Risk Factors for Malignancy of Thyroid Nodules in Patients Undergoing Thyroid Resection
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients and Methods
2.2. Diagnosis and Evaluation
2.3. Statistical Analysis
3. Results
3.1. Results Obtained from the Entire Study Group of Patients (n = 521)
| Cytology | No. of Malignant Cases (All) | ROM % |
|---|---|---|
| I | 8 (21) | 38.1 |
| II | 28 (180) | 15.6 |
| III | 25 (84) | 29.8 |
| IV | 13 (70) | 18.6 |
| V | 61 (67) | 91 |
| VI | 55 (59) | 93.2 |
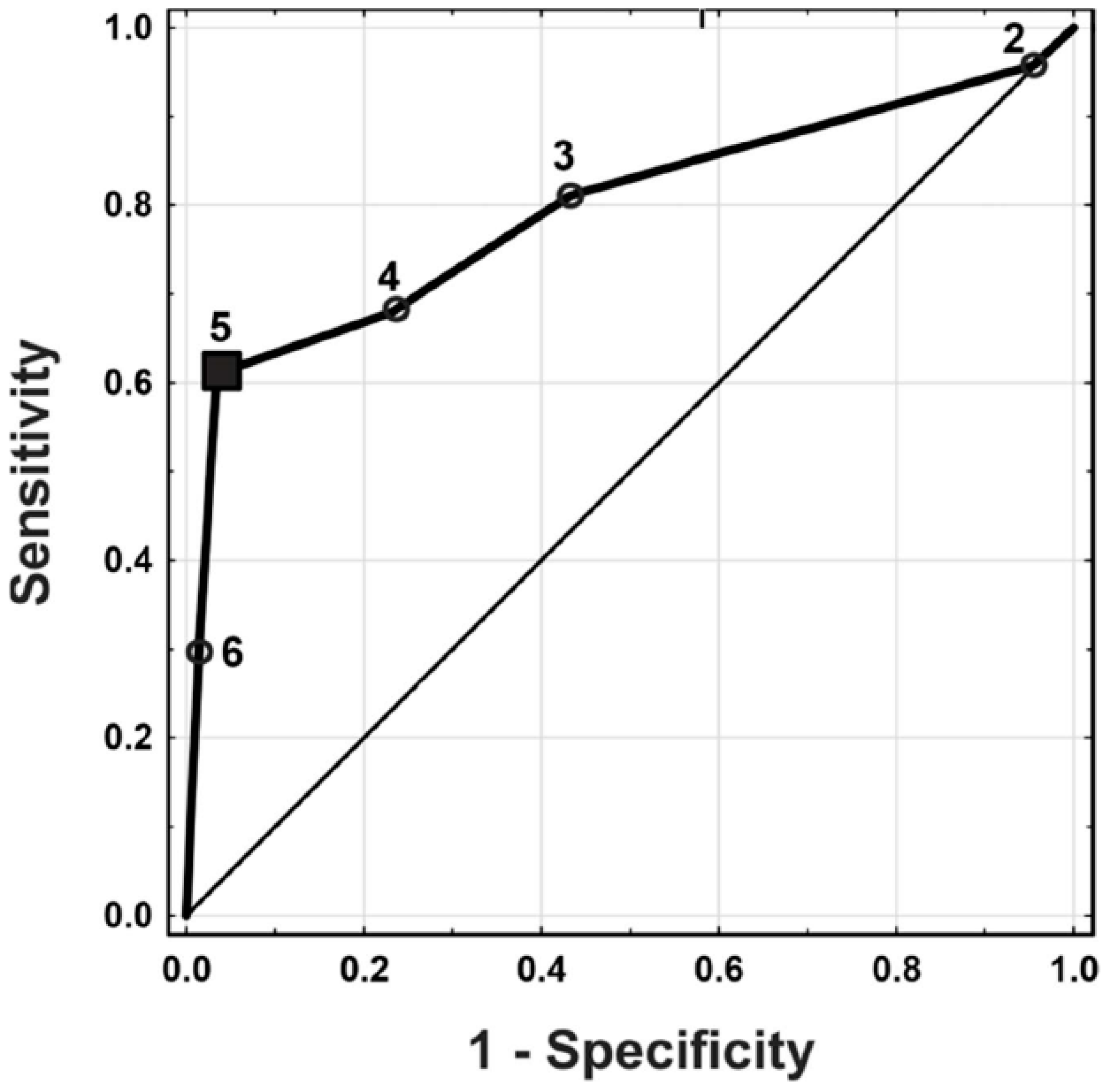
| Criterion | TP | FP | FN | TN | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|---|---|---|
| 6 | 55 | 4 | 135 | 287 | 0.29 (0.23, 0.36) | 0.99 (0.97, 1.00) | 0.93 (0.84, 0.98) | 0.68 (0.63, 0.72) |
| 5 | 116 | 10 | 74 | 281 | 0.61 (0.54, 0.68) | 0.97 (0.94, 0.98) | 0.92 (0.86, 0.96) | 0.79 (0.75, 0.83) |
| 4 | 129 | 67 | 61 | 224 | 0.68 (0.61, 0.74) | 0.77 (0.72, 0.82) | 0.66 (0.59, 0.72) | 0.79 (0.73, 0.83) |
| 3 | 154 | 126 | 36 | 165 | 0.81 (0.75, 0.86) | 0.57 (0.51, 0.62) | 0.55 (0.49, 0.61) | 0.82 (0.76, 0.87) |
| 2 | 182 | 278 | 8 | 13 | 0.96 (0.92, 0.98) | 0.04 (0.02, 0.08) | 0.40 (0.35, 0.44) | 0.62 (0.38, 0.82) |
3.2. Results of Patients in Bethesda DCs III, IV, and V (n = 221)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dean, D.S.; Gharib, H. Epidemiology of thyroid nodules. Best. Pract. Res. Clin. Endocrinol. Metab. 2008, 22, 901–911. [Google Scholar] [CrossRef] [PubMed]
- Guth, S.; Theune, U.; Aberle, J.; Galach, A.; Bamberger, C.M. Very high prevalence of thyroid nodules detected by high frequency (13 MHz) ultrasound examination. Eur. J. Clin. Investig. 2009, 39, 699–706. [Google Scholar] [CrossRef] [PubMed]
- Acar, T.; Ozbek, S.S.; Acar, S. Incidentally discovered thyroid nodules: Frequency in an adult population during Doppler ultrasonographic evaluation of cervical vessels. Endocrine 2014, 45, 73–78. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Miller, K.D.; Wagle, N.S.; Jemal, A. Cancer statistics, 2023. CA Cancer J. Clin. 2023, 73, 17–48. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Maso, L.D.; Vaccarella, S. Global trends in thyroid cancer incidence and the impact of overdiagnosis. Lancet Diabetes Endocrinol. 2020, 8, 468–470. [Google Scholar] [CrossRef]
- Lewis, C.M.; Chang, K.P.; Pitman, M.; Faquin, W.C.; Randolph, G.W. Thyroid fine-needle aspiration biopsy: Variability in reporting. Thyroid 2009, 19, 717–723. [Google Scholar] [CrossRef]
- Gupta, M.; Gupta, S.; Gupta, V.B. Correlation of fine needle aspiration cytology with histopathology in the diagnosis of solitary thyroid nodule. J. Thyroid. Res. 2010, 2010, 379051. [Google Scholar] [CrossRef]
- Russ, G.; Bonnema, S.J.; Erdogan, M.F.; Durante, C.; Ngu, R.; Leenhardt, L. European Thyroid Association Guidelines for Ultrasound Malignancy Risk Stratification of Thyroid Nodules in Adults: The EU-TIRADS. Eur. Thyroid. J. 2017, 6, 225–237. [Google Scholar] [CrossRef]
- Cibas, E.S.; Ali, S.Z. The 2017 Bethesda System for Reporting Thyroid Cytopathology. J. Am. Soc. Cytopathol. 2017, 6, 217–222. [Google Scholar] [CrossRef]
- Pusztaszeri, M.; Rossi, E.D.; Auger, M.; Baloch, Z.; Bishop, J.; Bongiovanni, M.; Chandra, A.; Cochand-Priollet, B.; Fadda, G.; Hirokawa, M.; et al. The Bethesda System for Reporting Thyroid Cytopathology: Proposed Modifications and Updates for the Second Edition from an International Panel. Acta Cytol. 2016, 60, 399–405. [Google Scholar] [CrossRef]
- Baloch, Z.W.; Cooper, D.S.; Gharib, H.; Alexander, E.K. Overview of diagnostic terminology and reporting. In The Bethesda System for Reporting Cytopathology: Definitions, Criteria and Explanatory Notes; Syed, Z., Ali, E.S.C., Eds.; Springer: Cham, Switzerland, 2018; pp. 1–6. [Google Scholar]
- Krajewska, J.; Chmielik, E.; Dedecjus, M.; Jarząb, B.; Hubalewska-Dydejczyk, A.; Karbownik-Lewińska, M.; Kos-Kudła, B.; Lewiński, A.; Ruchała, M. Diagnosis and treatment of thyroid cancer in adult patients—Recommendations of Polish Scientific Societies and the National Oncological Strategy. Update of the 2022. Endokrynol. Pol. 2022, 73, 799–802. [Google Scholar] [CrossRef] [PubMed]
- Kobaly, K.; Kim, C.S.; Mandel, S.J. Contemporary Management of Thyroid Nodules. Annu. Rev. Med. 2022, 73, 517–528. [Google Scholar] [CrossRef] [PubMed]
- EUROCRINE. Available online: https://eurocrine.eu (accessed on 28 April 2024).
- Jung, C.K.; Bychkov, A.; Kakudo, K. Update from the 2022 World Health Organization Classification of Thyroid Tumors: A Standardized Diagnostic Approach. Endocrinol. Metab. 2022, 37, 703–718. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing, version 4.4.2; R Foundation for Statistical Computing: Vienna, Austria, 2021; Available online: https://www.R-project.org/ (accessed on 31 October 2024).
- Osseis, M.; Jammal, G.; Kazan, D.; Noun, R. Comparison between Fine Needle Aspiration Cytology with Histopathology in the Diagnosis of Thyroid Nodules. J. Pers. Med. 2023, 13, 1197. [Google Scholar] [CrossRef]
- Sherman, S.I. Thyroid carcinoma. Lancet 2003, 361, 501–511. [Google Scholar] [CrossRef]
- McCoy, K.L.; Jabbour, N.; Ogilvie, J.B.; Ohori, N.P.; Carty, S.E.; Yim, J.H. The incidence of cancer and rate off alse-negative cytology in thyroid nodules greater than or equal to 4 cm in size. Surgery 2007, 142, 837–844.e3. [Google Scholar] [CrossRef]
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef]
- Hegedüs, L. The thyroid nodule. N. Engl. J. Med. 2004, 351, 1764–1771. [Google Scholar] [CrossRef]
- Rai, K.; Park, J.; Gokhale, S.; Irshaidat, F.; Singh, G. Diagnostic Accuracy of the Bethesda System for Reporting Thyroid Cytopathology (TBSRTC): An Institution Experience. Int. J. Endocrinol. 2023, 2023, 9615294. [Google Scholar] [CrossRef]
- Garg, S.; Desai, N.J.; Mehta, D.; Vaishnav, M. To Establish Bethesda System for Diagnosis of Thyroid Nodules on the Basis of Fnac with Histopathological Correlation. J. Clin. Diagn. Res. 2015, 9, EC17–EC21. [Google Scholar] [CrossRef]
- Nandedkar, S.S.; Dixit, M.; Malukani, K.; Varma, A.V.; Gambhir, S. Evaluation of Thyroid Lesions by Fine-needle Aspiration Cytology According to Bethesda System and its Histopathological Correlation. Int. J. Appl. Basic. Med. Res. 2018, 8, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.A.; Anandani, G.; Sharma, B.S.; Parmar, R.A. Study of Fine Needle Aspiration Cytology (FNAC) of Thyroid Gland According to the Bethesda System. Cureus 2023, 15, e37371. [Google Scholar] [CrossRef] [PubMed]
- Mondal, S.K.; Sinha, S.; Basak, B.; Roy, D.N.; Sinha, S.K. The Bethesda system for reporting thyroid fine needle aspirates: A cytologic study with histologic follow-up. J. Cytol. 2013, 30, 94–99. [Google Scholar] [CrossRef] [PubMed]
- Inabnet, W.B., 3rd; Palazzo, F.; Sosa, J.A.; Kriger, J.; Aspinall, S.; Barczynski, M.; Doherty, G.; Iacobone, M.; Nordenstrom, E.; Scott-Coombes, D.; et al. Correlating the Bethesda System for Reporting Thyroid Cytopathology with Histology and Extent of Surgery: A Review of 21,746 Patients from Four Endocrine Surgery Registries Across Two Continents. World J. Surg. 2020, 44, 426–435. [Google Scholar] [CrossRef] [PubMed]
- Anand, B.; Ramdas, A.; Ambroise, M.M.; Kumar, N.P. The Bethesda System for Reporting Thyroid Cytopathology: A Cytohistological Study. J. Thyroid. Res. 2020, 2020, 8095378. [Google Scholar] [CrossRef]
- Zarif, H.A.; Ghandurah, S.E.; Al-Garni, M.A.; Binmahfooz, S.K.; Alsaywid, B.S.; Satti, M.B. Thyroid Nodules Cytopathology Applying the Bethesda System with Histopathological Correlation. Saudi J. Med. Med. Sci. 2018, 6, 143–148. [Google Scholar] [CrossRef]
- Alshathry, A.H.; Almeshari, N.Z.; Alarifi, A.S.; Aleidy, A.M.; Aldhahri, S. The Prevalence of Thyroid Papillary Microcarcinoma in Patients With Benign Thyroid Fine Needle Aspiration. Cureus 2020, 12, e11820. [Google Scholar] [CrossRef]
- Gan, T.R.X.; Nga, M.E.; Lum, J.H.Y.; Wong, W.M.; Tan, W.B.; Parameswaran, R.; Ngiam, K.Y. Thyroid cytology—Nuclear versus architectural atypia within the “Atypia of undetermined significance/follicular lesion of undetermined significance” Bethesda category have significantly different rates of Malignancy. Cancer Cytopathol. 2017, 125, 245–256. [Google Scholar] [CrossRef]
- Mosca, L.; Silva, L.F.F.D.; Carneiro, P.C.; Chacon, D.A.; Araujo-Neto, V.J.F.; Araujo-Filho, V.J.F.; Cernea, C.R. Malignancy rates for Bethesda III subcategories in thyroid fine needle aspiration biopsy (FNAB). Clinics 2018, 73, e370. [Google Scholar] [CrossRef]
- Kim, S.J.; Roh, J.; Baek, J.H.; Hong, S.J.; Shong, Y.K.; Kim, W.B.; Song, D.E. Risk of malignancy according to sub-classification of the atypia of undetermined significance or follicular lesion of undetermined significance (AUS/FLUS) category in the Bethesda system for reporting thyroid cytopathology. Cytopathology 2017, 28, 65–73. [Google Scholar] [CrossRef]
- Erdogan-Durmus, S.; Balta, H.; Demirtas, R.; Kurt, A. Malignancy Rates of Atypia of Undetermined Significance/Follicular Lesion of Undetermined Significance (AUS/FLUS) Cases: A Tertiary Center Study. Acta Endocrinol. 2021, 17, 77–82. [Google Scholar] [CrossRef]
- Yang, W.; Fananapazir, G.; LaRoy, J.; Wilson, M.; Campbell, M.J. Can the American Thyroid Association, K-Tirads, and Acr-Tirads Ultrasound Classification Systems Be Used to Predict Malignancy in Bethesda Category IV Nodules? Endocr. Pract. 2020, 26, 945–952. [Google Scholar] [CrossRef] [PubMed]
- Marina, M.; Zatelli, M.C.; Goldoni, M.; Del Rio, P.; Corcione, L.; Martorana, D.; Percesepe, A.; Bonatti, F.; Mozzoni, P.; Crociara, A.; et al. Combination of ultrasound and molecular testing in malignancy risk estimate of Bethesda category IV thyroid nodules: Results from a single-institution prospective study. J. Endocrinol. Investig. 2021, 44, 2635–2643. [Google Scholar] [CrossRef] [PubMed]
- Ha, S.M.; Baek, J.H.; Na, D.G.; Jung, C.K.; Suh, C.H.; Shong, Y.K.; Sung, T.Y.; Song, D.E.; Lee, J.H. Assessing the diagnostic performance of thyroid biopsy with recommendations for appropriate interpretation. Ultrasonography 2021, 40, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Kwong, N.; Medici, M.; Angell, T.E.; Liu, X.; Marqusee, E.; Cibas, E.S.; Krane, J.F.; Barletta, J.A.; Kim, M.I.; Larsen, P.R.; et al. The Influence of Patient Age on Thyroid Nodule Formation, Multinodularity, and Thyroid Cancer Risk. J. Clin. Endocrinol. Metab. 2015, 100, 4434–4440. [Google Scholar] [CrossRef]
- Velsen, E.; Peeters, R.; Stegenga, M.; van Kemenade, F.; van Ginhoven, T.; Verburg, F.; Visser, E. The influence of age on disease outcome in 2015 ATA high-risk differentiated thyroid cancer patients. Eur. J. Endocrinol. 2021, 185, 421–429. [Google Scholar] [CrossRef]
- Raparia, K.; Min, S.K.; Mody, D.R.; Anton, R.; Amrikachi, M. Clinical outcomes for “suspicious” category in thyroid fine-needle aspiration biopsy: Patient’s sex and nodule size are possible predictors of Malignancy. Arch. Pathol. Lab. Med. 2009, 133, 787–790. [Google Scholar] [CrossRef]
- Konturek, A.; Barczyński, M.; Wierzchowski, W.; Stopa, M.; Nowak, W. Coexistence of papillary thyroid cancer with Hashimoto thyroiditis. Langenbeck’s Arch. Surg. 2013, 398, 389–394. [Google Scholar] [CrossRef]
- Zosin, I.; Balaş, M. Clinical, ultrasonographical and histopathological aspects in Hashimoto’s thyroiditis associated with malignant and benign thyroid nodules. Endokrynol. Pol. 2013, 64, 255–262. [Google Scholar] [CrossRef]
- Orlandella, F.M.; Imperlini, E.; Pane, K.; Luciano, N.; Braile, M.; De Stefano, A.E.; Iervolino, P.L.C.; Ruocco, A.; Orrù, S.; Franzese, M.; et al. miR-331-5p Affects Motility of Thyroid Cancer Cell Lines and Regulates BID Expression. Biomedicines 2024, 12, 658. [Google Scholar] [CrossRef]
| Total (N = 521) | Benign (N = 324) | Cancerous (N = 197) | p-Value | |
|---|---|---|---|---|
| Sex | 0.94 | |||
| Female | 425 (81.6%) | 264 (81.5%) | 161 (81.7%) | |
| Male | 96 (18.4%) | 60 (18.5%) | 36 (18.3%) | |
| BMI | 0.52 | |||
| Mean (SD) | 27.3 (4.87) | 27.4 (4.76) | 27.1 (5.08) | |
| Median [Q1–Q3] | 26.6 [23.5–30.5] | 26.7 [23.8–30.5] | 26.4 [23.2–30.8] | |
| Missing | 98 (18.8%) | 57 (17.6%) | 41 (20.8%) | |
| Obesity (BMI ≥ 30) | 0.76 | |||
| No | 302 (58.0%) | 192 (59.3%) | 110 (55.8%) | |
| Yes | 121 (23.2%) | 75 (23.1%) | 46 (23.4%) | |
| Missing | 98 (18.8%) | 57 (17.6%) | 41 (20.8%) | |
| Age | <0.0001 | |||
| Mean (SD) | 52.3 (15.2) | 55.3 (14.7) | 47.4 (14.9) | |
| Median [Q1–Q3] | 53.0 [40.0–65.0] | 57.0 [43.8–67.0] | 45.0 [36.0–59.0] | |
| Cytology | <0.0001 | |||
| I | 21 (4.0%) | 13 (4.0%) | 8 (4.1%) | |
| II | 180 (34.5%) | 152 (46.9%) | 28 (14.2%) | |
| III | 84 (16.1%) | 59 (18.2%) | 25 (12.7%) | |
| IV | 70 (13.4%) | 57 (17.6%) | 13 (6.6%) | |
| V | 67 (12.9%) | 6 (1.9%) | 61 (31.0%) | |
| VI | 59 (11.3%) | 4 (1.2%) | 55 (27.9%) | |
| Not performed | 40 (7.7%) | 33 (10.2%) | 7 (3.6%) | |
| Lymphocytic thyroiditis | <0.0001 | |||
| No | 442 (84.8%) | 292 (90.1%) | 150 (76.1%) | |
| Yes | 79 (15.2%) | 32 (9.9%) | 47 (23.9%) | |
| Malignancy | ||||
| PTC | 172 (33.0%) | 172 (87.3%) | ||
| FTC | 16 (3.1%) | 16 (8.1%) | ||
| MTC | 5 (1.0%) | 5 (2.5%) | ||
| ATC | 1 (0.2%) | 1 (0.5%) | ||
| OTC | 2 (0.4%) | 2 (1.0%) | ||
| Lymphoma | 1 (0.2%) | 1 (0.5%) | ||
| Thyroid operation | ||||
| Total thyroidectomy | 480 (92.1%) | 295 (91%) | 185 (94%) | |
| Unilateral lobectomy | 30 (5.7%) | 22 (6.8%) | 8 (4.1%) | |
| Other operation on thyroid gland | 11 (2.1%) | 7 (2.2%) | 4 (2.0%) | |
| Lymph nodes | ||||
| Bilateral central lymph node dissection | 191 (36.7%) | 89 (27.5%) | 102 (51.8%) | |
| Central lymph node dissection and one-sided lateral lymph node dissection | 18 (3.5%) | 2 (0.6%) | 16 (8.1%) | |
| Unilateral central lymph node dissection | 80 (15.4%) | 40 (12.3%) | 40 (20.3%) | |
| One-sided lateral lymph node dissection | 7 (1.3%) | 2 (0.6%) | 5 (2.5%) | |
| Bilateral lateral lymph node dissection | 2 (0.4%) | 0 (0%) | 2 (1%) | |
| None | 223 (42.8%) | 191 (59.0%) | 32 (16.2%) |
| Cytology | Total, n (%) | Histopathology | |||
|---|---|---|---|---|---|
| Benign, n (%) | Cancer, n (%) | ||||
| I | 21 (4.0%) | FA | 2 (15.4%) | FTC | 2 (25%) |
| GD | 1 (7.7%) | PTC | 6 (75%) | ||
| NG | 9 (69.2%) | ||||
| Other diagnosis | 1 (7.7%) | ||||
| II | 180 (34.5%) | FA | 15 (9.9%) | FTC | 4 (14.3%) |
| FT-UMP | 1 (0.7%) | MTC | 3 (10.7%) | ||
| GD | 1 (0.7%) | PTC | 21 (75%) | ||
| OA | 1 (0.7%) | ||||
| LT | 1 (0.7%) | ||||
| NG | 130 (85.5%) | ||||
| NIFTP | 2 (1.3%) | ||||
| III | 84 (16.1%) | FA | 14 (23.7%) | FTC | 7 (28.0%) |
| FT-UMP | 2 (3.4%) | OTC | 1 (4.0%) | ||
| OA | 1 (1.7%) | PTC | 17 (68.0%) | ||
| LT | 3 (5.1%) | ||||
| NG | 35 (59.3%) | ||||
| NIFTP | 2 (3.4%) | ||||
| WDT-UMP | 2 (3.4%) | ||||
| IV | 70 (13.4%) | FA | 15 (26.3%) | OTC | 1 (7.7%) |
| FT-UMP | 5 (8.8%) | PTC | 12 (92.3%) | ||
| OA | 13 (22.8%) | ||||
| LT | 2 (3.5%) | ||||
| NG | 18 (31.6%) | ||||
| NIFTP | 2 (3.5%) | ||||
| WDT-UMP | 2 (3.5%) | ||||
| V | 67 (12.9%) | FA | 1 (16.7%) | ATC | 1 (1.6%) |
| NG | 3 (50.0%) | FTC | 2 (3.3%) | ||
| NIFTP | 1 (16.7%) | PTC | 58 (95.1%) | ||
| Other diagnosis | 1 (16.7%) | ||||
| VI | 59 (11.3%) | NG | 2 (50.0%) | FTC | 1 (1.8%) |
| Other diagnosis | 2 (50.0%) | Lymphoma | 1 (1.8%) | ||
| MTC | 2 (3.6%) | ||||
| PTC | 51 (92.7%) | ||||
| Not performed | 40 (7.7%) | FA | 4 (12.1%) | PTC | 7 (100%) |
| GD | 3 (9.1%) | ||||
| OA | 2 (6.1%) | ||||
| LT | 1 (3.0%) | ||||
| NG | 19 (57.6%) | ||||
| NIFTP | 3 (9.1%) | ||||
| Total (N = 401) | II (N = 180) | III (N = 84) | IV (N = 70) | V (N = 67) | p-Value | |
|---|---|---|---|---|---|---|
| Sex | 0.39 | |||||
| Female | 326 (81.3%) | 140 (77.8%) | 69 (82.1%) | 60 (85.7%) | 57 (85.1%) | |
| Male | 75 (18.7%) | 40 (22.2%) | 15 (17.9%) | 10 (14.3%) | 10 (14.9%) | |
| Age | 0.00001 | |||||
| Mean (SD) | 53.6 (14.7) | 55.2 (14.4) | 54.6 (12.0) | 55.8 (16.3) | 45.8 (14.3) | |
| Median [Q1–Q3] | 54.0 [42.0–66.0] | 56.0 [44.0–67.0] | 57.0 [44.0–65.3] | 58.0 [42.0–68.0] | 42.0 [35.5–56.0] | |
| Histological main diagnosis | <0.0001 | |||||
| Benign | 274 (68.3%) | 152 (84.4%) | 59 (70.2%) | 57 (81.4%) | 6 (9.0%) | |
| Cancerous | 127 (31.7%) | 28 (15.6%) | 25 (29.8%) | 13 (18.6%) | 61 (91.0%) | |
| Lymphocytic thyroiditis | <0.0001 | |||||
| No | 340 (84.8%) | 163 (90.6%) | 74 (88.1%) | 62 (88.6%) | 41 (61.2%) | |
| Yes | 61 (15.2%) | 17 (9.4%) | 10 (11.9%) | 8 (11.4%) | 26 (38.8%) |
| Bethesda Categories | Malignancy | |
|---|---|---|
| n (%)/n (%) | p-Value | |
| III vs. II | 25 (29.8%)/28 (15.6%) | 0.019 |
| III vs. IV | 25 (29.8%)/13 (18.6%) | 0.161 |
| III vs. V | 25 (29.8%)/61 (91.0%) | <0.0001 |
| II vs. IV | 28 (15.6%)/13 (18.6%) | 0.572 |
| II vs. V | 28 (15.6%)/61 (91.0%) | <0.0001 |
| IV vs. V | 13 (18.6%)/61 (91.0%) | <0.0001 |
| Bethesda Categories | Lymphocytic Thyroiditis | |
|---|---|---|
| n (%)/n (%) | p-Value | |
| III vs. II | 10 (11.9%)/ 17(9.4%) | 0.98 |
| III vs. IV | 10 (11.9%)/ 8(11.4%) | 0.99 |
| III vs. V | 10 (11.9%)/ 26(38.8%) | 0.0008 |
| II vs. IV | 17 (9.4%)/ 8(11.4%) | 0.98 |
| II vs. V | 17 (9.4%)/ 26(38.8%) | <0.0001 |
| IV vs. V | 8 (11.4%)/ 26(38.8%) | 0.0009 |
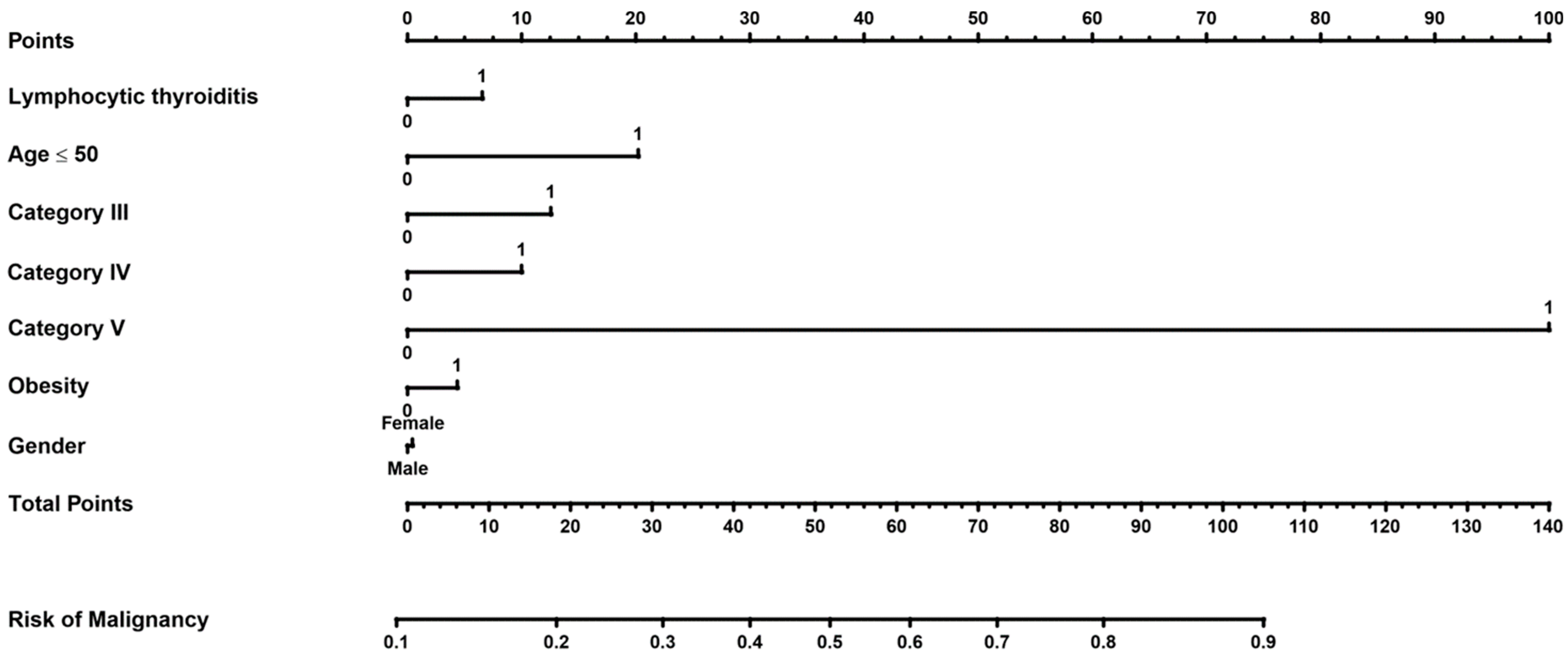
| Variable | OR per | Univariate | Multivariate | ||
|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | ||
| Sex | Female/male | 0.87 (0.51–1.51) | 0.63 | 1.02 (0.47–2.18) | 0.96 |
| Lymphocytic thyroiditis | Yes/no | 2.85 (1.63–4.96) | 0.0002 | 1.31 (0.55–3.11) | 0.54 |
| Bethesda III | Yes/no | 0.89 (0.53–1.51) | 0.67 | 1.68 (0.81–3.47) | 0.16 |
| Bethesda IV | Yes/no | 0.43 (0.23–0.83) | 0.011 | 1.51 (0.69–3.32) | 0.30 |
| Bethesda V | Yes/no | 41.28 (17.11–99.61) | <0.0001 | 62.34 (20.16–192.8) | <0.0001 |
| Age ≤ 50 | Yes/no | 2.67 (1.74–4.12) | <0.0001 | 2.31 (1.27–4.19) | 0.006 |
| Obesity (BMI ≥ 30) | Yes/no | 0.90 (0.53–1.51) | 0.68 | 1.2 (0.62–2.31) | 0.59 |
| Bethesda Category | TBSRTC [9], First Edition | TBSRTC [11], Second Edition | ROM of Our Study, n = 521 | ROM of Inabnet et al. [27], n = 1746 | ROM of Anand et al. [28], n = 646 | ROM of Zarif at al. [29], n = 373 |
|---|---|---|---|---|---|---|
| I—Non-diagnostic | 1–4% | 5–10% | 38.8% | 19.2% | 34.6% | |
| II—Benign | 0–3% | 0–3% | 15.6% | 12.7% | 8.5% | 15.6% |
| III—AUS/FLUS | 5–15% | 10–30% | 29.8% | 31.9% | 66.7% | 50% |
| IV—FN/SFN | 15–30% | 25–40% | 18.6% | 31.4% | 63.6% | 52% |
| V—SFM | 60–75% | 50–75% | 91.0% | 77.8% | 100% | 95.7% |
| VI—Malignant | 97–99% | 97–99% | 93.2% | 96.0% | 100% | 100% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krzentowska, A.; Gołkowski, F.; Broniatowska, E.; Konturek, A.; Barczyński, M. Risk Factors for Malignancy of Thyroid Nodules in Patients Undergoing Thyroid Resection. J. Clin. Med. 2024, 13, 7559. https://doi.org/10.3390/jcm13247559
Krzentowska A, Gołkowski F, Broniatowska E, Konturek A, Barczyński M. Risk Factors for Malignancy of Thyroid Nodules in Patients Undergoing Thyroid Resection. Journal of Clinical Medicine. 2024; 13(24):7559. https://doi.org/10.3390/jcm13247559
Chicago/Turabian StyleKrzentowska, Anna, Filip Gołkowski, Elżbieta Broniatowska, Aleksander Konturek, and Marcin Barczyński. 2024. "Risk Factors for Malignancy of Thyroid Nodules in Patients Undergoing Thyroid Resection" Journal of Clinical Medicine 13, no. 24: 7559. https://doi.org/10.3390/jcm13247559
APA StyleKrzentowska, A., Gołkowski, F., Broniatowska, E., Konturek, A., & Barczyński, M. (2024). Risk Factors for Malignancy of Thyroid Nodules in Patients Undergoing Thyroid Resection. Journal of Clinical Medicine, 13(24), 7559. https://doi.org/10.3390/jcm13247559







