Unveiling the Impact of Moderate and Severe Atopic Dermatitis: Insights on Burden, Clinical Characteristics, and Healthcare Resource Utilization in Adult Greek Patients from the APOLO Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Patient Disposition
3.2. Patient and Disease Characteristics
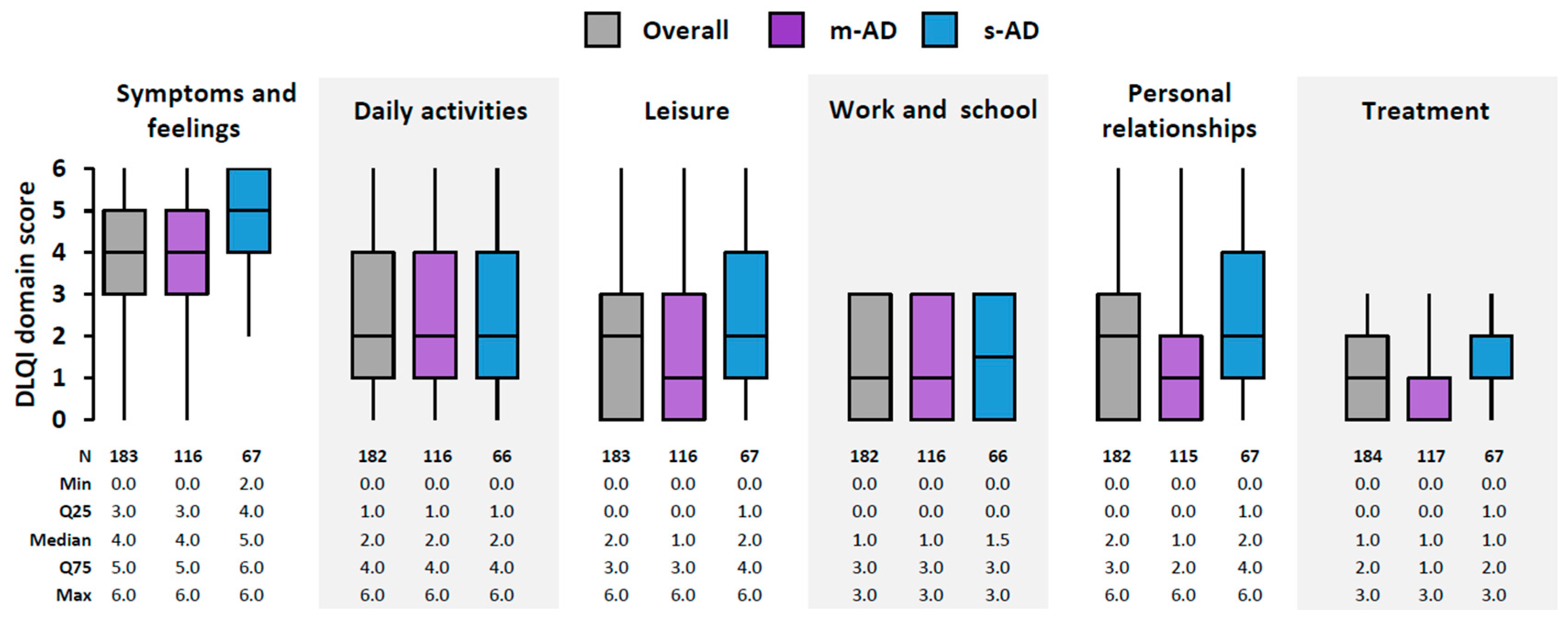
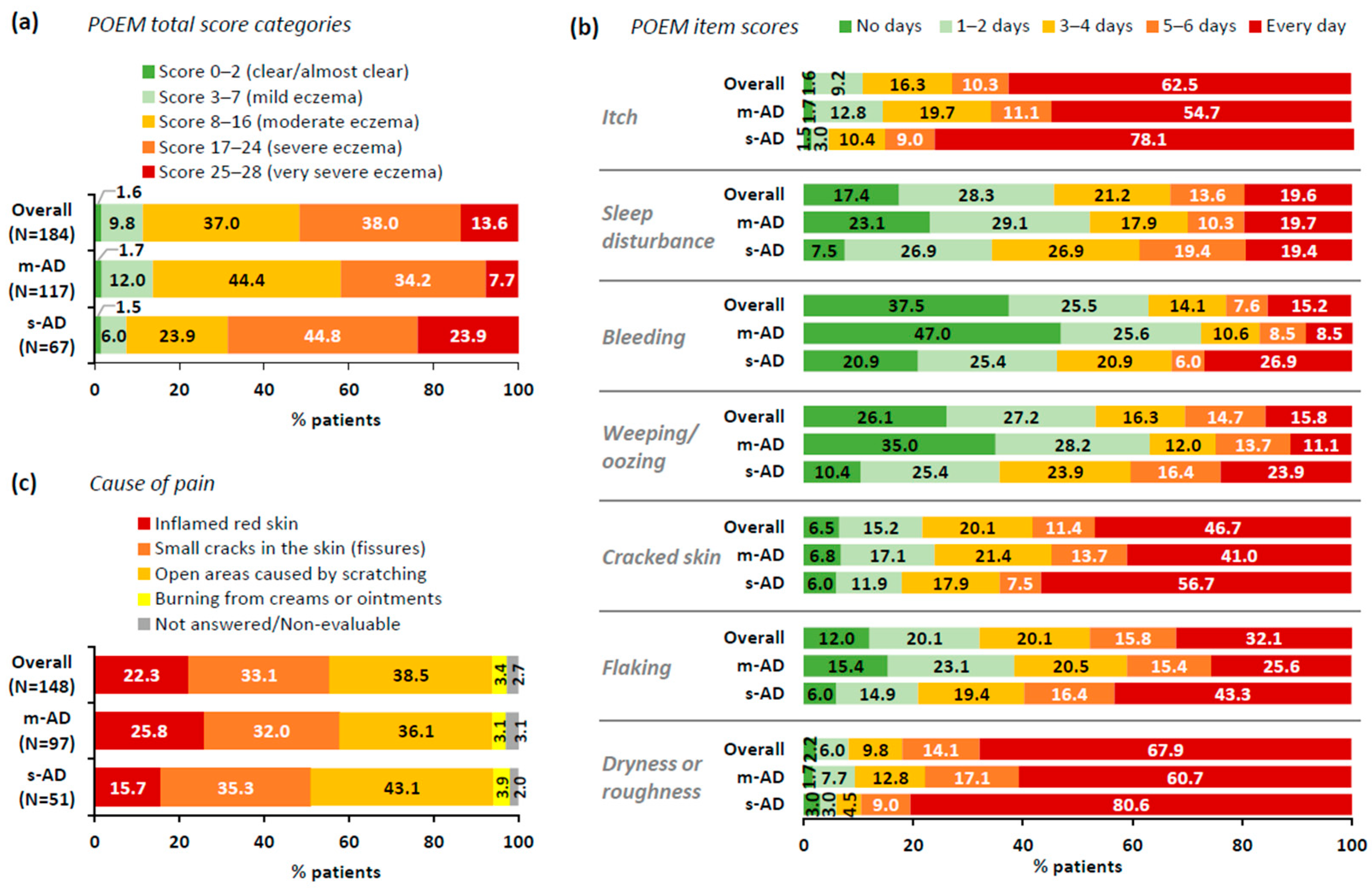
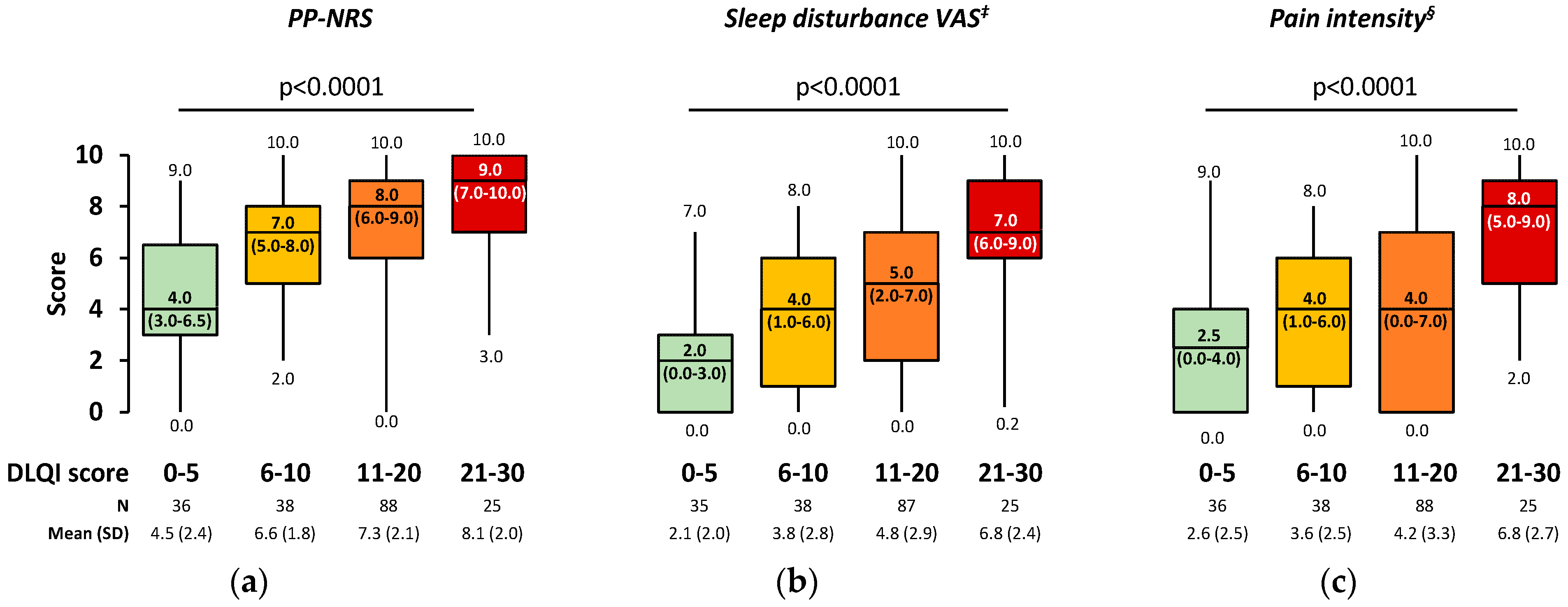
3.3. Dermatology-Specific Burden
3.4. Health-Related QoL (HRQoL)
3.5. Work Productivity and Activity Impairment
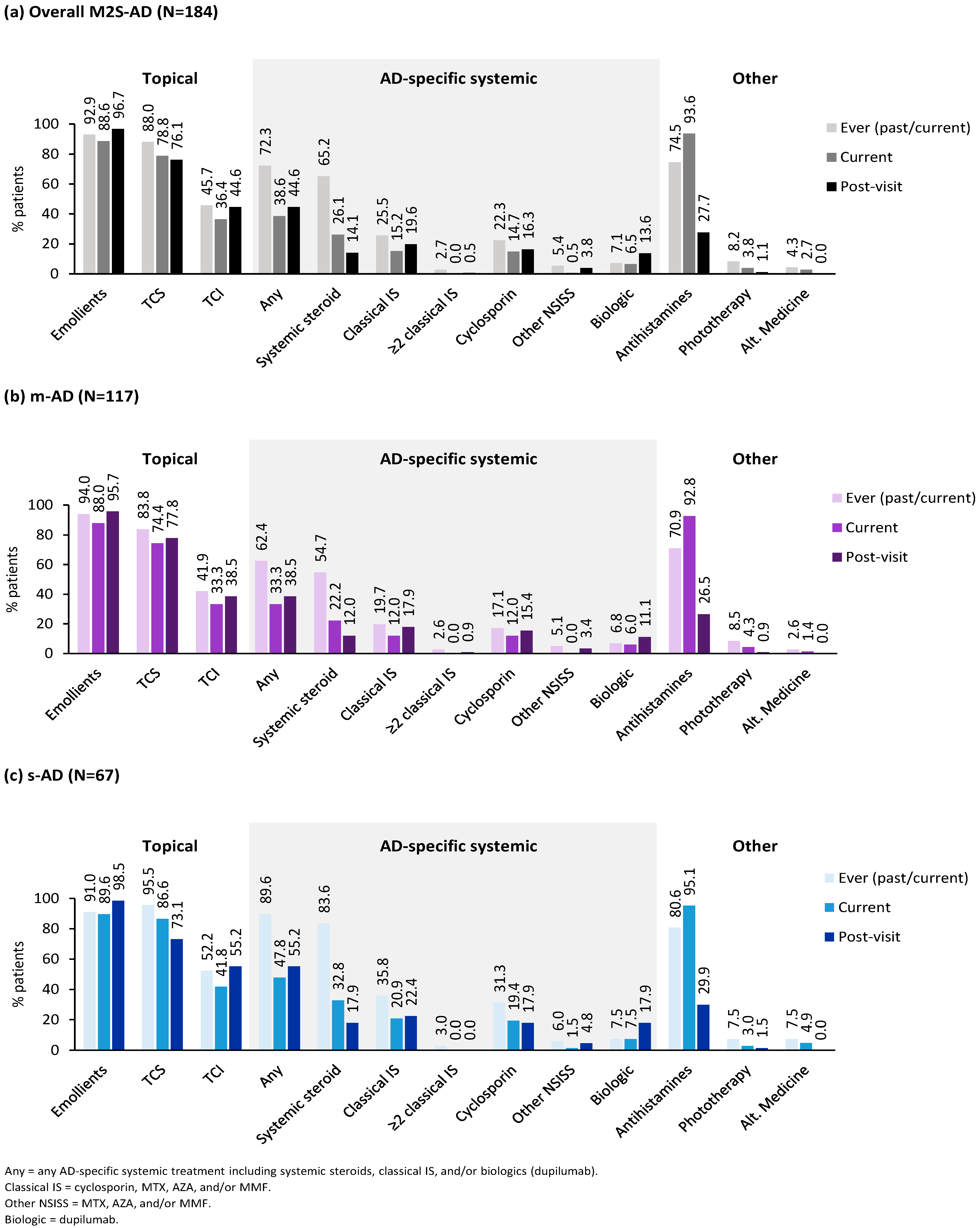
3.6. Treatments
3.7. AD-Related HCRU
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Silverberg, J.I. Atopic Dermatitis in Adults. Med. Clin. North Am. 2020, 104, 157–176. [Google Scholar] [CrossRef] [PubMed]
- Augustin, M.; Misery, L.; von Kobyletzki, L.; Armario-Hita, J.C.; Mealing, S.; Redding, M. Unveiling the true costs and societal impacts of moderate-to-severe atopic dermatitis in Europe. J. Eur. Acad. Dermatol. Venereol. 2022, 36 (Suppl. 7), 3–16. [Google Scholar] [CrossRef] [PubMed]
- Bylund, S.; Kobyletzki, L.B.; Svalstedt, M.; Svensson, Å. Prevalence and Incidence of Atopic Dermatitis: A Systematic Review. Acta Derm. Venereol. 2020, 100, adv00160. [Google Scholar] [CrossRef] [PubMed]
- Stefanou, G.; Gregoriou, S.; Kontodimas, S.; Sfaelos, K.; Vakirlis, E.; Kourlaba, G. Prevalence of adult self-reported atopic dermatitis in Greece: Results from a nationwide survey. Eur. J. Dermatol. 2022, 32, 597–606. [Google Scholar] [CrossRef]
- Weidinger, S.; Beck, L.A.; Bieber, T.; Kabashima, K.; Irvine, A.D. Atopic dermatitis. Nat. Rev. Dis. Primers 2018, 4, 1. [Google Scholar] [CrossRef]
- Leung, D.Y. New insights into atopic dermatitis: Role of skin barrier and immune dysregulation. Allergol. Int. 2013, 62, 151–161. [Google Scholar] [CrossRef]
- Hadi, H.A.; Tarmizi, A.I.; Khalid, K.A.; Gajdács, M.; Aslam, A.; Jamshed, S. The Epidemiology and Global Burden of Atopic Dermatitis: A Narrative Review. Life 2021, 11, 936. [Google Scholar] [CrossRef]
- Brunner, P.M.; Silverberg, J.I.; Guttman-Yassky, E.; Paller, A.S.; Kabashima, K.; Amagai, M.; Luger, T.A.; Deleuran, M.; Werfel, T.; Eyerich, K.; et al. Increasing Comorbidities Suggest that Atopic Dermatitis Is a Systemic Disorder. J. Investig. Dermatol. 2017, 137, 18–25. [Google Scholar] [CrossRef]
- Davis, D.M.R.; Drucker, A.M.; Alikhan, A.; Bercovitch, L.; Cohen, D.E.; Darr, J.M.; Eichenfield, L.F.; Frazer-Green, L.; Paller, A.S.; Silverberg, J.I.; et al. American Academy of Dermatology Guidelines: Awareness of comorbidities associated with atopic dermatitis in adults. J. Am. Acad. Dermatol. 2022, 86, 1335–1336.e1318. [Google Scholar] [CrossRef]
- Silverberg, J.I. Comorbidities and the impact of atopic dermatitis. Ann. Allergy Asthma Immunol. 2019, 123, 144–151. [Google Scholar] [CrossRef]
- Silverberg, J.I. Associations between atopic dermatitis and other disorders. F1000Research 2018, 7, 303. [Google Scholar] [CrossRef] [PubMed]
- Yew, Y.W.; Thyssen, J.P.; Silverberg, J.I. A systematic review and meta-analysis of the regional and age-related differences in atopic dermatitis clinical characteristics. J. Am. Acad. Dermatol. 2019, 80, 390–401. [Google Scholar] [CrossRef] [PubMed]
- Hanifin, J.M.; Thurston, M.; Omoto, M.; Cherill, R.; Tofte, S.J.; Graeber, M. The eczema area and severity index (EASI): Assessment of reliability in atopic dermatitis. EASI Evaluator Group. Exp. Dermatol. 2001, 10, 11–18. [Google Scholar] [CrossRef] [PubMed]
- Narla, S.; Silverberg, J.I. Which Clinical Measurement Tools for Atopic Dermatitis Severity Make the Most Sense in Clinical Practice? Dermatitis 2023, 35, S13–S23. [Google Scholar] [CrossRef]
- Andersen, L.; Nyeland, M.E.; Nyberg, F. Higher self-reported severity of atopic dermatitis in adults is associated with poorer self-reported health-related quality of life in France, Germany, the U.K. and the U.S.A. Br. J. Dermatol. 2020, 182, 1176–1183. [Google Scholar] [CrossRef]
- Eckert, L.; Gupta, S.; Amand, C.; Gadkari, A.; Mahajan, P.; Gelfand, J.M. Impact of atopic dermatitis on health-related quality of life and productivity in adults in the United States: An analysis using the National Health and Wellness Survey. J. Am. Acad. Dermatol. 2017, 77, 274–279.e273. [Google Scholar] [CrossRef]
- Gregoriou, S.; Stefanou, G.; Kontodimas, S.; Sfaelos, K.; Zavali, M.; Vakirlis, E.; Kourlaba, G. Burden of Atopic Dermatitis in Adults in Greece: Results from a Nationwide Survey. J. Clin. Med. 2022, 11, 4777. [Google Scholar] [CrossRef]
- Kleyn, C.E.; Barbarot, S.; Reed, C.; Losi, S.; von Arx, L.B.; Robert, C.; Anderson, P.; Grond, S.; Costanzo, A. Burden of Moderate to Severe Atopic Dermatitis in Adults from France, Italy, and the UK: Patient-Reported Outcomes and Treatment Patterns. Dermatol. Ther. 2022, 12, 1947–1965. [Google Scholar] [CrossRef]
- Girolomoni, G.; Luger, T.; Nosbaum, A.; Gruben, D.; Romero, W.; Llamado, L.J.; DiBonaventura, M. The Economic and Psychosocial Comorbidity Burden Among Adults with Moderate-to-Severe Atopic Dermatitis in Europe: Analysis of a Cross-Sectional Survey. Dermatol. Ther. 2021, 11, 117–130. [Google Scholar] [CrossRef]
- Ständer, S.; Simpson, E.L.; Guttman-Yassky, E.; Thyssen, J.P.; Kabashima, K.; Ball, S.G.; Rueda, M.J.; DeLozier, A.M.; Silverberg, J.I. Clinical Relevance of Skin Pain in Atopic Dermatitis. J. Drugs Dermatol. 2020, 19, 921–926. [Google Scholar] [CrossRef]
- Simpson, E.L.; Guttman-Yassky, E.; Margolis, D.J.; Feldman, S.R.; Qureshi, A.; Hata, T.; Mastey, V.; Wei, W.; Eckert, L.; Chao, J.; et al. Association of Inadequately Controlled Disease and Disease Severity With Patient-Reported Disease Burden in Adults With Atopic Dermatitis. JAMA Dermatol. 2018, 154, 903–912. [Google Scholar] [CrossRef] [PubMed]
- Wittkowski, A.; Richards, H.L.; Griffiths, C.E.; Main, C.J. The impact of psychological and clinical factors on quality of life in individuals with atopic dermatitis. J. Psychosom. Res. 2004, 57, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Wittkowski, A.; Richards, H.L.; Griffiths, C.E.; Main, C.J. Illness perception in individuals with atopic dermatitis. Psychol. Health Med. 2007, 12, 433–444. [Google Scholar] [CrossRef]
- Silverberg, J.I.; Gelfand, J.M.; Margolis, D.J.; Boguniewicz, M.; Fonacier, L.; Grayson, M.H.; Chiesa Fuxench, Z.C.; Simpson, E.L.; Ong, P.Y. Pain Is a Common and Burdensome Symptom of Atopic Dermatitis in United States Adults. J. Allergy Clin. Immunol. Pract. 2019, 7, 2699–2706.e2697. [Google Scholar] [CrossRef] [PubMed]
- Vakharia, P.P.; Chopra, R.; Sacotte, R.; Patel, K.R.; Singam, V.; Patel, N.; Immaneni, S.; White, T.; Kantor, R.; Hsu, D.Y.; et al. Burden of skin pain in atopic dermatitis. Ann. Allergy Asthma Immunol. 2017, 119, 548–552.e543. [Google Scholar] [CrossRef] [PubMed]
- Silverberg, J.I.; DeLozier, A.; Sun, L.; Thyssen, J.P.; Kim, B.; Yosipovitch, G.; Nunes, F.P.; Gugiu, P.C.; Doll, H.A.; Eichenfield, L.F. Psychometric properties of the itch numeric rating scale, skin pain numeric rating scale, and atopic dermatitis sleep scale in adult patients with moderate-to-severe atopic dermatitis. Health Qual. Life Outcomes 2021, 19, 247. [Google Scholar] [CrossRef]
- Thyssen, J.P.; Buhl, T.; Fernández-Peñas, P.; Kabashima, K.; Chen, S.; Lu, N.; DeLozier, A.M.; Casillas, M.; Ständer, S. Baricitinib Rapidly Improves Skin Pain Resulting in Improved Quality of Life for Patients with Atopic Dermatitis: Analyses from BREEZE-AD1, 2, and 7. Dermatol. Ther. 2021, 11, 1599–1611. [Google Scholar] [CrossRef]
- Ring, J.; Zink, A.; Arents, B.W.M.; Seitz, I.A.; Mensing, U.; Schielein, M.C.; Wettemann, N.; de Carlo, G.; Fink-Wagner, A. Atopic eczema: Burden of disease and individual suffering—Results from a large EU study in adults. J. Eur. Acad. Dermatol. Venereol. 2019, 33, 1331–1340. [Google Scholar] [CrossRef]
- Andersen, L.; Nyeland, M.E.; Nyberg, F. Increasing severity of atopic dermatitis is associated with a negative impact on work productivity among adults with atopic dermatitis in France, Germany, the U.K. and the U.S.A. Br. J. Dermatol. 2020, 182, 1007–1016. [Google Scholar] [CrossRef]
- Whiteley, J.; Emir, B.; Seitzman, R.; Makinson, G. The burden of atopic dermatitis in US adults: Results from the 2013 National Health and Wellness Survey. Curr. Med. Res. Opin. 2016, 32, 1645–1651. [Google Scholar] [CrossRef]
- Shrestha, S.; Miao, R.; Wang, L.; Chao, J.; Yuce, H.; Wei, W. Burden of Atopic Dermatitis in the United States: Analysis of Healthcare Claims Data in the Commercial, Medicare, and Medi-Cal Databases. Adv. Ther. 2017, 34, 1989–2006. [Google Scholar] [CrossRef] [PubMed]
- Drucker, A.M.; Qureshi, A.A.; Amand, C.; Villeneuve, S.; Gadkari, A.; Chao, J.; Kuznik, A.; Bégo-Le-Bagousse, G.; Eckert, L. Health Care Resource Utilization and Costs Among Adults with Atopic Dermatitis in the United States: A Claims-Based Analysis. J. Allergy Clin. Immunol. Pract. 2018, 6, 1342–1348. [Google Scholar] [CrossRef] [PubMed]
- Wollenberg, A.; Barbarot, S.; Bieber, T.; Christen-Zaech, S.; Deleuran, M.; Fink-Wagner, A.; Gieler, U.; Girolomoni, G.; Lau, S.; Muraro, A.; et al. Consensus-based European guidelines for treatment of atopic eczema (atopic dermatitis) in adults and children: Part I. J. Eur. Acad. Dermatol. Venereol. 2018, 32, 657–682. [Google Scholar] [CrossRef] [PubMed]
- Wollenberg, A.; Kinberger, M.; Arents, B.; Aszodi, N.; Avila Valle, G.; Barbarot, S.; Bieber, T.; Brough, H.A.; Calzavara Pinton, P.; Christen-Zäch, S.; et al. European guideline (EuroGuiDerm) on atopic eczema: Part I—Systemic therapy. J. Eur. Acad. Dermatol. Venereol. 2022, 36, 1409–1431. [Google Scholar] [CrossRef]
- Müller, S.; Maintz, L.; Bieber, T. Treatment of atopic dermatitis: Recently approved drugs and advanced clinical development programs. Allergy 2024, 79, 1501–1515. [Google Scholar] [CrossRef]
- Schneider, S.; Li, L.; Zink, A. The New Era of Biologics in Atopic Dermatitis: A Review. Dermatol. Pract. Concept. 2021, 11, e2021144. [Google Scholar] [CrossRef]
- Siafaka, V.; Zioga, A.; Evrenoglou, T.; Mavridis, D.; Tsabouri, S. Illness perceptions and quality of life in families with child with atopic dermatitis. Allergol. Et Immunopathol. 2020, 48, 603–611. [Google Scholar] [CrossRef]
- Simpson, E.; Bissonnette, R.; Eichenfield, L.F.; Guttman-Yassky, E.; King, B.; Silverberg, J.I.; Beck, L.A.; Bieber, T.; Reich, K.; Kabashima, K.; et al. The Validated Investigator Global Assessment for Atopic Dermatitis (vIGA-AD): The development and reliability testing of a novel clinical outcome measurement instrument for the severity of atopic dermatitis. J. Am. Acad. Dermatol. 2020, 83, 839–846. [Google Scholar] [CrossRef]
- Finlay, A.Y.; Khan, G.K. Dermatology Life Quality Index (DLQI)--a simple practical measure for routine clinical use. Clin. Exp. Dermatol. 1994, 19, 210–216. [Google Scholar] [CrossRef]
- Basra, M.K.; Fenech, R.; Gatt, R.M.; Salek, M.S.; Finlay, A.Y. The Dermatology Life Quality Index 1994–2007: A comprehensive review of validation data and clinical results. Br. J. Dermatol. 2008, 159, 997–1035. [Google Scholar] [CrossRef]
- Hongbo, Y.; Thomas, C.L.; Harrison, M.A.; Salek, M.S.; Finlay, A.Y. Translating the science of quality of life into practice: What do dermatology life quality index scores mean? J. Investig. Dermatol. 2005, 125, 659–664. [Google Scholar] [CrossRef] [PubMed]
- EuroQol--a new facility for the measurement of health-related quality of life. Health Policy 1990, 16, 199–208. [CrossRef] [PubMed]
- Yfantopoulos, J.N.; Chantzaras, A.E. Validation and comparison of the psychometric properties of the EQ-5D-3L and EQ-5D-5L instruments in Greece. Eur. J. Health Econ. 2017, 18, 519–531. [Google Scholar] [CrossRef] [PubMed]
- Charman, C.R.; Venn, A.J.; Williams, H.C. The Patient-Oriented Eczema Measure: Development and Initial Validation of a New Tool for Measuring Atopic Eczema Severity From the Patients’ Perspective. Arch. Dermatol. 2004, 140, 1513–1519. [Google Scholar] [CrossRef]
- Charman, C.R.; Venn, A.J.; Ravenscroft, J.C.; Williams, H.C. Translating Patient-Oriented Eczema Measure (POEM) scores into clinical practice by suggesting severity strata derived using anchor-based methods. Br. J. Dermatol. 2013, 169, 1326–1332. [Google Scholar] [CrossRef]
- Gerbens, L.A.; Prinsen, C.A.; Chalmers, J.R.; Drucker, A.M.; von Kobyletzki, L.B.; Limpens, J.; Nankervis, H.; Svensson, Å.; Terwee, C.B.; Zhang, J.; et al. Evaluation of the measurement properties of symptom measurement instruments for atopic eczema: A systematic review. Allergy 2017, 72, 146–163. [Google Scholar] [CrossRef]
- Yosipovitch, G.; Reaney, M.; Mastey, V.; Eckert, L.; Abbé, A.; Nelson, L.; Clark, M.; Williams, N.; Chen, Z.; Ardeleanu, M.; et al. Peak Pruritus Numerical Rating Scale: Psychometric validation and responder definition for assessing itch in moderate-to-severe atopic dermatitis. Br. J. Dermatol. 2019, 181, 761–769. [Google Scholar] [CrossRef]
- Reilly, M.C.; Zbrozek, A.S.; Dukes, E.M. The validity and reproducibility of a work productivity and activity impairment instrument. PharmacoEconomics 1993, 4, 353–365. [Google Scholar] [CrossRef]
- Prasad, M.; Wahlqvist, P.; Shikiar, R.; Shih, Y.C. A review of self-report instruments measuring health-related work productivity: A patient-reported outcomes perspective. PharmacoEconomics 2004, 22, 225–244. [Google Scholar] [CrossRef]
- Severity scoring of atopic dermatitis: The SCORAD index. Consensus Report of the European Task Force on Atopic Dermatitis. Dermatology 1993, 186, 23–31. [CrossRef]
- Guidelines for good pharmacoepidemiology practice (GPP). Pharmacoepidemiol. Drug Saf. 2016, 25, 2–10. [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Luger, T.; Romero, W.A.; Gruben, D.; Smith, T.W.; Cha, A.; Neary, M.P. Clinical and Humanistic Burden of Atopic Dermatitis in Europe: Analyses of the National Health and Wellness Survey. Dermatol. Ther. 2022, 12, 949–969. [Google Scholar] [CrossRef] [PubMed]
- Offidani, A.; Stingeni, L.; Neri, I.; Cipriani, F.; Chen, Z.; Rossi, A.B.; Lu, Y.; Moretti, D. Dupilumab treatment induced similar improvements in signs, symptoms, and quality of life in adults with moderate-to-severe atopic dermatitis with baseline Eczema Area and Severity Index Score <24 or ≥24. Ital. J. Dermatol. Venereol. 2022, 157, 39–46. [Google Scholar] [CrossRef]
- Chiesa Fuxench, Z.C.; Block, J.K.; Boguniewicz, M.; Boyle, J.; Fonacier, L.; Gelfand, J.M.; Grayson, M.H.; Margolis, D.J.; Mitchell, L.; Silverberg, J.I.; et al. Atopic Dermatitis in America Study: A Cross-Sectional Study Examining the Prevalence and Disease Burden of Atopic Dermatitis in the US Adult Population. J. Investig. Dermatol. 2019, 139, 583–590. [Google Scholar] [CrossRef]
- Long, Q.; Jin, H.; You, X.; Liu, Y.; Teng, Z.; Chen, Y.; Zhu, Y.; Zeng, Y. Eczema is a shared risk factor for anxiety and depression: A meta-analysis and systematic review. PLoS ONE 2022, 17, e0263334. [Google Scholar] [CrossRef]
- Silverberg, J.I. Validity and reliability of a novel numeric rating scale to measure skin-pain in adults with atopic dermatitis. Arch. Dermatol. Res. 2021, 313, 855–861. [Google Scholar] [CrossRef]
- Storck, M.; Sandmann, S.; Bruland, P.; Pereira, M.P.; Steinke, S.; Riepe, C.; Soto-Rey, I.; Garcovich, S.; Augustin, M.; Blome, C.; et al. Pruritus Intensity Scales across Europe: A prospective validation study. J. Eur. Acad. Dermatol. Venereol. 2021, 35, 1176–1185. [Google Scholar] [CrossRef]
- Augustin, M.; Costanzo, A.; Pink, A.; Seneschal, J.; Schuster, C.; Mert, C.; Guerreiro, M.; Tietz, N.; Grond, S.; De Bruin-Weller, M. Real-World Treatment Patterns and Treatment Benefits among Adult Patients with Atopic Dermatitis: Results from the Atopic Dermatitis Patient Satisfaction and Unmet Need Survey. Acta Derm. Venereol. 2022, 102, adv00830. [Google Scholar] [CrossRef]
- Yosipovitch, G.; Gooderham, M.J.; Ständer, S.; Fonacier, L.; Szepietowski, J.C.; Deleuran, M.; Girolomoni, G.; Su, J.C.; Bushmakin, A.G.; Cappelleri, J.C.; et al. Interpreting the Relationship Among Itch, Sleep, and Work Productivity in Patients with Moderate-to-Severe Atopic Dermatitis: A Post Hoc Analysis of JADE MONO-2. Am. J. Clin. Dermatol. 2023, 25, 127–138. [Google Scholar] [CrossRef]
- Patruno, C.; Napolitano, M.; Argenziano, G.; Peris, K.; Ortoncelli, M.; Girolomoni, G.; Offidani, A.; Ferrucci, S.M.; Amoruso, G.F.; Rossi, M.; et al. Dupilumab therapy of atopic dermatitis of the elderly: A multicentre, real-life study. J. Eur. Acad. Dermatol. Venereol. 2021, 35, 958–964. [Google Scholar] [CrossRef] [PubMed]
- Patruno, C.; Fabbrocini, G.; Longo, G.; Argenziano, G.; Ferrucci, S.M.; Stingeni, L.; Peris, K.; Ortoncelli, M.; Offidani, A.; Amoruso, G.F.; et al. Effectiveness and Safety of Long-Term Dupilumab Treatment in Elderly Patients with Atopic Dermatitis: A Multicenter Real-Life Observational Study. Am. J. Clin. Dermatol. 2021, 22, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Wollenberg, A.; Weidinger, S.; Worm, M.; Bieber, T. Tralokinumab in atopic dermatitis. J. Der Dtsch. Dermatol. Ges. 2021, 19, 1435–1442. [Google Scholar] [CrossRef]
- Silverberg, J.I.; Thyssen, J.P.; Simpson, E.L.; Yosipovitch, G.; Ständer, S.; Valdez, H.; Rojo, R.; Biswas, P.; Myers, D.E.; Feeney, C.; et al. Impact of Oral Abrocitinib Monotherapy on Patient-Reported Symptoms and Quality of Life in Adolescents and Adults with Moderate-to-Severe Atopic Dermatitis: A Pooled Analysis of Patient-Reported Outcomes. Am. J. Clin. Dermatol. 2021, 22, 541–554. [Google Scholar] [CrossRef]
- Simpson, E.L.; Bieber, T.; Guttman-Yassky, E.; Beck, L.A.; Blauvelt, A.; Cork, M.J.; Silverberg, J.I.; Deleuran, M.; Kataoka, Y.; Lacour, J.P.; et al. Two Phase 3 Trials of Dupilumab versus Placebo in Atopic Dermatitis. N. Engl. J. Med. 2016, 375, 2335–2348. [Google Scholar] [CrossRef]
- Long, D.; Bonsel, G.J.; Lubetkin, E.I.; Yfantopoulos, J.N.; Janssen, M.F.; Haagsma, J.A. Health-Related Quality of Life and Mental Well-Being during the COVID-19 Pandemic in Five Countries: A One-Year Longitudinal Study. J. Clin. Med. 2022, 11, 6467. [Google Scholar] [CrossRef]
- Rogers, A.M.; Lauren, B.N.; Woo Baidal, J.A.; Ozanne, E.M.; Hur, C. Persistent effects of the COVID-19 pandemic on diet, exercise, risk for food insecurity, and quality of life: A longitudinal study among U.S. adults. Appetite 2021, 167, 105639. [Google Scholar] [CrossRef]
- Colucci, E.; Nadeau, S.; Higgins, J.; Kehayia, E.; Poldma, T.; Saj, A.; de Guise, E. COVID-19 lockdowns’ effects on the quality of life, perceived health and well-being of healthy elderly individuals: A longitudinal comparison of pre-lockdown and lockdown states of well-being. Arch. Gerontol. Geriatr. 2022, 99, 104606. [Google Scholar] [CrossRef]
- Pieh, C.; Budimir, S.; Humer, E.; Probst, T. Comparing Mental Health During the COVID-19 Lockdown and 6 Months After the Lockdown in Austria: A Longitudinal Study. Front. Psychiatry 2021, 12, 625973. [Google Scholar] [CrossRef]

| Overall (N = 184) | m-AD (N = 117) | s-AD (N = 67) | ||
|---|---|---|---|---|
| Sociodemographic and anthropometric characteristics at the study visit * | ||||
| Age (years) | median (IQR) | 38.8 (24.7–52.7) | 39.2 (25.2–52.7) | 38.4 (24.3–52.5) |
| <65, n (%) | 164 (89.1) | 105 (89.7) | 59 (88.1) | |
| Female, n (%) | 94 (51.1) | 64 (54.7) | 30 (44.8) | |
| BMI (kg/m2), median (IQR) ** | 25.0 (22.2–27.8) | 24.8 (21.5–27.9) | 25.3 (22.7–27.2) | |
| BMI classification, n (%) | Underweight (BMI < 18.5 kg/m2) | 4 (2.2) | 3 (2.6) | 1 (1.5) |
| Normal (18.5 ≤ BMI < 25 kg/m2) | 87 (47.3) | 57 (48.7) | 30 (44.8) | |
| Overweight (25 ≤ BMI < 30 kg/m2) | 65 (35.3) | 38 (32.5) | 27 (40.3) | |
| Obese (BMI ≥ 30 kg/m2) | 27 (14.7) | 18 (15.4) | 9 (13.4) | |
| Missing/Not assessed | 1 (0.5) | 1 (0.9) | . | |
| Smoking (current), n (%) | 52 (28.3) | 30 (25.6) | 22 (32.8) | |
| Family history and physician-diagnosed comorbidities of interest | ||||
| Family history of AD and/or other allergic conditions, n (%) | 101 (54.9) | 65 (55.6) | 36 (53.7) | |
| History of allergic comorbidity (allergic rhinitis/allergic conjunctivitis/asthma/food allergy), n (%) | Any | 109 (59.2) | 65 (55.6) | 44 (65.7) |
| Allergic rhinitis | 82 (44.6) | 46 (39.3) | 36 (53.7) | |
| Allergic conjunctivitis | 63 (34.2) | 35 (29.9) | 28 (41.8) | |
| Asthma | 46 (25.0) | 24 (20.5) | 22 (32.8) | |
| Food allergy | 27 (14.7) | 15 (12.8) | 12 (17.9) | |
| Depression or anxiety disorder, n (%) | 49 (26.6) | 25 (21.4) | 24 (35.8) | |
| Anxiety disorder, n (%) | 42 (22.8) | 23 (19.7) | 19 (28.4) | |
| Contact dermatitis, n (%) | 41 (22.3) | 26 (22.2) | 15 (22.4) | |
| History of Herpes simplex infections, n (%) | 33 (17.9) | 21 (17.9) | 12 (17.9) | |
| Hypertension, n (%) | 27 (14.7) | 17 (14.5) | 10 (14.9) | |
| History of skin infections (requiring antibiotics), n (%) | 25 (13.6) | 12 (10.3) | 13 (19.4) | |
| Depression, n (%) | 20 (10.9) | 10 (8.5) | 10 (14.9) | |
| Diabetes, n (%) | 10 (5.4) | 7 (6.0) | 3 (4.5) | |
| Alopecia areata, n (%) | 9 (4.9) | 8 (6.8) | 1 (1.5) | |
| History of Herpes zoster infections, n (%) | 8 (4.3) | 4 (3.4) | 4 (6.0) | |
| Inflammatory bowel disease, n (%) | 6 (3.3) | 5 (4.3) | 1 (1.5) | |
| History of venous thromboembolism (VTE), n (%) | 2 (1.1) | . | 2 (3.0) | |
| Cancer, n (%) | 1 (0.5) | 1 (0.9) | . | |
| History of cerebrovascular accident (stroke), n (%) | 1 (0.5) | 1 (0.9) | . | |
| Disease characteristics | ||||
| Age at onset of AD (years) | median (IQR) | 19.0 (5.5–39.1) | 19.7 (6.3–37.4) | 16.4 (4.6–45.6) |
| ≥18, n (%) | 97 (52.7) | 65 (55.6) | 32 (47.8) | |
| Time from onset to diagnosis (months), median (IQR) | 1.9 (0.0–21.2) | 0.5 (0.0–12.0) | 12.0 (0.0–26.3) | |
| Disease duration (from onset to study visit) (years), median (IQR) | 11.8 (4.5–25.7) | 12.1 (5.1–26.1) | 11.5 (4.1–22.3) | |
| AD-affected BSA at the study visit (%), median (IQR) | 30.0 (20.0–40.0) | 22.0 (15.0–40.0) | 40.0 (30.0–60.0) | |
| Face/neck involvement at the study visit | face, n (%) | 123 (66.8) | 78 (66.7) | 45 (67.2) |
| neck, n (%) | 91 (49.5) | 52 (44.4) | 39 (58.2) | |
| Total EASI score at the study visit | mean (SD) | 18.7 (10.1) | 12.7 (4.2) | 29.2 (8.8) |
| median (IQR) | 16.9 (10.4–23.4) | 12.6 (8.9–16.2) | 26.0 (22.8–32.4) | |
| vIGA-AD at the study visit | 3, n (%) | 125 (67.9) | 97 (82.9) | 28 (41.8) |
| 4, n (%) | 59 (32.1) | 20 (17.1) | 39 (58.2) | |
| History of flare-ups in the last year | median (IQR) | 3.0 (2.0–6.0) | 3.0 (2.0–6.0) | 3.0 (3.0–6.0) |
| ≥1 flare-up(s), n (%) | 176 (95.7) | 113 (96.6) | 63 (94.0) | |
| ≥3 flare-up(s), n (%) | 127 (69.0) | 76 (65.0) | 51 (76.2) | |
| ≥10 flare-ups, n (%) | 30 (16.3) | 19 (16.2) | 11 (16.4) | |
| OLS Estimates (of Mean DLQI Total Score) | |||||
|---|---|---|---|---|---|
| n | Crude Betas (95% CI) | p-Value | Adjusted Betas (95% CI) | p-Value | |
| EASI score | 187 * | 0.18 (0.09–0.27) | <0.001 | 0.12 (0.00–0.23) † | 0.044 |
| PP-NRS total score | 187 * | 1.34 (0.97–1.71) | <0.001 | 1.11 (0.74–1.47) ‡ | <0.001 |
| Sleep disturbance (VAS) | 185 ** | 1.10 (0.80–1.39) | <0.001 | 0.96 (0.67–1.26) ‡ | <0.001 |
| Pain intensity NRS score | 187 * | 0.87 (0.57–1.16) | <0.001 | 0.64 (0.34–0.94) ‡ | <0.001 |
| Overall (N = 184) | m-AD (N = 117) | s-AD (N = 67) | ||
|---|---|---|---|---|
| All patients | ||||
| Employed, n | 112 | 72 | 40 | |
| Absenteeism | Completion rate, % (n/N) | 97.3 (109/112) | 95.8 (69/72) | 100.0 (40/40) |
| Mean (SD) score, % | 4.9 (12.0) | 4.9 (14.1) | 4.7 (7.2) | |
| Median (IQR) score, % | 0.0 (0.0–4.8) | 0.0 (0.0–2.0) | 0.0 (0.0–6.0) | |
| Presenteeism | Completion rate, % (n/N) | 99.1 (111/112) | 98.6 (71/72) | 100.0 (40/40) |
| Mean (SD) score, % | 27.1 (26.3) | 25.8 (27.0) | 29.5 (25.3) | |
| Median (IQR) score, % | 20.0 (0.0–40.0) | 20.0 (0.0–40.0) | 20.0 (10.0–45.0) | |
| Work productivity loss | Completion rate, % (n/N) | 97.3 (109/112) | 95.8 (69/72) | 100.0 (40/40) |
| Mean (SD) score, % | 29.8 (27.3) | 28.0 (28.5) | 32.8 (25.2) | |
| Median (IQR) score, % | 23.8 (2.4–50.0) | 20.0 (0.0–46.6) | 26.9 (10.0–51.0) | |
| Activity impairment | Completion rate, % (n/N) | 100.0 (184/184) | 100.0 (117/117) | 100.0 (67/67) |
| Mean (SD) score, % | 34.2 (30.0) | 29.5 (28.6) | 42.4 (30.7) | |
| Median (IQR) score, % | 30.0 (5.0–60.0) | 20.0 (0.0–50.0) | 40.0 (20.0–70.0) | |
| Patients reporting any work productivity loss/activity impairment | ||||
| Absenteeism | Patients reporting absenteeism, % (n/N) | 34.9 (38/109) | 27.5 (19/69) | 47.5 (19/40) |
| Mean (SD) score, % | 13.9 (17.1) | 17.9 (22.5) | 9.9 (7.6) | |
| Median (IQR) score, % | 7.0 (4.8–21.1) | 11.1 (4.0–23.7) | 6.5 (4.8–14.3) | |
| Presenteeism | Patients reporting presenteeism, % (n/N) | 71.2 (79/111) | 66.2 (47/71) | 80.0 (32/40) |
| Mean (SD) score, % | 38.1 (23.5) | 38.9 (24.2) | 36.9 (22.9) | |
| Median (IQR) score, % | 30.0 (20.0–60.0) | 30.0 (20.0–60.0) | 30.0 (20.0–55.0) | |
| Work productivity loss | Patients reporting work productivity loss, % (n/N) | 75.2 (82/109) | 69.6 (48/69) | 85.0 (34/40) |
| Mean (SD) score, % | 39.6 (24.5) | 40.3 (25.9) | 38.6 (22.7) | |
| Median (IQR) score, % | 33.3 (20.0–60.0) | 34.1 (20.0–60.0) | 31.7 (22.0–55.6) | |
| Activity impairment | Patients reporting activity impairment, % (n/N) | 75.0 (138/184) | 70.9 (83/117) | 82.1 (55/67) |
| Mean (SD) score, % | 45.6 (26.0) | 41.6 (25.5) | 51.6 (25.8) | |
| Median (IQR) score, % | 40.0 (20.0–70.0) | 40.0 (20.0–60.0) | 50.0 (30.0–70.0) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stratigos, A.J.; Chasapi, V.; Katoulis, A.; Vakirlis, E.; Psarros, F.; Georgiou, S.; Vourdas, D.; Makris, M.; Lazaridou, E.; Gregoriou, S.; et al. Unveiling the Impact of Moderate and Severe Atopic Dermatitis: Insights on Burden, Clinical Characteristics, and Healthcare Resource Utilization in Adult Greek Patients from the APOLO Cross-Sectional Study. J. Clin. Med. 2024, 13, 6327. https://doi.org/10.3390/jcm13216327
Stratigos AJ, Chasapi V, Katoulis A, Vakirlis E, Psarros F, Georgiou S, Vourdas D, Makris M, Lazaridou E, Gregoriou S, et al. Unveiling the Impact of Moderate and Severe Atopic Dermatitis: Insights on Burden, Clinical Characteristics, and Healthcare Resource Utilization in Adult Greek Patients from the APOLO Cross-Sectional Study. Journal of Clinical Medicine. 2024; 13(21):6327. https://doi.org/10.3390/jcm13216327
Chicago/Turabian StyleStratigos, Alexander J., Vasiliki Chasapi, Alexander Katoulis, Efstratios Vakirlis, Fotios Psarros, Sophia Georgiou, Dimitrios Vourdas, Michael Makris, Elizabeth Lazaridou, Stamatios Gregoriou, and et al. 2024. "Unveiling the Impact of Moderate and Severe Atopic Dermatitis: Insights on Burden, Clinical Characteristics, and Healthcare Resource Utilization in Adult Greek Patients from the APOLO Cross-Sectional Study" Journal of Clinical Medicine 13, no. 21: 6327. https://doi.org/10.3390/jcm13216327
APA StyleStratigos, A. J., Chasapi, V., Katoulis, A., Vakirlis, E., Psarros, F., Georgiou, S., Vourdas, D., Makris, M., Lazaridou, E., Gregoriou, S., Skiadas, I., Nakou, M., Koulias, C., & APOLO Study Group. (2024). Unveiling the Impact of Moderate and Severe Atopic Dermatitis: Insights on Burden, Clinical Characteristics, and Healthcare Resource Utilization in Adult Greek Patients from the APOLO Cross-Sectional Study. Journal of Clinical Medicine, 13(21), 6327. https://doi.org/10.3390/jcm13216327








