Obesity and Dental Caries in School Children
Abstract
1. Introduction
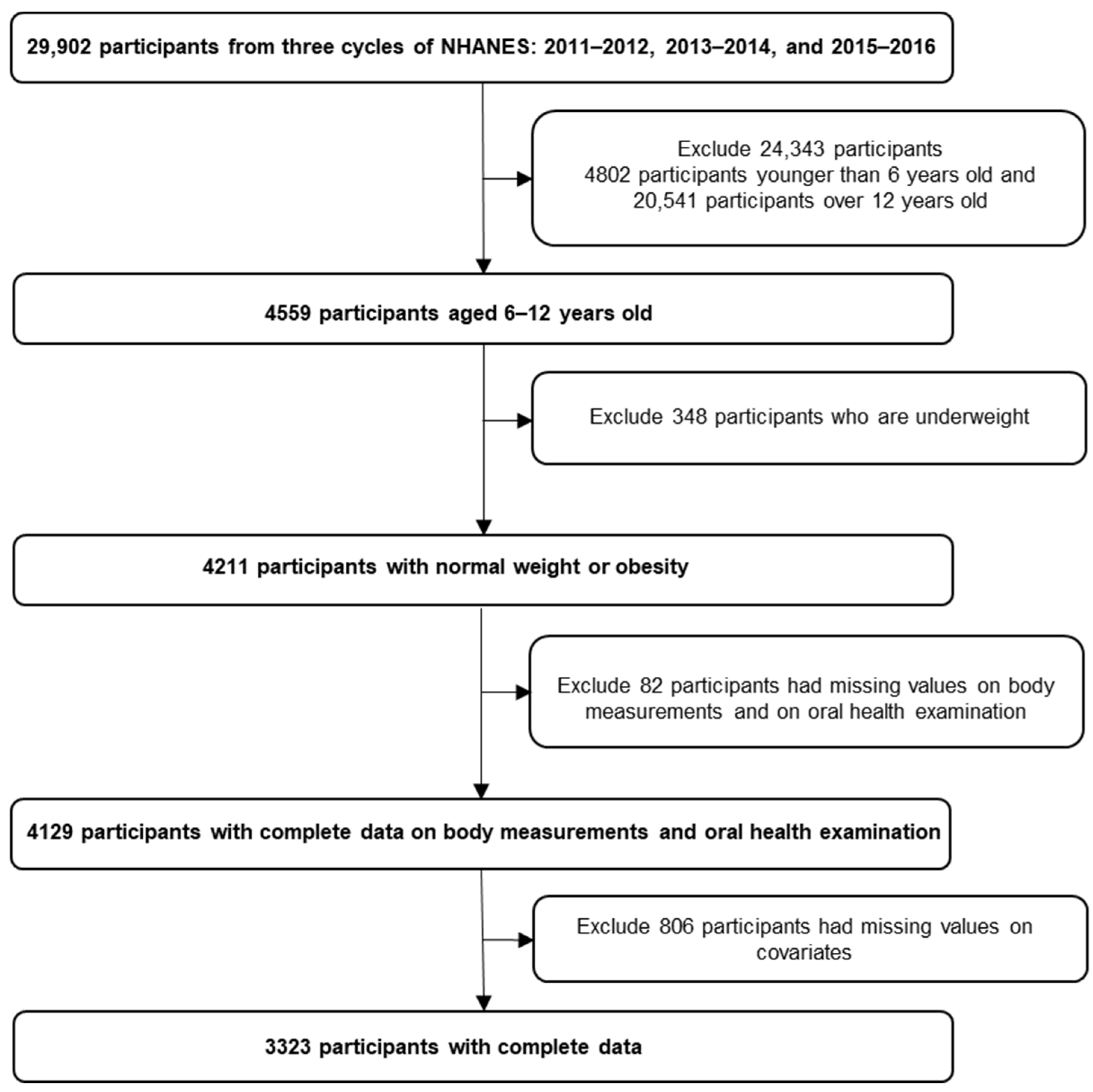
2. Materials and Methods
2.1. Data Source
2.2. Measures
2.2.1. Outcome Measure
2.2.2. Independent Variable
2.2.3. Covariates
2.2.4. Statistical Analyses
3. Results
4. Discussion
4.1. Implications
4.2. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| NHANES | National Health and Nutrition Examination Survey |
| CDC | Centers for Disease Control and Prevention |
| DMFT | decayed, missing and filled teeth |
| US | United States |
| MEC | mobile examination center |
| BMI | body mass index |
| FPED | Food Patterns Equivalent Database |
| USDA | US Department of Agriculture |
| tsp. eq. | teaspoon equivalent |
| OR | odds ratios |
| RR | rate ratios |
References
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A.; et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef]
- Tinanoff, N.; Baez, R.J.; Guillory, C.D.; Donly, K.J.; Feldens, C.A.; McGrath, C.; Phantumvanit, P.; Pitts, N.B.; Seow, W.K.; Sharkov, N.; et al. Early childhood caries epidemiology, aetiology, risk assessment, societal burden, management, education, and policy: Global perspective. Int. J. Paediatr. Dent. 2019, 29, 238–248. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Obesity and Overweight. 9 June 2021. Available online: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (accessed on 12 September 2023).
- Centers for Disease Control and Prevention. Obesity. 10 August 2022. Available online: https://www.cdc.gov/healthyschools/obesity/index.htm#print (accessed on 12 September 2023).
- Centers for Disease Control and Prevention. Prevalence of Total and Untreated Dental Caries Among Youth: United States, 2015–2016. 25 July 2018. Available online: https://www.cdc.gov/nchs/products/databriefs/db307.htm#:~:text=For%202015%E2%80%932016%2C%20prevalence%20of (accessed on 12 September 2023).
- Dye, B.; Gina, M.; Xianfen, M.; Iafolla, T. Dental Caries and Sealant Prevalence in Children and Adolescents in the United States, 2011–2012 Key Findings. NCHS. Data Brief. 2015, 191, 1–8. [Google Scholar]
- Chen, D.; Zhi, Q.; Zhou, Y.; Tao, Y.; Wu, L.; Lin, H. Association between Dental Caries and BMI in Children: A Systematic Review and Meta-Analysis. Caries Res. 2018, 52, 230–245. [Google Scholar] [CrossRef] [PubMed]
- Paisi, M.; Kay, E.; Bennett, C.; Kaimi, I.; Witton, R.; Nelder, R.; Lapthorne, D. Body mass index and dental caries in young people: A systematic review. BMC Pediatr. 2019, 19, 122. [Google Scholar] [CrossRef] [PubMed]
- Manohar, N.; Hayen, A.; Fahey, P.; Arora, A. Obesity and dental caries in early childhood: A systematic review and meta-analyses. Obes. Rev. 2019, 21, e12960. [Google Scholar] [CrossRef]
- Alotaibi, W.M.; Habbal, N.H.; Alghamdi, S.A.; Alanazi, M.O.; Alblowi, S.S.; Alijohani, A.M.; Aljohani, R.M. Dental Caries in Relation to Obesity in Children: A Systematic Review and Meta-analysis. Ann. Med. Health Sci. Res. 2020, 10, 1029–1033. [Google Scholar]
- Issrani, R.; Reddy, J.; Bader, A.K.; Albalawi, R.F.H.; Alserhani, E.D.M.; Alruwaili, D.S.R.; Alanazi, G.R.A.; Alruwaili, N.S.R.; Sghaireen, M.G.; Rao, K. Exploring an Association between Body Mass Index and Oral Health—A Scoping Review. Diagnostics 2023, 13, 902. [Google Scholar] [CrossRef]
- Ben-Assuli, O.; Bar, O.; Geva, G.; Siri, S.; Tzur, D.; Almoznino, G. Body Mass Index and Caries: Machine Learning and Statistical Analytics of the Dental, Oral, Medical Epidemiological (DOME) Nationwide Big Data Study. Metabolites 2023, 13, 37. [Google Scholar] [CrossRef]
- Ramirez, I.; Alves, D.E.; Kuchler, P.C.; Madalena, I.R.; Lima, D.C.d.; Barbosa, M.C.F.; Oliveira, M.A.H.d.M.; Thedei Júnior, G.; Baratto-Filho, F.; Küchler, E.C.; et al. Geographic Information Systems (GIS) to Assess Dental Caries, Overweight and Obesity in Schoolchildren in the City of Alfenas, Brazil. Int. J. Environ. Res. Public Health 2023, 20, 2443. [Google Scholar] [CrossRef]
- Marshall, T.A.; Eichenberger-Gilmore, J.M.; Broffitt, B.A.; Warren, J.J.; Levy, S.M. Dental caries and childhood obesity: Roles of diet and socioeconomic status. Community Dent. Oral Epidemiol. 2007, 35, 449–458. [Google Scholar] [CrossRef] [PubMed]
- Coker, M.O.; Lebeaux, R.M.; Hoen, A.G.; Moroishi, Y.; Gilbert-Diamond, D.; Dade, E.F.; Palys, T.J.; Madan, J.C.; Karagas, M.R. Metagenomic analysis reveals associations between salivary microbiota and body composition in early childhood. Sci. Rep. 2022, 12, 13075. [Google Scholar] [CrossRef] [PubMed]
- Hatipoglu, O.; Maras, E.; Hatipoglu, F.; Saygin, A. Salivary flow rate, pH, and buffer capacity in the individuals with obesity and overweight; A meta-analysis. Niger. J. Clin. Pract. 2022, 25, 1126. [Google Scholar] [CrossRef] [PubMed]
- Leme, L.A.F.P.; Rizzardi, K.F.; Santos, I.B.; Parisotto, T.M. Exploring the Relationship between Salivary Levels of TNF-α, Lactobacillus acidophilus, Lactobacillus gasseri, Obesity, and Caries in Early Childhood. Pathogens 2022, 11, 579. [Google Scholar] [CrossRef] [PubMed]
- Von Philipsborn, P.; Stratil, J.M.; Burns, J.; Busert, L.K.; Pfadenhauer, L.M.; Polus, S.; Hozapfel, C.; Hauner, H.; Rehfuess, E. Environmental interventions to reduce the consumption of sugar-sweetened beverages and their effects on health. Cochrane Database Syst. Rev. 2019, 6, CD012292. [Google Scholar] [CrossRef] [PubMed]
- National Center for Health Statistics. NCHS Ethics Review Board (ERB) Approval. 24 August 2022. Available online: https://www.cdc.gov/nchs/nhanes/irba98.htm (accessed on 5 January 2024).
- National Center for Health Statistics. NHANES Response Rates and Population Totals. Centers for Disease Control. Available online: https://wwwn.cdc.gov/nchs/nhanes/responserates.aspx#population-totals (accessed on 23 May 2023).
- National Center for Health Statistics. National Health and Nutrition Examination Survey. Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/nchs/nhanes/ (accessed on 24 May 2023).
- Muswell Hill Smile. The Transition between the Primary and Permanent Teeth. Available online: https://muswellhillsmile.co.uk/blog/transition-between-primary-and-permanent-teeth/#:~:text=Between%206%2D8%20years%20of%20to%20replace%20their%20deciduous%20predecessors (accessed on 5 January 2024).
- National Health and Nutrition Examination Survey. Oral Health Examiners Manual. Centers for Disease Control and Prevention. January 2020. Available online: www.cdc.gov/nchs/data/nhanes/2019-2020/manuals/2020-Oral-Health-Examiners-Manual-508.pdf (accessed on 24 May 2023).
- National Health and Nutrition Examination Survey. Anthropometry Procedures Manual. Centers for Disease Control and Prevention. May 2021. Available online: https://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf (accessed on 24 May 2023).
- Centers for Disease Control and Prevention. Healthy Weight, Nutrition, and Physical Activity. About Child & Teen BMI. Available online: https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html (accessed on 24 May 2023).
- Ahluwalia, N.; Dwyer, J.; Terry, A.; Moshfegh, A.; Johnson, C. Update on NHANES Dietary Data: Focus on Collection, Release, Analytical Considerations, and Uses to Inform Public Policy. Adv. Nutr. 2016, 7, 121–134. [Google Scholar] [CrossRef] [PubMed]
- USDA. Food Patterns Equivalents Database. Available online: https://www.ars.usda.gov/northeast-area/beltsville-md-bhnrc/beltsville-human-nutrition-research-center/food-surveys-research-group/docs/fped-overview/ (accessed on 24 May 2023).
- Rogers, R.; Eagle, T.F.; Sheetz, A.; Woodward, A.; Leibowitz, R.; Song, M.; Sylvester, R.; Corriveau, N.; Kline-Rogers, E.; Jiang, Q.; et al. The Relationship between Childhood Obesity, Low Socioeconomic Status, and Race/Ethnicity: Lessons from Massachusetts. Child. Obes. 2015, 11, 691–695. [Google Scholar] [CrossRef]
- Whitaker, R.C.; Orzol, S.M. Obesity Among US Urban Preschool Children. Arch. Pediat. Adolesc. Med. 2006, 160, 578. [Google Scholar] [CrossRef]
- Martinez-Mier, E.A.; Zandona, A.F. The Impact of Gender on Caries Prevalence and Risk Assessment. Dent. Clin. N. Am. 2013, 57, 301–315. [Google Scholar] [CrossRef]
- Bowman, S. Added sugars: Definition and estimation in the USDA Food Patterns Equivalents Databases. J. Food Compos. Anal. 2017, 64, 64–67. [Google Scholar] [CrossRef]
- Yang, F.; Zhang, Y.; Yuan, X.; Yu, J.; Chen, S.; Chen, Z.; Guo, D.; Cai, J.; Ma, N.; Guo, E. Caries experience and its association with weight status among 8-year-old children in Qingdao, China. J. Int. Soc. Prev. Community Dent. 2015, 5, 52–58. [Google Scholar] [CrossRef]
- Farsi, D.J.; Elkhodary, H.M.; Merdad, L.A.; Farsi, N.M.; Alaki, S.M.; Alamoudi, N.M.; Bakhaidar, H.A.; Alolayyan, M.A. Prevalence of obesity in elementary school children and its association with dental caries. Saudi Med. J. 2016, 37, 1387–1394. [Google Scholar] [CrossRef]
- Juarez-Lopez, M.L.A.; Villa-Ramos, A. Caries prevalence in preschool children with overweight and obesity. Rev. Investig. Clínica 2010, 62, 115–120. [Google Scholar]
- Ravaghi, V.; Rezaee, A.; Pallan, M.; Morris, A.J. Childhood obesity and dental caries: An ecological investigation of the shape and moderators of the association. BMC Oral Health 2020, 20, 338. [Google Scholar] [CrossRef] [PubMed]
- D’Mello, G.; Chia, L.; Hamilton, S.D.; Thomson, W.M.; Drummon, B.K. Childhood obesity and dental caries among pediatric dental clinic attenders. Int. J. Paediatr. Dent. 2011, 21, 217–222. [Google Scholar] [CrossRef] [PubMed]
- Burkhauser, R.; Cawley, J. Beyond BMI: The value of more accurate measures of fatness and obesity in social science research. J. Health Econ. 2008, 27, 519–529. [Google Scholar] [CrossRef]
| n (%) | Untreated Caries | DMFT | |||
|---|---|---|---|---|---|
| n (%) | p-Value * | Mean (SD) | p-Value | ||
| Total | 3323 (100) | 6 37 (19.2) | NA | 1.69 (2.61) | NA |
| Sex | |||||
| Boys | 1682 (50.6) | 341 (20.3) | 0.07 | 1.81 (2.72) | 0.02 a |
| Girls | 1641 (49.4) | 296 (18.0) | 1.57 (2.49) | ||
| Race and ethnicity | |||||
| Mexican American | 691 (20.8) | 164 (23.7) | <0.001 | 2.14 (2.92) | <0.001 b |
| Non-Hispanic Asian | 249 (7.5) | 48 (19.3) | 1.78 (2.65) | ||
| Non-Hispanic Black | 865 (26.0) | 180 (20.8) | 1.74 (2.59) | ||
| Non-Hispanic White | 912 (27.4) | 142 (15.6) | 1.38 (2.39) | ||
| Other Race 1 | 214 (6.4) | 28 (13.1) | 1.35 (2.40) | ||
| Other Hispanic | 392 (11.8) | 75 (19.1) | 1.62 (2.53) | ||
| Ratio of family income to poverty | |||||
| ≤1 | 1136 (34.2) | 276 (24.3) | <0.001 | 2.12 (2.81) | <0.001 a |
| >1 | 2187 (65.8) | 361 (16.5) | 1.46 (2.47) | ||
| Child intake of added sugars | |||||
| Q1 | 829 (24.9) | 155 (18.7) | 0.91 | 1.49 (2.40) | 0.02 b |
| Q2 | 829 (24.9) | 161 (19.4) | 1.73 (2.74) | ||
| Q3 | 831 (25.0) | 166 (20.0) | 1.60 (2.44) | ||
| Q4 | 834 (25.1) | 155 (18.6) | 1.93 (2.82) | ||
| n (%) | Obesity | ||
|---|---|---|---|
| n (%) | p-Value * | ||
| Total | 3323 (100) | 1270 (38.2) | NA |
| Sex | |||
| Boys | 1682 (50.6) | 632 (37.6) | 0.87 |
| Girls | 1641 (49.4) | 638 (38.9) | |
| Race and ethnicity | |||
| Mexican American | 691 (20.8) | 336 (48.6) | <0.001 |
| Non-Hispanic Asian | 249 (7.5) | 61 (24.5) | |
| Non-Hispanic Black | 865 (26.0) | 328 (37.9) | |
| Non-Hispanic White | 912 (27.4) | 294 (32.2) | |
| Other Race | 214 (6.4) | 78 (36.4) | |
| Other Hispanic | 392 (11.8) | 173 (44.1) | |
| Ratio of family income to poverty | |||
| ≤1 | 1136 (34.2) | 468 (41.2) | <0.001 |
| >1 | 2187 (65.8) | 802 (36.7) | |
| Child intake of added sugars | |||
| Q1 | 829 (24.9) | 337 (40.7) | 0.59 |
| Q2 | 829 (24.9) | 306 (36.9) | |
| Q3 | 831 (25.0) | 319 (38.4) | |
| Q4 | 834 (25.1) | 308 (36.9) | |
| n (%) | Model 1 1 | Model 2 2 | Model 3 3 | |
|---|---|---|---|---|
| OR [95% CI] | OR [95% CI] | OR [95% CI] | ||
| Untreated Caries | ||||
| Normal | 375 (58.9) | Reference | Reference | Reference |
| Obese | 262 (41.1) | 1.163 [0.975, 1.387] | 1.128 [0.943, 1.350] | 1.125 [0.939, 1.347] |
| Caries Experience | RR [95% CI] | RR [95% CI] | RR [95% CI] | |
| Normal | N/A | Reference | Reference | Reference |
| Obese | N/A | 0.919 [0.765–1.103] | 0.899 [0.749–1.080] | 0.899 [0.749–1.078] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohajeri, A.; Berg, G.; Watts, A.; Cheever, V.J.; Hung, M. Obesity and Dental Caries in School Children. J. Clin. Med. 2024, 13, 860. https://doi.org/10.3390/jcm13030860
Mohajeri A, Berg G, Watts A, Cheever VJ, Hung M. Obesity and Dental Caries in School Children. Journal of Clinical Medicine. 2024; 13(3):860. https://doi.org/10.3390/jcm13030860
Chicago/Turabian StyleMohajeri, Amir, Gabrielle Berg, April Watts, Val Joseph Cheever, and Man Hung. 2024. "Obesity and Dental Caries in School Children" Journal of Clinical Medicine 13, no. 3: 860. https://doi.org/10.3390/jcm13030860
APA StyleMohajeri, A., Berg, G., Watts, A., Cheever, V. J., & Hung, M. (2024). Obesity and Dental Caries in School Children. Journal of Clinical Medicine, 13(3), 860. https://doi.org/10.3390/jcm13030860








