Evaluation of an OSA Risk Screening Smartphone App in a General, Non-Symptomatic Population Sample (ESOSA)
Abstract
1. Introduction
2. Materials and Methods
2.1. Target Population, Recruitment and Pre-Screening
2.2. Observational Procedure
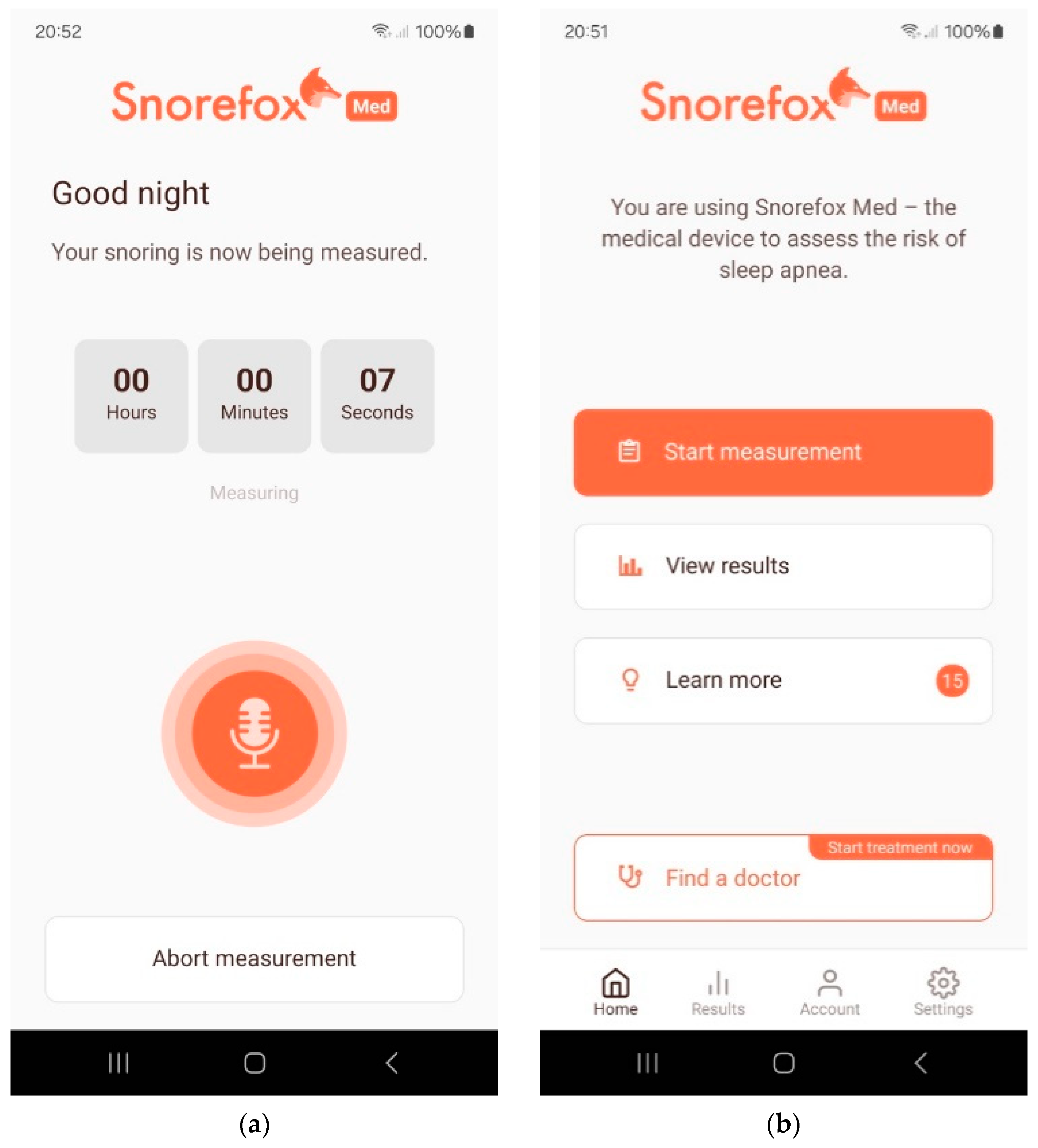
2.3. OSA Screening Smartphone App
2.4. Reference Measurement
2.5. Evaluation and Follow-Up
2.6. Study Endpoints
- (a)
- number of participants without a study result due to not completing the study, user mistakes, or measurement failures of the PSG measuring device or the Snorefox M measurement were evaluated as a secondary endpoint.
- (b)
- performance of the Snorefox M software application to detect an AHI ≥ 15 on the entirety of all subjects for whom a full night PSG result is provided, including those in which the Snorefox M device did not provide a result, including the latter cases in the denominator for the calculation of the sensitivity and specificity with corresponding confidence intervals.
- (c)
- subgroup analysis for significant differences in the performance endpoints for sex, age, body mass index (BMI), and ethnicity.
2.7. Statistics
3. Results
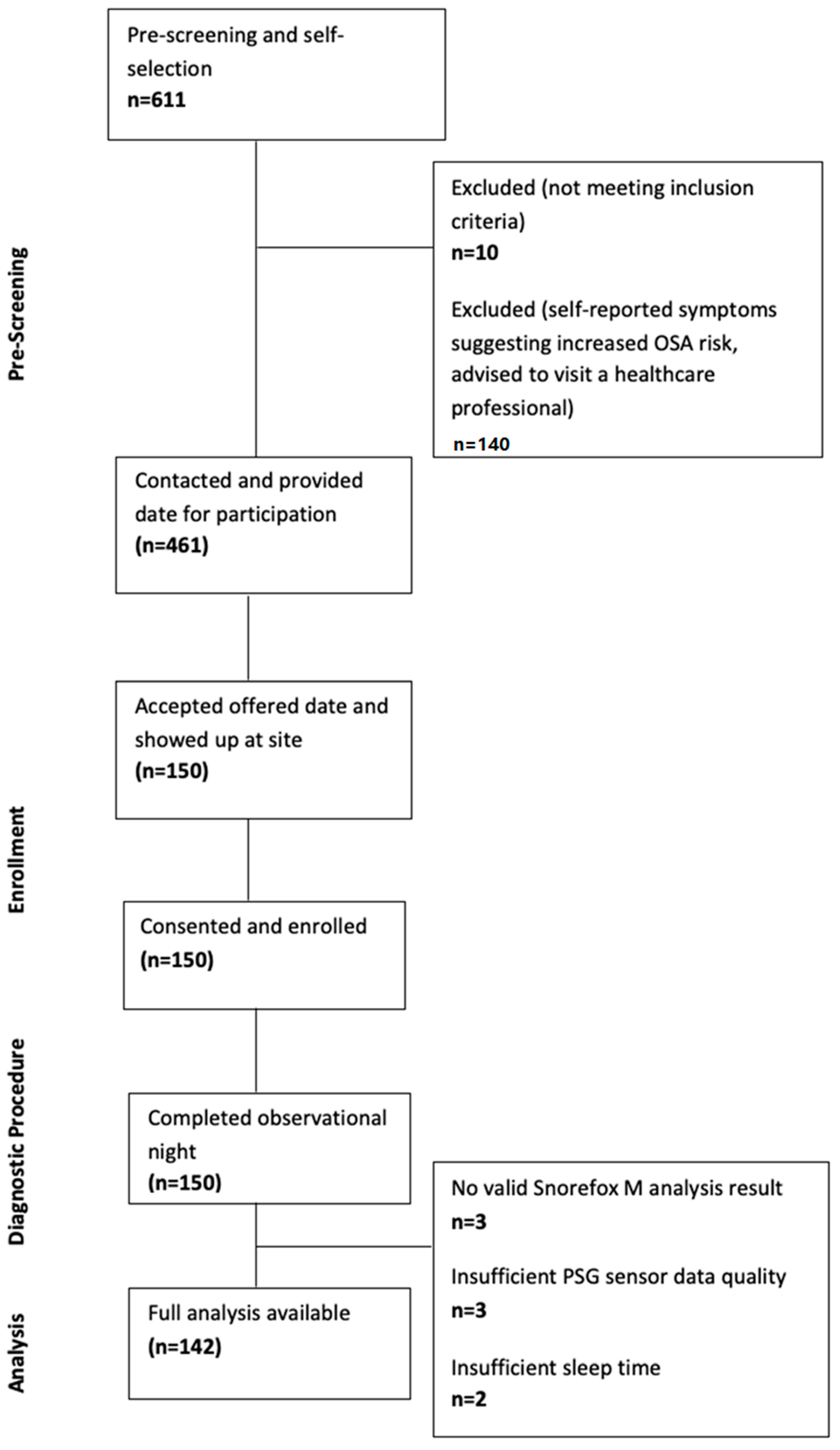
3.1. Pre-Screening
3.2. Observational Night
3.3. Performance of the Snorefox M Compared to the Reference PSG
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grote, L. The global burden of sleep apnoea. Lancet Respir. Med. 2019, 7, 645–647. [Google Scholar] [CrossRef] [PubMed]
- Fietze, I.; Laharnar, N.; Obst, A.; Ewert, R.; Felix, S.B.; Garcia, C.; Gläser, S.; Glos, M.; Schmidt, C.O.; Stubbe, B.; et al. Prevalence and association analysis of obstructive sleep apnea with gender and age differences—Results of SHIP-Trend. J. Sleep Res. 2019, 28, e12770. [Google Scholar] [CrossRef] [PubMed]
- Gonzaga, C.; Bertolami, A.; Bertolami, M.; Amodeo, C.; Calhoun, D. Obstructive sleep apnea, hypertension and cardiovascular diseases. J. Hum. Hypertens. 2015, 29, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Phillips, C.L.; O’Driscoll, D.M. Hypertension and obstructive sleep apnea. Nat. Sci. Sleep 2013, 5, 43–52. [Google Scholar] [CrossRef]
- Muxfeldt, E.S.; Margallo, V.; Costa, L.M.S.; Guimarães, G.; Cavalcante, A.H.; Azevedo, J.C.M.; Souza, F.; Cardoso, C.R.L.; Salles, G.F. Effects of continuous positive airway pressure treatment on clinic and ambulatory blood pressures in patients with obstructive sleep apnea and resistant hypertension: A randomized controlled trial. Hypertension 2015, 65, 736–742. [Google Scholar] [CrossRef] [PubMed]
- Thunström, E.; Manhem, K.; Rosengren, A.; Peker, Y. Blood Pressure Response to Losartan and Continuous Positive Airway Pressure in Hypertension and Obstructive Sleep Apnea. Am. J. Respir. Crit. Care Med. 2016, 193, 310–320. [Google Scholar] [CrossRef]
- Haentjens, P.; Van Meerhaeghe, A.; Moscariello, A.; De Weerdt, S.; Poppe, K.; Dupont, A.; Velkeniers, B. The impact of continuous positive airway pressure on blood pressure in patients with obstructive sleep apnea syndrome: Evidence from a meta-analysis of placebo-controlled randomized trials. Arch. Intern. Med. 2007, 167, 757–764. [Google Scholar] [CrossRef] [PubMed]
- Benjafield, A.V.; Ayas, N.T.; Eastwood, P.R.; Heinzer, R.; Ip, M.S.M.; Morrell, M.J.; Nunez, C.M.; Patel, S.R.; Penzel, T.; Pépin, J.-L.; et al. Estimation of the global prevalence and burden of obstructive sleep apnea: A literature-based analysis. Lancet Respir. Med. 2019, 7, 687–698. [Google Scholar] [CrossRef]
- Becerra, M.B.; Becerra, B.J.; Teodorescu, M. Healthcare burden of obstructive sleep apnea and obesity among asthma hospitalizations: Results from the U.S.-based Nationwide Inpatient Sample. Respir. Med. 2016, 117, 230–236. [Google Scholar] [CrossRef]
- Frost und Sullivan. Hidden Health Crisis Costing America Billions; Frost und Sullivan: San Antonio, TX, USA, 2016. [Google Scholar]
- Knauert, M.; Naik, S.; Gillespie, M.B.; Kryger, M. Clinical consequences and economic costs of untreated obstructive sleep apnea syndrome. World J. Otorhinolaryngol.-Head Neck Surg. 2015, 1, 17–27. [Google Scholar] [CrossRef]
- Ronksley, P.E.; Hemmelgarn, B.R.; Tsai, W.H. Comorbidity and healthcare costs in patients with obstructive sleep apnea. Breathe 2011, 8, 95–104. [Google Scholar] [CrossRef][Green Version]
- Wickwire, E.M. Value-based sleep and breathing: Health economic aspects of obstructive sleep apnea. Fac. Rev. 2021, 10, 40. [Google Scholar] [CrossRef]
- Howard, M.E.; Desai, A.V.; Grunstein, R.R.; Hukins, C.; Armstrong, J.G.; Joffe, D.; Swann, P.; Campbell, D.A.; Pierce, R.J. Sleepiness, sleep-disordered breathing, and accident risk factors in commercial vehicle drivers. Am. J. Respir. Crit. Care Med. 2004, 170, 1014–1021. [Google Scholar] [CrossRef] [PubMed]
- Tregear, S.; Reston, J.; Schoelles, K.; Phillips, B. Continuous positive airway pressure reduces risk of motor vehicle crash among drivers with obstructive sleep apnea: Systematic review and meta-analysis. Sleep 2010, 33, 1373–1380. [Google Scholar] [CrossRef] [PubMed]
- Martínez-García, M.A.; Catalán Serra, P. Is sleep apnoea a specialist condition? The role of general practitioners. Breathe 2010, 7, 144–156. [Google Scholar] [CrossRef]
- Sia, C.-H.; Hong, Y.; Tan, L.W.L.; Dam, R.M.; Lee, C.-H.; Tan, A. Awareness and knowledge of obstructive sleep apnea among the general population. Sleep Med. 2017, 36, 10–17. [Google Scholar] [CrossRef] [PubMed]
- Heinzer, R.; Vat, S.; Marques-Vidal, P.; Marti-Soler, H.; Andries, D.; Tobback, N.; Mooser, V.; Preisig, M.; Malhotra, A.; Waeber, G.; et al. Prevalence of sleep-disordered breathing in the general population: The HypnoLaus study. Lancet Respir. Med. 2015, 3, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Flemons, W.W.; Douglas, N.J.; Kuna, S.T.; Rodenstein, D.O.; Wheatley, J. Access to diagnosis and treatment of patients with suspected sleep apnea. Am. J. Respir. Crit. Care Med. 2004, 169, 668–672. [Google Scholar] [CrossRef] [PubMed]
- Baptista, P.M.; Martin, F.; Ross, H.; Reina, C.; Plaza, G.; Casale, M. A systematic review of smartphone applications and devices for obstructive sleep apnea. Braz. J. Otorhinolaryngol. 2022, 88 (Suppl. S5), S188–S197. [Google Scholar] [CrossRef]
- Kapur, V.K.; Auckley, D.H.; Chowdhuri, S.; Kuhlmann, D.C.; Mehra, R.; Ramar, K.; Harrod, C.G. Clinical Practice Guideline for Diagnostic Testing for Adult Obstructive Sleep Apnea: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2017, 13, 479–504. [Google Scholar] [CrossRef]
- Berry, R.B.; Gamaldo, C.E.; Harding, S.M.; Lloyd, R.M.; Marcus, C.L.; Vaughn, B.V. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications, Version 3 Hrsg.; American Academy of Sleep Medicine: Darien, IL, USA, 2023. [Google Scholar]
- Epstein, L.J.; Kristo, D.; Strollo, P.J.J.; Friedman, N.; Malhotra, A.; Patil, S.P.; Ramar, K.; Rogers, R.; Schwab, R.J.; Weaver, E.M.; et al. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J. Clin. Sleep Med. 2009, 5, 263–276. [Google Scholar] [PubMed]
- Garvey, J.F.; Pengo, M.F.; Drakatos, P.; Kent, B.D. Epidemiological aspects of obstructive sleep apnea. J. Thorac. Dis. 2015, 7, 920–929. [Google Scholar] [PubMed]
- Shiao, Y.H.; Yu, C.C.; Yeh, Y.C. Validation of Downloadable Mobile Snore Applications by Polysomnography (PSG). Nat. Sci. Sleep 2024, 16, 489–501. [Google Scholar] [CrossRef] [PubMed]
- Klaus, K.; Stummer, A.L.; Ruf, S. Accuracy of a Smartphone Application Measuring Snoring in Adults—How Smart Is It Actually? Int. J. Environ. Res. Public Health 2021, 18, 7326. [Google Scholar] [CrossRef]
- Roeder, M.; Bradicich, M.; Schwarz, E.I.; Thiel, S.; Gaisl, T.; Held, U.; Kohler, M. Night-to-night variability of respiratory events in obstructive sleep apnea: A systematic review and meta-analysis. Thorax 2020, 75, 1095–1102. [Google Scholar] [CrossRef]
| Section 1 Pre-Screening Questions to Assess Inclusion Criteria | |
|---|---|
| Participants answering “no” to one or more of the questions in Section 1 were excluded from the further recruitment process. |
|
| |
| |
| Section 2 Pre-Screening Questions to Self-Assess OSA-Related Symptoms | |
| Pre-screening questions to self-assess OSA-related symptoms |
|
| |
In the following situations, how likely are you doze off or fall asleep, in contrast to just feeling tired? Use the following scale to choose the most appropriate number for each situation:
|
|
| Physiological Channel |
|---|
| 6 × EEG (F3/M2, F4/M1, C3/M2, C4/M1, O1/M2, O2/M1) EOG (left/right) EMG Chin (3×) ECG Leg movements (left/right) Respiration (flow, thermistor) Effort (thorax, abdomen) Oxygen saturation SpO2 Heart rate Pulse wave Snoring (contact microphone) Body position |
| Diagnosis According to Current Standard (Type II PSG) | |||
|---|---|---|---|
| Snorefox M analysis | Positive (OSA) | Positive (OSA) | Negative (no OSA) |
| A | B | ||
| Negative (no OSA) | C | D | |
| Effectiveness Measures | Definition | ||
| Sensitivity | |||
| Specificity | |||
| Positive Predictive Value (PPV) | |||
| Negative Predictive Value (NPV) | |||
| False Negative Rate | 1-sensitivity | ||
| False Positive Rate | 1-specificity | ||
| Mean | Range | |
|---|---|---|
| Age (years) | 46.5 | 22–75 |
| Height (cm) | 172.7 | 149–195 |
| Weight (kg) | 83.2 | 45–150 |
| BMI (kg/m2) | 27.9 | 18.4–53.1 |
| sex | number of subjects | percent (%) |
| female | 83 | 55 |
| male | 67 | 45 |
| of those female | number of subjects | percent (%) |
| pre-menopausal | 48 | 58 |
| post-menopausal | 27 | 32 |
| would not say | 8 | 10 |
| ethnicity | number of subjects | percent (%) |
| Hispanic | 0 | 0.0 |
| American Indian | 0 | 0.0 |
| Asian | 3 | 2.0 |
| Black | 1 | 0.7 |
| Native Hawaiian | 0 | 0.0 |
| White | 146 | 97.3 |
| Question | Yes | No | % Yes |
|---|---|---|---|
| witnessed apnea | 46 | 104 | 31 |
| snoring | 129 | 21 | 86 |
| hypertension | 25 | 125 | 17 |
| ESS score | mean 4.3 | range 0–10 |
| Number of Subjects | |
|---|---|
| Subjects enrolled | 150 |
| Subjects that did not complete the study | 0 |
| Snorefox M did not provide a result | 3 |
| PSG invalid result (no SpO2 data) | 3 |
| Insufficient sleep time according to EEG | 2 |
| All Subjects with a Completed Snorefox M Analysis and a PSG Result (n = 142) | (95% CI) |
|---|---|
| True prevalence | 0.24 (0.17, 0.32) |
| Sensitivity 1 | 0.91 (0.76, 0.98) |
| Specificity 1 | 0.83 (0.75, 0.90) |
| Positive predictive value | 0.63 (0.48, 0.77) |
| Negative predictive value | 0.97 (0.91, 0.99) |
| Subgroup: Sex | Male | Female | |
|---|---|---|---|
| Total subjects (n) | 64/142 (45%) | 78/142(55%) | p = 0.003 |
| True prevalence | 0.36 (0.24, 0.49) | 0.14 (0.07, 0.24) | |
| Sensitivity | 0.91 (0.72, 0.99) | 0.91 (0.59, 1.00) | |
| Specificity | 0.80 (0.65, 0.91) | 0.85 (0.74, 0.93) | |
| PPV | 0.72 (0.53, 0.87) | 0.50 (0.27, 0.73) | |
| NPV | 0.94 (0.81, 0.99) | 0.98 (0.91, 1.00) | |
| Subgroup: age (split at median) | lower half | upper half | |
| Mean (range) | 34.9 (22–48) | 57.6 (49–75) | p < 0.001 |
| Total subjects | 71/142 | 71/142 | |
| True prevalence | 0.08 (0.03, 0.17) | 0.39 (0.28, 0.52) | |
| Sensitivity | 1.00 (0.54, 1.00) | 0.89 (0.72, 0.98) | |
| Specificity | 0.88 (0.77, 0.95) | 0.77 (0.61, 0.88) | |
| PPV | 0.43 (0.18, 0.71) | 0.71 (0.54, 0.85) | |
| NPV | 1.00 (0.94, 1.00) | 0.92 (0.78, 0.98) | |
| Subgroup: BMI (split at median) | lower half | upper half | |
| Mean (range) | 23.3 (18.4–26.3) | 32.1 (26.4–53.1) | p < 0.001 |
| Total subjects (n) | 71/142 | 71/142 | |
| True prevalence | 0.10 (0.04, 0.19) | 0.38 (0.27, 0.50) | |
| Sensitivity | 0.86 (0.42, 1.00) | 0.93 (0.76, 0.99) | |
| Specificity | 0.84 (0.73, 0.92) | 0.82 (0.67, 0.92) | |
| PPV | 0.38 (0.15, 0.65) | 0.76 (0.58, 0.89) | |
| NPV | 0.98 (0.90, 1.00) | 0.95 (0.82, 0.99) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sommer, J.U.; Lindner, L.; Kent, D.T.; Heiser, C. Evaluation of an OSA Risk Screening Smartphone App in a General, Non-Symptomatic Population Sample (ESOSA). J. Clin. Med. 2024, 13, 4664. https://doi.org/10.3390/jcm13164664
Sommer JU, Lindner L, Kent DT, Heiser C. Evaluation of an OSA Risk Screening Smartphone App in a General, Non-Symptomatic Population Sample (ESOSA). Journal of Clinical Medicine. 2024; 13(16):4664. https://doi.org/10.3390/jcm13164664
Chicago/Turabian StyleSommer, J. Ulrich, Lisa Lindner, David T. Kent, and Clemens Heiser. 2024. "Evaluation of an OSA Risk Screening Smartphone App in a General, Non-Symptomatic Population Sample (ESOSA)" Journal of Clinical Medicine 13, no. 16: 4664. https://doi.org/10.3390/jcm13164664
APA StyleSommer, J. U., Lindner, L., Kent, D. T., & Heiser, C. (2024). Evaluation of an OSA Risk Screening Smartphone App in a General, Non-Symptomatic Population Sample (ESOSA). Journal of Clinical Medicine, 13(16), 4664. https://doi.org/10.3390/jcm13164664






