] [CrossRef]
- DiMarco, A.F.; Romaniuk, J.R.; Kowalski, K.E.; Supinski, G. Pattern of expiratory muscle activation during lower thoracic spinal cord stimulation. J. Appl. Physiol. 1999, 86, 1881–1889. [Google Scholar] [CrossRef]
- DiMarco, A.F.; Kowalski, K.E. Activation of inspiratory muscles via spinal cord stimulation. Respir. Physiol. Neurobiol. 2013, 189, 438–449. [Google Scholar] [CrossRef]
- Gonzalez-Rothi, E.J.; Streeter, K.A.; Hanna, M.H.; Stamas, A.C.; Reier, P.J.; Baekey, D.M.; Fuller, D.D. High-frequency epidural stimulation across the respiratory cycle evokes phrenic short-term potentiation after incomplete cervical spinal cord injury. J. Neurophysiol. 2017, 118, 2344–2357. [Google Scholar] [CrossRef]
- Jensen, V.N.; Alilain, W.J.; Crone, S.A. Role of Propriospinal Neurons in Control of Respiratory Muscles and Recovery of Breathing Following Injury. Front. Syst. Neurosci. 2020, 13, 84. [Google Scholar] [CrossRef]
- Nair, J.; Bezdudnaya, T.; Zholudeva, L.V.; Detloff, M.R.; Reier, P.J.; Lane, M.A.; Fuller, D.D. Histological identification of phrenic afferent projections to the spinal cord. Respir. Physiol. Neurobiol. 2017, 236, 57–68. [Google Scholar] [CrossRef] [PubMed]
- Nair, J.; Streeter, K.A.; Turner, S.M.F.; Sunshine, M.D.; Bolser, D.C.; Fox, E.J.; Davenport, P.W.; Fuller, D.D. Anatomy and physiology of phrenic afferent neurons. J. Neurophysiol. 2017, 118, 2975–2990. [Google Scholar] [CrossRef] [PubMed]
- Baumann, S.B.; Wozny, D.R.; Kelly, S.K.; Meno, F.M. The electrical conductivity of human cerebrospinal fluid at body temperature. IEEE Trans. Biomed. Eng. 1997, 44, 220–223. [Google Scholar] [CrossRef] [PubMed]
- Tawfik, V.L.; Chang, S.Y.; Hitti, F.L.; Roberts, D.W.; Leiter, J.C.; Jovanovic, S.; Lee, K.H. Deep brain stimulation results in local glutamate and adenosine release: Investigation into the role of astrocytes. Neurosurgery 2010, 67, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Karnup, S.V.; de Groat, W.C. Propriospinal Neurons of L3–L4 Segments Involved in Control of the Rat External Urethral Sphincter. Neuroscience 2020, 425, 12–28. [Google Scholar] [CrossRef] [PubMed]
- de Groat, W.C.; Yoshimura, N. Afferent nerve regulation of bladder function in health and disease. Handb. Exp. Pharmacol. 2009, 194, 91–138. [Google Scholar]
- Chéhensse, C.; Facchinetti, P.; Bahrami, S.; Andrey, P.; Soler, J.M.; Chrétien, F.; Bernabe, J.; Clement, P.; Denys, P.; Giuliano, F. Human spinal ejaculation generator. Ann. Neurol. 2017, 81, 35–45. [Google Scholar] [CrossRef]
- Boggs, J.W.; Wenzel, B.J.; Gustafson, K.J.; Grill, W.M. Frequency-dependent selection of reflexes by pudendal afferents in the cat. J. Physiol. 2006, 577 Pt 1, 115–126. [Google Scholar] [CrossRef] [PubMed]
- de Groat, W.C.; Ryall, R.W. Reflexes to sacral parasympathetic neurones concerned with micturition in the cat. J. Physiol. 1969, 200, 87–108. [Google Scholar] [CrossRef]
- Tai, C.; Wang, J.; Wang, X.; de Groat, W.C.; Roppolo, J.R. Bladder inhibition or voiding induced by pudendal nerve stimulation in chronic spinal cord injured cats. Neurourol. Urodyn. 2007, 26, 570–577. [Google Scholar] [CrossRef]
- Schurch, B.; Reilly, I.; Reitz, A.; Curt, A. Electrophysiological recordings during the peripheral nerve evaluation (PNE) test in complete spinal cord injury patients. World J. Urol. 2003, 20, 319–322. [Google Scholar] [CrossRef]
- Burns, M.; Solinsky, R. Toward rebalancing blood pressure instability after spinal cord injury with spinal cord electrical stimulation: A mini review and critique of the evolving literature. Auton. Neurosci. 2022, 237, 102905. [Google Scholar] [CrossRef] [PubMed]
- Squair, J.W.; Gautier, M.; Mahe, L.; Soriano, J.E.; Rowald, A.; Bichat, A.; Cho, N.; Anderson, M.A.; James, N.D.; Gandar, J.; et al. Neuroprosthetic baroreflex controls haemodynamics after spinal cord injury. Nature 2021, 590, 308–314. [Google Scholar] [CrossRef] [PubMed]
- DiMarco, A.F.; Kowalski, K.E.; Geertman, R.T.; Hromyak, D.R. Spinal cord stimulation: A new method to produce an effective cough in patients with spinal cord injury. Am. J. Respir. Crit. Care Med. 2006, 173, 1386–1389. [Google Scholar] [CrossRef]
- DiMarco, A.F.; Kowalski, K.E.; Geertman, R.T.; Hromyak, D.R.; Frost, F.S.; Creasey, G.H.; Nemunaitis, G.A. Lower thoracic spinal cord stimulation to restore cough in patients with spinal cord injury: Results of a National Institutes of Health-Sponsored clinical trial. Part II: Clinical outcomes. Arch. Phys. Med. Rehabil. 2009, 90, 726–732. [Google Scholar] [CrossRef]
- DiMarco, A.F.; Geertman, R.T.; Tabbaa, K.; Polito, R.R.; Kowalski, K.E. Case report: Minimally invasive method to activate the expiratory muscles to restore cough. J. Spinal Cord Med. 2018, 41, 562–566. [Google Scholar] [CrossRef]
- DiMarco, A.F.; Geertman, R.T.; Tabbaa, K.; Nemunaitis, G.A.; Kowalski, K.E. Restoration of cough via spinal cord stimulation improves pulmonary function in tetraplegics. J. Spinal Cord Med. 2020, 43, 579–585. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, D.F.; Cohen, M.I.; Sica, A.L.; Zhang, H. Responses of early and late onset phrenic motoneurons to lung inflation. Respir. Physiol. 1985, 61, 69–83. [Google Scholar] [CrossRef] [PubMed]
- Sieck, G.C. Physiological effects of diaphragm muscle denervation and disuse. Clin. Chest Med. 1994, 15, 641–659. [Google Scholar] [CrossRef] [PubMed]
- DiMarco, A.F.; Kowalski, K.E. High-frequency spinal cord stimulation of inspiratory muscles in dogs: A new method of inspiratory muscle pacing. J. Appl. Physiol. 2009, 107, 662–669. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 29, 372. [Google Scholar]
- Barolat, G.; Myklebust, J.B.; Wenninger, W. Enhancement of voluntary motor function following spinal cord stimulation—Case study. Appl. Neurophysiol. 1986, 49, 307–314. [Google Scholar] [CrossRef] [PubMed]
- Boakye, M.; Ball, T.; Dietz, N.; Sharma, M.; Angeli, C.; Rejc, E.; Kirshblum, S.; Forrest, G.; Arnold, F.W.; Harkema, S. Spinal cord epidural stimulation for motor and autonomic function recovery after chronic spinal cord injury: A case series and technical note. Surg. Neurol. Int. 2023, 14, 87. [Google Scholar] [CrossRef]
- Gorgey, A.S.; Goldsmith, J.; Alazzam, A.; Trainer, R. Effects of percutaneously-implanted epidural stimulation on cardiovascular autonomic function and spasticity after complete spinal cord injury: A case report. Front. Neurosci. 2023, 17, 1112853. [Google Scholar] [CrossRef]
- Gorgey, A.S.; Trainer, R.; Sutor, T.W.; Goldsmith, J.A.; Alazzam, A.; Goetz, L.L.; Lester, D.; Lavis, T.D. A case study of percutaneous epidural stimulation to enable motor control in two men after spinal cord injury. Nat. Commun. 2023, 14, 2064. [Google Scholar] [CrossRef]
- Gupta, R.; Johnson, R.; Samadani, U. Recovery of volitional movement with epidural stimulation after “complete” spinal cord injury due to gunshot: A case report and literature review. Surg. Neurol. Int. 2023, 14, 68. [Google Scholar] [CrossRef]
- Hoover, C.; Schuerger, W.; Balser, D.; McCracken, P.; Murray, T.A.; Morse, L.; Parr, A.; Samadani, U.; Netoff, T.I.; Darrow, D.P. Neuromodulation Through Spinal Cord Stimulation Restores Ability to Voluntarily Cycle after Motor Complete Paraplegia. J. Neurotrauma, 2023; online ahead of print. [Google Scholar] [CrossRef]
- Samejima, S.; Shackleton, C.; Malik, R.N.; Cao, K.; Bohorquez, A.; Nightingale, T.E.; Sachdeva, R.; Krassioukov, A.V. Spinal Cord Stimulation Prevents Autonomic Dysreflexia in Individuals with Spinal Cord Injury: A Case Series. J. Clin. Med. 2023, 12, 2897. [Google Scholar] [CrossRef]
- Kandhari, S.; Sharma, D.; Tomar, A.K.; Matis, G.; Lavrov, I.A.; Majumdar, P. Epidural electrical spinal cord stimulation of the thoracic segments (T2–T5) facilitates respiratory function in patients with complete spinal cord injury. Respir. Physiol. Neurobiol. 2022, 300, 103885. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.C.; Angeli, C.A.; Ugiliweneza, B.; Weber, K.A., 2nd; Bert, R.J.; Negahdar, M.; Mesbah, S.; Boakye, M.; Harkema, S.J.; Rejc, E. Spinal cord imaging markers and recovery of standing with epidural stimulation in individuals with clinically motor complete spinal cord injury. Exp. Brain Res. 2022, 240, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Moshonkina, T.R.; Makarovski, A.N.; Bogacheva, I.N.; Scherbakova, N.A.; Savohin, A.A.; Gerasimenko, Y.P. Effects of spinal cord electrical stimulation in patients with vertebrospinal pathology. Bull. Exp. Biol. Med. 2012, 153, 16–20. [Google Scholar] [CrossRef]
- Lu, D.C.; Edgerton, V.R.; Modaber, M.; AuYong, N.; Morikawa, E.; Zdunowski, S.; Sarino, M.E.; Sarrafzadeh, M.; Nuwer, M.R.; Roy, R.R.; et al. Engaging Cervical Spinal Cord Networks to Reenable Volitional Control of Hand Function in Tetraplegic Patients. Neurorehabil. Neural Repair 2016, 30, 951–962. [Google Scholar] [CrossRef] [PubMed]
- Minassian, K.; Hofstoetter, U.S.; Danner, S.M.; Mayr, W.; McKay, W.B.; Tansey, K.; Dimitrijevic, M.R. Mechanisms of rhythm generation of the human lumbar spinal cord in response to tonic stimulation without and with step-related sensory feedback. Biomed. Tech. 2013, 58. [Google Scholar] [CrossRef] [PubMed]
- Katz, P.G.; Greenstein, A.; Severs, S.L.; Zampieri, T.A.; Singh Sahni, K. Effect of implanted epidural stimulator on lower urinary tract function in spinal-cord-injured patients. Eur. Urol. 1991, 20, 103–106. [Google Scholar] [PubMed]
- Beck, L.; Veith, D.; Linde, M.; Gill, M.; Calvert, J.; Grahn, P.; Garlanger, K.; Husmann, D.; Lavrov, I.; Sayenko, D.; et al. Impact of long-term epidural electrical stimulation enabled task-specific training on secondary conditions of chronic paraplegia in two humans. J. Spinal Cord Med. 2021, 44, 800–805. [Google Scholar] [CrossRef] [PubMed]
- Herrity, A.N.; Aslan, S.C.; Ugiliweneza, B.; Mohamed, A.Z.; Hubscher, C.H.; Harkema, S.J. Improvements in Bladder Function Following Activity-Based Recovery Training with Epidural Stimulation after Chronic Spinal Cord Injury. Front. Syst. Neurosci. 2021, 14, 614691. [Google Scholar] [CrossRef]
- Terson de Paleville, D.G.L.; Harkema, S.J.; Angeli, C.A. Epidural stimulation with locomotor training improves body composition in individuals with cervical or upper thoracic motor complete spinal cord injury: A series of case studies. J. Spinal Cord Med. 2019, 42, 32–38. [Google Scholar] [CrossRef]
- DiMarco, A.F.; Geertman, R.T.; Tabbaa, K.; Nemunaitis, G.A.; Kowalski, K.E. Effects of Lower Thoracic Spinal Cord Stimulation on Bowel Management in Individuals with Spinal Cord Injury. Arch. Phys. Med. Rehabil. 2021, 102, 1155–1164. [Google Scholar] [CrossRef]
- Burns, P.B.; Rohrich, R.J.; Chung, K.C. The levels of evidence and their role in evidence-based medicine. Plast. Reconstr. Surg. 2011, 128, 305–310. [Google Scholar] [CrossRef]
- Walter, M.; Lee, A.H.X.; Kavanagh, A.; Phillips, A.A.; Krassioukov, A.V. Epidural Spinal Cord Stimulation Acutely Modulates Lower Urinary Tract and Bowel Function Following Spinal Cord Injury: A Case Report. Front. Physiol. 2018, 9, 1816. [Google Scholar] [CrossRef]
- Bolash, R.; Creamer, M.; Rauck, R.; Vahedifar, P.; Calodney, A.; Fox, I.; Ozaktay, C.; Vanquathem, N. Multi-waveform Spinal Cord Stimulation with High Frequency Electromagnetic Coupled (HF-EMC) Powered Implanted Electrode Array and Receiver for the Treatment of Chronic Back and Leg Pain (SURF Study). Pain Physician 2022, 25, 67–76. [Google Scholar]
- Labaran, L.; Jain, N.; Puvanesarajah, V.; Jain, A.; Buchholz, A.L.; Hassanzadeh, H. A Retrospective Database Review of the Indications, Complications, and Incidence of Subsequent Spine Surgery in 12,297 Spinal Cord Stimulator Patients. Neuromodulation 2020, 23, 634–638. [Google Scholar] [CrossRef] [PubMed]
- Deer, T.R.; Mekhail, N.; Provenzano, D.; Pope, J.; Krames, E.; Thomson, S.; Raso, L.; Burton, A.; DeAndres, J.; Buchser, E.; et al. Neuromodulation Appropriateness Consensus Committee. The appropriate use of neurostimulation: Avoidance and treatment of complications of neurostimulation therapies for the treatment of chronic pain. Neuromodulation Appropriateness Consensus Committee. Neuromodulation 2014, 17, 571–597, discussion 597–598. [Google Scholar] [CrossRef] [PubMed]
- Herrity, A.N.; Williams, C.S.; Angeli, C.A.; Harkema, S.J.; Hubscher, C.H. Lumbosacral spinal cord epidural stimulation improves voiding function after human spinal cord injury. Sci. Rep. 2018, 8, 8688. [Google Scholar] [CrossRef] [PubMed]
- Nightingale, T.E.; Walter, M.; Williams, A.M.M.; Lam, T.; Krassioukov, A.V. Ergogenic effects of an epidural neuroprosthesis in one individual with spinal cord injury. Neurology 2019, 92, 338–340. [Google Scholar] [CrossRef] [PubMed]
- Harkema, S.J.; Legg Ditterline, B.; Wang, S.; Aslan, S.; Angeli, C.A.; Ovechkin, A.; Hirsch, G.A. Epidural Spinal Cord Stimulation Training and Sustained Recovery of Cardiovascular Function in Individuals with Chronic Cervical Spinal Cord Injury. JAMA Neurol. 2018, 75, 1569–1571. [Google Scholar] [CrossRef]
- Jiang, S.D.; Dai, L.Y.; Jiang, L.S. Osteoporosis after spinal cord injury. Osteoporos. Int. 2006, 17, 180–192, Erratum in Osteoporos. Int. 2006, 17, 1278–1281.. [Google Scholar] [CrossRef]
- Battaglino, R.A.; Lazzari, A.A.; Garshick, E.; Morse, L.R. Spinal cord injury-induced osteoporosis: Pathogenesis and emerging therapies. Curr. Osteoporos. Rep. 2012, 10, 278–285. [Google Scholar] [CrossRef]
- Jilge, B.; Minassian, K.; Rattay, F.; Pinter, M.M.; Gerstenbrand, F.; Binder, H.; Dimitrijevic, M.R. Initiating extension of the lower limbs in subjects with complete spinal cord injury by epidural lumbar cord stimulation. Exp. Brain Res. 2004, 154, 308–326. [Google Scholar] [CrossRef]
- Ganley, K.J.; Willis, W.T.; Carhart, M.R.; He, J.; Herman, R.M. Epidural spinal cord stimulation improves locomotor performance in low ASIA C, wheelchair-dependent, spinal cord-injured individuals: Insights from metabolic response. Top. Spinal Cord Inj. Rehabilit. 2005, 11, 50–63. [Google Scholar] [CrossRef]
- Minassian, K.; Persy, I.; Rattay, F.; Pinter, M.M.; Kern, H.; Dimitrijevic, M.R. Human lumbar cord circuitries can be activated by extrinsic tonic input to generate locomotor-like activity. Hum. Mov. Sci. 2007, 26, 275–295. [Google Scholar] [CrossRef]
- Danner, S.M.; Hofstoetter, U.S.; Freundl, B.; Binder, H.; Mayr, W.; Rattay, F.; Minassian, K. Human spinal locomotor control is based on flexibly organized burst generators. Brain 2015, 138 Pt 3, 577–588. [Google Scholar] [CrossRef]
- Hofstoetter, U.S.; Danner, S.M.; Freundl, B.; Binder, H.; Mayr, W.; Rattay, F.; Minassian, K. Periodic modulation of repetitively elicited monosynaptic reflexes of the human lumbosacral spinal cord. J. Neurophysiol. 2015, 114, 400–410. [Google Scholar] [CrossRef]
- Grahn, P.J.; Lavrov, I.A.; Sayenko, D.G.; Van Straaten, M.G.; Gill, M.L.; Strommen, J.A.; Calvert, J.S.; Drubach, D.I.; Beck, L.A.; Linde, M.B.; et al. Enabling Task-Specific Volitional Motor Functions via Spinal Cord Neuromodulation in a Human with Paraplegia. Mayo Clin. Proc. 2017, 92, 544–554. [Google Scholar] [CrossRef] [PubMed]
- Aslan, S.C.; Legg Ditterline, B.E.; Park, M.C.; Angeli, C.A.; Rejc, E.; Chen, Y.; Ovechkin, A.V.; Krassioukov, A.; Harkema, S.J. Epidural Spinal Cord Stimulation of Lumbosacral Networks Modulates Arterial Blood Pressure in Individuals with Spinal Cord Injury-Induced Cardiovascular Deficits. Front. Physiol. 2018, 9, 565. [Google Scholar] [CrossRef] [PubMed]
- Gill, M.L.; Linde, M.B.; Hale, R.F.; Lopez, C.; Fautsch, K.J.; Calvert, J.S.; Veith, D.D.; Beck, L.A.; Garlanger, K.L.; Sayenko, D.G.; et al. Alterations of Spinal Epidural Stimulation-Enabled Stepping by Descending Intentional Motor Commands and Proprioceptive Inputs in Humans with Spinal Cord Injury. Front. Syst. Neurosci. 2021, 14, 590231. [Google Scholar] [CrossRef] [PubMed]
- Herrity, A.N.; Aslan, S.C.; Mesbah, S.; Siu, R.; Kalvakuri, K.; Ugiliweneza, B.; Mohamed, A.; Hubscher, C.H.; Harkema, S.J. Targeting bladder function with network-specific epidural stimulation after chronic spinal cord injury. Sci. Rep. 2022, 12, 11179. [Google Scholar] [CrossRef] [PubMed]
- Kandhari, S.; Sharma, D.; Samuel, S.; Sharma, G.; Majumdar, P.; Edgerton, V.R.; Gad, P. Epidural Spinal Stimulation Enables Global Sensorimotor and Autonomic Function Recovery after Complete Paralysis: 1st Study from India. IEEE Trans. Neural Syst. Rehabil. Eng. 2022, 30, 2052–2059. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 55, i4919. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chalif, J.I.; Chavarro, V.S.; Mensah, E.; Johnston, B.; Fields, D.P.; Chalif, E.J.; Chiang, M.; Sutton, O.; Yong, R.; Trumbower, R.; et al. Epidural Spinal Cord Stimulation for Spinal Cord Injury in Humans: A Systematic Review. J. Clin. Med. 2024, 13, 1090. https://doi.org/10.3390/jcm13041090
Chalif JI, Chavarro VS, Mensah E, Johnston B, Fields DP, Chalif EJ, Chiang M, Sutton O, Yong R, Trumbower R, et al. Epidural Spinal Cord Stimulation for Spinal Cord Injury in Humans: A Systematic Review. Journal of Clinical Medicine. 2024; 13(4):1090. https://doi.org/10.3390/jcm13041090
Chicago/Turabian StyleChalif, J. I., V. S. Chavarro, E. Mensah, B. Johnston, D. P. Fields, E. J. Chalif, M. Chiang, O. Sutton, R. Yong, R. Trumbower, and et al. 2024. "Epidural Spinal Cord Stimulation for Spinal Cord Injury in Humans: A Systematic Review" Journal of Clinical Medicine 13, no. 4: 1090. https://doi.org/10.3390/jcm13041090
APA StyleChalif, J. I., Chavarro, V. S., Mensah, E., Johnston, B., Fields, D. P., Chalif, E. J., Chiang, M., Sutton, O., Yong, R., Trumbower, R., & Lu, Y. (2024). Epidural Spinal Cord Stimulation for Spinal Cord Injury in Humans: A Systematic Review. Journal of Clinical Medicine, 13(4), 1090. https://doi.org/10.3390/jcm13041090







