Do Acute Illness Perceptions Moderate the Association of Pre-Collision Welfare Benefits and Later Neck Pain or Disability Following Whiplash Trauma? A Prospective Multicentre Cohort Study
Abstract
1. Introduction
2. Materials and Methods
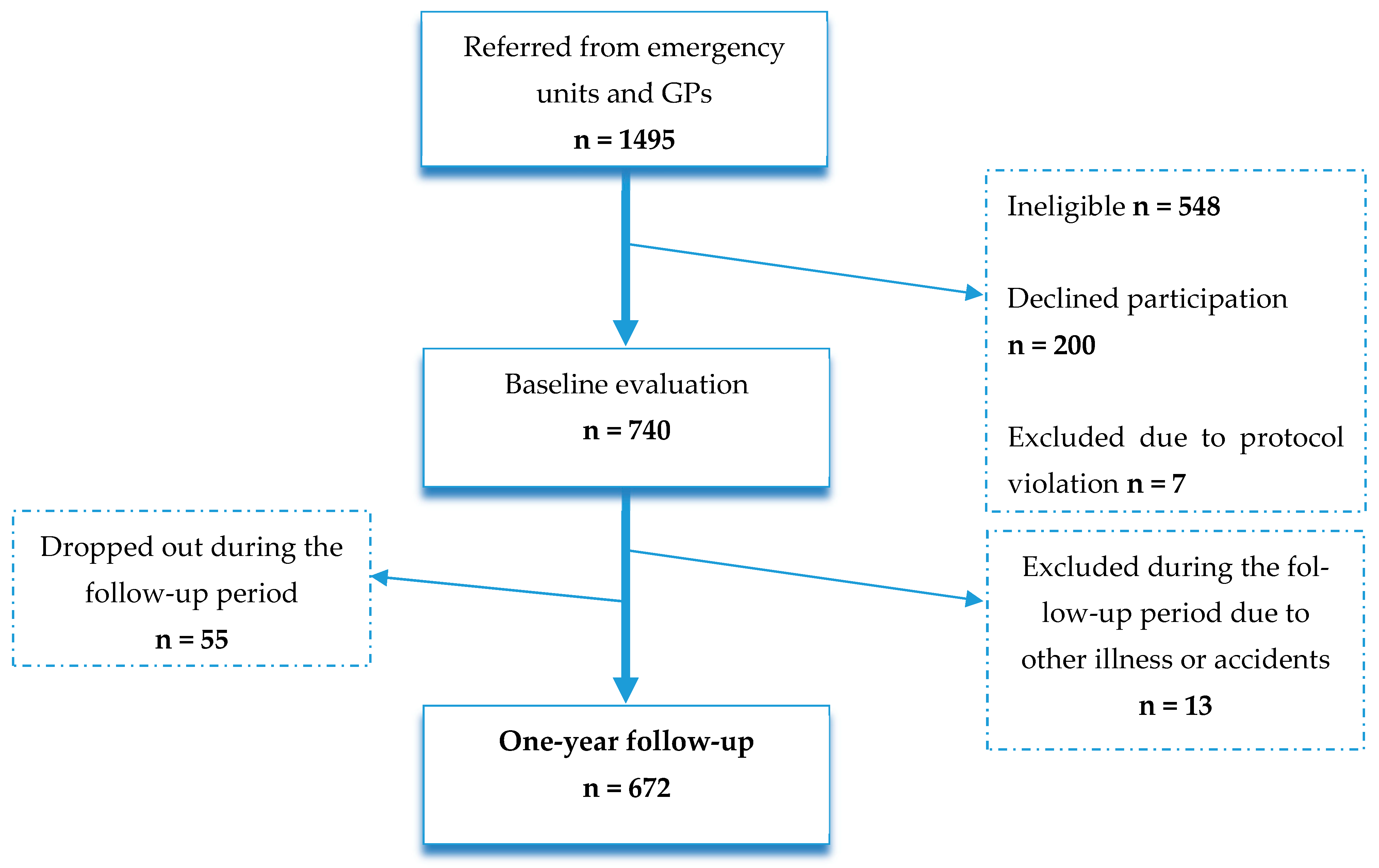
2.1. Study Design and Population
2.2. Measures
2.2.1. Explanatory Variables
2.2.2. Hypothesised Moderators
2.2.3. Outcome Measures
Neck Pain Intensity
Neck-Related Disability
2.2.4. Covariates
2.3. Statistical Analyses
2.3.1. Descriptive Statistics
2.3.2. Multiple Logistic Regression Analyses
2.3.3. Attrition Analysis
3. Results
3.1. Participant Characteristics
3.2. Multiple Logistic Regression Analyses
3.3. Attrition Analysis
4. Discussion
4.1. Summary of Findings
4.2. Interpretation of Findings
4.3. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Al-Khazali, H.M.; Ashina, H.; Iljazi, A.; Lipton, R.B.; Ashina, M.; Ashina, S.; Schytz, H.W. Neck pain and headache after whiplash injury: A systematic review and meta-analysis. Pain 2020, 161, 880–888. [Google Scholar] [CrossRef] [PubMed]
- Shearer, H.; Carroll, L.; Côté, P.; Randhawa, K.; Southerst, D.; Varatharajan, S.; Wong, J.; Yu, H.; Sutton, D.; van der Velde, G.; et al. The course and factors associated with recovery of whiplash-associated disorders: An updated systematic review by the Ontario protocol for traffic injury management (OPTIMa) collaboration. Eur. J. Physiother. 2020, 23, 279–294. [Google Scholar] [CrossRef]
- Spitzer, W.O.; Skovron, M.L.; Salmi, L.R.; Cassidy, J.D.; Duranceau, J.; Suissa, S.; Zeiss, E. Scientific monograph of the Quebec Task Force on Whiplash-Associated Disorders: Redefining “whiplash” and its management. Spine 1995, 20, 1S–73S. [Google Scholar] [PubMed]
- Giummarra, M.J.; Ioannou, L.; Ponsford, J.; Cameron, P.A.; Jennings, P.A.; Gibson, S.J.; Georgiou-Karistianis, N. Chronic Pain Following Motor Vehicle Collision: A Systematic Review of Outcomes Associated With Seeking or Receiving Compensation. Clin. J. Pain 2016, 32, 817–827. [Google Scholar] [CrossRef]
- Craig, A.; Tran, Y.; Guest, R.; Gopinath, B.; Jagnoor, J.; Bryant, R.A.; Collie, A.; Tate, R.; Kenardy, J.; Middleton, J.W.; et al. Psychological impact of injuries sustained in motor vehicle crashes: Systematic review and meta-analysis. BMJ Open 2016, 6, e011993. [Google Scholar] [CrossRef]
- Oka, H.; Matsudaira, K.; Fujii, T.; Tanaka, S.; Kitagawa, T. Epidemiology and psychological factors of whiplash associated disorders in Japanese population. J. Phys. Ther. Sci. 2017, 29, 1510–1513. [Google Scholar] [CrossRef]
- Dantoft, T.M.; Ebstrup, J.F.; Linneberg, A.; Skovbjerg, S.; Madsen, A.L.; Mehlsen, J.; Brinth, L.; Eplov, L.F.; Carstensen, T.W.; Schroder, A.; et al. Cohort description: The Danish study of Functional Disorders. Clin. Epidemiol. 2017, 9, 127–139. [Google Scholar] [CrossRef]
- Samoborec, S.; Ruseckaite, R.; Ayton, D.; Evans, S. Biopsychosocial factors associated with non-recovery after a minor transport-related injury: A systematic review. PLoS ONE 2018, 13, e0198352. [Google Scholar] [CrossRef]
- Oka, H.; Matsudaira, K.; Fujii, T.; Okazaki, H.; Shinkai, Y.; Tsuji, Y.; Tanaka, S.; Kato, R. Risk Factors for Prolonged Treatment of Whiplash-Associated Disorders. PLoS ONE 2015, 10, e0132191. [Google Scholar] [CrossRef]
- Osterland, T.B.; Kasch, H.; Frostholm, L.; Bendix, T.; Jensen, T.S.; Jensen, J.S.; Carstensen, T.B.W. Precollision Medical Diagnoses Predict Chronic Neck Pain Following Acute Whiplash Trauma. Clin. J. Pain 2019, 35, 304–314. [Google Scholar] [CrossRef]
- Bendix, T.; Kjellberg, J.; Ibsen, R.; Jennum, P.J. Whiplash(-like) injury diagnoses and co-morbidities--both before and after the injury: A national registry-based study. BMC Musculoskelet. Disord. 2016, 17, 24. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Carstensen, T.B.; Fink, P.; Oernboel, E.; Kasch, H.; Jensen, T.S.; Frostholm, L. Sick Leave within 5 Years of Whiplash Trauma Predicts Recovery: A Prospective Cohort and Register-Based Study. PLoS ONE 2015, 10, e0130298. [Google Scholar] [CrossRef] [PubMed]
- Myrtveit, S.M.; Wilhelmsen, I.; Petrie, K.J.; Skogen, J.C.; Sivertsen, B. What characterizes individuals developing chronic whiplash?: The Nord-Trondelag Health Study (HUNT). J. Psychosom. Res. 2013, 74, 393–400. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Williamson, E.; Williams, M.A.; Gates, S.; Lamb, S.E. Risk factors for chronic disability in a cohort of patients with acute whiplash associated disorders seeking physiotherapy treatment for persisting symptoms. Physiotherapy 2015, 101, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Leventhal, H.; Phillips, L.A.; Burns, E. The Common-Sense Model of Self-Regulation (CSM): A dynamic framework for understanding illness self-management. J. Behav. Med. 2016, 39, 935–946. [Google Scholar] [CrossRef]
- Richardson, E.M.; Schüz, N.; Sanderson, K.; Scott, J.L.; Schüz, B. Illness representations, coping, and illness outcomes in people with cancer: A systematic review and meta-analysis. Psychooncology 2017, 26, 724–737. [Google Scholar] [CrossRef]
- McAndrew, L.M.; Crede, M.; Maestro, K.; Slotkin, S.; Kimber, J.; Phillips, L.A. Using the common-sense model to understand health outcomes for medically unexplained symptoms: A meta-analysis. Health Psychol. Rev. 2019, 13, 427–446. [Google Scholar] [CrossRef]
- Dempster, M.; Howell, D.; McCorry, N.K. Illness perceptions and coping in physical health conditions: A meta-analysis. J. Psychosom. Res. 2015, 79, 506–513. [Google Scholar] [CrossRef]
- De Gucht, V. Illness perceptions mediate the relationship between bowel symptom severity and health-related quality of life in IBS patients. Qual. Life Res. 2015, 24, 1845–1856. [Google Scholar] [CrossRef]
- van Erp, S.J.; Brakenhoff, L.K.; Vollmann, M.; van der Heijde, D.; Veenendaal, R.A.; Fidder, H.H.; Hommes, D.W.; Kaptein, A.A.; van der Meulen-de Jong, A.E.; Scharloo, M. Illness Perceptions and Outcomes in Patients with Inflammatory Bowel Disease: Is Coping a Mediator? Int. J. Behav. Med. 2017, 24, 205–214. [Google Scholar] [CrossRef]
- Berner, C.; Erlacher, L.; Fenzl, K.H.; Dorner, T.E. A cross-sectional study on self-reported physical and mental health-related quality of life in rheumatoid arthritis and the role of illness perception. Health Qual Life Outcomes 2018, 16, 238. [Google Scholar] [CrossRef] [PubMed]
- Hoving, J.L.; van der Meer, M.; Volkova, A.Y.; Frings-Dresen, M.H. Illness perceptions and work participation: A systematic review. Int. Arch. Occup. Environ. Health 2010, 83, 595–605. [Google Scholar] [CrossRef] [PubMed]
- Gehrt, T.B.; Wisbech Carstensen, T.B.; Ornbol, E.; Fink, P.K.; Kasch, H.; Frostholm, L. The role of illness perceptions in predicting outcome after acute whiplash trauma: A multicenter 12-month follow-up study. Clin. J. Pain 2015, 31, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Kongsted, A.; Qerama, E.; Kasch, H.; Bach, F.W.; Korsholm, L.; Jensen, T.S.; Bendix, T. Education of patients after whiplash injury: Is oral advice any better than a pamphlet? Spine 2008, 33, E843–E848. [Google Scholar] [CrossRef]
- Kongsted, A.; Qerama, E.; Kasch, H.; Bendix, T.; Winther, F.; Korsholm, L.; Jensen, T.S. Neck collar, “act-as-usual” or active mobilization for whiplash injury? A randomized parallel-group trial. Spine 2007, 32, 618–626. [Google Scholar] [CrossRef]
- Textor, J.; van der Zander, B.; Gilthorpe, M.S.; Liskiewicz, M.; Ellison, G.T. Robust causal inference using directed acyclic graphs: The R package ‘dagitty’. Int. J. Epidemiol. 2016, 45, 1887–1894. [Google Scholar] [CrossRef]
- Hjollund, N.H.; Larsen, F.B.; Andersen, J.H. Register-based follow-up of social benefits and other transfer payments: Accuracy and degree of completeness in a Danish interdepartmental administrative database compared with a population-based survey. Scand. J. Public Health 2007, 35, 497–502. [Google Scholar] [CrossRef]
- Du Bois, M.; Szpalski, M.; Donceel, P. Patients at risk for long-term sick leave because of low back pain. Spine J. 2009, 9, 350–359. [Google Scholar] [CrossRef]
- Rivera, E.; Levoy, K.; Park, C.; Villalobos, A.; Martin, P.; Jung Kim, M.; Hirschman, K.B. Internal consistency reliability of the Revised Illness Perceptions Questionnaire: A systematic review and reliability generalization meta-analysis. J. Health Psychol. 2024, 29, 734–746. [Google Scholar] [CrossRef]
- Frostholm, L.; Fink, P.; Christensen, K.S.; Toft, T.; Oernboel, E.; Olesen, F.; Weinman, J. The patients’ illness perceptions and the use of primary health care. Psychosom. Med. 2005, 67, 997–1005. [Google Scholar] [CrossRef]
- Broadbent, E.; Wilkes, C.; Koschwanez, H.; Weinman, J.; Norton, S.; Petrie, K.J. A systematic review and meta-analysis of the Brief Illness Perception Questionnaire. Psychol. Health 2015, 30, 1361–1385. [Google Scholar] [CrossRef] [PubMed]
- Collins, S.L.; Moore, R.A.; McQuay, H.J. The visual analogue pain intensity scale: What is moderate pain in millimetres? Pain 1997, 72, 95–97. [Google Scholar] [CrossRef] [PubMed]
- Bobos, P.; MacDermid, J.C.; Walton, D.M.; Gross, A.; Santaguida, P.L. Patient-Reported Outcome Measures Used for Neck Disorders: An Overview of Systematic Reviews. J. Orthop. Sports Phys. Ther. 2018, 48, 775–788. [Google Scholar] [CrossRef] [PubMed]
- Zieliński, G.; Gawda, P. Analysis of the Use of Sample Size and Effect Size Calculations in a Temporomandibular Disorders Randomised Controlled Trial-Short Narrative Review. J. Pers. Med. 2024, 14, 655. [Google Scholar] [CrossRef] [PubMed]
- Peduzzi, P.; Concato, J.; Kemper, E.; Holford, T.R.; Feinstein, A.R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 1996, 49, 1373–1379. [Google Scholar] [CrossRef]
- Harrell, F.E., Jr. Regression Modelling Strategies: With Applications to Linear Models, Logistic Regression, and Survival Analysis, 2nd ed.; Springer: New York, NY, USA, 2015. [Google Scholar]
- Hosmer, D.W.; Lemeshow, S.; Sturdivant, R. Applied Logistic Regression, 3rd ed.; Whiley Series in Probability and Statistics; Balding, D.J., Ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2013. [Google Scholar]
- StataCorp. STATA 18.0; STATA Corporation: College Station, TX, USA, 2023. [Google Scholar]
- Edwards, R.R.; Dworkin, R.H.; Sullivan, M.D.; Turk, D.C.; Wasan, A.D. The Role of Psychosocial Processes in the Development and Maintenance of Chronic Pain. J. Pain 2016, 17 (Suppl. S9), T70–T92. [Google Scholar] [CrossRef]
- Diatchenko, L.; Fillingim, R.B.; Smith, S.B.; Maixner, W. The phenotypic and genetic signatures of common musculoskeletal pain conditions. Nat. Rev. Rheumatol. 2013, 9, 340–350. [Google Scholar] [CrossRef]
- Stewart, D.E.; Yuen, T. A systematic review of resilience in the physically ill. Psychosomatics 2011, 52, 199–209. [Google Scholar] [CrossRef]
- Ritchie, C.; Smith, A.; Sterling, M. Medical and allied health service use during acute and chronic post-injury periods in whiplash injured individuals. BMC Health Serv. Res. 2020, 20, 260. [Google Scholar] [CrossRef]

| Overall Sample | ||
|---|---|---|
| Pre-collision measures five years back | N = 740 | |
| Social assistance, N (%) | 1: No social assistance | 608 (82.2) |
| 2: >=1 week Missing data, N = 0 | 132 (17.8) | |
| Sick leave, N (%) | 1: No sick leave | 423 (57.2) |
| 2: Short term sick leave (1–12 weeks) | 178 (24.1) | |
| 3: Long term sick leave (>12 weeks) Missing data, N = 0 | 139 (18.8) | |
| Unemployment, N (%) | 1: No unemployment | 409 (55.3) |
| 2: Short term unemployment (1–52 weeks) | 204 (27.6) | |
| 3: Long term unemployment (>52 weeks) Missing data, N = 0 | 127 (17.2) | |
| Baseline measures | ||
| Sex, N (%) | Female | 474 (64.1) |
| Missing data, N = 0 | ||
| Education (vocational), N (%) | Unskilled | 150 (20.3) |
| Skilled | 231 (31.2) | |
| Further education <= 4 years Further education > 4 years | 167 (22.6) | |
| 63 (8.5) | ||
| Other | 83 (11.2) | |
| Missing data | 46 (6.2) | |
| Negative illness perceptions, mean (SD) | Range (0–3) Missing data, N = 19 (2.6%) | 0.49 (0.52) |
| Age years, mean (SD) | Range 18–67 years | 34.8 (11.4) |
| Missing data, N = 0 | ||
| Post-collision measures three-months follow-up | ||
| Negative illness perceptions, mean (SD) | Range 0–3 | 0.59 (0.68) |
| Missing data N = 206 (27.8%) | ||
| Outcome measures one-year follow-up | ||
| Considerable neck pain, N (%) | Yes | 189 (25.5) |
| Missing data | 211 (28.5) | |
| Considerable neck-related disability, N (%) | Yes | 179 (24.2) |
| Missing data | 226 (30.5) |
| Neck Pain a,b,i | Neck-Related Disability c,d,j | |||
|---|---|---|---|---|
| Social Assistance | OR (±95% CI) | p Value | OR (±95% CI) | p Value |
| 1. Social assistance before collision (≥1 week) | 1.6 (0.73; 3.6) | 0.242 | 2.5 (1.1; 5.5) | 0.029 |
| 2. Negative illness perceptions at baseline (mean) | 3.4 (2.1; 5.5) | <0.001 | 4.0 (2.4; 6.5) | <0.001 |
| 3. Interaction (illness perceptions x social assistance) | ||||
| Social assistance (≥1 week) | 0.72 (0.25; 2.1) | 0.535 | 0.55 (0.18; 1.6) | 0.278 |
| Neck pain a,e,i | Neck-related disability c,f,j | |||
| Sick leave | OR (±95% CI) | p value | OR (±95% CI) | p value |
| 1. No sick leave before collision Short term sick leave (1–12 weeks) | 0.94 (0.44; 2.0) | 0.862 | 0.99 (0.46; 2.1) | 0.986 |
| Long term sick leave (>12 weeks) | 2.5 (1.1; 5.8) | 0.029 | 2.6 (1.1; 6.2) | 0.029 |
| 2. Negative illness perceptions at baseline (mean) | 2.2 (1.2; 3.8) | 0.006 | 2.8 (1.6; 4.8) | <0.001 |
| 3. Interaction (illness perceptions × sick leave) | ||||
| Short term sick leave (1–12 weeks) Long term sick leave (>12 weeks) | 1.9 (0.64; 5.8) 4.2 (0.91; 18.9) | 0.242 0.066 | 1.5 (0.49; 4.5) 3.0 (0.64; 14.2) | 0.480 0.163 |
| Neck pain a,g,i | Neck-related disability c,h,j | |||
| Unemployment | OR (±95% CI) | p value | OR (±95% CI) | p value |
| 1. No unemployment before collision | ||||
| Short term unemployment (1–52 weeks) | 1.0 (0.51; 2.1) | 0.930 | 0.84 (0.40; 1.8) | 0.634 |
| Long term unemployment (>52 weeks) | 1.2 (0.53; 2.5) | 0.716 | 1.3 (0.58; 2.9) | 0.527 |
| 2. Negative illness perceptions at baseline (mean) | 2.8 (1.6; 5.1) | <0.001 | 3.4 (1.9; 6.2) | <0.001 |
| 3. Interaction (illness perceptions × unemployment) | ||||
| Short term unemployment (1–52 weeks) | 1.0 (0.39; 2.7) | 0.959 | 1.1 (0.40; 3.1) | 0.846 |
| Long term unemployment (>52 weeks) | 2.2 (0.59; 7.9) | 0.243 | 1.2 (0.34; 4.8) | 0.710 |
| Neck Pain a,b,i | Neck-Related Disability c,d,j | |||
|---|---|---|---|---|
| Social Assistance | OR (±95% CI) | p Value | OR (±95% CI) | p Value |
| 1. Social assistance before collision (≥1 week) | 1.8 (0.73; 4.4) | 0.202 | 1.9 (0.78; 4.8) | 0.158 |
| 2. Negative illness perceptions at 3-months FU (mean) | 6.1 (3.8; 9.6) | <0.001 | 6.5 (4.0; 10.5) | <0.001 |
| 3. Interaction (illness perceptions × social assistance) | ||||
| Social assistance (≥1 week) | 0.52 (0.21; 1.3) | 0.176 | 0.69 (0.24; 2.0) | 0.494 |
| Neck pain a,e,i | Neck-related disability c,f,j | |||
| Sick leave | OR (±95% CI) | p value | OR (±95% CI) | p value |
| 1. No sick leave before collision Short term sick leave (1–12 weeks) | ||||
| 0.92 (0.39; 2.2) | 0.853 | 1.1 (0.45; 2.7) | 0.830 | |
| Long term sick leave (>12 weeks) | 2.3 (0.92; 5.6) | 0.074 | 6.0 (2.5; 14.5) | <0.001 |
| 2. Negative illness perceptions at 3-month FU (mean) | 4.0 (2.2; 7.1) | <0.001 | 7.6 (3.9; 14.6) | <0.001 |
| 3. Interaction (illness perceptions × sick leave) | ||||
| Short term sick leave (1–12 weeks) Long term sick leave (>12 weeks) | 1.2 (0.46; 3.0) 3.2 (0.81; 12.6) | 0.727 0.094 | 0.71 (0.25; 2.1) 0.54 (0.18; 1.6) | 0.530 0.278 |
| Neck pain a,g,i | Neck-related disability c,h,j | |||
| Unemployment | OR (±95% CI) | p value | OR (±95% CI) | p value |
| 1. No unemployment before collision | ||||
| Short term unemployment (1–52 weeks) | 1.7 (0.75; 3.8) | 0.205 | 0.76 (0.31; 1.8) | 0.545 |
| Long term unemployment (>52 weeks) | 1.1 (0.45; 2.8) | 0.809 | 1.1 (0.47; 2.7) | 0.785 |
| 2. Negative illness perceptions at 3-month FU (mean) | 6.1 (3.4; 10.8) | <0.001 | 6.1 (3.3; 11.1) | <0.001 |
| 3. Interaction (illness perceptions × unemployment) | ||||
| Short term unemployment (1–52 weeks) | 0.66 (0.26; 1.7) | 0.384 | 1.3 (0.46; 4.0) | 0.591 |
| Long term unemployment (>52 weeks) | 0.91 (0.34; 2.4) | 0.842 | 0.78 (0.28; 2.2) | 0.640 |
| Pre-Collision Measures Five-Years Back | Non-Missing on the Three Measures N = 444 (60%) | Missing on at Least One of the Three Measures * N = 296 (40%) | χ2 Test | |||
|---|---|---|---|---|---|---|
| χ2 | df | p | ||||
| Social assistance, N (%) | 1: No social assistance | 383 (86.3) | 225 (76.0) | |||
| 2: ≥1 week Missing data, N = 0 | 61 (13.7) | 71 (24.0) | 12.7 | 1 | <0.001 | |
| Sick leave, N (%) | 1: No sick leave | 269 (60.6) | 154 (52.0) | |||
| 2: Short term sick leave (1–12 weeks) | 99 (22.3) | 79 (26.7) | ||||
| 3: Long term sick leave (>12 weeks) Missing data, N = 0 | 76 (17.1) | 63 (21.3) | 5.3 | 2 | 0.069 | |
| Unemployment, N (%) | 1: No unemployment | 260 (58.6) | 149 (50.3) | |||
| 2: Short term unemployment (1–52 weeks) | 106 (23.9) | 98 (33.1) | ||||
| 3: Long term unemployment (>52 weeks) Missing data, N = 0 | 78 (17.6) | 49 (16.6) | 7.8 | 2 | 0.021 | |
| Mann Whitney’s U test | ||||||
| Baseline measures | U | z | p | |||
| Age years, mean (SD) | Missing data N = 0 | 36.2 (11.8) | 32.7 (10.6) | 8,115,428.00 | 3.9 | <0.0001 |
| Negative illness perceptions at baseline, mean (SD) | Missing data N = 19 | 0.46 (0.48) | 0.54 (0.58) | 7,372,178.33 | −0.765 | 0.4445 |
| χ2 test | ||||||
| χ2 | df | p | ||||
| Sex, N (%) | Female | 304 (68.5) | 170 (57.4) | |||
| Male Missing data N = 0 | 140 (31.5) | 126 (42.6) | 9.4 | 1 | 0.002 | |
| Education (vocational), N (%) | Unskilled | 75 (18.1) | 75 (26.8) | |||
| Skilled | 141 (34.1) | 90 (32.1) | ||||
| Further education ≤ 4 years Further education > 4 years | 114 (27.5) | 53 (18.9) | ||||
| 40 (9.7) | 23 (8.2) | |||||
| Other | 44 (10.6) | 39 (13.9) | 13.0 | 4 | 0.011 | |
| Missing data N = 46 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carstensen, T.B.W.; Ravn, S.L.; Andersen, T.E.; Sæther, S.M.M.; Ørnbøl, E.; Wellnitz, K.B.; Kasch, H.; Frostholm, L. Do Acute Illness Perceptions Moderate the Association of Pre-Collision Welfare Benefits and Later Neck Pain or Disability Following Whiplash Trauma? A Prospective Multicentre Cohort Study. J. Clin. Med. 2024, 13, 7072. https://doi.org/10.3390/jcm13237072
Carstensen TBW, Ravn SL, Andersen TE, Sæther SMM, Ørnbøl E, Wellnitz KB, Kasch H, Frostholm L. Do Acute Illness Perceptions Moderate the Association of Pre-Collision Welfare Benefits and Later Neck Pain or Disability Following Whiplash Trauma? A Prospective Multicentre Cohort Study. Journal of Clinical Medicine. 2024; 13(23):7072. https://doi.org/10.3390/jcm13237072
Chicago/Turabian StyleCarstensen, Tina B. W., Sophie L. Ravn, Tonny E. Andersen, Solbjørg M. M. Sæther, Eva Ørnbøl, Kaare B. Wellnitz, Helge Kasch, and Lisbeth Frostholm. 2024. "Do Acute Illness Perceptions Moderate the Association of Pre-Collision Welfare Benefits and Later Neck Pain or Disability Following Whiplash Trauma? A Prospective Multicentre Cohort Study" Journal of Clinical Medicine 13, no. 23: 7072. https://doi.org/10.3390/jcm13237072
APA StyleCarstensen, T. B. W., Ravn, S. L., Andersen, T. E., Sæther, S. M. M., Ørnbøl, E., Wellnitz, K. B., Kasch, H., & Frostholm, L. (2024). Do Acute Illness Perceptions Moderate the Association of Pre-Collision Welfare Benefits and Later Neck Pain or Disability Following Whiplash Trauma? A Prospective Multicentre Cohort Study. Journal of Clinical Medicine, 13(23), 7072. https://doi.org/10.3390/jcm13237072







