Abstract
(1) Background: Our aim was to determine changes in the prevalence of physical activity (PA) in adults with asthma between 2014 and 2020 in Spain, investigate sex differences and the effect of other variables on adherence to PA, and compare the prevalence of PA between individuals with and without asthma. (2) Methods: This study was a cross-sectional, population-based, matched, case–control study using European Health Interview Surveys for Spain (EHISS) for 2014 and 2020. (3) Results: We identified 1262 and 1103 patients with asthma in the 2014 and 2020 EHISS, respectively. The prevalence of PA remained stable (57.2% vs. 55.7%, respectively), while the percentage of persons who reported walking continuously for at least 2 days a week increased from 73.9% to 82.2% (p < 0.001). Male sex, younger age, better self-rated health, and lower body mass index (BMI) were significantly associated with greater PA. From 2014 to 2020, the number of walking days ≥2 increased by 64% (OR1.64 95%CI 1.34–2.00). Asthma was associated with less PA (OR0.87 95%CI 0.47–0.72) and a lower number of walking days ≥2 (OR0.84 95%0.72–0.97). (4) Conclusions: Walking frequency improved over time among people with asthma. Differences in PA were detected by age, sex, self-rated health status, and BMI. Asthma was associated with less LTPA and a lower number of walking days ≥2.
1. Introduction
Asthma is a common disease characterized by airflow limitation and respiratory symptoms associated with chronic airway and systemic inflammation, bronchial hyperreactivity, and exercise-induced bronchoconstriction. It is associated with a serious health burden, underscoring the importance of symptom management and disease control [1]. Thus, once the diagnosis of asthma has been made, treatment should begin to control symptoms and reduce the risk of exacerbation. Pharmacological stepwise therapy is the first line of treatment for asthma. Current treatment guidelines for this disease highlight management with inhaled corticosteroids alone or in combination with a long-acting beta-agonist [2,3,4]. Severe forms of asthma may require other pharmacological strategies and biological therapies and may even need hospitalization and ventilatory support [5,6,7]. Recent controversy has been raised regarding the use of ketamine in severe asthma exacerbations. However, a recent review does not support the use of this drug as so far, and a limited number of prospective studies have been published with large heterogeneity [5]. Biological therapies include monoclonal antibodies directed to key inflammatory cytokines involved in asthma pathogenesis [6]. The use of noninvasive ventilation is recommended for severe asthma as it may prevent the need for endotracheal intubation in selected patients; this is important since patients who have been intubated for severe asthma are at increased risk of death [7]. Nevertheless, optimal asthma control is complicated by costs, drug side effects, and a lack of adherence to prescribed medication. Poor adherence to prescribed medication necessitates more frequent emergency treatment, thus increasing health system costs [2,3,4].
Different non-pharmacological therapeutic approaches can also improve the symptoms of patients with asthma, but in many cases they are not applied [8]. Although their potential benefits have not been sufficiently studied [9,10], current guidelines recommend that patients with asthma undertake regular physical activity (PA) [11,12]. Engaging in leisure time PA (LTPA) has proven to be a cost-effective strategy, as it improves symptoms, asthma control, pulmonary function, health-related quality of life, and use of health services [9,13,14]. Thus, PA is an important outcome that should be assessed in patients with asthma [15].
Despite the benefits described, population-based studies have revealed that patients with asthma engage in less PA than those without asthma [16], probably owing to several barriers, including fear of exercise-induced bronchoconstriction [17], a transitory condition that occurs in 40% to 90% of people with asthma and causes airway narrowing during or after exercise [1,17,18]. Several pharmacologic approaches can be adopted to prevent this phenomenon, with bronchodilators representing the mainstay approach [19]. However, patients suffering from exercise-induced bronchoconstriction may limit or avoid exertion due to symptoms of shortness of breath, cough, wheezing, and chest tightness. This could have negative consequences for their health, since exercise avoidance may increase social isolation, and this can lead to obesity and poor health. In fact, exercise has paradoxically been shown to improve exercise-induced bronchoconstriction severity, pulmonary function, and airway inflammation in these patients. Early detection, diagnosis confirmed by the change in lung function during exercise, and appropriate treatment can improve their quality of life, allowing patients with asthma to perform PA without limitations [20].
Psychological issues and lack of motivation have been also reported as barriers to PA in patients with asthma. Applying behavior change techniques as part of a PA program may help overcome the mentioned barriers and facilitate PA in these patients [21].
Identifying changes in the PA of patients with asthma over time and associated factors make it imperative to conduct health promotion activities and lifestyle interventions in those at risk of low PA and, therefore, reduce health disparities. We aimed to determine whether the prevalence of PA in adults with asthma changed between 2014 and 2020 in Spain. We also investigated possible sex differences and the effect of other sociodemographic and health-related variables on adherence to PA among adults with asthma. Finally, we compared the prevalence of PA between individuals with asthma and age- and sex-matched individuals without this condition.
2. Materials and Methods
We conducted an observational study encompassing both cross-sectional and case–control designs. The data utilized for this research were sourced from the European Health Interview Survey for Spain (EHISS) corresponding to the years 2014 and 2020. These surveys are undertaken on a representative sample of the Spanish population comprising over 22,000 individuals aged ≥15 years residing in private households.
The recruitment periods spanned 12 months to account for seasonal variability, namely January to December 2014 for EHISS 2014 and July 2019 to June 2020 for EHISS 2020. Data collection was facilitated through face-to-face interviews with participants in their homes. Owing to the COVID-19 pandemic, data collection transitioned to telephone interviews between March and July 2020. Detailed information regarding the EHISS can be accessed online [22,23].
The EHISS uses a three-stage random sampling method to ensure nationwide and autonomous community representation. The final sampling level is the household, where, if multiple individuals aged ≥15 years reside, a single participant is randomly selected from the inhabitants.
Our study population comprised all individuals from both surveys aged 18 years and above. The analysis excluded participants who either did not respond or answered “I don’t know” to questions concerning asthma and the PA questions.
For the case–control study, each participant with asthma (case) from the study population was paired with a participant without asthma (control) matched by survey year, sex, and age. When multiple controls were available for a case, one was chosen at random.
2.1. Study Variables
All variables in this study are based on self-reported responses to questions in the 2014 and 2020 EHISS questionnaires. Supplementary Table S1 elucidates the survey questions, possible answers, and their categorization for the creation of variables.
Participants were classified as having asthma if they answered “Yes” to the question, “Have you been diagnosed with asthma by a physician?” Those who answered “No” were considered not to have asthma.
Our study outcomes were the frequency and type of PA during free time and the number of days the person interviewed walked for at least 10 consecutive minutes in a week.
The two questions utilized to quantify PA were as follows:
- (1)
- What frequency of physical activity do you engage in during your free time? There were four potential responses: (i) I do not exercise. My leisure time is primarily sedentary. (ii) I engage in occasional physical or sports activities (e.g., walking, cycling, gardening, light gymnastics, recreational activities requiring minimal effort). (iii) I participate in physical activities several times a month (e.g., sports, gymnastics, running, swimming, cycling, team games). (iv) I undergo athletic or physical training multiple times a week. Based on these responses, the variable “leisure time physical activity” (LTPA) was created and classified into two categories: “None” for those who selected the first option, and “Occasional or frequent” for any of the other three choices.
- (2)
- In a typical week, how many days do you walk for at least 10 consecutive minutes? Participants could respond within a range of zero to seven days. This led to the definition of the variable “Number of walking Days”, categorized as “None or one” and “Two or more”.
Table S1 also lists all the covariates analyzed, including sociodemographic characteristics, self-perceived health status, self-declared chronic illnesses diagnosed by a physician, alcohol consumption, current smoking habits, and body mass index (BMI), which was calculated using participant-provided weight and height data.
2.2. Statistical Analysis
Descriptive statistics for the study population included absolute and relative frequencies and means and standard deviations for quantitative variables. Proportions were compared using Fisher’s exact test for unpaired data and McNemar’s test for paired data. Mean differences were analyzed using the t test.
Multivariable logistic regression models were constructed to identify variables associated with LTPA and “number of walking days” among individuals with asthma. Two additional models evaluated the impact of self-reported asthma (outcome variable) on the PA variables, adjusting for other covariates and aiming to confirm the results of the matching method. Models were created following the guidelines suggested by Hosmer et al. [24] with four consecutive steps.
(1) Univariate analysis of each variable. (2) Selection of variables for multivariable model. We included variables that showed statistical significance in the univariate tests and those deemed scientifically relevant based on the reviewed literature or prior research. The inclusion of scientifically relevant variables, despite their statistical significance, ensured that the model was grounded in theoretical or empirical evidence. (3) Fit and refinement of the multivariable model. Post the initial model fitting, the significance of each variable included in the model was scrutinized with the Wald statistic, which tested the significance of individual coefficients in the model. Each variable’s coefficient in the multivariate model was compared with its coefficient in a univariate model. Variables that did not contribute meaningfully (as indicated by statistical tests and theoretical relevance) were removed. The model was then refitted, and this process of elimination and refitting continued until a robust model was achieved. The likelihood ratio test was used for comparing the fit of the new model against the previous versions, ensuring the retained variables were essential. (4) Final assessment of the model: Once a stable model was established, we assessed the linearity of the relationships and checked for interaction effects among variables.
It is important to remember that while this approach helps in understanding associations, it does not imply causation.
As a measure of association, the odds ratio (OR) with the 95% confidence interval (CI) was calculated.
All statistical analyses were conducted using STATA 14.0 (StataCorp LP., College Station, TX, USA).
2.3. Ethical Considerations
The anonymized EHISS datasets are freely accessible on the Ministry of Health’s website, obviating the need for ethics committee evaluation [25].
3. Results
The total number of individuals with asthma interviewed in EHISS 2014 and EHISS 2020 was 1262 and 1103, respectively. In both surveys, women represented approximately 60%. The mean age increased slightly from 52.7 to 54.1 years (p = 0.073). As shown in Table 1, almost half of the participants with asthma perceived their health as fair/poor/very poor. If we analyze the two surveys together, we find that the most frequently self-reported comorbidities were high blood pressure (32.6%), chronic obstructive pulmonary disease (24.5%), and mental disorders (23.9%). Regarding lifestyles, 24.2% were obese (BMI ≥ 30), 20.5% smoked, and 52.3% consumed alcohol. None of these variables changed in frequency from 2014 to 2020.

Table 1.
Distribution according to study variables of participants in the European Health Interview Surveys for Spain (EHISS) conducted in the years 2014 and 2020, with self-reported asthma.
The prevalence of occasional or frequent LTPA remained stable, with values of 57.2% in EHISS2014 and 55.7% in EHISS2020 (p = 0.45), and the proportion of individuals with asthma who reported walking continuously for at least two days a week increased significantly from 73.9% to 82.2% (p < 0.001).
Figure 1 shows the prevalence of occasional or frequent LTPA and the number of walking days ≥2 according to sex. Women with asthma reported less PA, measured with either of the two study variables, in both surveys. Analysis by age group (Figure 2) showed that both occasional and frequent LTPA and the number of walking days ≥2 decreased with age in 2014 and 2020.
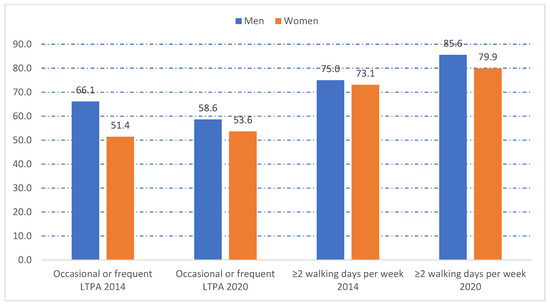
Figure 1.
Frequency of occasional or frequent leisure time physical activity (LTPA) and number of walking days per week ≥2 according to sex among participants in the European Health Interview Surveys for Spain (EHISS) conducted in years 2014 and 2020, with self-reported asthma. LTPA: leisure time physical activity. All differences between men and women were statistically significant (p < 0.01).
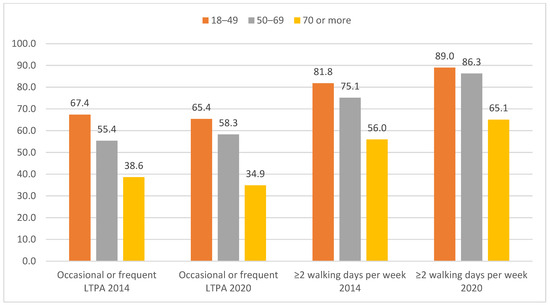
Figure 2.
Frequency of occasional or frequent leisure time physical activity (LTPA) and number of walking days per week ≥2 according to age groups among participants in the European Health Interview Surveys for Spain (EHISS) conducted in the years 2014 and 2020, with self-reported asthma. LTPA: leisure time physical activity. Age was associated with occasional or frequent LTPA and ≥2 walking days per week in both surveys (p < 0.01).
Table 2 compares the prevalence of occasional or frequent LTPA and the number of walking days ≥2 between individuals with asthma and their age- and sex-matched controls according to sociodemographic variables. For all the categories of these covariables, individuals with asthma reported lower values for occasional or frequent LTPA and number of walking days ≥2 than controls. Among individuals with asthma, a higher educational level was associated with a higher prevalence of the two PA variables.

Table 2.
Occasional or frequent leisure time physical activity and number of walking days per week ≥2 among subjects with asthma and sex/age-matched subjects without asthma participants in the European Health Interview Surveys for Spain (EHISS) conducted in the years 2014 and 2020 according to socio-demographic variables.
Table 3 shows the prevalence of occasional or frequent LTPA in individuals with asthma in the EHISS for 2014 and 2020 and their matched controls stratified by self-rated health, comorbidities, and lifestyles. Individuals with asthma had significantly lower prevalence values for occasional or frequent LTPA than the matched controls in all the covariables studied except self-rated health of very good/good and current smoking, where no difference was found. The lowest levels of occasional or frequent LTPA among the asthma population were observed in those who reported stroke (28.8%), heart disease (35.3%), and diabetes (37.2%). On the other hand, the highest prevalence was found among those who self-rated their health as very good/good (69.9%) followed by those with the lowest BMI (63%).

Table 3.
Occasional or frequent leisure time physical activity among subjects with asthma and sex/age-matched subjects without asthma participants in the European Health Interview Surveys for Spain (EHISS) conducted in the years 2014 and 2020 according to clinical variables and lifestyles.
Table 4 shows the prevalence of “number of walking days ≥2” in individuals with asthma in the EHISS for 2014 and 2020 and their matched controls stratified by self-rated health, comorbidities, and lifestyles. The prevalence of “number of walking days ≥2” among individuals with asthma was lower than among controls without asthma for heart disease (57.7% vs. 63.1%; p < 0.01), stroke (47.9% vs. 54.9%; p < 0.01), cancer (66.6% vs. 72.3%; p < 0.01), mental disorders (59.6% vs. 61.8%; p = 0.017), high blood pressure (69.2% vs. 74.7%; p < 0.01), and BMI > 30 (68.7% vs. 76.6%; p < 0.01).

Table 4.
Number of walking days per week ≥2 among subjects with asthma and sex/age-matched subjects without asthma participants in the European Health Interview Surveys for Spain (EHISS) conducted in the years 2014 and 2020 according to clinical variables and lifestyles.
The results of the multivariable analysis to identify variables associated with occasional or frequent LTPA and the number of walking days ≥2 among participants with asthma are shown in Table 5. Male sex, younger age, better self-rated health status, and lower BMI were significantly associated with more PA measured using both study variables. Of the comorbidities studied, only heart disease was associated with less PA measured according to the two variables, and mental illness was associated with a lower number of walking days ≥2. Smoking at the time of the survey was associated with less LTPA. The analysis of changes between 2014 and 2020 revealed that the number of walking days ≥2 had increased by 64% (OR 1.64 95%CI 1.34–2.00).

Table 5.
Variables associated with occasional or frequent leisure time physical activity and number of walking days per week ≥2 among participants with asthma. Results of multivariable logistic regression analysis.
The effect of having asthma, after adjusting for the remaining covariables, is shown in Table S2. Having asthma was associated with less LTPA (OR 0.87 95%CI 0.47–0.72) and a number of walking days ≥2 (OR 0.84 95%0.72–0.97).
4. Discussion
Our study revealed favorable trends in PA among patients with asthma, although these are still far from optimal. In fact, the prevalence of any type of LTPA among adult patients with asthma was low and did not change significantly over time. These findings indicate that a gap continues to exist between clinical guideline recommendations [7] and current practice, as previously reported for pharmacological treatment [26,27,28]. This may be a consequence of various barriers, both internal (lack of awareness, unfamiliarity, disagreement with the content of the guidelines, and lack of knowledge about their effectiveness) and external (patient-related or environmental factors) [29,30]. However, we demonstrated that the proportion of individuals with asthma who report walking continuously for at least two days a week was higher and increased significantly over time. The challenge that remains now is to overcome the heterogeneous and complex nature of this disease and achieve significant changes in participation in PA over time [21].
Our results are in line with previous reports that asthma patients undertake less PA than those without asthma [9,31,32] and that the level of PA in asthma is influenced by age and sex [9,33,34]. Regarding age, we observed that both LTPA and the number of walking days ≥2 decrease as age increases. Among the plausible biological mechanisms that could justify this association are the changes that affect the lungs in relation to age, which lead to an increase in breathing effort and are more marked in individuals with respiratory diseases. Furthermore, disease duration is more likely to be longer in older asthma patients, who consequently undergo a greater degree of airway remodeling [9,35]. Additionally, it has been reported that, in older asthma patients, the decrease in PA appears earlier in women than in men [36,37].
Previous studies have also reported lower PA in women than in men with asthma [38,39]. A possible explanation is that the consequences of this disease are more serious or have a more marked impact in women. In fact, among patients with asthma with a similar severity of airway obstruction, women tend to report poorer control [9].
Another factor associated with PA in our study was self-rated health status. Several studies have shown that an increase in PA improves quality of life in patients with asthma [40]. One of the reasons that could justify this association is that PA reduces the likelihood of asthma symptoms owing to cardiorespiratory adjustment to exercise, a decrease in BMI, improved self-esteem and mood, and less frequent symptoms of anxiety and depression [41]. In fact, PA and self-rated health have been shown to be related to good mental health in patients with asthma. Therefore, asthma patients who engage in PA and have a favorable self-rated health status present less psychological distress [2].
Our study also showed that a higher BMI was associated with reduced PA in asthma patients. The combination of obesity and reduced PA is associated with poor asthma control and a weaker response to treatment [42,43]. Therefore, it is necessary to take into account that obesity is associated with other chronic diseases, which, in turn, could be involved in lower PA levels [44].
Regarding comorbidity, we found that heart disease was associated with less PA measured according to the two variables and that mental illness was associated with a lower number of walking days ≥2. Comorbidities and decreased PA are especially relevant in the management of asthma because they have been shown to contribute to an increase in the likelihood of symptoms and the risk of exacerbation [45].
COPD was one of the most frequently self-reported comorbidities in patients with asthma in our study. The term “asthma–COPD overlap” (ACO) has been applied to the condition in which a person has a persistent airflow limitation with clinical features of both asthma and COPD. In the patients with asthma, the prevalence of ACO ranges between 11.1% and 61.0% [46]. Harada et al. found that the prevalence of ACO among patients who were previously diagnosed with asthma was 27.1%, a figure slightly higher than that found in our study [47]. Patients with ACO have more frequent and severe attacks, resulting in a greater number of hospitalizations, emergency visits, and higher health costs than patients with asthma and COPD [48]. Regarding PA, it has been demonstrated that more than three out of ten adults with ACO do not achieve the established recommendations. Therefore, it is recommended to implement programs that promote the importance and benefits of PA among patients with ACO, focusing especially on older adults and those who are obese [49].
Smoking was associated with less PA in our study. It has also been associated with poor asthma control and exacerbation of the disease [50]. Thus, it is important to ask patients about this harmful habit and encourage them to quit, as repeated attempts to quit smoking can reduce smoking rates significantly [51].
The strengths of this study include the utilization of a structured survey conducted during two different periods, thus allowing for comparison, as well as the large sample size assessed. However, several limitations must be considered. First, a main limitation of this work is the absence of comparative data in the same population between the two periods. The EHISS surveys are conducted every six years. Between the EHISS2014 and the EHISS2020, in the years 2016/17, the National Health Interview Survey of Spain was carried out with a similar methodology, but unfortunately, some of the variables used in the EHISS are collected with different questions, which means these surveys could not be merged for joint analysis [52]. Second, the last EHISS was carried out in 2020, the year the COVID-19 pandemic began; therefore, the lack of improvement in PA compared with the 2014 survey could have been due to social isolation during the pandemic. Third, in our investigation, we lack relevant clinical information, as it is not collected in the questionaries of the EHISS, such as which patients were being treated with inhaled corticosteroids, the severity of asthma, or the degree of control obtained. Fourth, it is well known that the presence of atopy may influence PA in terms of environmental exposure. Unfortunately, the EHISS surveys do not include atopy as one of the conditions inquired about. In any case, the EHISS surveys are conducted throughout the twelve months of the year to avoid the seasonal effect of environmental exposure on some diseases [22,23]. Fifth, population surveys lack many variables, such as those pointed out in the previous limitations, which are relevant and should be included in multivariable models in future research. In any case, the practice of PA is not usually recorded in clinical histories, and population surveys, despite their limitations, have been used to evaluate the practice of PA, from an epidemiological point of view, by various authors [2,3,31,32,39]. Sixth, as this is a cross-sectional study, it does not add information on whether the associations are causal and, if so, their significance. Seventh, as we used self-reported answers on diseases that were not confirmed with medical histories, the existence of social desirability or recall biases cannot be dismissed. Finally, the measurement of PA using questionnaires is another limitation, since it is not possible to quantify activity objectively.
5. Conclusions
In summary, although the proportion of individuals with asthma who report walking continuously for at least two days a week has increased significantly from 2014 to 2020, our study shows that the prevalence of any type of LTPA among adult patients with asthma is low and has not changed significantly over time. Male sex, younger age, better self-rated health, and lower BMI were significantly associated with more PA measured according to both study variables. Asthma was associated with less LTPA and a lower number of walking days ≥2 than in individuals who did not have asthma. Therefore, healthcare providers should identify the risk factors and clinical characteristics that are associated with reduced PA in patients with asthma and develop strategies to modify behavior and to increase PA in this population.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm13020591/s1, Table S1: Definition of variables according to the questions included in the European Health Interview Surveys in Spain conducted in years 2014 and 2020; Table S2: Variables associated with occasional or frequent leisure time physical activity and number of walking days per week ≥2 among participants in the European Health Interview Surveys in Spain conducted in the years 2014 and 2020. Results of multivariable logistic regression analysis.
Author Contributions
Conceptualization, J.D.-M.-D., C.L.-S., R.J.-G. and N.P.-F.; methodology, T.S.V. and A.L.-d.-A.; validation, D.C.-A. and F.C.; formal analysis, B.R.-G.; funding, A.L.-d.-A. and R.J.-G.; writing—original draft, J.D.-M.-D., C.L.-S. and N.P.-F.; writing—review and editing, R.J.-G., T.S.V., D.C.-A., A.L.-d.-A., F.C. and B.R.-G. All authors have read and agreed to the published version of the manuscript.
Funding
This study is part of the research funded by the Madrid Government (Comunidad de Madrid-Spain) under the Multiannual Agreement with Universidad Complutense de Madrid in the line Excellence Programme for university teaching staff, in the context of the V PRICIT (Regional Programme of Research and Technological Innovation), and by Universidad Complutense de Madrid. Grupo de Investigación en Epidemiología de las Enfermedades Crónicas de Alta Prevalencia en España (970970).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The anonymized EHISS datasets are freely accessible and can be downloaded by anyone on the Ministry of Health’s website. https://www.sanidad.gob.es/estadEstudios/estadisticas/EncuestaEuropea/home.htm (accessed on 8 October 2023). All other relevant data are included in the paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- De Lima, F.F.; Pinheiro, D.H.A.; de Carvalho, C.R.F. Physical training in adults with asthma: An integrative approach on strategies, mechanisms, and benefits. Front. Rehabil. Sci. 2023, 4, 1115352. [Google Scholar] [CrossRef] [PubMed]
- Denche-Zamorano, Á.; Urbano-Mairena, J.; Pastor-Cisneros, R.; Muñoz-Bermejo, L.; Barrios-Fernandez, S.; Garcia-Gordillo, M..; Colmenarez-Mendoza, A.; Guerra-Bustamante, J.; Mendoza-Muñoz, M. A Cross-Sectional Study on Physical Activity and Psychological Distress in Adults with Asthma. Healthcare 2022, 10, 2469. [Google Scholar] [CrossRef] [PubMed]
- Ye, W.; Li, X.; Huang, Y. Relationship Between Physical Activity and Adult Asthma Control Using NHANES 2011-2020 Data. Med. Sci. Monit. 2023, 29, e939350. [Google Scholar] [CrossRef] [PubMed]
- Kuder, M.M.; Clark, M.; Cooley, C.; Prieto-Centurion, V.; Danley, A.; Riley, I.; Siddiqi, A.; Weller, K.; Kitsiou, S.; Nyenhuis, S.M. A Systematic Review of the Effect of Physical Activity on Asthma Outcomes. J. Allergy Clin. Immunol. Pract. 2021, 9, 3407–3421.e8. [Google Scholar] [CrossRef] [PubMed]
- La Via, L.; Sanfilippo, F.; Cuttone, G.; Dezio, V.; Falcone, M.; Brancati, S.; Crimi, C.; Astuto, M. Use of ketamine in patients with refractory severe asthma exacerbations: Systematic review of prospective studies. Eur. J. Clin. Pharmacol. 2022, 78, 1613–1622. [Google Scholar] [CrossRef] [PubMed]
- Kardas, G.; Kuna, P.; Panek, M. Biological Therapies of Severe Asthma and Their Possible Effects on Airway Remodeling. Front. Immunol. 2020, 11, 1134. [Google Scholar] [CrossRef]
- Leatherman, J. Mechanical Ventilation for Severe Asthma. Chest 2015, 147, 1671–1680. [Google Scholar] [CrossRef]
- Clemente-Suárez, V.J.; Mielgo-Ayuso, J.; Ramos-Campo, D.J.; Beltran-Velasco, A.I.; Martínez-Guardado, I.; Jimenez, E.N.; Redondo-Flórez, L.; Yáñez-Sepúlveda, R.; Tornero-Aguilera, J.F. Basis of preventive and non-pharmacological interventions in asthma. Front. Public Health 2023, 11, 1172391. [Google Scholar] [CrossRef]
- Cordova-Rivera, L.; Gibson, P.G.; Gardiner, P.A.; McDonald, V.M. A Systematic Review of Associations of Physical Activity and Sedentary Time with Asthma Outcomes. J. Allergy Clin. Immunol. Pract. 2018, 6, 1968–1981.e2. [Google Scholar] [CrossRef]
- Lee, H.; Ryu, J.; Chung, S.J.; Park, D.W.; Park, T.S.; Moon, J.; Kim, T.; Sohn, J.W.; Yoon, H.J.; Kim, S. Overall and respiratory mortality reduction with physical activity in subjects with and without asthma. Allergy 2023, 78, 1677–1680. [Google Scholar] [CrossRef]
- British Thoracic Society. SIGN 158 Guidelines on the Management of Asthma: A National Clinical Guidelines. 2019. Available online: https://www.brit-thoracic.org.uk/quality-improvement/guidelines/asthma/ (accessed on 22 December 2023).
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. Updated July 2023. 2023. Available online: www.ginasthma.org (accessed on 22 December 2023).
- Hansen, E.S.H.; Pitzner-Fabricius, A.; Toennesen, L.L.; Rasmusen, H.K.; Hostrup, M.; Hellsten, Y.; Backer, V.; Henriksen, M. Effect of aerobic exercise training on asthma in adults: A systematic review and meta-analysis. Eur. Respir. J. 2020, 56, 2000146. [Google Scholar] [CrossRef] [PubMed]
- Pascual, S.; Dorado, S.; Urrutia, I. Physical Activity and Asthma. Arch. Bronconeumol. 2022, 58, 733–734. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, J.M.; Spositon, T.; Rugila, D.F.; Pitta, F.; Furlanetto, K.C. Validity of the International Physical Activity Questionnaire (short form) in adults with asthma. PLoS ONE 2023, 18, e0282137. [Google Scholar] [CrossRef] [PubMed]
- Van’t Hul, A.J.; Frouws, S.; Van Den Akker, E.; Van Lummel, R.; Starrenburg-Razenberg, A.; van Bruggen, A.; Braunstahl, G.J.; In’t Veen, J.C. Decreased physical activity in adults with bronchial asthma. Respir. Med. 2016, 114, 72–77. [Google Scholar] [CrossRef]
- Nyenhuis, S.M.; Kahwash, B.; Cooke, A.; Gregory, K.L.; Greiwe, J.; Nanda, A. Recommendations for Physical Activity in Asthma: A Work Group Report of the AAAAI Sports, Exercise, and Fitness Committee. J. Allergy Clin. Immunol. Pract. 2022, 10, 433–443. [Google Scholar] [CrossRef]
- De Lima, F.F.; Lunardi, A.C.; Pinheiro, D.H.A.; Carvalho-Pinto, R.M.; Stelmach, R.; Giavina-Bianchi, P.; Agondi, R.C.; Carvalho, C.R. Identifying the Characteristics of Responders and Nonresponders in a Behavioral Intervention to Increase Physical Activity Among Patients with Moderate to Severe Asthma: Protocol for a Prospective Pragmatic Study. JMIR Res. Protoc. 2023, 12, e49032. [Google Scholar] [CrossRef]
- Bonini, M.; Cilluffo, G.; La Grutta, S.; Boccabella, C.; Usmani, O.; Viegi, G.; Palange, P. Anti-muscarinic drugs as preventive treatment of exercise-induced bronchoconstriction (EIB) in children and adults. Respir. Med. 2020, 172, 106128. [Google Scholar] [CrossRef]
- Gerow, M.; Bruner, P.J. Exercise-Induced Asthma. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023; Last Update: 7 August 2023. [Google Scholar]
- Guerrero, P.D.U.; Gibson, P.G. A Real-World Analysis to Create Real-World Change: The Need for an Individualized Approach to Improving Physical Activity in Asthma. J. Allergy Clin. Immunol. Pract. 2023, 11, 2801–2802. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadística. European Health Interview Surveys for Spain. Available online: https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176784&menu=metodologia&idp=1254735573175 (accessed on 8 October 2023).
- Ministerio de Sanidad. European Health Survey in Spain. 2020. Available online: https://www.mscbs.gob.es/estadEstudios/estadisticas/EncuestaEuropea/Enc_Eur_Salud_en_Esp_2020.htm (accessed on 8 October 2023).
- Hosmer, D.W.; Lemeshow, S.; Sturdivant, R.X. Regresión Logística Aplicada, 3rd ed; John Wiley & Sons, Inc: Hoboken, NJ, USA, 2013. [Google Scholar]
- Ministry of Health. European Health Survey in Spain. Available online: https://www.sanidad.gob.es/estadEstudios/estadisticas/EncuestaEuropea/home.htm (accessed on 8 October 2023).
- Adams, R.J.; Fuhlbrigge, A.; Guilbert, T.; Lozano, P.; Martinez, F. Inadequate use of asthma medication in the united states: Results of the asthma in america national population survey. J. Allergy Clin. Immunol. 2002, 110, 58–64. [Google Scholar] [CrossRef]
- Lai, C.K.; de Guia, T.S.; Kim, Y.-Y.; Kuo, S.-H.; Mukhopadhyay, A.; Soriano, J.B.; Trung, P.L.; Zhong, N.S.; Zainudin, N.; Zainudin, B.M.; et al. Asthma control in the Asia-Pacific region: The asthma insights and reality in Asia-Pacific study. J. Allergy Clin. Immunol. 2003, 111, 263–268. [Google Scholar] [CrossRef]
- Cazzoletti, L.; Marcon, A.; Janson, C.; Corsico, A.; Jarvis, D.; Pin, I.; Accordini, S.; Almar, E.; Bugiani, M.; Carolei, A.; et al. Asthma control in Europe: A real-world evaluation based on an international population-based study. J. Allergy Clin. Immunol. 2007, 120, 1360–1367. [Google Scholar] [CrossRef] [PubMed]
- Cabana, M.D.; Ebel, B.E.; Cooper-Patrick, L.; Powe, N.R.; Rubin, H.R.; Rand, C.S. Barriers pediatricians face when using asthma practice guidelines. Arch. Pediatr. Adolesc. Med. 2000, 154, 685–693. [Google Scholar] [CrossRef] [PubMed]
- Cabana, M.D.; Rand, C.S.; Becher, O.J.; Rubin, H.R. Reasons for Pediatrician Nonadherence to Asthma Guidelines. Arch. Pediatr. Adolesc. Med. 2001, 155, 1057–1062. [Google Scholar] [CrossRef] [PubMed]
- Ford, E.S.; Heath, G.W.; Mannino, D.M.; Redd, S.C. Leisure-Time Physical Activity Patterns Among US Adults with Asthma. Chest 2003, 124, 432–437. [Google Scholar] [CrossRef] [PubMed]
- Teramoto, M.; Moonie, S. Physical Activity Participation among Adult Nevadans with Self-Reported Asthma. J. Asthma 2011, 48, 517–522. [Google Scholar] [CrossRef]
- Teixeira e Seabra, A.F.; Maia, J.A.; Mendonça, D.M.; Thomis, M.; Caspersen, C.J.; Fulton, J.E. Age and Sex Differences in Physical Activity of Portuguese Adolescents. Med. Sci. Sports Exerc. 2008, 40, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Gerovasili, V.; Agaku, I.T.; Vardavas, C.I.; Filippidis, F.T. Levels of physical activity among adults 18–64 years old in 28 European countries. Prev. Med. 2015, 81, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Gibson, P.G.; McDonald, V.M.; Marks, G.B. Asthma in older adults. Lancet 2010, 376, 803–813. [Google Scholar] [CrossRef]
- Chen, Y.; Dales, R.; Krewski, D. Leisure-time energy expenditure in asthmatics and non-asthmatics. Respir. Med. 2001, 95, 13–18. [Google Scholar] [CrossRef]
- Dogra, S.; Meisner, B.A.; Baker, J. Psychosocial predictors of physical activity in older aged asthmatics. Age Ageing 2008, 37, 449–454. [Google Scholar] [CrossRef][Green Version]
- O’Donoghue, G.; Perchoux, C.; Mensah, K.; Lakerveld, J.; van der Ploeg, H.; Bernaards, C.; Chastin, S.F.M.; Simon, C.; O’Gorman, D.; Nazare, J.A.; et al. A systematic review of correlates of sedentary behaviour in adults aged 18–65 years: A socio-ecological approach. BMC Public Health 2016, 16, 163. [Google Scholar] [CrossRef] [PubMed]
- Almatruk, Z.; Axon, D.R. Factors associated with frequent physical activity among United States adults with asthma. J. Asthma 2023, 60, 1237–1245. [Google Scholar] [CrossRef] [PubMed]
- Lochte, L.; Petersen, P.E.; Nielsen, K.G.; Andersen, A.; Platts-Mills, T.A.E. Associations of physical activity with childhood asthma, a population study based on the WHO-health behaviour in school-aged children survey. Asthma Res. Pract. 2018, 4, 6. [Google Scholar] [CrossRef] [PubMed]
- Denche-Zamorano, Á.; Pastor-Cisneros, R.; Moreno-Moreno, L.; Carlos-Vivas, J.; Mendoza-Muñoz, M.; Contreras-Barraza, N.; Gil-Marín, M.; Barrios-Fernández, S. Physical Activity Frequency and Health-Related Quality of Life in Spanish Children and Adolescents with Asthma: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2022, 19, 14611. [Google Scholar] [CrossRef] [PubMed]
- Jakicic, J.M.; Davis, K.K. Obesity and Physical Activity. Psychiatr. Clin. N. Am. 2011, 34, 829–840. [Google Scholar] [CrossRef] [PubMed]
- Lu, K.D.; Manoukian, K.; Radom-Aizik, S.; Cooper, D.M.; Galant, S.P. Obesity, Asthma, and Exercise in Child and Adolescent Health. Pediatr. Exerc. Sci. 2016, 28, 264–274. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Castillo, S.; Smith, L.; Díaz Suárez, A.; López Sánchez, G.F. Levels of Physical Activity in Spanish Asthmatics: A Cross-Sectional Study. Medicina 2020, 56, 643. [Google Scholar] [CrossRef]
- Freitas, P.D.; Silva, A.G.; Ferreira, P.G.; DA Silva, A.; Salge, J.M.; Carvalho-Pinto, R.M.; Cukier, A.; Brito, C.M.; Mancini, M.C.; Carvalho, C.R.F. Exercise Improves Physical Activity and Comorbidities in Obese Adults with Asthma. Med. Sci. Sports Exerc. 2018, 50, 1367–1376. [Google Scholar] [CrossRef]
- Uchida, A.; Sakaue, K.; Inoue, H. Epidemiology of asthma-chronic obstructive pulmonary disease overlap (ACO). Allergol. Int. 2018, 67, 165–171. [Google Scholar] [CrossRef]
- Harada, T.; Yamasaki, A.; Fukushima, T.; Hashimoto, K.; Takata, M.; Kodani, M.; Okazaki, R.; Takeda, K.; Watanabe, M.; Kurai, J.; et al. Causes of death in patients with asthma and asthma-chronic obstructive pulmonary disease overlap syndrome. Int. J. Chronic Obstr. Pulm. Dis. 2015, 10, 595–602. [Google Scholar] [CrossRef]
- Sevimli, N.; Yapar, D.; Turktas, H. The Prevalence of Asthma-COPD Overlap (ACO) Among Patients with Asthma. Turk. Thorac. J. 2019, 20, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Sánchez Castillo, S.; Smith, L.; Díaz Suárez, A.; López Sánchez, G.F. Physical activity behavior in people with asthma and COPD overlap residing in Spain: A cross-sectional analysis. J. Asthma 2022, 59, 917–925. [Google Scholar] [CrossRef] [PubMed]
- Yawn, B.P.; Rank, M.A.; Bertram, S.L.; Wollan, P.C. Obesity, low levels of physical activity and smoking present opportunities for primary care asthma interventions: An analysis of baseline data from The Asthma Tools Study. NPJ Prim. Care Respir. Med. 2015, 25, 15058. [Google Scholar] [CrossRef] [PubMed]
- Lemmens, V.; Oenema, A.; Knut, I.K.; Brug, J. Effectiveness of smoking cessation interventions among adults: A systematic review of reviews. Eur. J. Cancer Prev. 2008, 17, 535–544. [Google Scholar] [CrossRef]
- Instituto Nacional de Estadística. Spanish National Health Survey. 2017. Available online: https://www.sanidad.gob.es/estadEstudios/estadisticas/encuestaNacional/encuesta2017.htm (accessed on 8 January 2024).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).