Headache Attributed to Refractive Error: Improvement after Topography-Guided Photorefractive Keratectomy with Corneal Cross-Linking in Patients with Keratoconus
Abstract
1. Introduction
2. Methods
3. Results
3.1. Preoperative Characteristics of Headache and Non-Headache Groups
3.2. Postoperative Characteristics of Headache and Non-Headache Groups
3.3. Differences in Headache Diagnosis, Characteristics, and Treatment after Surgery
3.3.1. Headache Diagnosis According to IHS Criteria
3.3.2. Headache Days and Duration
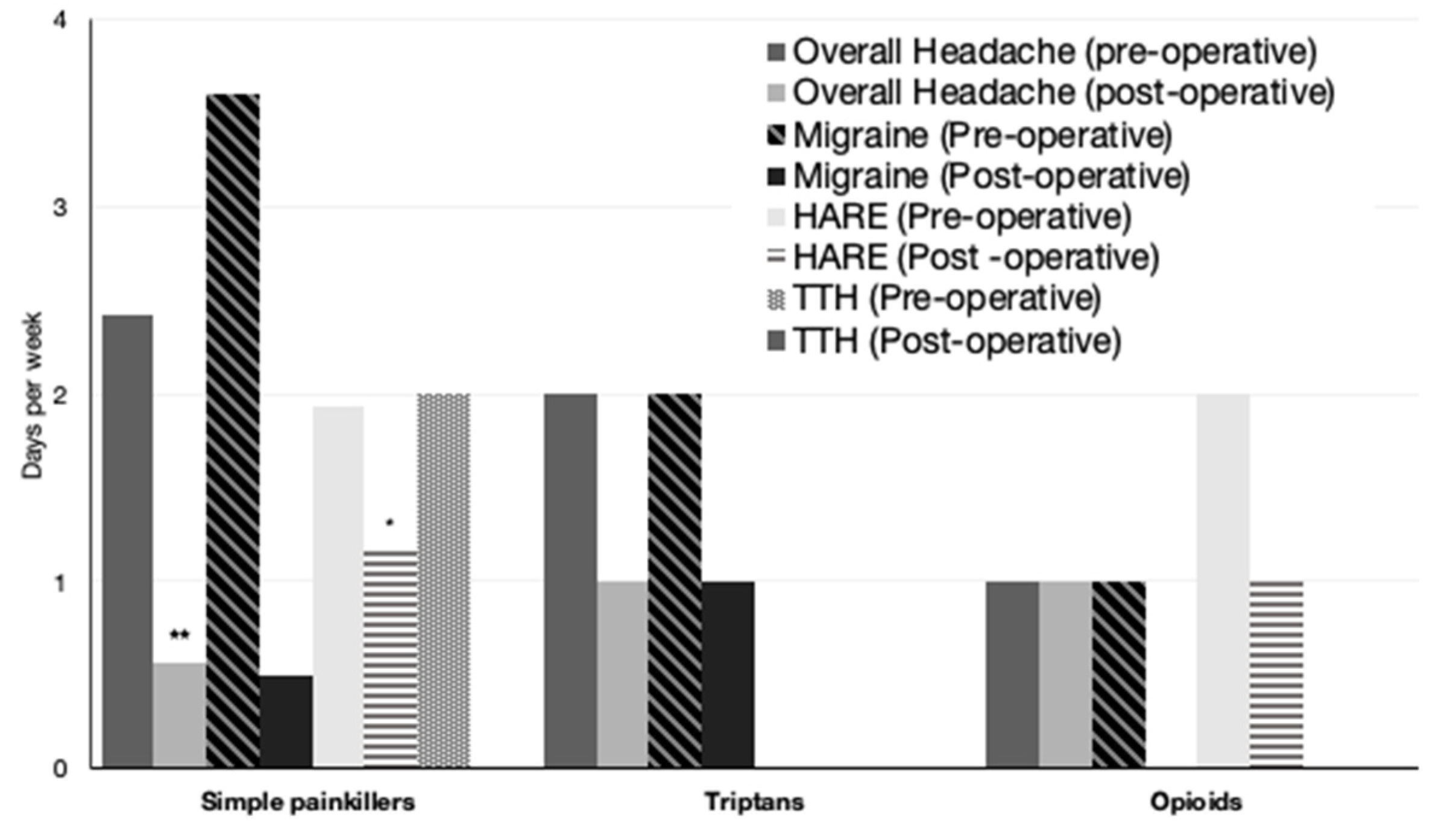
3.3.3. Analgesia Use
3.3.4. Headache Impact and HIT-6 Score
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
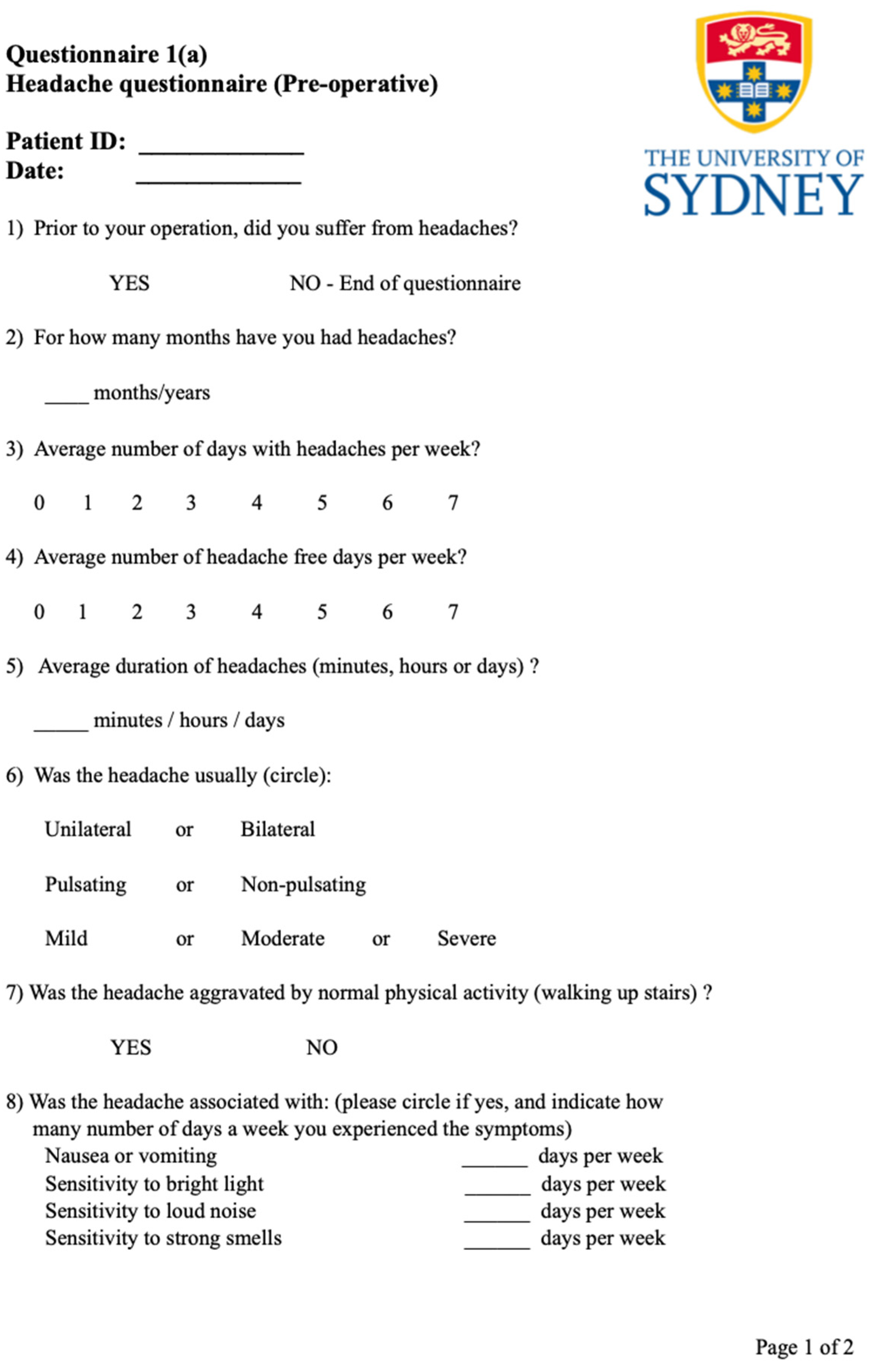
Appendix A. Headache Questionnaire Devised with the Expert Advice of Our Headache Advisor, a Neurology Consultant
References
- Stovner, L.J.; Hagen, K.; Linde, M.; Steiner, T.J. The global prevalence of headache: An update, with analysis of the influences of methodological factors on prevalence estimates. J. Headache Pain 2022, 23, 34. [Google Scholar] [CrossRef]
- Burch, R.; Rizzoli, P.; Loder, E. The prevalence and impact of migraine and severe headache in the United States: Updated age, sex, and socioeconomic-specific estimates from government health surveys. Headache 2021, 61, 60–68. [Google Scholar] [CrossRef]
- Saylor, D.; Steiner, T.J. The Global Burden of Headache. Semin. Neurol. 2018, 38, 182–190. [Google Scholar] [CrossRef]
- Tassorelli, C.; Diener, H.-C.; Dodick, D.W.; Silberstein, S.D.; Lipton, R.B.; Ashina, M.; Becker, W.J.; Ferrari, M.D.; Goadsby, P.J.; Pozo-Rosich, P.; et al. Guidelines of the International Headache Society for controlled trials of preventive treatment of chronic migraine in adults. Cephalalgia 2018, 38, 815–832. [Google Scholar] [CrossRef]
- Pearce, J.M. Historical aspects of migraine. J. Neurol. Neurosurg. Psychiatry 1986, 49, 1097–1103. [Google Scholar] [CrossRef]
- Eckhardt, L.; McLean, J.; Goodell, H. Experimental studies on headache: The genesis of pain from the eye. Proc. Assoc. Res. Nerv. Ment. 1943, 23, 209–227. [Google Scholar]
- Lajmi, H.; Choura, R.; Ben Achour, B.; Doukh, M.; Amin, Z.; Hmaied, W. Headache associated with refractive errors: Characteristics and risk factors. Rev. Neurol. 2021, 177, 947–954. [Google Scholar] [CrossRef]
- Gil-Gouveia, R.; Martins, I.P. Headaches associated with refractive errors: Myth or reality? Headache 2002, 42, 256–262. [Google Scholar] [CrossRef]
- Akinci, A.; Güven, A.; Degerliyurt, A.; Kibar, E.; Mutlu, M.; Citirik, M. The correlation between headache and refractive errors. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2008, 12, 290–293. [Google Scholar] [CrossRef]
- Gordon, G.E.; Chronicle, E.P.; Rolan, P. Why do we still not know whether refractive error causes headaches? Towards a framework for evidence based practice. Ophthalmic Physiol. Opt. 2001, 21, 45–50. [Google Scholar] [CrossRef]
- Griffith, A. The Eyes as a Cause of Headache. Br. Med. J. 1934, 2, 296–297. [Google Scholar] [CrossRef]
- Bearden, W.H.; Anderson, R.L. Corrugator superciliaris muscle excision for tension and migraine headaches. Ophthal. Plast. Reconstr. Surg. 2005, 21, 418–422. [Google Scholar] [CrossRef]
- Panella, N.J.; Wallin, J.L.; Goldman, N.D. Patient outcomes, satisfaction, and improvement in headaches after endoscopic brow-lift. JAMA Facial Plast. Surg. 2013, 15, 263–267. [Google Scholar] [CrossRef]
- Sahebjada, S.; Al-Mahrouqi, H.H.; Moshegov, S.; Panchatcharam, S.M.; Chan, E.; Daniell, M.; Baird, P.N. Eye rubbing in the aetiology of keratoconus: A systematic review and meta-analysis. Graefe’s Arch. Clin. Exp. Ophthalmol. 2021, 259, 2057–2067. [Google Scholar] [CrossRef]
- Mazharian, A.; Panthier, C.; Courtin, R.; Jung, C.; Rampat, R.; Saad, A.; Gatinel, D. Incorrect sleeping position and eye rubbing in patients with unilateral or highly asymmetric keratoconus: A case-control study. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 258, 2431–2439. [Google Scholar] [CrossRef] [PubMed]
- Mohammadpour, M.; Heidari, Z.; Hashemi, H. Updates on Managements for Keratoconus. J. Curr. Ophthalmol. 2018, 30, 110–124. [Google Scholar] [CrossRef]
- Jinabhai, A.; Radhakrishnan, H.; Tromans, C.; O’Donnell, C. Visual performance and optical quality with soft lenses in keratoconus patients. Ophthalmic Physiol. Opt. 2012, 32, 100–116. [Google Scholar] [CrossRef]
- Metlapally, S.; Bharadwaj, S.R.; Roorda, A.; Nilagiri, V.K.; Yu, T.T.; Schor, C.M. Binocular cross-correlation analyses of the effects of high-order aberrations on the stereoacuity of eyes with keratoconus. J. Vis. 2019, 19, 12. [Google Scholar] [CrossRef]
- Kymionis, G.D.; Kontadakis, G.A.; Kounis, G.A.; Portaliou, D.M.; Karavitaki, A.E.; Magarakis, M.; Yoo, S.; Pallikaris, I.G. Simultaneous topography-guided PRK followed by corneal collagen cross-linking for keratoconus. J. Refract. Surg. 2009, 25, S807-11. [Google Scholar] [CrossRef]
- Deshmukh, R.; Ong, Z.Z.; Rampat, R.; Alió Del Barrio, J.L.; Barua, A.; Ang, M.; Mehta, J.S.; Said, D.G.; Dua, H.S.; Ambrósio, R.; et al. Management of keratoconus: An updated review. Front. Med. 2023, 10, 1212314. [Google Scholar] [CrossRef]
- Al-Mohaimeed, M.M. Combined corneal CXL and photorefractive keratectomy for treatment of keratoconus: A review. Int. J. Ophthalmol. 2019, 12, 1929–1938. [Google Scholar] [CrossRef]
- D’Oria, F.; Bagaglia, S.A.; Alio del Barrio, J.L.; Alessio, G.; Alio, J.L.; Mazzotta, C. Refractive surgical correction and treatment of keratoconus. Surv. Ophthalmol. 2024, 69, 122–139. [Google Scholar] [CrossRef]
- Houts, C.R.; McGinley, J.S.; Wirth, R.J.; Cady, R.; Lipton, R.B. Reliability and validity of the 6-item Headache Impact Test in chronic migraine from the PROMISE-2 study. Qual. Life Res. 2021, 30, 931–943. [Google Scholar] [CrossRef] [PubMed]
- Yang, M.; Rendas-Baum, R.; Varon, S.F.; Kosinski, M. Validation of the Headache Impact Test (HIT-6TM) across episodic and chronic migraine. Cephalalgia 2011, 31, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Gunes, A.; Demirci, S.; Tok, L.; Tok, O.; Koyuncuoglu, H.; Yurekli, V.A. Refractive Errors in Patients with Migraine Headache. Semin. Ophthalmol. 2014, 31, 492–494. [Google Scholar] [CrossRef] [PubMed]
- Hendricks, T.J.W.; De Brabander, J.; Van der Horst, F.G.; Hendrikse, F.; Knottnerus, J.A. Relationship Between Habitual Refractive Errors and Headache Complaints in Schoolchildren. Optom. Vis. Sci. 2007, 84, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Harle, D.E.; Evans, B.J.W. The correlation between migraine headache and refractive errors. Optom. Vis. Sci. 2006, 83, 82–87. [Google Scholar] [CrossRef] [PubMed]
- Holopainen, J.M.; Vuori, E.; Tervo, T.M.T.; Soinila, S. Relief of migraine following refractive surgery for anisometropia. J. Neurol. 2005, 252, 998–999. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, B.S.; Stewart, W.F.; Lipton, R.B. Lost workdays and decreased work effectiveness associated with headache in the workplace. J. Occup. Environ. Med. 1997, 39, 320–327. [Google Scholar] [CrossRef]
- Begasse de Dhaem, O.; Sakai, F. Migraine in the workplace. eNeurologicalSci 2022, 27, 100408. [Google Scholar] [CrossRef]
- Patel, U.K.; Malik, P.; Shah, D.; Sharma, A.; Bhela, J.; Chauhan, B.; Patel, D.; Khan, N.; Kapoor, A.; Kavi, T. The Opioid Epidemic and Primary Headache Disorders: A Nationwide Population-Based Study. Cureus 2020, 12, e9743. [Google Scholar] [CrossRef] [PubMed]

| Preoperative Refractive Errors | Overall Headache (n = 24) | Migraine (n = 5) | HARE (n = 14) | TTH (n = 5) | Non-Headache (n = 16) | p Value (Overall Headache vs. Non-Headache) |
|---|---|---|---|---|---|---|
| Myopia | ||||||
| Mild (−0.5 to −3.0 D) | 7 (29.2%) | 2 (40%) | 3 (21.4%) | 2 (40%) | 8 (50%) | 0.092 |
| Moderate (−3.0 to −6.0 D) | 11 (45.8%) | 1 (20%) | 5 (35.7%) | 1 (20%) | 3 (18.8%) | 0.039 |
| Severe (>6.0 D) | 6 (25%) | 2 (40%) | 4 (28.6%) | 2 (40%) | 5 (31.3%) | 0.667 |
| Astigmatism | ||||||
| Mild (1.0 to 3.0 D) | 10 (41.6%) | 2 (40%) | 4 (28.5%) | 2 (40%) | 4 (25%) | 0.897 |
| Moderate (3.0 to 6.0D) | 7 (29.2%) | 2 (40%) | 2 (14.3%) | 3 (60%) | 6 (37.5%) | 0.582 |
| Severe (>6.0 D) | 7 (29.2%) | 1 (20%) | 5 (35.7%) | 0 (0%) | 3 (18.8%) | 0.453 |
| Group | Headache (Days/Week) | Headache Duration (Minutes) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | Mean Reduction | p Value (Paired t Test) | Preoperative | Postoperative | Mean Reduction | p Value (Paired t Test) | |||||
| Mean | Range | Mean | Range | Mean | Range | Mean | Range | |||||
| Overall Headache | 4.4 | 1–7 | 0.5 | 0–3 | 3.9 | <0.001 | 108.5 | 10–360 | 34.4 | 0–240 | 74.1 | 0.002 |
| (n = 24) | ||||||||||||
| Migraine | 3.8 | 2–7 | 0.4 | 0–1 | 3.4 | 0.007 | 125.0 | 30–240 | 60.0 | 0–120 | 65.0 | 0.208 |
| (n = 5) | ||||||||||||
| HARE | 4.7 | 1–7 | 0.6 | 0–3 | 4.1 | <0.001 | 115.0 | 10–360 | 97.5 | 5–240 | 17.5 | 0.045 |
| (n = 14) | ||||||||||||
| TTH | 4.0 | 1–7 | 0.2 | 0–1 | 3.8 | 0.030 | 72.0 | 15–180 | 30.0 | 0–60 | 42.0 | 0.072 |
| (n = 5) | ||||||||||||
| Group | Mean HIT-6 Score | ||
|---|---|---|---|
| Preoperative | Postoperative | p Value | |
| Overall headache group (n = 24) | 62.4 | 46.6 | <0.001 |
| (40–78) | (36–78) | ||
| Migraine group (n = 5) | 62.0 | 45.0 | 0.006 |
| (57–66) | (36–60) | ||
| HARE group (n = 14) | 63.0 | 47.0 | 0.001 |
| (49–78) | (36–78) | ||
| TTH group (n = 5) | 56.0 | 42.8 | 0.176 |
| (40–70) | (36–58) | ||
| HIT-6 Score Categories | Overall Headache Group (n = 24) | Migraine Group (n = 5) | HARE Group (n = 14) | TTH Group (n = 5) | ||||
|---|---|---|---|---|---|---|---|---|
| Preoperative | Postoperative | Preoperative | Postoperative | Preoperative | Postoperative | Preoperative | Postoperative | |
| >60 (disabling pain) | 16 (66.7%) | 4 (16.7%) | 4 (80%) | 1 (20%) | 10 (71.4%) | 3 (21.4%) | 2 (40%) | 0 (0%) |
| p value | 0.001 | 0.045 | 0.082 | 0.157 | ||||
| 56–59 (substantial impact) | 2 (8.3%) | 1(4.17%) | 1 (20%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (20%) | 1 (20%) |
| p value | 0.006 | 0.065 | n/a | 1.000 | ||||
| 50–55 | 4 (16.7%) | 0 (0%) | 0 (0%) | 0 (0%) | 3 (21.4%) | 0 (0%) | 1 (20%) | 0 (0%) |
| (some impact) | ||||||||
| p value | 0.001 | n/a | 0.083 | 0.065 | ||||
| <49 | 2 (8.3%) | 19 (79.2%) | 0 (0%) | 4 (80%) | 1 (7.1%) | 11 (78.6%) | 1 (20%) | 4 (80%) |
| (minimal impact) | ||||||||
| p value | <0.001 | 0.730 | 0.005 | 0.045 | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khoo, N.T.-H.; Burgos-Blasco, B.; Antoniou, A.; Jenkins, B.; Fraser, C.L.; Moloney, G. Headache Attributed to Refractive Error: Improvement after Topography-Guided Photorefractive Keratectomy with Corneal Cross-Linking in Patients with Keratoconus. J. Clin. Med. 2024, 13, 690. https://doi.org/10.3390/jcm13030690
Khoo NT-H, Burgos-Blasco B, Antoniou A, Jenkins B, Fraser CL, Moloney G. Headache Attributed to Refractive Error: Improvement after Topography-Guided Photorefractive Keratectomy with Corneal Cross-Linking in Patients with Keratoconus. Journal of Clinical Medicine. 2024; 13(3):690. https://doi.org/10.3390/jcm13030690
Chicago/Turabian StyleKhoo, Nigel Terk-Howe, Barbara Burgos-Blasco, Angelique Antoniou, Bronwyn Jenkins, Clare L. Fraser, and Gregory Moloney. 2024. "Headache Attributed to Refractive Error: Improvement after Topography-Guided Photorefractive Keratectomy with Corneal Cross-Linking in Patients with Keratoconus" Journal of Clinical Medicine 13, no. 3: 690. https://doi.org/10.3390/jcm13030690
APA StyleKhoo, N. T.-H., Burgos-Blasco, B., Antoniou, A., Jenkins, B., Fraser, C. L., & Moloney, G. (2024). Headache Attributed to Refractive Error: Improvement after Topography-Guided Photorefractive Keratectomy with Corneal Cross-Linking in Patients with Keratoconus. Journal of Clinical Medicine, 13(3), 690. https://doi.org/10.3390/jcm13030690