New Perspectives of Therapies in Osteogenesis Imperfecta—A Literature Review
Abstract
1. Introduction
1.1. History
1.2. Pathophysiology
1.3. Classification
| Type of OI | Mode of Inheritance | Mutated Genes | Clinical Characteristics |
|---|---|---|---|
| I | AD | COL1A1 COL1A2 | Mild form with increased bone fragility Non-deforming Normal stature Blue-gray sclerae Hearing-impaired |
| II | AD | COL1A1 COL1A2 | Perinatal death |
| AR | CRTAP P3H1 | Severe to lethal forms | |
| III | AD | COL1A1 COL1A2 IFITM5 | Progressive deformity |
| Mild-to-moderate form | |||
| AR | SERPINF1 (type VI in the previous classifications) | Moderate to severe form; healthy at birth; no fracture until 6 months of age | |
| CRTAP P3H1 SERPINH1 | Severe to lethal forms | ||
| WNT1 | Moderate to severe form | ||
| BMP1 | Fewer than 20 individuals were diagnosed with this mild-to-severe form; increased bone mineral density (BMD) | ||
| FKBP10 | Broad spectrum of disease includes a lethal form of OI previously classified as type IX, Kuskokwim syndrome, and Bruck syndrome | ||
| IV | AD | COL1A1 COL1A2 | Moderately deforming |
| WNT1 | Moderately severe | ||
| IFITM5 | Mild-to-moderate form | ||
| AR | FKBP10 | Progressive form, deforming | |
| SP7 | Moderate form | ||
| V | AD | IFITM5 | Moderately deforming; calcification of interosseous membranes |
1.4. Current Treatment of OI
1.4.1. Medical Management or Pharmacological Treatment
1.4.2. Orthopedic Treatment
1.5. Aim and Scope
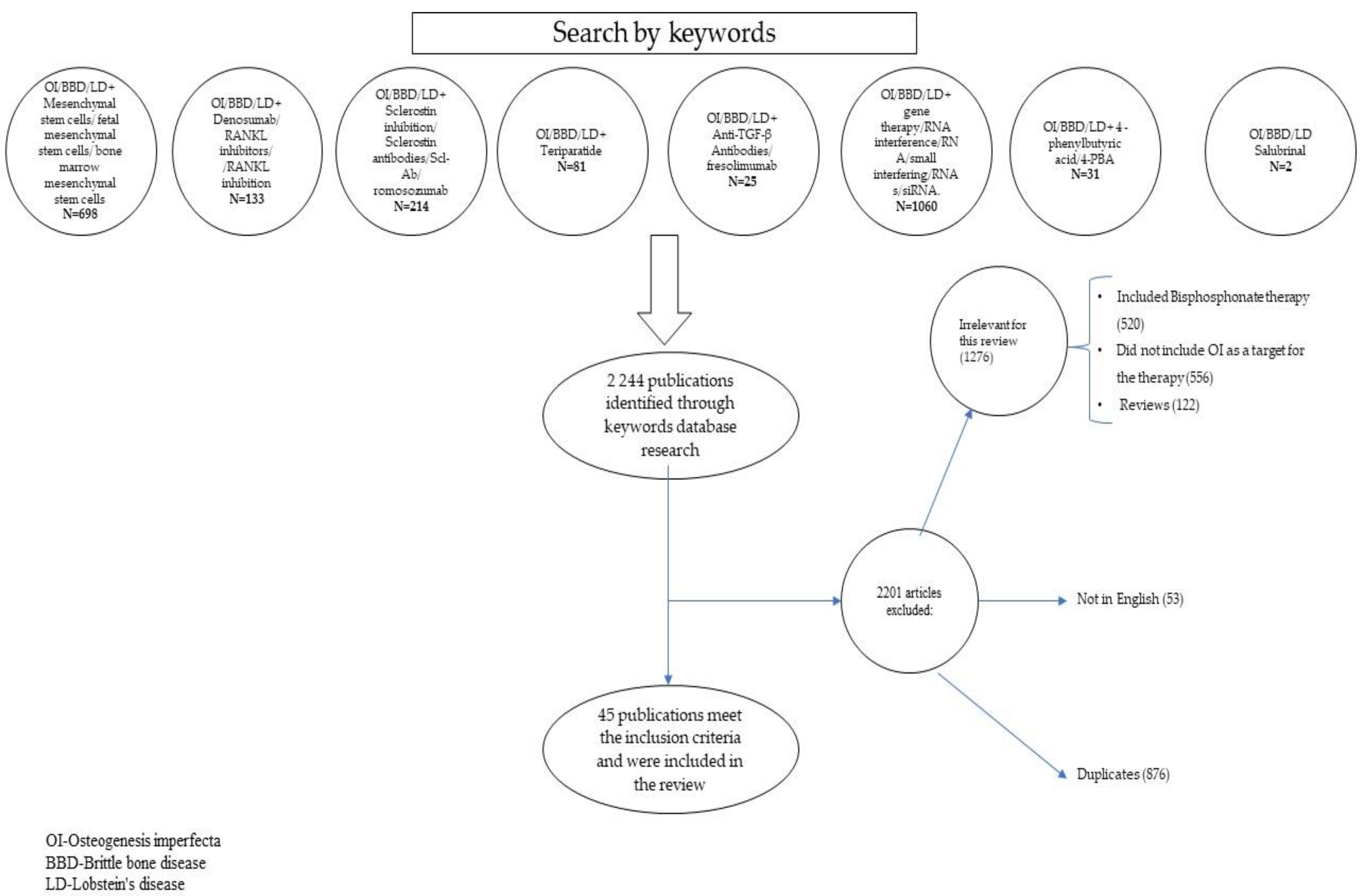
2. Materials and Methods
2.1. Search Strategies
2.2. Inclusion Criteria
2.3. Data Extraction
3. Discussions
3.1. Mesenchymal Stem Cells (MSCs) (Table 2)
3.1.1. Mechanism of Action
3.1.2. Murine Studies
3.1.3. Human Studies
Bone Marrow MSCs (BMSCs)
Fetal MSCs
| Reference | Methods | Comments |
|---|---|---|
| Horwitz et al. 1999, 2001 [31,32] | Case series: 3 children with OI type III; duration: 2 years | They enrolled 3 children with OI type III and intravenously administered BMSCs from siblings, with reported improvements in bone density and growth velocity and reduced fracture frequency in the first 3 months. Two years later, they published a follow-up study comparing the evolution of the 3 children treated with 2 control patients. The growth rate declined or reached a plateau phase in time, but the BMD continued to increase at a similar rate to healthy children. No complications were reported. |
| Götherström et al. 2005, 2013 [34,35] | Case series: 2 fetuses with OI (type III and IV); duration: 10 years and 1 year | The study included OI patients transplanted with hfMSCs pre- and postnatal:
|
| Infante et al. 2021 [33] | Clinical trial, phase 1, 2 children with OI | Two patients, a 6-year-old boy with a severe form of OI and an 8-year-old girl with a moderate form of OI, duration of 2.5 years. Both patients showed an increase in BMD and BV/TV, a decrease in fracture rates, and chronic pain. Benefits were observed after a 2-year follow-up visit after the ending of the therapy. No complications were reported. |
| Battle et al. 2021 [22] | Meta-analysis of animal studies, control trials in OI mice models of stem cell therapy period: 13 years | Ten studies were reviewed. The authors found an increase in mechanical proprieties like maximum load (p = 0.02), a decrease in fracture incidence (p < 0.00001), and a beneficial effect on structural proprieties: cortical thickness and BV/TV, but without statistical significance (p = 0.4; respectively, p = 0.31). Also, the meta-analysis had data about cell engraftment in 5 studies with poor results. |
3.2. Anti-RANKL Antibody (Table 3)
3.2.1. Mechanism of Action
3.2.2. Human Studies
| Reference | Methods | Comments |
|---|---|---|
| Semler et al. 2012 [43] | Case reports: 4 children with OI type VI (AR-SERPINF1); duration: 24 months | All of the subjects who were previously treated with bisphosphonates without response received Denosumab (1 mg/kg) every 3 months for 24 months. An increase in BMD and improvement in pain were noticed. One patient had mild hypocalcemia. |
| Hoyer-Kuhn et al. 2014 [44] | Case reports: 2 children with OI (COL1A1/A2); duration: 36 weeks | They report 2 cases of children with poor responses to bisphosphonates for 4 years, who received 1 mg/kg Denosumab every 12 weeks (1 of them received 1 dose and 1 of them 3 doses). After treatment, an increase in metaphyseal density on X-rays was reported, with no complications. |
| Ward et al. 2016 [47] | Case report: 23-month-old male patient with OI type VI; duration: 12 months | A 23-month-old male child with OI type VI, previously treated with 2 doses of Zolendronate at 4 months apart, was inefficient (the same rate of bone fractures, 3 fractures in 6 months). He received Denosumab, 1 mg/kg every 3 months for 12 months. The results were poor, the fracture rate continued to be high, and the bone sample obtained after 5 doses of treatment at 15 months showed no change in mineralization, with an increased number of osteoclasts in trabecular bone. No complications were reported. |
| Hoyer-Kuhn et al. 2016 [45] | Prospective, single-arm, phase-2 trial: 10 children with OI, 8 type I and 2 type III; duration: 48 weeks (36 weeks administration and 12 weeks follow-up) | Ten children with OI who received at least 2 years of bisphosphonate, calcium, and vitamin D were included and treated with 4 doses of Denosumab (1 mg/kg every 12 weeks). An increase in the mean height was noticed but without a significant change in the z-score (p = 0.70). Four fractures occurred during this period. The treatment did not influence bone pain (p = 0.70) or mobility (p = 0.15), but the lumbar spine bone mineral density (LS-BMD) increased from −2.23 ± 2.03 to −1.27 ± 2.37 (p = 0.0006). Two patients reported arthralgia, and 1 child reported mild hypocalcemia. |
| Uehara et al. 2017 [48] | Case reports: 3 females with OI type I, 2 adults (42 and 40 years), 1 adolescent of 14 years; duration: 30 months | All 3 patients were treated with 5 doses of Denosumab (1 dose every 6 months). The results consist of the enhancement of BMD during treatment, improved resorption markers and bone formation, and no new fractures. The adolescent had an increase in height of 2 cm during treatment. No complications were reported. |
| Trejo et al. 2018 [49] | Case reports: 4 children with OI type V; duration variable from 1.3 years to 3.5 years. | The patients with bisphosphonate treatment failure received Denosumab 1 mg/kg every 3 months.
|
| Kobayashi et al. 2018 [50] | Case series: 8 OI type I patients (5 adults, 3 children); duration: 54 months. | These patients received 60 mg of Denosumab every 6 months (from 1 to 9 doses), and calcium and cholecalciferol. The BMD generally increased in all patients and the fracture rate and bone turnover markers decreased in most of the patients. No complications were reported. |
| Maldonado et al. 2019 [51] | Case report: a 9-year-old girl with OI type IV, cerebral palsy, and epilepsy; duration: 18 months | The child had a history of treatment with Pamindronate and Zolendronate with 40 fractures. She started Denosumab (3 doses of 60 mg, a dose every 6 months) with a decrease in bone resorption and an increase in quality of life; no fracture during the Denosumab treatment time, but hypercalcemia was reported. |
| Hoyer-Kuhn et al. 2019 [46] | Prospective cohort study: 10 children with OI, 8 with type I, and 2 with type III; duration: 48 weeks treatment and 12 months follow-up | Ten children with OI received Denosumab at a mean interval of 20.33 weeks for 48 weeks (4 doses). BMDs had a significant reduction during the first follow-up year, but at the end of the follow-up, it was still higher than at the start of the trial. Vertebral shape improved further in the follow-up. Growth was not influenced, and mobility was not significantly different. As side effects, a decrease in the mean of serum calcium levels (p = 0.00039) and, for one child, symptomatic hypercalciuria with urolithiasis were reported in the first year of follow-up. |
3.3. Sclerostin Inhibition (Table 4)
3.3.1. Mechanism of Action
3.3.2. Animal Studies
3.3.3. Human Studies
| Reference | Methods | Comments |
|---|---|---|
| Sinder et al. 2013 [58] | Animal study: 8-week-old Brtl/+ mice; duration: 2 weeks | Randomized 8-week-old Brtl/+ mice and WT mice received 25 mg/kg Scl-Ab twice a week for 2 weeks. The body length was unchanged, but increased anabolic responses in the treated mice and an increase in BV/TV, cortical formation, and mechanical proprieties were reported. |
| Jacobsen et al. 2014 [59] | Animal study: 6-week-old Col1a2+/p. G610C mice, model human OI type IV; duration: 6 weeks | Randomized OI type IV 6-week-old mice models received 25 mg/kg Scl-Ab twice a week for 6 weeks. At the end of the study, a significant rise in BV/TV, BMD, and bone strength was present in the treated mice compared with the OI model controller. The bone parameters were similar to or even greater than the wild-type mice without treatment. No complications were reported. |
| Sinder et al. 2014 [60] | Animal study: 6-month-old Brtl/+ mice, model human OI type IV; duration: 5 weeks | Randomized OI type IV 6-month-old mice models received 25 mg/kg Scl-Ab twice a week for 5 weeks. An increase in bone formation rate and trabecular cortical bone mass were reported. Also, the mechanical tests and the strength and stiffness of the femoral bones increased. No complications were reported. |
| Roschger et al. 2014 [61] | Animal study: growing (4 weeks) and adult (20 weeks) Col1a1Jrt/+ mice, pediatric and adult model of severe OI; duration: 4 weeks | Growing (4 weeks) and adult (20 weeks) Col1a1Jrt/+ mice, pediatric and adult models of severe OI, received 100 mg/kg Scl-Ab once a week for 4 weeks, with no significant changes in bone formation or resorption markers but higher trabecular volume and cortical thickness in growing mice, and no changes in the adult ones. The additional cortical formation reported in younger mice was located on the endocortical surface, with a minor effect on bone resistance to bending and the mechanical testing did not reveal a positive change in both growing and old OI mice. The authors concluded that this treatment was less effective in severe OI mouse models, pediatric or adult. No complications were reported. |
| Sinder et al. 2015 [62] | Animal study: 3-week-old Brtl/+ mice, model human OI type IV; duration: 5 weeks | Randomized OI type IV 3-week-old mice models received 25 mg/kg Scl-Ab twice a week for 5 weeks, and an increase in bone formation, bone cortical mass, and improvements in mechanical strength in the models treated with Scl-Ab were noticed without complications. |
| Sinder et al. 2016 [63] | Animal study: growing (3 weeks) and adult (6 months) Brtl/+ mice, pediatric and adult model of human OI type IV; duration: 5 weeks | Growing (3 weeks) and adult (6 months) Brtl/+ mice, pediatric and adult models of human OI type IV, received 25 mg/kg Scl-Ab twice a week for 5 weeks. The collected bone samples from the right femur showed the mineral matrix enhanced in the adult model but not significantly in the pediatric one. The elastic module was not increased in any model. No complications were reported. |
| Grafe et al. 2016 [64] | Animal study: 1 and 6 weeks Crtap−/− mice, pediatric and young adult models of recessive OI; duration: 6 and 7 weeks | Crtap−/− mice models for recessive OI were treated with 25 mg/kg Scl-Ab twice a week for 6 weeks in the young adult model (6 weeks old) and for 7 weeks in the pediatric ones. The improvement in bone mass, bone formation, parameters of strength, and trabecular microarchitecture were reported, and there was a decrease in the number of osteoclasts without complications. |
| Glorieux et al. 2017 [55] | Randomized, controlled human phase 2 study: 13 adults with moderate OI completed the study. They defined moderate OI as types I, III, or IV with a history of at least two fractures. In the control group (5), 2 had OI type I, and 3 had OI type III/IV. One of them was lost to follow-up and did not receive a DXA scan in the end. They do not specify what type this subject was. In the treatment group (9), 4 of them were type I, and 5 were type III/IV; duration: 21 weeks | The treatment group received 3 doses of Scl-Ab (BPS804) (day 1: 5 mg/kg; day 15: 10 mg/kg; day 29: 20 mg/kg) and was followed for 14 weeks. The biomarkers were significantly increased, and downregulation of the bone resorption marker (CTX-1) in the study drug group was noticed, compared to the control group (44% vs. 7%). The lumbar spine BMD (LsBMD) on day 141 was increased by 4% in the Scl-Ab group compared with only a 1% increase in the reference group. No serious adverse events were reported in the BPS804 treatment group (no abnormal calcium blood levels or other laboratory test abnormalities). Three fractures in the treatment group (2 on day 2 and 1 on day 48) were present, and none in the control group. The Scl-Ab increased the BMD, reduced resorption, and stimulated bone formation, and thus, the study opens the possibility of a phase 3 trial study. |
| Cardinal et al. 2019 [65] | Animal study: 5-week-old B6C3Fe a/a-Col1a2oim/J mice, model for OI type III; duration: 9 weeks | Wild-type and old mice were treated with Scl-Ab for 9 weeks, 50 mg/kg once a week, with an increase in BMD, ultimate load, stiffness, plastic energy, and elastic modulus, and significantly reduced long bone fractures, with no complications. |
| Uehara et al. 2021 [67] | Case report: 64-year-old severe osteoporotic man with OI type I, previously treated with alendronate for 1 year, 8 years before this article; duration: 12 months | The subject received romosozumab, one dose of 210 mg monthly for 12 months, and vitamin D (eldecalcitol). The evaluation of BDM at 6 and 12 months of treatment revealed an improvement in BMD and in the turnover markers, with no fracture or other complications during the study time. |
| Wang et al. 2022 [66] | Animal study: Col1a2+/G610C.ApoE−/− mice, OI mice with Ang II infusion; duration: 4 weeks | Col1a2+/G610C.ApoE−/− mice, OI mice with AngII infusion were treated with 25 mg/kg Apc001PE twice a week for 4 weeks. This model was used to assess the cardiovascular risk Apc001PE, a Scl-Ab that targets only loop 3 of sclerostin, theorizing that the inhibition of the first 2 loops increases the cardiovascular risk. Apc001PE promoted the formation of the bone, without an increase in the cardiovascular risk. |
| Dattagupta et al. 2023 [68] | Case report: 52-year-old woman with type I OI; duration: 12 months | The patient received romosozumab, one dose of 210 mg monthly for 12 months, with improvements in BMD (10.3% in the spine and 5.4% in the right hip, p > 0.05) and no complications reported. |
3.4. Recombinant Human Parathormone
3.4.1. Mechanism of Action
3.4.2. Human Studies
3.5. Anti-Transforming Growth Factor βeta (TGF-β) Antibodies
3.5.1. Mechanism of Action
3.5.2. Human Studies
3.6. Genes Therapy (Table 5)
3.6.1. Mechanism of Action
3.6.2. Animal Studies
3.6.3. Cell Studies
| Reference | Methods | Comments |
|---|---|---|
| Wang and Marini, 1996 [81] | Cell study: fibroblasts from a patient with OI type IV (COL1A2 mutation heterozygous dominant) | The suppression of the mutant message is realized, but it was insufficient for clinical intervention (~50% suppression of the mutant chain). |
| Millington-Ward et al., 2004 [82] | Cell study: MPCs with COL1A1 heterozygous dominant mutation | The mutation is downgraded successfully (up to 85%), but the study concluded the need for allele specificity. |
| Chamberlain et al., 2004 [83] | Cell study: MSCs from 2 individuals with OI and COL1A1 heterozygous dominant mutation | The AAV-COLe1INpA gene-targeting vector was used to disrupt the exon 1 of the COL1A1 chromosome. The targeted cells showed an improvement in collagen stability, and the produced fibrils were closer to the wild-type mice, producing normal collagen. |
| Chamberlain et al., 2008 [84] | Cell study: MSCs from patients with OI heterozygous dominant COL1A2 mutation | AAV, initially targeting exon 4, was used with unsuccessful results, so by targeting exon 2, the production of abnormal proα2(I) chains was eliminated, producing normal type I procollagen. |
| Lindahl et al., 2008 [85] | Cell study: bone cells from OI heterozygous dominant COL1A2 mutation | siRNA could successfully silence COL1A2 (0.3 µg siRNA dosing, 71%; 0.45 µg, 77%; 0.6 µg, 82%) in bone cells from OI individuals. |
| Lindahl et al., 2013 [86] | Cell study: bone cells from OI heterozygous dominant COL1A1 and COL1A2 mutations | Using siRNA, the average mRNA levels from both genes were successfully significantly reduced. |
| Rousseau et al., 2013 [79] | Animal in vitro and in vivo study: Brtl OI mouse (Col1a1tm1.1 Jcm, MGI: 2158863) | With one siRNA (F-Mut) used in vivo, there was 52% suppression of the mutant allele with only 14% of the normal allele with a ~ 40% decrease in the mutant protein. |
3.7. 4-Phenylbutiric Acid (4-PBA) (Table 6)
3.7.1. Mechanism of Action
3.7.2. Animal Studies
3.7.3. Cell Studies
| Reference | Methods | Comments |
|---|---|---|
| Gioia et al. 2017 [89] | Animal study: Zebrafish larvae Chihuahua (Chi/+), model for OI. They had 6 groups of fish, 2 placebo groups (WT, Chihuahua) and 4 treated groups (WT, Chihuahua) with either 4-PBA or tauro-ursodeoxycholic acid (TUDCA); duration: 3.5 months | The authors found an enlargement of ER in fibroblasts and osteoblasts due to the mutant collagen retention. By reducing ER stress with 4-PBA, an amelioration of skeletal deformities and an increase in BMD was noticed in the treatment group with 4-PBA, so 4-PBA would be an effective treatment in OI trough reduction in ER stress. |
| Besio et al. 2018 [93] | Human cells, fibroblast from 10 patients OI type II and III (5 with mutations in COL1A1 and 5 in COL1A2); duration: 15 h | In treated cells with mutations α2-G697C and α2-G745C, a decrease in stress and apoptotic markers are observed, and an increase in general protein secretion in all treated cells. |
| Takeyari et al. 2019 [94] | Human cells: fibroblasts from 6 OI patients; duration: not specified | 4-PBA improved overglycosylation, the capability of calcification, and decreased the production of excessive collagen type I and its accumulation in fibroblasts. |
| Takeyari et al. 2021 [88] | Human cells: fibroblasts from 6 OI patients; duration: 28 days | Improvement in osteoblast mineralization reduced ER stress and normalization of the production of type I collagen was observed. |
| Duran et al. 2022 [90] | Animal study: 2-month-old Aga2+/− mice, model for moderately severe OI; duration: 5 weeks | The mice were treated with 50 mg/day 4-PBA, and a reduction in ER stress and better bone quality in vivo was noticed, with an increase in growth and bone resistance in the study’s drug group. |
| Scheiber et al. 2022 [91] | Animal study: 3-week-old OI model mice Col1a2(+/G610C) Four groups:
| The treated mice displayed a reduction in growth deficiency, an improvement in the femur length, an improvement in BV/TV, trabecular BMD, and thickness, but without an amelioration in bone fragility, with no significant effect on biomechanical proprieties. No complications were reported. |
| Daponte et al. 2023 [92] | Animal study: Zebrafish, 2 models, a dominant one (Chihuahua” (Chi/+)), and a recessive one (p3h1−/−). They had 4 groups of fish: 2 placebo groups (model WT/model Chihuahua) and 2 treatment groups (model WT/ model Chihuahua); duration: 14 days | The study was conducted on 5 groups of fish: 3 placebo groups (wild-type) and the 2 models; 2 treatment groups of the 2 models. They amputated the caudal fins and allowed them to grow back to investigate the synthesis of collagen and bone differentiation with a beneficial effect of 4-PBA in the recessive model. No complications were reported. |
3.8. Inhibition of Eukaryotic Translation Initiation Factor 2 (eIF2α) Phosphatase Enzymes (Salubrinal)
3.8.1. Mechanism of Action
3.8.2. Murine Studies
3.8.3. Human Studies
4. Limits
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Baljet, B. Aspects of the History of Osteogenesis Imperfecta (Vrolik’s Syndrome). Ann. Anat.-Anat. Anz. 2002, 184, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Marini, J.C.; Forlino, A.; Bächinger, H.P.; Bishop, N.J.; Byers, P.H.; De Paepe, A.; Fassier, F.; Fratzl-Zelman, N.; Kozloff, K.M.; Krakow, D.; et al. Osteogenesis Imperfecta. Nat. Rev. Dis. Primers 2017, 3, 17052. [Google Scholar] [CrossRef] [PubMed]
- Deguchi, M.; Tsuji, S.; Katsura, D.; Kasahara, K.; Kimura, F.; Murakami, T. Current Overview of Osteogenesis Imperfecta. Med. (B Aires) 2021, 57, 464. [Google Scholar] [CrossRef] [PubMed]
- Sillence, D.O.; Senn, A.; Danks, D.M. Genetic Heterogeneity in Osteogenesis Imperfecta. J. Med. Genet. 1979, 16, 101–116. [Google Scholar] [CrossRef] [PubMed]
- Hoyer-Kuhn, H.; Netzer, C.; Semler, O. Osteogenesis Imperfecta: Pathophysiology and Treatment. Wien. Med. Wochenschr. 2015, 165, 278–284. [Google Scholar] [CrossRef] [PubMed]
- Forlino, A.; Marini, J.C. Osteogenesis Imperfecta. Lancet 2016, 387, 1657–1671. [Google Scholar] [CrossRef]
- Botor, M.; Fus-Kujawa, A.; Uroczynska, M.; Stepien, K.L.; Galicka, A.; Gawron, K.; Sieron, A.L. Osteogenesis Imperfecta: Current and Prospective Therapies. Biomolecules 2021, 11, 1493. [Google Scholar] [CrossRef]
- Chetty, M.; Roomaney, I.A.; Beighton, P. The Evolution of the Nosology of Osteogenesis Imperfecta. Clin. Genet. 2021, 99, 42–52. [Google Scholar] [CrossRef]
- Hald, J.D.; Evangelou, E.; Langdahl, B.L.; Ralston, S.H. Bisphosphonates for the Prevention of Fractures in Osteogenesis Imperfecta: Meta-Analysis of Placebo-Controlled Trials. J. Bone Miner. Res. 2015, 30, 929–933. [Google Scholar] [CrossRef]
- Rijks, E.B.G.; Bongers, B.C.; Vlemmix, M.J.G.; Boot, A.M.; van Dijk, A.T.H.; Sakkers, R.J.B.; van Brussel, M. Efficacy and Safety of Bisphosphonate Therapy in Children with Osteogenesis Imperfecta: A Systematic Review. Horm. Res. Paediatr. 2015, 84, 26–42. [Google Scholar] [CrossRef]
- Ralston, S.H.; Gaston, M.S. Management of Osteogenesis Imperfecta. Front Endocrinol 2020, 10, 924. [Google Scholar] [CrossRef]
- Glorieux, F.H.; Bishop, N.J.; Plotkin, H.; Chabot, G.; Lanoue, G.; Travers, R. Cyclic Administration of Pamidronate in Children with Severe Osteogenesis Imperfecta. N. Engl. J. Med. 1998, 339, 947–952. [Google Scholar] [CrossRef]
- Marginean, O.; Tamasanu, R.C.; Mang, N.; Mozos, I.; Brad, G.F. Therapy with Pamidronate in Children with Osteogenesis Imperfecta. Drug Des. Dev. Ther. 2017, 11, 2507–2515. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, B.; Zambrano, M.B.; Vanz, A.P.; Brizola, E.; de Souza, L.T.; Félix, T.M. Cyclic Pamidronate Treatment for Osteogenesis Imperfecta: Report from a Brazilian Reference Center. Genet. Mol. Biol. 2019, 42, 252–260. [Google Scholar] [CrossRef] [PubMed]
- Dwan, K.; Phillipi, C.A.; Steiner, R.D.; Basel, D. Bisphosphonate Therapy for Osteogenesis Imperfecta. Cochrane Database Syst. Rev. 2016, 2016, CD005088. [Google Scholar] [CrossRef] [PubMed]
- Besio, R.; Forlino, A. New Frontiers for Dominant Osteogenesis Imperfecta Treatment: Gene/Cellular Therapy Approaches. Adv. Regen. Biol. 2015, 2, 27964. [Google Scholar] [CrossRef]
- Liu, Y.; Wu, J.; Zhu, Y.; Han, J. Therapeutic Application of Mesenchymal Stem Cells in Bone and Joint Diseases. Clin. Exp. Med. 2014, 14, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Undale, A.H.; Westendorf, J.J.; Yaszemski, M.J.; Khosla, S. Mesenchymal Stem Cells for Bone Repair and Metabolic Bone Diseases. Mayo Clin. Proc. 2009, 84, 893–902. [Google Scholar] [CrossRef] [PubMed]
- Bobis, S.; Jarocha, D.; Majka, M. Mesenchymal Stem Cells: Characteristics and Clinical Applications. Folia Histochem. Cytobiol. 2006, 44, 215–230. [Google Scholar]
- Ranzoni, A.M.; Corcelli, M.; Hau, K.-L.; Kerns, J.G.; Vanleene, M.; Shefelbine, S.; Jones, G.N.; Moschidou, D.; Dala-Ali, B.; Goodship, A.E.; et al. Counteracting Bone Fragility with Human Amniotic Mesenchymal Stem Cells. Sci. Rep. 2016, 6, 39656. [Google Scholar] [CrossRef]
- Kangari, P.; Talaei-Khozani, T.; Razeghian-Jahromi, I.; Razmkhah, M. Mesenchymal Stem Cells: Amazing Remedies for Bone and Cartilage Defects. Stem Cell Res. Ther. 2020, 11, 492. [Google Scholar] [CrossRef] [PubMed]
- Battle, L.; Yakar, S.; Carriero, A. A Systematic Review and Meta-Analysis on the Efficacy of Stem Cell Therapy on Bone Brittleness in Mouse Models of Osteogenesis Imperfecta. Bone Rep. 2021, 15, 101108. [Google Scholar] [CrossRef] [PubMed]
- Pittenger, M.F.; Discher, D.E.; Péault, B.M.; Phinney, D.G.; Hare, J.M.; Caplan, A.I. Mesenchymal Stem Cell Perspective: Cell Biology to Clinical Progress. NPJ Regen. Med. 2019, 4, 22. [Google Scholar] [CrossRef]
- Sagar, R.; Walther-Jallow, L.; David, A.L.; Götherström, C.; Westgren, M. Fetal Mesenchymal Stromal Cells: An Opportunity for Prenatal Cellular Therapy. Curr. Stem Cell Rep. 2018, 4, 61–68. [Google Scholar] [CrossRef]
- Jones, G.N.; Moschidou, D.; Abdulrazzak, H.; Kalirai, B.S.; Vanleene, M.; Osatis, S.; Shefelbine, S.J.; Horwood, N.J.; Marenzana, M.; De Coppi, P.; et al. Potential of Human Fetal Chorionic Stem Cells for the Treatment of Osteogenesis Imperfecta. Stem Cells Dev. 2014, 23, 262–276. [Google Scholar] [CrossRef]
- Guillot, P.V.; De Bari, C.; Dell’Accio, F.; Kurata, H.; Polak, J.; Fisk, N.M. Comparative Osteogenic Transcription Profiling of Various Fetal and Adult Mesenchymal Stem Cell Sources. Differentiation 2008, 76, 946–957. [Google Scholar] [CrossRef]
- Lang, E.; Semon, J.A. Mesenchymal Stem Cells in the Treatment of Osteogenesis Imperfecta. Cell Regen. 2023, 12, 7. [Google Scholar] [CrossRef] [PubMed]
- Götherström, C.; Walther-Jallow, L. Stem Cell Therapy as a Treatment for Osteogenesis Imperfecta. Curr. Osteoporos. Rep. 2020, 18, 337–343. [Google Scholar] [CrossRef]
- Niyibizi, C.; Li, F. Potential Implications of Cell Therapy for Osteogenesis Imperfecta. Int. J. Clin. Rheumtol 2009, 4, 57–66. [Google Scholar] [CrossRef]
- Guillot, P.V.; Abass, O.; Bassett, J.H.D.; Shefelbine, S.J.; Bou-Gharios, G.; Chan, J.; Kurata, H.; Williams, G.R.; Polak, J.; Fisk, N.M. Intrauterine Transplantation of Human Fetal Mesenchymal Stem Cells from First-Trimester Blood Repairs Bone and Reduces Fractures in Osteogenesis Imperfecta Mice. Blood 2008, 111, 1717–1725. [Google Scholar] [CrossRef]
- Horwitz, E.M.; Prockop, D.J.; Fitzpatrick, L.A.; Koo, W.W.K.; Gordon, P.L.; Neel, M.; Sussman, M.; Orchard, P.; Marx, J.C.; Pyeritz, R.E.; et al. Transplantability and Therapeutic Effects of Bone Marrow-Derived Mesenchymal Cells in Children with Osteogenesis Imperfecta. Nat. Med. 1999, 5, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Horwitz, E.M.; Prockop, D.J.; Gordon, P.L.; Koo, W.W.K.; Fitzpatrick, L.A.; Neel, M.D.; McCarville, M.E.; Orchard, P.J.; Pyeritz, R.E.; Brenner, M.K. Clinical Responses to Bone Marrow Transplantation in Children with Severe Osteogenesis Imperfecta. Blood 2001, 97, 1227–1231. [Google Scholar] [CrossRef] [PubMed]
- Infante, A.; Gener, B.; Vázquez, M.; Olivares, N.; Arrieta, A.; Grau, G.; Llano, I.; Madero, L.; Bueno, A.M.; Sagastizabal, B.; et al. Reiterative Infusions of MSCs Improve Pediatric Osteogenesis Imperfecta Eliciting a Pro-osteogenic Paracrine Response: TERCELOI Clinical Trial. Clin. Transl. Med. 2021, 11, e265. [Google Scholar] [CrossRef] [PubMed]
- Le Blanc, K.; Götherström, C.; Ringdén, O.; Hassan, M.; McMahon, R.; Horwitz, E.; Anneren, G.; Axelsson, O.; Nunn, J.; Ewald, U.; et al. Fetal Mesenchymal Stem-Cell Engraftment in Bone after In Utero Transplantation in a Patient with Severe Osteogenesis Imperfecta. Transplantation 2005, 79, 1607–1614. [Google Scholar] [CrossRef] [PubMed]
- Götherström, C.; Westgren, M.; Shaw, S.W.S.; Åström, E.; Biswas, A.; Byers, P.H.; Mattar, C.N.Z.; Graham, G.E.; Taslimi, J.; Ewald, U.; et al. Pre- and Postnatal Transplantation of Fetal Mesenchymal Stem Cells in Osteogenesis Imperfecta: A Two-Center Experience. Stem Cells Transl. Med. 2014, 3, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Lindgren, P.; Chitty, L.S.; David, A.; Ek, S.; Nordberg, E.A.; Goos, A.; Kublickas, M.; Oepekes, D.; Sagar, R.; Verweij, J. OC09.07: Boost Brittle Bones before Birth (BOOSTB4): A Clinical Trial of Prenatal Stem Cell Transplantation for Treatment of Osteogenesis Imperfecta. Ultrasound Obstet. Gynecol. 2022, 60, 28–29. [Google Scholar]
- Götherström, C. Karolinska Institutet Boost Brittle Bones before Birth (BOOSTB4). Available online: https://www.clinicaltrials.gov/ct2/show/NCT03706482 (accessed on 17 October 2023).
- Majdoub, F.; Ferjani, H.L.; Ben Nessib, D.; Kaffel, D.; Maatallah, K.; Hamdi, W. Denosumab Use in Osteogenesis Imperfecta: An Update on Therapeutic Approaches. Ann. Pediatr. Endocrinol. Metab. 2023, 28, 98–106. [Google Scholar] [CrossRef]
- Kendler, D.L.; Cosman, F.; Stad, R.K.; Ferrari, S. Denosumab in the Treatment of Osteoporosis: 10 Years Later: A Narrative Review. Adv. Ther. 2022, 39, 58–74. [Google Scholar] [CrossRef]
- Hildebrand, G.K.; Kasi, A. Denosumab. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Hanley, D.A.; Adachi, J.D.; Bell, A.; Brown, V. Denosumab: Mechanism of Action and Clinical Outcomes. Int. J. Clin. Pr. 2012, 66, 1139–1146. [Google Scholar] [CrossRef]
- Fili, S.; Karalaki, M.; Schaller, B. Therapeutic Implications of Osteoprotegerin. Cancer Cell Int. 2009, 9, 26. [Google Scholar] [CrossRef]
- Semler, O.; Netzer, C.; Hoyer-Kuhn, H.; Becker, J.; Eysel, P.; Schoenau, E. First Use of the RANKL Antibody Denosumab in Osteogenesis Imperfecta Type VI. J. Musculoskelet. Neuronal Interact. 2012, 12, 183–188. [Google Scholar] [PubMed]
- Hoyer-Kuhn, H.; Semler, O.; Schoenau, E. Effect of Denosumab on the Growing Skeleton in Osteogenesis Imperfecta. J. Clin. Endocrinol. Metab. 2014, 99, 3954–3955. [Google Scholar] [CrossRef] [PubMed]
- Hoyer-Kuhn, H.; Franklin, J.; Allo, G.; Kron, M.; Netzer, C.; Eysel, P.; Hero, B.; Schoenau, E.; Semler, O. Safety and Efficacy of Denosumab in Children with Osteogenesis Imperfect—A First Prospective Trial. J. Musculoskelet. Neuronal Interact. 2016, 16, 24–32. [Google Scholar] [PubMed]
- Hoyer-Kuhn, H.; Rehberg, M.; Netzer, C.; Schoenau, E.; Semler, O. Individualized Treatment with Denosumab in Children with Osteogenesis Imperfecta—Follow up of a Trial Cohort. Orphanet J. Rare Dis. 2019, 14, 219. [Google Scholar] [CrossRef] [PubMed]
- Ward, L.; Bardai, G.; Moffatt, P.; Al-Jallad, H.; Trejo, P.; Glorieux, F.H.; Rauch, F. Osteogenesis Imperfecta Type VI in Individuals from Northern Canada. Calcif. Tissue Int. 2016, 98, 566–572. [Google Scholar] [CrossRef]
- Uehara, M.; Nakamura, Y.; Takahashi, J.; Kamimura, M.; Ikegami, S.; Suzuki, T.; Uchiyama, S.; Yamaguchi, T.; Kosho, T.; Kato, H. Efficacy of Denosumab for Osteoporosis in Three Female Patients with Osteogenesis Imperfecta. Tohoku J. Exp. Med. 2017, 242, 115–120. [Google Scholar] [CrossRef]
- Trejo, P.; Rauch, F.; Ward, L. Hypercalcemia and Hypercalciuria during Denosumab Treatment in Children with Osteogenesis Imperfecta Type VI. J. Musculoskelet. Neuronal Interact. 2018, 18, 76–80. [Google Scholar] [PubMed]
- Kobayashi, T.; Nakamura, Y.; Suzuki, T.; Yamaguchi, T.; Takeda, R.; Takagi, M.; Hasegawa, T.; Kosho, T.; Kato, H. Efficacy and Safety of Denosumab Therapy for Osteogenesis Imperfecta Patients with Osteoporosis—Case Series. J. Clin. Med. 2018, 7, 479. [Google Scholar] [CrossRef]
- Maldonado, G.; Ferro, C.; Paredes, C.; Ríos, C. Use of Denosumab in Osteogenesis Imperfecta: A Case Report. Rev. Colomb. De Reumatol. (Engl. Ed.) 2019, 26, 68–73. [Google Scholar] [CrossRef]
- Wang, D.; Tang, X.; Shi, Q.; Wang, R.; Tang, X.; Guo, W. Denosumab in pediatric bone disorders and the role of RANKL blockade: A narrative review. Transl. Pediatr. 2012, 3, 470–486. [Google Scholar] [CrossRef]
- Suen, P.K.; Qin, L. Sclerostin, an Emerging Therapeutic Target for Treating Osteoporosis and Osteoporotic Fracture: A General Review. J. Orthop. Transl. 2016, 4, 1–13. [Google Scholar] [CrossRef]
- Lewiecki, E.M.; Shah, A.; Shoback, D. Sclerostin Inhibition: A Novel Therapeutic Approach In the Treatment of Osteoporosis. Int. J. Womens Health 2015, 7, 565. [Google Scholar] [CrossRef] [PubMed]
- Glorieux, F.H.; Devogelaer, J.; Durigova, M.; Goemaere, S.; Hemsley, S.; Jakob, F.; Junker, U.; Ruckle, J.; Seefried, L.; Winkle, P.J. BPS804 Anti-Sclerostin Antibody in Adults With Moderate Osteogenesis Imperfecta: Results of a Randomized Phase 2a Trial. J. Bone Miner. Res. 2017, 32, 1496–1504. [Google Scholar] [CrossRef]
- Chen, L.; Gao, G.; Shen, L.; Yue, H.; Zhang, G.; Zhang, Z. Serum Sclerostin and Its Association with Bone Turnover Marker in Metabolic Bone Diseases. Dis. Markers 2022, 2022, 7902046. [Google Scholar] [CrossRef]
- Palomo, T.; Glorieux, F.H.; Rauch, F. Circulating Sclerostin in Children and Young Adults with Heritable Bone Disorders. J. Clin. Endocrinol. Metab. 2014, 99, E920–E925. [Google Scholar] [CrossRef][Green Version]
- Sinder, B.P.; Eddy, M.M.; Ominsky, M.S.; Caird, M.S.; Marini, J.C.; Kozloff, K.M. Sclerostin Antibody Improves Skeletal Parameters in a Brtl/+ Mouse Model of Osteogenesis Imperfecta. J. Bone Miner. Res. 2013, 28, 73–80. [Google Scholar] [CrossRef]
- Jacobsen, C.M.; Barber, L.A.; Ayturk, U.M.; Roberts, H.J.; Deal, L.E.; Schwartz, M.A.; Weis, M.; Eyre, D.; Zurakowski, D.; Robling, A.G.; et al. Targeting the LRP5 Pathway Improves Bone Properties in a Mouse Model of Osteogenesis Imperfecta. J. Bone Miner. Res. 2014, 29, 2297–2306. [Google Scholar] [CrossRef] [PubMed]
- Sinder, B.P.; White, L.E.; Salemi, J.D.; Ominsky, M.S.; Caird, M.S.; Marini, J.C.; Kozloff, K.M. Adult Brtl/+ Mouse Model of Osteogenesis Imperfecta Demonstrates Anabolic Response to Sclerostin Antibody Treatment with Increased Bone Mass and Strength. Osteoporos. Int. 2014, 25, 2097–2107. [Google Scholar] [CrossRef] [PubMed]
- Roschger, A.; Roschger, P.; Keplingter, P.; Klaushofer, K.; Abdullah, S.; Kneissel, M.; Rauch, F. Effect of Sclerostin Antibody Treatment in a Mouse Model of Severe Osteogenesis Imperfecta. Bone 2014, 66, 182–188. [Google Scholar] [CrossRef]
- Sinder, B.P.; Salemi, J.D.; Ominsky, M.S.; Caird, M.S.; Marini, J.C.; Kozloff, K.M. Rapidly Growing Brtl/+ Mouse Model of Osteogenesis Imperfecta Improves Bone Mass and Strength with Sclerostin Antibody Treatment. Bone 2015, 71, 115–123. [Google Scholar] [CrossRef]
- Sinder, B.P.; Lloyd, W.R.; Salemi, J.D.; Marini, J.C.; Caird, M.S.; Morris, M.D.; Kozloff, K.M. Effect of Anti-Sclerostin Therapy and Osteogenesis Imperfecta on Tissue-Level Properties in Growing and Adult Mice While Controlling for Tissue Age. Bone 2016, 84, 222–229. [Google Scholar] [CrossRef] [PubMed]
- Grafe, I.; Alexander, S.; Yang, T.; Lietman, C.; Homan, E.P.; Munivez, E.; Chen, Y.; Jiang, M.M.; Bertin, T.; Dawson, B.; et al. Sclerostin Antibody Treatment Improves the Bone Phenotype of Crtap −/− Mice, a Model of Recessive Osteogenesis Imperfecta. J. Bone Miner. Res. 2016, 31, 1030–1040. [Google Scholar] [CrossRef] [PubMed]
- Cardinal, M.; Tys, J.; Roels, T.; Lafont, S.; Ominsky, M.S.; Devogelaer, J.-P.; Chappard, D.; Mabilleau, G.; Ammann, P.; Nyssen-Behets, C.; et al. Sclerostin Antibody Reduces Long Bone Fractures in the Oim/Oim Model of Osteogenesis Imperfecta. Bone 2019, 124, 137–147. [Google Scholar] [CrossRef]
- Wang, L.; Yu, Y.; Ni, S.; Li, D.; Liu, J.; Xie, D.; Chu, H.Y.; Ren, Q.; Zhong, C.; Zhang, N.; et al. Therapeutic Aptamer Targeting Sclerostin Loop3 for Promoting Bone Formation without Increasing Cardiovascular Risk in Osteogenesis Imperfecta Mice. Theranostics 2022, 12, 5645–5674. [Google Scholar] [CrossRef]
- Uehara, M.; Nakamura, Y.; Nakano, M.; Miyazaki, A.; Suzuki, T.; Takahashi, J. Efficacy of Romosozumab for Osteoporosis in a Patient with Osteogenesis Imperfecta: A Case Report. Mod. Rheumatol. Case Rep. 2022, 6, 128–133. [Google Scholar] [CrossRef]
- Dattagupta, A.; Petak, S. Osteoporosis Improved by Romosozumab Therapy in a Patient With Type I Osteogenesis Imperfecta. AACE Clin. Case Rep. 2023, 9, 209–212. [Google Scholar] [CrossRef]
- Vall, H.; Pamar, M. Teriparatide; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- Hauser, B.; Alonso, N.; Riches, P.L. Review of Current Real-World Experience with Teriparatide as Treatment of Osteoporosis in Different Patient Groups. J. Clin. Med. 2021, 10, 1403. [Google Scholar] [CrossRef] [PubMed]
- Orwoll, E.S.; Shapiro, J.; Veith, S.; Wang, Y.; Lapidus, J.; Vanek, C.; Reeder, J.L.; Keaveny, T.M.; Lee, D.C.; Mullins, M.A.; et al. Evaluation of Teriparatide Treatment in Adults with Osteogenesis Imperfecta. J. Clin. Investig. 2014, 124, 491–498. [Google Scholar] [CrossRef]
- Leali, P. Efficacy of Teriparatide vs Neridronate in Adults with Osteogenesis Imperfecta Type I: A Prospective Randomized International Clinical Study. Clin. Cases Miner. Bone Metab. 2017, 14, 153. [Google Scholar] [CrossRef]
- Hald, J.D.; Keerie, C.; Weir, C.J.; Javaid, M.K.; Lam, W.; Osborne, P.; Walsh, J.; Langdahl, B.L.; Ralston, S.H. Protocol of a Randomised Trial of Teriparatide Followed by Zoledronic Acid to Reduce Fracture Risk in Adults with Osteogenesis Imperfecta. BMJ Open 2023, 13, e078164. [Google Scholar] [CrossRef]
- Grafe, I.; Yang, T.; Alexander, S.; Homan, E.P.; Lietman, C.; Jiang, M.M.; Bertin, T.; Munivez, E.; Chen, Y.; Dawson, B.; et al. Excessive Transforming Growth Factor-β Signaling Is a Common Mechanism in Osteogenesis Imperfecta. Nat. Med. 2014, 20, 670–675. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Zhang, X.; Zhao, D.; Liu, B.; Wang, B.; Yu, W.; Li, J.; Yu, X.; Cao, F.; Zheng, G.; et al. TGF-β1 Promotes the Osteoinduction of Human Osteoblasts via the PI3K/AKT/MTOR/S6K1 Signalling Pathway. Mol. Med. Rep. 2019, 19, 3505–3518. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.; Chen, G.; Li, Y.-P. TGF-β and BMP Signaling in Osteoblast, Skeletal Development, and Bone Formation, Homeostasis and Disease. Bone Res. 2016, 4, 16009. [Google Scholar] [CrossRef] [PubMed]
- Song, I.-W.; Nagamani, S.C.S.; Nguyen, D.; Grafe, I.; Sutton, V.R.; Gannon, F.H.; Munivez, E.; Jiang, M.-M.; Tran, A.; Wallace, M.; et al. Targeting TGF-β for Treatment of Osteogenesis Imperfecta. J. Clin. Investig. 2022, 132, e152571. [Google Scholar] [CrossRef] [PubMed]
- Ljunggren, Ö.; Lindahl, K.; Rubin, C.-J.; Kindmark, A. Allele-Specific Gene Silencing in Osteogenesis Imperfecta. Endocr. Dev. 2011, 21, 85–90. [Google Scholar] [PubMed]
- Rousseau, J.; Gioia, R.; Layrolle, P.; Lieubeau, B.; Heymann, D.; Rossi, A.; Marini, J.C.; Trichet, V.; Forlino, A. Allele-Specific Col1a1 Silencing Reduces Mutant Collagen in Fibroblasts from Brtl Mouse, a Model for Classical Osteogenesis Imperfecta. Eur. J. Hum. Genet. 2014, 22, 667–674. [Google Scholar] [CrossRef] [PubMed]
- Schindeler, A.; Lee, L.R.; O’Donohue, A.K.; Ginn, S.L.; Munns, C.F. Curative Cell and Gene Therapy for Osteogenesis Imperfecta. J. Bone Miner. Res. 2022, 37, 826–836. [Google Scholar] [CrossRef]
- Wang, Q.; Marini, J.C. Antisense Oligodeoxynucleotides Selectively Suppress Expression of the Mutant Alpha 2(I) Collagen Allele in Type IV Osteogenesis Imperfecta Fibroblasts. A Molecular Approach to Therapeutics of Dominant Negative Disorders. J. Clin. Investig. 1996, 97, 448–454. [Google Scholar] [CrossRef]
- Millington-Ward, S.; McMahon, H.P.; Allen, D.; Tuohy, G.; Kiang, A.-S.; Palfi, A.; Kenna, P.F.; Humphries, P.; Farrar, G.J. RNAi of COL1A1 in Mesenchymal Progenitor Cells. Eur. J. Hum. Genet. 2004, 12, 864–866. [Google Scholar] [CrossRef][Green Version]
- Chamberlain, J.R.; Schwarze, U.; Wang, P.-R.; Hirata, R.K.; Hankenson, K.D.; Pace, J.M.; Underwood, R.A.; Song, K.M.; Sussman, M.; Byers, P.H.; et al. Gene Targeting in Stem Cells from Individuals with Osteogenesis Imperfecta. Science 2004, 303, 1198–1201. [Google Scholar] [CrossRef]
- Chamberlain, J.R.; Deyle, D.R.; Schwarze, U.; Wang, P.; Hirata, R.K.; Li, Y.; Byers, P.H.; Russell, D.W. Gene Targeting of Mutant COL1A2 Alleles in Mesenchymal Stem Cells From Individuals With Osteogenesis Imperfecta. Mol. Ther. 2008, 16, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Lindahl, K.; Kindmark, A.; Laxman, N.; Åström, E.; Rubin, C.-J.; Ljunggren, Ö. Allele Dependent Silencing of Collagen Type I Using Small Interfering RNAs Targeting 3′UTR Indels—A Novel Therapeutic Approach in Osteogenesis Imperfecta. Int. J. Med. Sci. 2013, 10, 1333–1343. [Google Scholar] [CrossRef] [PubMed]
- Lindahl, K.; Rubin, C.-J.; Kindmark, A.; Ljunggren, Ö. Allele Dependent Silencing of COL1A2 Using Small Interfering RNAs. Int. J. Med. Sci. 2008, 5, 361–365. [Google Scholar] [CrossRef] [PubMed]
- Kolb, P.S.; Ayaub, E.A.; Zhou, W.; Yum, V.; Dickhout, J.G.; Ask, K. The Therapeutic Effects of 4-Phenylbutyric Acid in Maintaining Proteostasis. Int. J. Biochem. Cell Biol. 2015, 61, 45–52. [Google Scholar] [CrossRef]
- Takeyari, S.; Kubota, T.; Ohata, Y.; Fujiwara, M.; Kitaoka, T.; Taga, Y.; Mizuno, K.; Ozono, K. 4-Phenylbutyric Acid Enhances the Mineralization of Osteogenesis Imperfecta IPSC-Derived Osteoblasts. J. Biol. Chem. 2021, 296, 100027. [Google Scholar] [CrossRef]
- Gioia, R.; Tonelli, F.; Ceppi, I.; Biggiogera, M.; Leikin, S.; Fisher, S.; Tenedini, E.; Yorgan, T.A.; Schinke, T.; Tian, K.; et al. The Chaperone Activity of 4PBA Ameliorates the Skeletal Phenotype of Chihuahua, a Zebrafish Model for Dominant Osteogenesis Imperfecta. Hum. Mol. Genet. 2017, 26, 2897–2911. [Google Scholar] [CrossRef]
- Duran, I.; Zieba, J.; Csukasi, F.; Martin, J.H.; Wachtell, D.; Barad, M.; Dawson, B.; Fafilek, B.; Jacobsen, C.M.; Ambrose, C.G.; et al. 4-PBA Treatment Improves Bone Phenotypes in the Aga2 Mouse Model of Osteogenesis Imperfecta. J. Bone Miner. Res. 2022, 37, 675–686. [Google Scholar] [CrossRef]
- Scheiber, A.L.; Wilkinson, K.J.; Suzuki, A.; Enomoto-Iwamoto, M.; Kaito, T.; Cheah, K.S.E.; Iwamoto, M.; Leikin, S.; Otsuru, S. 4PBA Reduces Growth Deficiency in Osteogenesis Imperfecta by Enhancing Transition of Hypertrophic Chondrocytes to Osteoblasts. JCI Insight 2022, 7, e149636. [Google Scholar] [CrossRef]
- Daponte, V.; Tonelli, F.; Masiero, C.; Syx, D.; Exbrayat-Héritier, C.; Biggiogera, M.; Willaert, A.; Rossi, A.; Coucke, P.J.; Ruggiero, F.; et al. Cell Differentiation and Matrix Organization Are Differentially Affected during Bone Formation in Osteogenesis Imperfecta Zebrafish Models with Different Genetic Defects Impacting Collagen Type I Structure. Matrix Biol. 2023, 121, 105–126. [Google Scholar] [CrossRef]
- Besio, R.; Iula, G.; Garibaldi, N.; Cipolla, L.; Sabbioneda, S.; Biggiogera, M.; Marini, J.C.; Rossi, A.; Forlino, A. 4-PBA Ameliorates Cellular Homeostasis in Fibroblasts from Osteogenesis Imperfecta Patients by Enhancing Autophagy and Stimulating Protein Secretion. Biochim. Et. Biophys. Acta (BBA)-Mol. Basis Dis. 2018, 1864, 1642–1652. [Google Scholar] [CrossRef] [PubMed]
- Takeyari, S.; Ohata, Y.; Kubota, T.; Taga, Y.; Mizuno, K.; Ozono, K. Analysis of Osteogenesis Imperfecta in Pathology and the Effects of 4-Phenylbutyric Acid Using Patient-Derived Fibroblasts and Induced Pluripotent Stem Cells. Bone Abstr. 2019, 7. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, N. Regulation of NFATc1 in Osteoclast Differentiation. J. Bone Metab. 2014, 21, 233. [Google Scholar] [CrossRef] [PubMed]
- He, L.; Lee, J.; Jang, J.H.; Sakchaisri, K.; Hwang, J.; Cha-Molstad, H.J.; Kim, K.A.; Ryoo, I.J.; Lee, H.G.; Kim, S.O.; et al. Osteoporosis Regulation by Salubrinal through EIF2α Mediated Differentiation of Osteoclast and Osteoblast. Cell Signal. 2013, 25, 552–560. [Google Scholar] [CrossRef] [PubMed]
- Hamamura, K.; Chen, A.; Tanjung, N.; Takigawa, S.; Sudo, A.; Yokota, H. In Vitro and in Silico Analysis of an Inhibitory Mechanism of Osteoclastogenesis by Salubrinal and Guanabenz. Cell Signal. 2015, 27, 353–362. [Google Scholar] [CrossRef]
- Takigawa, S.; Frondorf, B.; Liu, S.; Liu, Y.; Li, B.; Sudo, A.; Wallace, J.M.; Yokota, H.; Hamamura, K. Salubrinal Improves Mechanical Properties of the Femur in Osteogenesis Imperfecta Mice. J. Pharmacol. Sci. 2016, 132, 154–161. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dinulescu, A.; Păsărică, A.-S.; Carp, M.; Dușcă, A.; Dijmărescu, I.; Pavelescu, M.L.; Păcurar, D.; Ulici, A. New Perspectives of Therapies in Osteogenesis Imperfecta—A Literature Review. J. Clin. Med. 2024, 13, 1065. https://doi.org/10.3390/jcm13041065
Dinulescu A, Păsărică A-S, Carp M, Dușcă A, Dijmărescu I, Pavelescu ML, Păcurar D, Ulici A. New Perspectives of Therapies in Osteogenesis Imperfecta—A Literature Review. Journal of Clinical Medicine. 2024; 13(4):1065. https://doi.org/10.3390/jcm13041065
Chicago/Turabian StyleDinulescu, Alexandru, Alexandru-Sorin Păsărică, Mădălina Carp, Andrei Dușcă, Irina Dijmărescu, Mirela Luminița Pavelescu, Daniela Păcurar, and Alexandru Ulici. 2024. "New Perspectives of Therapies in Osteogenesis Imperfecta—A Literature Review" Journal of Clinical Medicine 13, no. 4: 1065. https://doi.org/10.3390/jcm13041065
APA StyleDinulescu, A., Păsărică, A.-S., Carp, M., Dușcă, A., Dijmărescu, I., Pavelescu, M. L., Păcurar, D., & Ulici, A. (2024). New Perspectives of Therapies in Osteogenesis Imperfecta—A Literature Review. Journal of Clinical Medicine, 13(4), 1065. https://doi.org/10.3390/jcm13041065







