Abstract
The objective was to explore the associations between patient involvement in the rehabilitation process and improvements in function and goal attainment in the first year after rehabilitation. The longitudinal multicenter study RehabNytte provided data from participants who had been referred to rehabilitation (n = 2113). Quality indicator (QI) pass rates (% yes) were used to assess patient involvement in the rehabilitation process. The Patient-Specific Functional Scale (PSFS) (10 = best possible) was used to assess function. The outcome QI on goal achievement (response options of yes/no) was used to assess goal attainment. Logistic regression and paired sample t-tests were used to examine associations and mean changes in function from rehabilitation admission up to 3, 6, and 12 months. Most participants (95%) were involved in goal-setting, which was positively associated with younger age (OR 0.97, 95% CI 0.95–0.99) and female sex (OR 1.87, 95% CI 1.15–3.02). Function improved over the follow-up period, with greater improvements in the active goal-setting group. Being involved in goal planning almost tripled the odds of goal attainment (OR 2.78, 95% CI 1.60–4.83) and involvement in the rehabilitation plan almost doubled it (OR 1.99, 95% CI 1.41–2.81). Most participants were involved in rehabilitation goal-setting/planning and being involved was associated with beneficial functional outcomes and greater goal attainment.
1. Introduction
A participatory healthcare approach is considered important for enhancing the quality of healthcare services [1]. Patient engagement (PE) is part of this approach. PE can be described as facilitating processes that strengthen the capacity for patients to be actively involved in decisions about their care [2] and include active involvement at different levels of healthcare [3]. The micro-level is suggested to include direct care, involving person-to-person collaboration, for example, between patients and healthcare professionals. At the micro-level, patients are involved in their own health decisions such as goal-setting processes. The meso-level refers to the involvement of patients as representatives in the development and delivery of healthcare services and systems, such as structural healthcare attributes, processual activities, tasks, and behaviors of the involved stakeholders. PE at the meso-level is often organized into patient advisory boards, councils, or forums [4,5]. As co-creators of political incentives at the macro-level, patient representatives often represent patient organizations or patient advocacy groups to highlight the groups’ special interests [5].
Even if patient involvement is considered a criterion for the quality of healthcare services [6], meaningful involvement faces several barriers [7]. Patients’ health literacy and their desire to be actively involved in their health vary and healthcare professionals have reported a lack of knowledge regarding the implementation of PE [8]. Additionally, healthcare systems often lack the necessary structures to promote PE effectively [9,10,11].
In rehabilitation processes, active involvement in goal-setting and the development of goal-driven rehabilitation plans are key components of PE at the micro-level [8,12]. The process of short- and long-term goal-setting can be patient-directed, mutually agreed upon, or staff-driven [13].
In Norway, patients have a legal right to be involved at every level of healthcare [14]. The basic assumption is that facilitating structures at the macro- and meso-levels enhances patient involvement at the micro-level, which again may be associated with improvements in functioning, goal attainment, and quality of life [15,16,17]. However, there is a lack of evidence supporting the associations between meso- and micro-level PE and additional research is needed [11]. Hence, the aim of this study was to explore the possible associations between demographic characteristics and patient involvement in setting rehabilitation goals and between patient-reported involvement in the rehabilitation process (reflecting the implementation of meso-level structures) and the changes in function and goal attainment in the first year after rehabilitation (micro-level).
2. Materials and Methods
2.1. Study Design, Participants, Setting, and Data Collection
The current study is part of the RehabNytte study, which is a large prospective longitudinal multicenter study with a 12-month follow-up period. In total, more than 3000 participants ≥18 years old with different diagnoses who received rehabilitation at 17 rehabilitation centers from all Norwegian health regions were included between January 2019 and March 2020. Patients were invited to participate during their first encounter with a healthcare professional at the point of admission to rehabilitation and were given oral and written information before providing informed consent. The centers offer inpatient and outpatient rehabilitation, target various diagnoses, and also have different rehabilitation specialties, contents, facilities, and resources. A flowchart outlining the data collection process in the current study is shown in Figure 1. The data were collected through a web-based portal that required authentication in accordance with GDPR data security level four. Collection was performed at admission (baseline) and at discharge and at 3, 6, and 12 months after admission to rehabilitation.
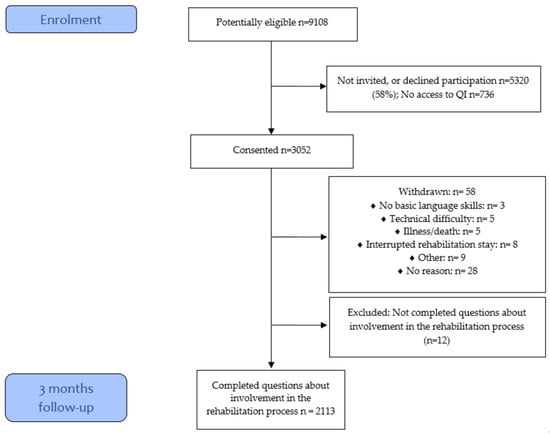
Figure 1.
Participant flowchart.
2.2. Variables
The demographic variables included sex, age, living with a partner (yes/no), duration of pain ≥3 months (yes/no), and work status (full-time work/part-time work/not in paid work). Education was registered as education ≥12 years (yes/no). The variable diagnosis was collapsed from twenty-six categories into four main categories comprising the three most common diagnoses as follows: rheumatic and musculoskeletal diseases (RMDs), lifestyle-related diseases (primarily overweight), neurological diseases, and “other”. The “other” category included smaller diagnostic groups, such as those with sensory disabilities and multiple types of trauma. Age was categorized into 17–39 years, 40–49 years, 50–59 years, 60–69 years, and 70–>80 years.
To measure PE, we used a quality indicator (QI) set developed for the rehabilitation of people with RMDs [18] and tested for responsiveness with good results [19]. The QI set comprises 19 items related to structure, 11 related to process, and 3 related to outcomes of the rehabilitation process. The QIs reflect the quality of care at a meso-level [20] where structural indicators are reported by leaders at the rehabilitation centers (meso-level), whereas process indicators are reported by patients responding with a yes or no to each item, thereby reflecting patients’ experiences of the implementation of structures for the PE process at the meso-level. In the present study, the following five QIs were included: “Were you actively involved in setting specific goals for the rehabilitation?”, “Were you actively involved in preparing a specific written plan for the rehabilitation period?”, “Did you participate in at least two meetings with the team (or a health professional representing the team) during which your goal(s) and goal attainment thus far were discussed?”, “Were you asked if you wanted attendance in any of the meetings for your next of kin?”, and “Were you asked if you wanted attendance in any of the meetings for professionals you would be related to after the rehabilitation period?” (e.g., external healthcare personnel, a general practitioner, a social worker or someone from the workplace to participate in their rehabilitation meetings). We calculated the pass rates for each indicator as the total number of patients who answered “yes” for this particular indicator divided by the total number of responses for the same indicator. The pass rate scores were thereafter normalized to 100 to report the values as a percentage (0–100%, with 100% being the best score). The first process QI was additionally used as a measure of involvement in goalsetting, whereas the outcome QI of “as a result of the rehab period, have you achieved one or several goals that are important to you”, was used as a measure of individual goal attainment (micro-level) [18].
Functioning was measured with the Patient Specific Functioning Scale (PSFS), which was randomly allocated to half of the participants as part of the larger RehabNytte study. In the PSFS, patients list up to five important activities that they currently find difficult to perform due to their health condition. The experienced performance of each activity is scored on an 11-point scale (0–10), with 0 indicating “unable to perform” and 10 indicating “no problem at all”. The mean activity scores were thereafter calculated [21].
2.3. Statistics
Descriptive statistics are presented as the frequency and percentage or mean/median, as applicable. Groups were compared using t- tests or chi-squared tests. Paired sample t-tests were used to explore changes in function from baseline to 3, 6, and 12 months after rehabilitation admission. Logistic regression analyses were used to examine associations between the dependent variable of “active involvement in goal-setting” and patient characteristics (independent variables) as well as associations between the dependent outcome variable of “goal attainment” and patient characteristics and patient involvement in the rehabilitation process (independent variables). The results are presented as the means with standard deviations or as odds ratios with 95% confidence intervals. Both regression analyses and paired sample t-tests were two-sided, and the alpha level was set to p ≤ 0.05. All the statistical analyses were performed using IBM SPSS Statistics version 28, Armonk, NY, USA [22].
2.4. Ethics
The study was carried out following the principles outlined in the Helsinki Declaration and was designed according to the Personal Data Act and the General Data Protection Regulation (GDPR). The study was recommended by the data protection officer at Diakonhjemmet Hospital (DS-00040), dated 17 October 2018, and registered at ClinicalTrials.gov (NCT03764982). It was considered by the regional ethical committee to not require approval since the overarching goal was to evaluate the delivery of rehabilitation services (2018/1645/REK South-East A). The study participants were covered by the Norwegian System of Patient Injury Compensation while they were staying at the rehabilitation institution. The electronic data collection system used was provided by CheckWare and inclusion protocols were stored in lockable cabinets in the local project coordinator offices during the project period. When the data collection was completed, de-identified data were transferred to the research server at Diakonhjemmet Hospital and the code list was stored on a locked, encrypted USB flash drive. All identifiable data files will be anonymized within five years after completion, and the final report will be sent to the data protection office no later than 2027.
2.5. Patient Research Partner Involvement
Two patient research partners were engaged in all phases of the research project, including ensuring the use of inclusive language in the final manuscript and developing plain language summaries in Norwegian and English. They as well as the rehabilitation centers that participated in the study will also provide valuable support in sharing the results and putting the findings into practice. All patient research partners were included as authors following the Vancouver Declaration.
3. Results
A total of 2113 participants reported the QI score for involvement in goal-setting and 2100 reported the QI score for goal attainment. The mean age was 53 years (SD = 13.5) and the majority of participants were women (70%). The vast majority (92%) reported long pain durations (≥3 months) before rehabilitation, approximately half of the participants had ≥12 years of education, and half of the participants were working before rehabilitation admission. The largest diagnostic groups were RMDs (53%), lifestyle diseases (13%), and neurological injuries and diseases (11%) (Table 1).

Table 1.
Baseline characteristics of all participants (n = 2113).
3.1. Patient Involvement in the Rehabilitation Process
A total of 95% of participants reported being involved in setting rehabilitation goals, 79% reported being involved in preparing their rehabilitation plan, and 84% reported having participated in at least two rehabilitation meetings. However, 23% were asked if they wanted attendance at any of the meetings for their next of kin and 19% were asked if they wanted attendance of professionals whom they would relate to after the rehabilitation period. Compared with participants in the highest age group (89%), a greater percentage of participants in the younger age group were involved (95–97%) in goal-setting (Table 2).

Table 2.
Patient characteristics and involvement in the rehabilitation process (total n = 2113) are reported as proportions.
3.2. Associations between Patient Characteristics and Involvement in Goal-Setting
Ninety-five percent reported being actively involved in setting rehabilitation goals. There was a greater likelihood of involvement among women than men (odds ratio [OR] 1.87, 95% CI 1.15–3.02) and among participants of younger ages (OR 0.97, 95% CI 0.95–0.99) (Table 3).

Table 3.
Associations between patient characteristics and involvement in goal-setting (yes/no) (n = 1531).
3.3. Associations between Involvement in Goal-Setting and Improvements in Functioning
A total of 779 participants completed the PSFS at baseline of which 778 were included in the analyses of changes after 3 months, 591 after 6 months, and 584 after 12 months. In general, there was a small mean improvement over the one-year follow-up period among participants. However, compared with participants reporting no involvement in goal-setting, those who were actively involved had greater improvement at all time points, with a significant improvement from baseline to 12 months [19] (Figure 2).
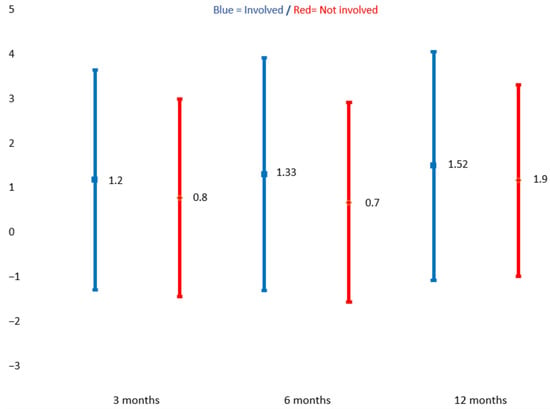
Figure 2.
Mean change for those involved and not involved in goal-setting 3, 6, and 12 months after baseline. Patient-specific functional scale (scored 0–10, with 0 being the worst possible function). □ = involved in goal-setting, ◊ = not involved in goal-setting. Paired sample t–test.
3.4. Associations between Patient Characteristics, Involvement in the Rehabilitation Process, and Goal Attainment
There were positive associations between goal attainment and higher age (OR 1.03, 95% CI 1.02–1.04) and having a lifestyle disease (OR 4.93, 95% CI 2.35–10.35). Compared with having less than 12 years of education, having higher education was negatively associated with goal attainment (OR 0.71, 95% CI 0.53–0.95), whereas having less than three months of continuous pain before rehabilitation admission was positively associated with goal attainment (OR 2.17, 95% CI 1.17–4.00). When examining the associations between involvement in the rehabilitation process and goal attainment, being involved in formulating goals (OR 2.79, 95% CI 1.60–4.87) and preparing the rehabilitation plan (OR 2.04, 95% CI 1.44–2.87) were positively associated with goal attainment (Table 4).

Table 4.
Associations between patient characteristics, involvement in the rehabilitation process, and goal attainment (n = 1501).
4. Discussion
The main goals of this study were to explore the associations between patient involvement in the rehabilitation process and improvements in function and goal attainment in the first year after rehabilitation. The results showed that most participants were involved in goal-setting, developing a rehabilitation plan, and in multidisciplinary team meetings, which are important elements of the rehabilitation process. In contrast, only about one in five participants were asked if they wanted their next of kin or health professionals outside the rehabilitation institution to attend any meetings; these elements may be important for ensuring the follow-up and implementation of lifestyle changes and self-management strategies initiated during the time spent by the patients in rehabilitation [23,24,25,26,27]. These results align with those found in prior studies [15,18,28], suggesting that while coordination across services is recognized as a crucial aspect of a high-quality rehabilitation process, it appears to be one of the weakest elements within the rehabilitation trajectory.
Engaging the relevant stakeholders as part of the rehabilitation process in secondary care has been shown to facilitate rehabilitation follow-up in primary care [29]. Additionally, improved communication skills, education of health professionals, and patient education are the most important PE facilitators [30,31]. In line with this, the results from a previous mixed methods study indicated that an emphasis on the post-discharge rehabilitation process significantly relied not only on the behaviors and the communication skills of individual providers but also on the support from team leaders as well as the local institutional context [28]. Consequently, forthcoming initiatives aimed at enhancing patient involvement in the rehabilitation process should concentrate on the meso-level. This involves implementing training programs for health professionals in patient–professional cooperation, refining referral routines, enhancing information flow among providers and affiliated services, and ensuring adequate competence and human resources at every level of care.
Our results demonstrated that the vast majority of the patients included were actively involved in setting goals and preparing their rehabilitation plans. However, the findings also showed a reduced likelihood of men and older individuals actively participating in developing rehabilitation goals. Results from a recent national survey demonstrated that health literacy declines with advancing age [32]. One factor contributing to the lower engagement among older individuals may therefore be lower health literacy, which impacts their capability and desire to actively engage in the rehabilitation process [33]. Other factors may include low resilience, reduced intrinsic capacity, and depressed moods among older persons [34,35]. Consequently, future goal-setting initiatives should recognize the significance of promoting mental well-being in addition to physical function [36]. Another explanation may be ageism, meaning that health professionals may expect less involvement or engage elderly people in setting goals to a lesser extent. Additionally, it was previously common practice that multidisciplinary teams would formulate goals on behalf of patients; therefore, based on experience, older individuals may expect professionals to set achievable goals on their behalf. However, this paternalistic patient–therapist dynamic contradicts current national strategies that underscore the importance of involving patients in their rehabilitation process [37]. Addressing the trend toward diminished engagement among men and older patients necessitates a proactive meso-level approach. This can be achieved, for instance, by implementing methods specifically designed to encourage patients to take a more active approach [38,39].
An important finding in our study is that function, as measured through the PSFS, improved in both groups over the one-year follow-up period. Interestingly, participants who actively engaged in goalsetting exhibited a more substantial enhancement in function, which is in line with findings from a recent study [40]. Additionally, these participants had significantly greater PSFS scores from baseline to the 12-month post-rehabilitation assessment. One reason for this finding may be that rehabilitation goals that individuals have ownership of motivate them to exert a high level of personal effort to achieve these goals both during and after the inpatient rehabilitation period. Another explanation may be the focus on activity and participation-related goals enhanced through the use of the PSFS as such goals have been found to be associated with better outcomes [41].
We also found that involvement in goal-setting almost tripled the odds of goal attainment and that being involved in developing their rehabilitation plan nearly doubled the odds of attaining their own rehabilitation goals. These findings are comparable with the results of a previous study demonstrating a positive association between PE and goal attainment after rehabilitation [42]. Taken together, the results from our study point to the importance of facilitating patient involvement as engaged patients benefit more from rehabilitation than those who do not.
A strength of this study is the large sample recruited from a large number of rehabilitation centers across Norway. The results may therefore be relevant to people with a wide variety of diseases and to rehabilitation in various contexts. However, as participants were recruited from rehabilitation institutions in Norway, the results may not necessarily be generalizable to other countries or healthcare systems.
Another strength is the use of patient-reported outcome measures as these are believed to complement physician-rated outcomes in the sense of coming closer to patients’ preferred levels of involvement [43,44]. It is essential to acknowledge certain limitations that may impact the generalizability and interpretability of the findings. The data included were limited to the population referred to specialized rehabilitation, which may be a different population with different functional problems than patients who receive rehabilitation in hospitals or primary care. Patients in specialized rehabilitation may be prone to having more stable conditions and higher functional levels than those receiving rehabilitation in hospitals or primary care. Second, people with poor oral or written Norwegian language skills were not included. Third, the study results are affected by the outcome measures used. The reliance on patient-reported outcomes in this study may have introduced constraints in capturing a comprehensive understanding of patient function and rehabilitation outcomes. Self-reported data are at risk of recall bias and response bias, such as response shift, and the natural tendency for people to overstate social acts, such as the degree of goal attainment and/or involvement during the rehabilitation process [45,46,47]
The majority of participants actively engaged in their rehabilitation process as well as those who participated in goal-setting and planning experienced more favorable outcomes compared with those who did not. To improve patient involvement in rehabilitation, future initiatives should focus on the meso-level. This involves implementing training programs that enhance the communication skills of healthcare professionals, ensuring effective information flow among providers and affiliated services, and ensuring sufficient competence and human resources at every level of care.
Author Contributions
J.S.S., H.D., I.K. and R.H.M. analyzed and interpreted the patient data and prepared the first version of the manuscript. All the authors took part in planning the project, developing the research questions, and collecting the data. All authors have read and agreed to the published version of the manuscript.
Funding
The authors thank the DAM Foundation (2020/FO293894) and the Research Council of Norway (No. 328657) for their support. The funding bodies were not involved in the design of the study; the collection, analysis, or interpretation of the data; or the writing of the manuscript.
Institutional Review Board Statement
This study was conducted following approved guidelines in accordance with the Declaration of Helsinki and approved by the data protection officer at Diakonhjemmet Hospital (DS-00040). All participants were informed about the purpose of the study and provided written informed consent. The RehabNytte study is registered in Clinical Trials, NCT03764982.
Informed Consent Statement
Informed consent was obtained from all participants involved in the study.
Data Availability Statement
The dataset is available from the corresponding author upon reasonable request.
Acknowledgments
The authors acknowledge all the participants in this study and * the RehabNytte Consortium of collaborating research centers for making this study possible. * the RehabNytte Consortium includes the following collaborating institutions: the Norwegian National Center for Occupational Rehabilitation (NKARR); the Regional Center for Knowledge Translation in Rehabilitation (RKR); Virke Rehab; the Norwegian Federation of Organizations of Disabled People (FFO); the National Advisory Unit on Rehabilitation in Rheumatology (NKRR); the Center for Treatment of Rheumatic and Musculoskeletal Diseases (REMEDY); Avonova Ringerike Rehabilitation Center; Evjeklinikken Rehabilitation Center; Helsepartner Rehabilitation Center; Hernes Institute; HLF Briskeby Rehabilitation Center; Montebello Rehabilitation Center; Muritunet as Rehabilitation Center; NKS Helsehus Rehabilitation Center; Ravneberghaugen Rehabilitation Center; Røde Kors Haugland Rehabilitation Center; Røysumtunet Rehabilitation Center; Selli Rehabilitation Center; Skogli Health and Rehabilitation Center; Sørlandet Rehabilitation Center; Stiftelsen Cato Rehabilitation Center; Vikersund Rehabilitation Center; and Åstveit Rehabilitation Center.
Conflicts of Interest
All the authors declare that they have no competing interests regarding this work.
References
- World Health Organization (WHO). Quality of Care. Available online: https://www.who.int/health-topics/quality-of-care#tab=tab_1 (accessed on 20 September 2023).
- Sheikh, S.A.; Donaldson, L.; Dhingra-Kumar, N.; Bates, D.; Kelley, E.; Larizgoitia, I.; Panesar, S.; Singh, C.; de Silva, D.; Valderas, J.; et al. Patient Engagement: Technical Series on Safer Primary Care; WHO: Geneva, Switzerland, 2016.
- Steele Gray, C.; Grudniewicz, A.; Armas, A.; Mold, J.; Im, J.; Boeckxstaens, P. Goal-Oriented Care: A Catalyst for Person-Centred System Integration. Int. J. Integr. Care 2020, 20, 8. [Google Scholar] [CrossRef] [PubMed]
- Coulter, A.; Oldham, J. Person-centred care: What is it and how do we get there? Future Hosp. J. 2016, 3, 114–116. [Google Scholar] [CrossRef] [PubMed]
- Andreassen, T.A. Service user involvement and repositioning of healthcare professionals: A framework for examining implications of different forms of involvement. Nordisk Välfärdsforskning|Nordic. Welfare Res. 2018, 3, 58–69. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Disability; WHO: Geneva, Switzerland, 2011. Available online: https://www.who.int/publications/i/item/9789241564182. (accessed on 1 September 2023).
- Spijk-de Jonge, M.J.; Weijers, J.M.; Teerenstra, S.; Elwyn, G.; van de Laar, M.A.; van Riel, P.L.; Huis, A.M.; Hulscher, M.E. Patient involvement in rheumatoid arthritis care to improve disease activity-based management in daily practice: A randomized controlled trial. Patient Educ. Couns. 2022, 105, 1244–1253. [Google Scholar] [CrossRef] [PubMed]
- Kang, E.; Kim, M.Y.; Lipsey, K.L.; Foster, E.R. Person-Centered Goal Setting: A Systematic Review of Intervention Components and Level of Active Engagement in Rehabilitation Goal-Setting Interventions. Arch. Phys. Med. Rehabil. 2022, 103, 121–130.e123. [Google Scholar] [CrossRef] [PubMed]
- Rosengren, K.; Brannefors, P.; Carlstrom, E. Adoption of the concept of person-centred care into discourse in Europe: A systematic literature review. J. Health Organ. Manag. 2021, 35, 265–280. [Google Scholar] [CrossRef]
- Flynn, K.E.; Smith, M.A.; Vanness, D. A typology of preferences for participation in healthcare decision making. Soc. Sci. Med. 2006, 63, 1158–1169. [Google Scholar] [CrossRef]
- Sagen, J.S.; Smedslund, G.; Simonsen, A.E.; Habberstad, A.; Kjeken, I.; Dagfinrud, H.; Moe, R.H. Patient engagement in the development and delivery of healthcare services: A systematic scoping review. BMJ Open Qual. 2023, 12, e002309. [Google Scholar] [CrossRef]
- Rose, A.; Rosewilliam, S.; Soundy, A. Shared decision making within goal setting in rehabilitation settings: A systematic review. Patient Educ. Couns. 2017, 100, 65–75. [Google Scholar] [CrossRef]
- Siegert, R.J.; Taylor, W.J. Theoretical aspects of goal-setting and motivation in rehabilitation. Disabil. Rehabil. 2004, 26, 1–8. [Google Scholar] [CrossRef]
- Pasient- og brukerrettighetsloven. Lov om pasient- og brukerrettigheter (LOV-2023-12-20-106). Lovdata. 2001. §3. Available online: https://lovdata.no/lov/1999-07-02-63 (accessed on 28 December 2023).
- Sand-Svartrud, A.L.; Berdal, G.; Azimi, M.; Bø, I.; Dager, T.N.; Eppeland, S.G.; Fredheim, G.O.; Hagland, A.S.; Klokkeide, Å.; Linge, A.D.; et al. Associations between quality of health care and clinical outcomes in patients with rheumatic and musculoskeletal diseases: A rehabilitation cohort study. BMC Musculoskelet Disord. 2022, 23, 357. [Google Scholar] [CrossRef] [PubMed]
- Yun, D.; Choi, J. Person-centered rehabilitation care and outcomes: A systematic literature review. Int. J. Nurs. Stud. 2019, 93, 74–83. [Google Scholar] [CrossRef] [PubMed]
- Smit, E.B.; Bouwstra, H.; Hertogh, C.M.; Wattel, E.M.; van der Wouden, J.C. Goal-setting in geriatric rehabilitation: A systematic review and meta-analysis. Clin. Rehabil. 2019, 33, 395–407. [Google Scholar] [CrossRef] [PubMed]
- Johansen, I.; Klokkerud, M.; Anke, A.; Børke, J.B.; Glott, T.; Hauglie, U.; Høyem, A.; Klovning, A.; Lande, K.A.; Larsen, M.; et al. A quality indicator set for use in rehabilitation team care of people with rheumatic and musculoskeletal diseases; development and pilot testing. BMC Health Serv. Res. 2019, 19, 265. [Google Scholar] [CrossRef] [PubMed]
- Sand-Svartrud, A.L.; Berdal, G.; Azimi, M.; Bø, I.; Dager, T.N.; Eppeland, S.G.; Fredheim, G.O.; Hagland, A.S.; Klokkeide, Å.; Linge, A.D.; et al. A quality indicator set for rehabilitation services for people with rheumatic and musculoskeletal diseases demonstrates adequate responsiveness in a pre-post evaluation. BMC Health Serv. Res. 2021, 21, 164. [Google Scholar] [CrossRef] [PubMed]
- Santana, M.J.; Manalili, K.; Jolley, R.J.; Zelinsky, S.; Quan, H.; Lu, M. How to practice person-centred care: A conceptual framework. Health Expect 2018, 21, 429–440. [Google Scholar] [CrossRef]
- Moseng, T.; Tveter, A.T.; Holm, I.; Dagfinrud, H. Pasient-Spesifikk Funksjonsskala. Et nyttig verktøy for fysioterpaeuter i primaerhelsetjenesten. Nor. J. Physiother. 2013, 2, 20–26. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, version 28; IBM Corp: Armonk, NY, USA, 2021. [Google Scholar]
- Fairley, J.L.; Seneviwickrama, M.; Yeh, S.; Anthony, S.; Chou, L.; Cicuttini, F.M.; Sullivan, K.; Briggs, A.M.; Wluka, A.E. Person-centred care in osteoarthritis and inflammatory arthritis: A scoping review of people’s needs outside of healthcare. BMC Musculoskelet Disord. 2021, 22, 341. [Google Scholar] [CrossRef]
- Chi-Lun-Chiao, A.; Chehata, M.; Broeker, K.; Gates, B.; Ledbetter, L.; Cook, C.; Ahern, M.; Rhon, D.I.; Garcia, A.N. Patients’ perceptions with musculoskeletal disorders regarding their experience with healthcare providers and health services: An overview of reviews. Arch. Physiother. 2020, 10, 17. [Google Scholar] [CrossRef]
- Bergström, M.; Larsson Ranada, Å.; Sverker, A.; Thyberg, I.; Björk, M. A dyadic exploration of support in everyday life of persons with RA and their significant others. Scand J. Occup. Ther. 2023, 30, 616–627. [Google Scholar] [CrossRef]
- Jones, F. Strategies to enhance chronic disease self-management: How can we apply this to stroke? Disabil. Rehabil. 2006, 28, 841–847. [Google Scholar] [CrossRef] [PubMed]
- Valaas, H.L.; Klokkerud, M.; Hildeskår, J.; Hagland, A.S.; Kjønli, E.; Mjøsund, K.; Øie, L.; Wigers, S.H.; Eppeland, S.G.; Høystad, T.; et al. Follow-up care and adherence to self-management activities in rehabilitation for patients with rheumatic and musculoskeletal diseases: Results from a multicentre cohort study. Disabil. Rehabil. 2022, 44, 8001–8010. [Google Scholar] [CrossRef] [PubMed]
- Sand-Svartrud, A.L.; Berdal, G.; Aanerud, G.J.; Azimi, M.; Bjørnerud, A.M.; Nygaard Dager, T.; Van den Ende, C.H.M.; Johansen, I.; Lindtvedt Valaas, H.; Dagfinrud, H.; et al. Delivery of a quality improvement program in team-based rehabilitation for patients with rheumatic and musculoskeletal diseases: A mixed methods study. Disabil. Rehabil. 2023, 1–13. [Google Scholar] [CrossRef]
- Cott, C. Client-centred rehabilitation: Client perspectives. Disabil. Rehabil. 2004, 26, 1411–1422. [Google Scholar] [CrossRef] [PubMed]
- Leach, E.; Cornwell, P.; Fleming, J.; Haines, T. Patient centered goal-setting in a subacute rehabilitation setting. Disabil. Rehabil. 2010, 32, 159–172. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, S.H.; Greenfield, S.; Ware, J.E., Jr. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med. Care 1989, 27, S110–S127. [Google Scholar] [CrossRef] [PubMed]
- Le, C.; Finbråten, H.S.; Pettersen, K.S.; Joranger, P.; Guttersrud, Ø. Befolkningens Helsekompetanse, del I. The International Health Literacy Population Survey 2019–2021 (HLS19)–et Samarbeidsprosjekt Med Nettverket M-POHL tilknyttet WHO-EHII. Rapport IS-2959. 2021. Available online: https://www.researchgate.net/publication/348834876_Befolkningens_helsekompetanse_del_I_The_International_Health_Literacy_Population_Survey_2019-2021_HLS19_-_et_samarbeidsprosjekt_med_nettverket_M-POHL_tilknyttet_WHO-EHII_Rapport_IS-2959 (accessed on 28 December 2023).
- Aimée Hartford Kvæl, L.; Gautun, H. Social inequality in navigating the healthcare maze: Care trajectories from hospital to home via intermediate care for older people in Norway. Soc. Sci. Med. 2023, 333, 116142. [Google Scholar] [CrossRef]
- Chen, Z.-J.; Tang, F.-P.; Chang, S.-Y.; Chung, H.-L.; Tsai, W.-H.; Chou, S.-S.; Yeh, H.-C.; Tung, H.-H. Resilience-happiness nexus in community-dwelling middle-aged and older adults: Results from Gan-Dau Healthy Longevity Plan. Arch. Gerontol. Geriatr. 2024, 116, 105162. [Google Scholar] [CrossRef]
- Lin, Y.H.; Han, D.S.; Lee, Y.H.; Chan, D.C.; Chang, C.H.; Yang, K.C.; Chang, F.C. Social network associated with depressed mood and sarcopenia among older adults in Taiwan. J. Formos. Med. Assoc. 2023. Preprint. [Google Scholar] [CrossRef]
- Preede, L.; Soberg, H.L.; Dalen, H.; Nyquist, A.; Jahnsen, R.; Saebu, M.; Bautz-Holter, E.; Røe, C. Rehabilitation Goals and Effects of Goal Achievement on Outcome Following an Adapted Physical Activity-Based Rehabilitation Intervention. Patient Prefer. Adherence 2021, 15, 1545–1555. [Google Scholar] [CrossRef]
- Feiring, M. Rehabilitation—Between management and knowledge practices: An historical overview of public action in Norwegian welfare reforms. Policy Soc. 2012, 31, 119–129. [Google Scholar] [CrossRef]
- Institute of Medicine Committee on Quality of Health Care in America. Crossing the Quality Chasm: A New Health System for the 21st Century; National Academies Press (US): Washington, DC, USA, 2001. [Google Scholar]
- Kvæl, L.A.H.; Debesay, J.; Bye, A.; Langaas, A.; Bergland, A. Choice, Voice, and Coproduction in Intermediate Care: Exploring Geriatric Patients’ and Their Relatives’ Perspectives on Patient Participation. SAGE Open 2019, 9, 2158244019876318. [Google Scholar] [CrossRef]
- Valaas, H.L.; Klokkerud, M.; Hildeskår, J.; Hagland, A.S.; Kjønli, E.; Mjøsund, K.; Øie, L.; Wigers, S.H.; Eppeland, S.G.; Høystad, T.; et al. Rehabilitation goals described by patients with rheumatic and musculoskeletal diseases: Content and attainment during the first year after rehabilitation. Disabil. Rehabil. 2022, 44, 7947–7957. [Google Scholar] [CrossRef]
- Amundsen, O.; Vøllestad, N.K.; Meisingset, I.; Robinson, H.S. Associations between treatment goals, patient characteristics, and outcome measures for patients with musculoskeletal disorders in physiotherapy practice. BMC Musculoskelet Disord. 2021, 22, 182. [Google Scholar] [CrossRef] [PubMed]
- Ashford, S.; Turner-Stokes, L.; Rose, H.; Singer, B. Patient engagement and satisfaction with goal planning: Impact on outcome from rehabilitation. Int. J. Ther. Rehabil. 2015, 22, 210–216. [Google Scholar] [CrossRef]
- Grine, L.; Janssens, R.; van Overbeeke, E.; Derijcke, D.; Silva, M.; Delys, B.; Dusart, I.; Aertsen, V.; Mertens de Wilmars, M.; Robaczewska, J.; et al. Improving Patient Involvement in the Lifecycle of Medicines: Insights From the EUPATI BE Survey. Front. Med. 2020, 7, 36. [Google Scholar] [CrossRef] [PubMed]
- de Wit, M.P.T.; Berlo, S.E.; Aanerud, G.J.; Aletaha, D.; Bijlsma, J.W.; Croucher, L.; Da Silva, J.A.P.; Glusing, B.; Gossec, L.; Hewlett, S.; et al. European League Against Rheumatism recommendations for the inclusion of patient representatives in scientific projects. Ann. Rheum. Dis. 2011, 70, 722–726. [Google Scholar] [CrossRef]
- Rosenman, R.; Tennekoon, V.; Hill, L.G. Measuring bias in self-reported data. Int. J. Behav. Healthc. Res. 2011, 2, 320–332. [Google Scholar] [CrossRef]
- Howard, G.S. Response-Shift Bias: A Problem in Evaluating Interventions with Pre/Post Self-Reports. Eval. Rev. 1980, 4, 93–106. [Google Scholar] [CrossRef]
- Zini, M.L.L.; Banfi, G. A Narrative Literature Review of Bias in Collecting Patient Reported Outcomes Measures (PROMs). Int. J. Environ. Res. Public Health 2021, 18, 12445. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).