Aspirin in Primary Prevention: Looking for Those Who Enjoy It
Abstract
1. Introduction
2. Pharmacology of Aspirin: Joys and Sorrows
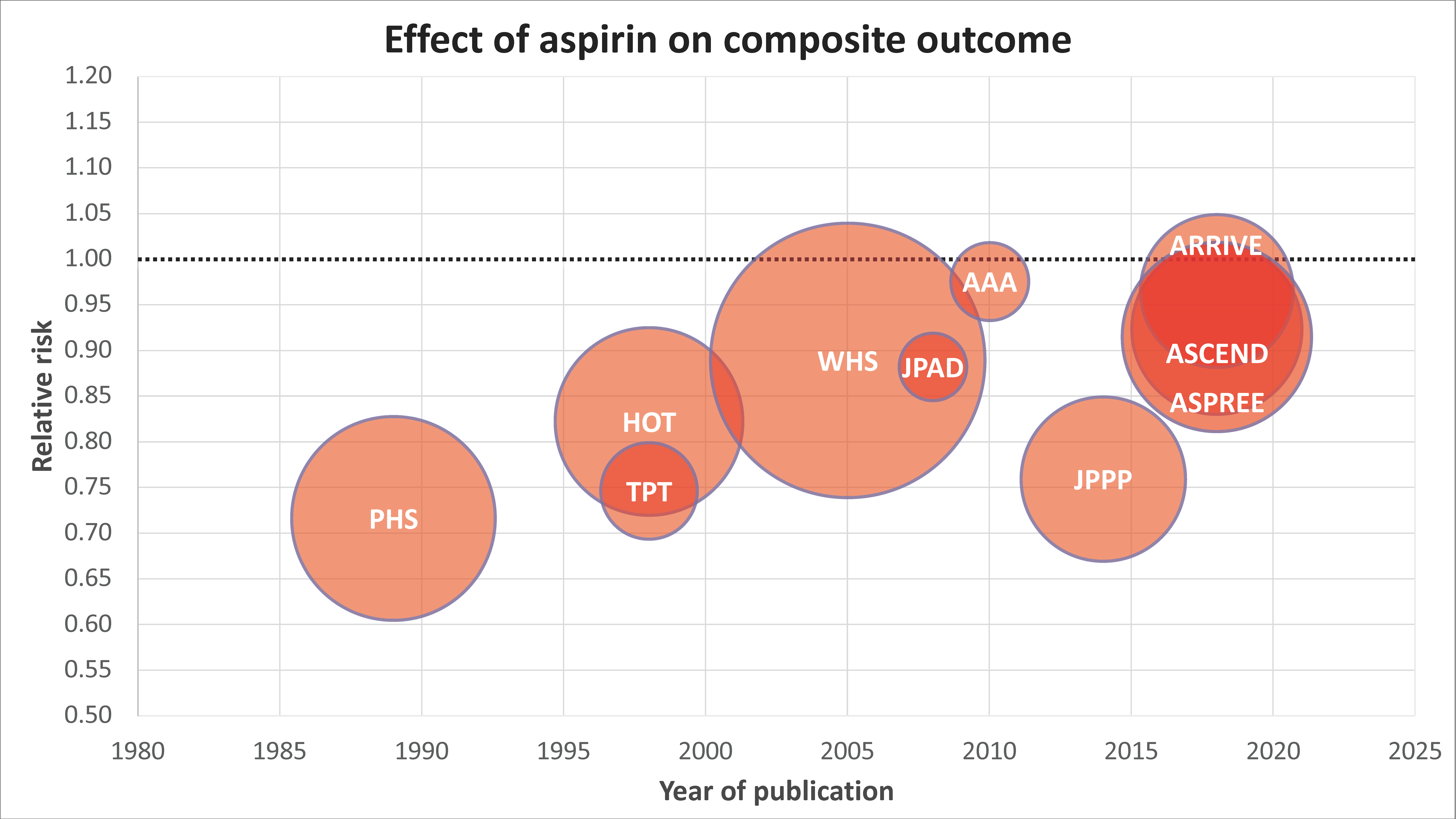
3. Deep Diving in Data: How Effective and Safe Is Aspirin?
4. Looking for a Scapegoat: Can Subgroup Effects Account for the Lack of Benefit?
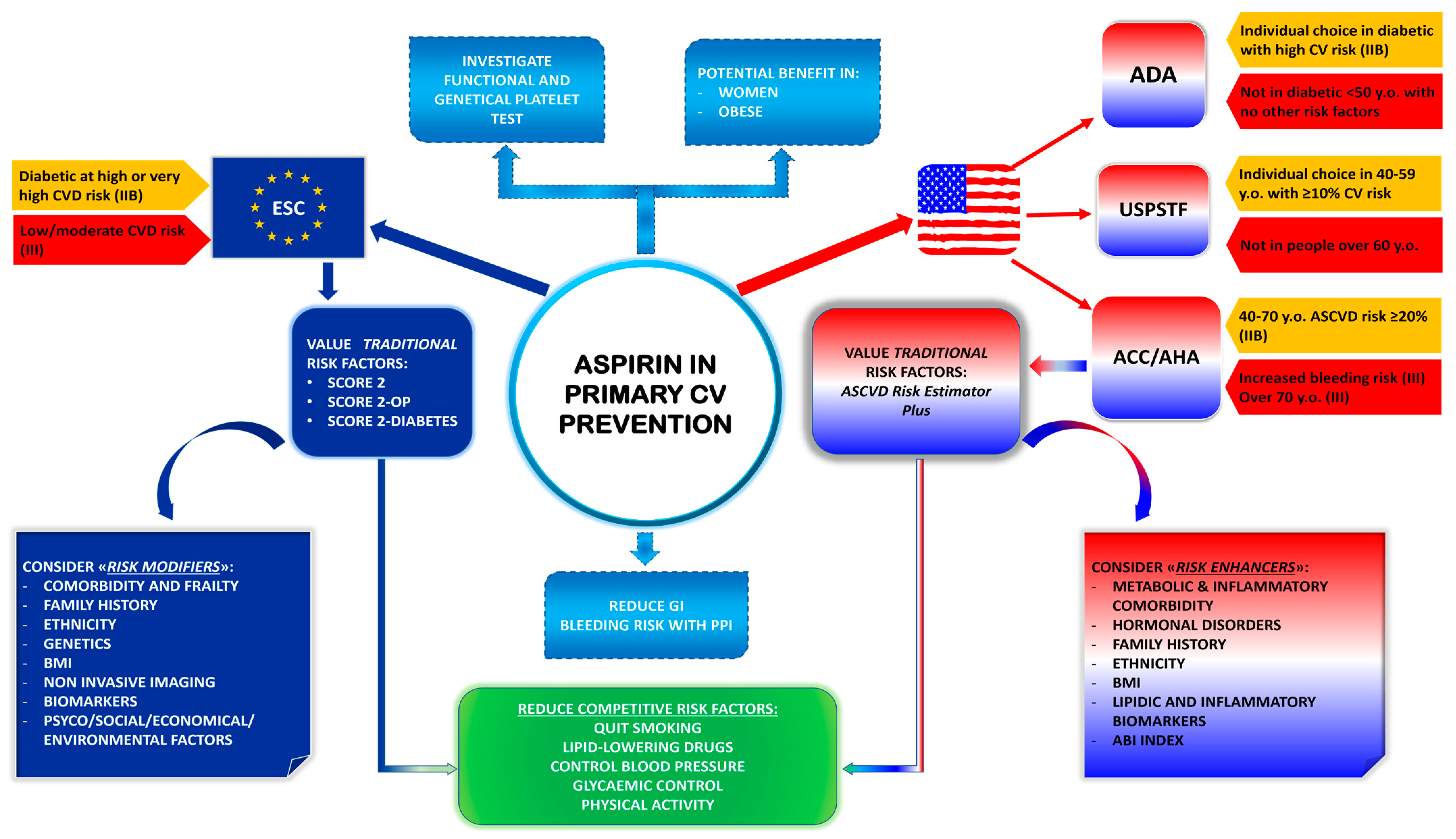
4.1. Diabetics
4.2. Obese
4.3. Women
5. Aspirin in Primary Prevention and Cancer
6. Guideline Recommendations
7. Considerations for a Modern Approach to Cardiovascular Primary Prevention
7.1. Defining the Threshold of Intervention
7.2. Competing Benefit of Alternative Therapies
7.3. Potential “Facilitators” of Aspirin-Based Primary Prevention
8. Conclusions
Funding
Conflicts of Interest
References
- Edney, P.; Jackson, P.; Burrell, B.; Lawton, N.; Leigh, N.; Lindsay McLellan, P.; Newman, C.; Pickard, J.; Weiser, R.; Williams, S.; et al. Secondary Prevention of Vascular Disease by Prolonged Antiplatelet Treatment. Br. Med. J. (Clin. Res. Ed.) 1988, 296, 320. [Google Scholar] [CrossRef]
- Benenati, S.; Galli, M.; De Marzo, V.; Pescetelli, F.; Toma, M.; Andreotti, F.; Della Bona, R.; Canepa, M.; Ameri, P.; Crea, F.; et al. Very Short vs. Long Dual Antiplatelet Therapy after Second Generation Drug-Eluting Stents in 35 785 Patients Undergoing Percutaneous Coronary Interventions: A Meta-Analysis of Randomized Controlled Trials. Eur. Heart J. Cardiovasc. Pharmacother. 2021, 7, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Benenati, S.; Crimi, G.; Canale, C.; Pescetelli, F.; De Marzo, V.; Vergallo, R.; Galli, M.; Della Bona, R.; Canepa, M.; Ameri, P.; et al. Duration of Dual Antiplatelet Therapy and Subsequent Monotherapy Type in Patients Undergoing Drug-Eluting Stent Implantation: A Network Meta-Analysis. Eur. Heart J. Cardiovasc. Pharmacother. 2022, 8, 56–64. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, C.W.; Juraschek, S.P.; Wee, C.C. Prevalence of Aspirin Use for Primary Prevention of Cardiovascular Disease in the United States: Results from the 2017 National Health Interview Survey. Ann. Intern. Med. 2019, 171, 596. [Google Scholar] [CrossRef] [PubMed]
- Capodanno, D.; Angiolillo, D.J. Aspirin for Primary Cardiovascular Risk Prevention and Beyond in Diabetes Mellitus. Circulation 2016, 134, 1579–1594. [Google Scholar] [CrossRef] [PubMed]
- Patrono, C.; García Rodríguez, L.A.; Landolfi, R.; Baigent, C. Low-Dose Aspirin for the Prevention of Atherothrombosis. N. Engl. J. Med. 2005, 353, 2373–2383. [Google Scholar] [CrossRef] [PubMed]
- FitzGerald, G.A. Mechanisms of Platelet Activation: Thromboxane A2 as an Amplifying Signal for Other Agonists. Am. J. Cardiol. 1991, 68, B11–B15. [Google Scholar] [CrossRef] [PubMed]
- Moncada, S.; Vane, J.R. Arachidonic Acid Metabolites and the Interactions between Platelets and Blood-Vessel Walls. N. Engl. J. Med. 1979, 300, 1142–1147. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, T.; Tahara, Y.; Matsumoto, M.; Iguchi, M.; Sano, H.; Murayama, T.; Arai, H.; Oida, H.; Yurugi-Kobayashi, T.; Yamashita, J.K.; et al. Roles of Thromboxane A(2) and Prostacyclin in the Development of Atherosclerosis in ApoE-Deficient Mice. J. Clin. Investig. 2004, 114, 784–794. [Google Scholar] [CrossRef]
- Patrignani, P.; Filabozzi, P.; Patrono, C. Selective Cumulative Inhibition of Platelet Thromboxane Production by Low-Dose Aspirin in Healthy Subjects. J. Clin. Investig. 1982, 69, 1366–1372. [Google Scholar] [CrossRef]
- Mcadam, B.F.; Catella-Lawson, F.; Mardini, I.A.; Kapoor, S.; Lawson, J.A.; Fitzgerald, G.A. Systemic Biosynthesis of Prostacyclin by Cyclooxygenase (COX)-2: The Human Pharmacology of a Selective Inhibitor of COX-2. Proc. Natl. Acad. Sci. USA 1999, 96, 272–277. [Google Scholar] [CrossRef] [PubMed]
- FitzGerald, G.A.; Oates, J.A.; Hawiger, J.; Maas, R.L.; Roberts, L.J.; Lawson, J.A.; Brash, A.R. Endogenous Biosynthesis of Prostacyclin and Thromboxane and Platelet Function during Chronic Administration of Aspirin in Man. J. Clin. Investig. 1983, 71, 676–688. [Google Scholar] [CrossRef] [PubMed]
- Patrono, C.; Ciabarroni, G.; Patrignani, P.; Pugliese, F.; Filabozzi, P.; Catella, F.; Davi, G.; Forni, L. Clinical Pharmacology of Platelet Cyclooxygenase Inhibition. Circulation 1985, 72, 1177–1184. [Google Scholar] [CrossRef] [PubMed]
- Hansson, L.; Zanchetti, A.; Carruthers, S.G.; Dahlöf, B.; Elmfeldt, D.; Julius, S.; Ménard, J.; Rahn, K.H.; Wedel, H.; Westerling, S. Effects of Intensive Blood-Pressure Lowering and Low-Dose Aspirin in Patients with Hypertension: Principal Results of the Hypertension Optimal Treatment (HOT) Randomised Trial. Lancet 1998, 351, 1755–1762. [Google Scholar] [CrossRef] [PubMed]
- Snowden, S.; Nelson, R. The Effects of Nonsteroidal Anti-Inflammatory Drugs on Blood Pressure in Hypertensive Patients. Cardiol. Rev. 2011, 19, 184–191. [Google Scholar] [CrossRef]
- Reilly, I.; FitzGerald, G. Inhibition of Thromboxane Formation In Vivo and Ex Vivo: Implications for Therapy With Platelet Inhibitory Drugs. Blood 1987, 69, 180–186. [Google Scholar] [CrossRef] [PubMed]
- Maree, A.O.; Curtin, R.J.; Dooley, M.; Conroy, R.M.; Crean, P.; Cox, D.; Fitzgerald, D.J. Platelet Response to Low-Dose Enteric-Coated Aspirin in Patients With Stable Cardiovascular Disease. J. Am. Coll. Cardiol. 2005, 46, 1258–1263. [Google Scholar] [CrossRef] [PubMed]
- Denis, M.M.; Tolley, N.D.; Bunting, M.; Schwertz, H.; Jiang, H.; Lindemann, S.; Yost, C.C.; Rubner, F.J.; Albertine, K.H.; Swoboda, K.J.; et al. Escaping the Nuclear Confines: Signal-Dependent Pre-MRNA Splicing in Anucleate Platelets. Cell 2005, 122, 379–391. [Google Scholar] [CrossRef]
- Evangelista, V.; Manarini, S.; Di Santo, A.; Capone, M.L.; Ricciotti, E.; Di Francesco, L.; Tacconelli, S.; Sacchetti, A.; D’Angelo, S.; Scilimati, A.; et al. De Novo Synthesis of Cyclooxygenase-1 Counteracts the Suppression of Platelet Thromboxane Biosynthesis by Aspirin. Circ. Res. 2006, 98, 593–595. [Google Scholar] [CrossRef]
- Cagnina, A.; Chabot, O.; Davin, L.; Lempereur, M.; Maréchal, P.; Oury, C.; Lancellotti, P. Atherosclerosis—An Inflammatory Disease. N. Engl. J. Med. 1999, 77, 302–309. [Google Scholar] [CrossRef]
- Lindemann, S.; Tolley, N.D.; Dixon, D.A.; McIntyre, T.M.; Prescott, S.M.; Zimmerman, G.A.; Weyrich, A.S. Activated Platelets Mediate Inflammatory Signaling by Regulated Interleukin 1β Synthesis. J. Cell Biol. 2001, 154, 485–490. [Google Scholar] [CrossRef]
- Brown, J.R.; DuBois, R.N. COX-2: A Molecular Target for Colorectal Cancer Prevention. J. Clin. Oncol. 2005, 23, 2840–2855. [Google Scholar] [CrossRef]
- Thun, M.J.; Jacobs, E.J.; Patrono, C. The Role of Aspirin in Cancer Prevention. Nat. Rev. Clin. Oncol. 2012, 9, 259–267. [Google Scholar] [CrossRef]
- Peto, R.; Gray, R.; Collins, R.; Wheatley, K.; Hennekens, C.; Jamrozik, K.; Warlow, C.; Hafner, B.; Thompson, E.; Norton, S.; et al. Randomised Trial of Prophylactic Daily Aspirin in British Male Doctors. Br. Med. J. (Clin. Res. Ed.) 1988, 296, 313–316. [Google Scholar] [CrossRef]
- Steering Committee of the Physicians’ Health Study Research Group. Final Report on the Aspirin Component of the Ongoing Physicians’ Health Study. N. Engl. J. Med. 1989, 321, 129–135. [Google Scholar] [CrossRef]
- Meade, T.W.; Wilkes, H.C.; Kelleher, C.C.; Roderick, P.J.; Brennan, P.J.; Wilson, C.W.; Howarth, D.J.; Stirling, Y.; Garrow, K.; Dickinson, C.J.; et al. Thrombosis Prevention Trial: Randomised Trial of Low-Intensity Oral Anticoagulation with Warfarin and Low-Dose Aspirin in the Primary Prevention of Ischaemic Heart Disease in Men at Increased Risk. Lancet 1998, 351, 233–241. [Google Scholar] [CrossRef]
- Sacco, M.; Pellegrini, F.; Roncaglioni, M.C.; Avanzini, F.; Tognoni, G.; Nicolucci, A. Primary Prevention of Cardiovascular Events with Low-Dose Aspirin and Vitamin E in Type 2 Diabetic Patients: Results of the Primary Prevention Project (PPP) Trial. Diabetes Care 2003, 26, 3264–3272. [Google Scholar] [CrossRef]
- Ridker, P.M.; Cook, N.R.; Lee, I.-M.; Gordon, D.; Gaziano, J.M.; Manson, J.E.; Hennekens, C.H.; Buring, J.E. A Randomized Trial of Low-Dose Aspirin in the Primary Prevention of Cardiovascular Disease in Women. N. Engl. J. Med. 2005, 352, 1293–1304. [Google Scholar] [CrossRef]
- Belch, J.; MacCuish, A.; Campbell, I.; Cobbe, S.; Taylor, R.; Prescott, R.; Lee, R.; Bancroft, J.; MacEwan, S.; Shepherd, J.; et al. The Prevention of Progression of Arterial Disease and Diabetes (POPADAD) Trial: Factorial Randomised Placebo Controlled Trial of Aspirin and Antioxidants in Patients with Diabetes and Asymptomatic Peripheral Arterial Disease. Br. Med. J. 2008, 337, a1840. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, H.; Nakayama, M.; Morimoto, T.; Uemura, S.; Kanauchi, M.; Doi, N.; Jinnouchi, H.; Sugiyama, S.; Saito, Y. Low-Dose Aspirin for Primary Prevention of Atherosclerotic Events in Patients with Type 2 Diabetes: A Randomized Controlled Trial. J. Am. Med. Assoc. 2008, 300, 2134–2141. [Google Scholar] [CrossRef] [PubMed]
- Collins, R.; Peto, R.; Hennekens, C.; Doll, R.; Bubes, V.; Buring, J.; Dushkesas, R.; Gaziano, M.; Brennan, P.; Meade, T.; et al. Aspirin in the Primary and Secondary Prevention of Vascular Disease: Collaborative Meta-Analysis of Individual Participant Data from Randomised Trials. Lancet 2009, 373, 1849. [Google Scholar] [CrossRef]
- Gaziano, J.M.; Brotons, C.; Coppolecchia, R.; Cricelli, C.; Darius, H.; Gorelick, P.B.; Howard, G.; Pearson, T.A.; Rothwell, P.M.; Ruilope, L.M.; et al. Use of Aspirin to Reduce Risk of Initial Vascular Events in Patients at Moderate Risk of Cardiovascular Disease (ARRIVE): A Randomised, Double-Blind, Placebo-Controlled Trial. Lancet 2018, 392, 1036–1046. [Google Scholar] [CrossRef]
- McNeil, J.J.; Wolfe, R.; Woods, R.L.; Tonkin, A.M.; Donnan, G.A.; Nelson, M.R.; Reid, C.M.; Lockery, J.E.; Kirpach, B.; Storey, E.; et al. Effect of Aspirin on Cardiovascular Events and Bleeding in the Healthy Elderly. N. Engl. J. Med. 2018, 379, 1509–1518. [Google Scholar] [CrossRef]
- Bowman, L.; Mafham, M.; Wallendszus, K.; Stevens, W.; the ASCEND Study Collaborative Group Effects of Aspirin for Primary Prevention in Persons with Diabetes Mellitus. Effects of Aspirin for Primary Prevention in Persons with Diabetes Mellitus. N. Engl. J. Med. 2018, 379, 1529–1539. [Google Scholar] [CrossRef] [PubMed]
- Zheng, S.L.; Roddick, A.J. Association of Aspirin Use for Primary Prevention with Cardiovascular Events and Bleeding Events: A Systematic Review and Meta-Analysis. J. Am. Med. Assoc. 2019, 321, 277–287. [Google Scholar] [CrossRef]
- Shah, R.; Khan, B.; Latham, S.B.; Khan, S.A.; Rao, S.V. A Meta-Analysis of Aspirin for the Primary Prevention of Cardiovascular Diseases in the Context of Contemporary Preventive Strategies. Am. J. Med. 2019, 132, 1295–1304.e3. [Google Scholar] [CrossRef] [PubMed]
- Galli, M.; Andreotti, F.; D’amario, D.; Vergallo, R.; Montone, R.A.; Porto, I.; Crea, F. Aspirin in Primary Prevention of Cardiovascular Disease in the Elderly. Eur. Heart J. Cardiovasc. Pharmacother. 2020, 6, 326–327. [Google Scholar] [CrossRef]
- Guirguis-Blake, J.M.; Evans, C.V.; Perdue, L.A.; Bean, S.I.; Senger, C.A. Aspirin Use to Prevent Cardiovascular Disease and Colorectal Cancer: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. J. Am. Med. Assoc. 2022, 327, 1585–1597. [Google Scholar] [CrossRef]
- Saito, Y.; Okada, S.; Ogawa, H.; Soejima, H.; Sakuma, M.; Nakayama, M.; Doi, N.; Jinnouchi, H.; Waki, M.; Masuda, I.; et al. Low-Dose Aspirin for Primary Prevention of Cardiovascular Events in Patients with Type 2 Diabetes Mellitus: 10-Year Follow-Up of a Randomized Controlled Trial. Circulation 2017, 135, 659–670. [Google Scholar] [CrossRef]
- Cook, N.R.; Cole, S.R.; Buring, J.E. Aspirin in the Primary Prevention of Cardiovascular Disease in the Women’s Health Study: Effect of Noncompliance. Eur. J. Epidemiol. 2012, 27, 431. [Google Scholar] [CrossRef]
- Ardeshna, D.; Khare, S.; Jagadish, P.S.; Bhattad, V.; Cave, B.; Khouzam, R.N. The Dilemma of Aspirin Resistance in Obese Patients. Ann. Transl. Med. 2019, 7, 404. [Google Scholar] [CrossRef]
- Dal Canto, E.; Ceriello, A.; Rydén, L.; Ferrini, M.; Hansen, T.B.; Schnell, O.; Standl, E.; Beulens, J.W.J. Diabetes as a Cardiovascular Risk Factor: An Overview of Global Trends of Macro and Micro Vascular Complications. Eur. J. Prev. Cardiol. 2019, 26, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Capodanno, D.; Patel, A.; Dharmashankar, K.; Ferreiro, J.L.; Ueno, M.; Kodali, M.; Tomasello, S.D.; Capranzano, P.; Seecheran, N.; Darlington, A.; et al. Pharmacodynamic Effects of Different Aspirin Dosing Regimens in Type 2 Diabetes Mellitus Patients with Coronary Artery Disease. Circ. Cardiovasc. Interv. 2011, 4, 180–187. [Google Scholar] [CrossRef]
- Spectre, G.; Arnetz, L.; Östenson, C.G.; Brismar, K.; Li, N.; Hjemdahl, P. Twice Daily Dosing of Aspirin Improves Platelet Inhibition in Whole Blood in Patients with Type 2 Diabetes Mellitus and Micro-or Macrovascular Complications. Thromb. Haemost. 2011, 106, 491–499. [Google Scholar] [CrossRef]
- DiChiara, J.; Bliden, K.P.; Tantry, U.S.; Hamed, M.S.; Antonino, M.J.; Suarez, T.A.; Bailon, O.; Singla, A.; Gurbel, P.A. The Effect of Aspirin Dosing on Platelet Function in Diabetic and Nondiabetic Patients: An Analysis from the Aspirin-Induced Platelet Effect (ASPECT) Study. Diabetes 2007, 56, 3014–3019. [Google Scholar] [CrossRef]
- Gurbel, P.A.; Bliden, K.P.; DiChiara, J.; Newcomer, J.; Weng, W.; Neerchal, N.K.; Gesheff, T.; Chaganti, S.K.; Etherington, A.; Tantry, U.S. Evaluation of Dose-Related Effects of Aspirin on Platelet Function: Results from the Aspirin-Induced Platelet Effect (ASPECT) Study. Circulation 2007, 115, 3156–3164. [Google Scholar] [CrossRef] [PubMed]
- Addad, F.; Chakroun, T.; Elalamy, I.; Abderazek, F.; Chouchene, S.; Dridi, Z.; Gerotziafas, G.T.; Hatmi, M.; Hassine, M.; Gamra, H. Antiplatelet Effect of Once- or Twice-Daily Aspirin Dosage in Stable Coronary Artery Disease Patients with Diabetes. Int. J. Hematol. 2010, 92, 296–301. [Google Scholar] [CrossRef]
- Dillinger, J.G.; Drissa, A.; Sideris, G.; Bal Dit Sollier, C.; Voicu, S.; Manzo Silberman, S.; Logeart, D.; Drouet, L.; Henry, P. Biological Efficacy of Twice Daily Aspirin in Type 2 Diabetic Patients with Coronary Artery Disease. Am. Heart J. 2012, 164, 600–606.e1. [Google Scholar] [CrossRef] [PubMed]
- Bethel, M.A.; Harrison, P.; Sourij, H.; Sun, Y.; Tucker, L.; Kennedy, I.; White, S.; Hill, L.; Oulhaj, A.; Coleman, R.L.; et al. Randomized Controlled Trial Comparing Impact on Platelet Reactivity of Twice-Daily with Once-Daily Aspirin in People with Type 2 Diabetes. Diabet. Med. 2016, 33, 224–230. [Google Scholar] [CrossRef]
- Jones, W.S.; Mulder, H.; Wruck, L.M.; Pencina, M.J.; Kripalani, S.; Muñoz, D.; Crenshaw, D.L.; Effron, M.B.; Re, R.N.; Gupta, K.; et al. Comparative Effectiveness of Aspirin Dosing in Cardiovascular Disease. N. Engl. J. Med. 2021, 384, 1981–1990. [Google Scholar] [CrossRef]
- Pulcinelli, F.M.; Biasucci, L.M.; Riondino, S.; Giubilato, S.; Leo, A.; Di Renzo, L.; Trifir, E.; Mattiello, T.; Pitocco, D.; Liuzzo, G.; et al. COX-1 Sensitivity and Thromboxane A2 Production in Type 1 and Type 2 Diabetic Patients under Chronic Aspirin Treatment. Eur. Heart J. 2009, 30, 1279–1286. [Google Scholar] [CrossRef] [PubMed]
- Santilli, F.; Vazzana, N.; Liani, R.; Guagnano, M.T.; Davì, G. Platelet Activation in Obesity and Metabolic Syndrome. Obes. Rev. 2012, 13, 27–42. [Google Scholar] [CrossRef] [PubMed]
- Cox, D.; Maree, A.O.; Dooley, M.; Conroy, R.; Byrne, M.F.; Fitzgerald, D.J. Effect of Enteric Coating on Antiplatelet Activity of Low-Dose Aspirin in Healthy Volunteers. Stroke 2006, 37, 2153–2158. [Google Scholar] [CrossRef] [PubMed]
- Norgard, N.B.; Monte, S.V.; Fernandez, S.F.; Ma, Q. Aspirin Responsiveness Changes in Obese Patients Following Bariatric Surgery. Cardiovasc. Ther. 2017, 35, e12268. [Google Scholar] [CrossRef] [PubMed]
- Petrucci, G.; Zaccardi, F.; Giaretta, A.; Cavalca, V.; Capristo, E.; Cardillo, C.; Pitocco, D.; Porro, B.; Schinzari, F.; Toffolo, G.; et al. Obesity Is Associated with Impaired Responsiveness to Once-Daily Low-Dose Aspirin and in Vivo Platelet Activation. J. Thromb. Haemost. 2019, 17, 885–895. [Google Scholar] [CrossRef] [PubMed]
- Becker, D.M.; Segal, J.; Vaidya, D.; Yanek, L.R.; Herrera-Galeano, J.E.; Bray, P.F.; Moy, T.F.; Becker, L.C.; Faraday, N. Sex Differences in Platelet Reactivity and Response to Low-Dose Aspirin Therapy. J. Am. Med. Assoc. 2006, 295, 1420–1427. [Google Scholar] [CrossRef] [PubMed]
- Qayyum, R.; Becker, D.M.; Yanek, L.R.; Moy, T.F.; Becker, L.C.; Faraday, N.; Vaidya, D. Platelet Inhibition by Aspirin 81 and 325 Mg/Day in Men versus Women without Clinically Apparent Cardiovascular Disease. Am. J. Cardiol. 2008, 101, 1359–1363. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.P.; Ryu, J.; Kim, S.H.; Yoon, H.J. Low-Dose Aspirin in the Primary Prevention of Cardiovascular Diseases: A Retrospective, Propensity Score Matched Study. Atherosclerosis 2023, 371, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Cattaneo, M.; Faioni, E.M. Why Does Ticagrelor Induce Dyspnea? Thromb. Haemost. 2012, 108, 1031–1036. [Google Scholar] [CrossRef]
- Benenati, S.; Canale, C.; De Marzo, V.; Della Bona, R.; Rosa, G.M.; Porto, I. Atrial Fibrillation and Alzheimer’s Disease: A Conundrum. Eur. J. Clin. Investig. 2021, 51, e13451. [Google Scholar] [CrossRef]
- Pollard, M.; Luckert, P.H. Effect of Indomethacin on Intestinal Tumors Induced in Rats by the Acetate Derivative of Dimethylnitrosamine. Science 1981, 214, 558–559. [Google Scholar] [CrossRef]
- Thun, M.J.; Namboodiri, M.M.; Heath, C.W. Aspirin Use and Reduced Risk of Fatal Colon Cancer. N. Engl. J. Med. 1991, 325, 1593–1596. [Google Scholar] [CrossRef]
- Kune, G.; Kune, S.; Watson, L.F. Colorectal Cancer Risk, Chronic Illnesses, Operations, and Medications: Case Control Results from the Melbourne Colorectal Cancer Study. Cancer Res. 1988, 48, 4399–4404. [Google Scholar] [CrossRef]
- Gann, P.H.; Manson, J.E.; Glynn, R.J.; Buring, J.E.; Hennekens, C.H. Low-Dose Aspirin and Incidence of Colorectal Tumors in a Randomized Trial. J. Natl. Cancer Inst. 1993, 85, 1220–1224. [Google Scholar] [CrossRef] [PubMed]
- Burn, J.; Bishop, D.T.; Mecklin, J.-P.; Macrae, F.; Möslein, G.; Olschwang, S.; Bisgaard, M.-L.; Ramesar, R.; Eccles, D.; Maher, E.R.; et al. Effect of Aspirin or Resistant Starch on Colorectal Neoplasia in the Lynch Syndrome. N. Engl. J. Med. 2008, 359, 2567–2578. [Google Scholar] [CrossRef] [PubMed]
- Cook, N.R.; Lee, I.M.; Zhang, S.M.; Moorthy, M.V.; Buring, J.E. Alternate-Day, Low-Dose Aspirin and Cancer Risk: Long-Term Observational Follow-up of a Randomized Trial. Ann. Intern. Med. 2013, 159, 77–85. [Google Scholar] [CrossRef]
- Burn, J.; Gerdes, A.M.; MacRae, F.; Mecklin, J.P.; Moeslein, G.; Olschwang, S.; Eccles, D.; Evans, D.G.; Maher, E.R.; Bertario, L.; et al. Long-Term Effect of Aspirin on Cancer Risk in Carriers of Hereditary Colorectal Cancer: An Analysis from the CAPP2 Randomised Controlled Trial. Lancet 2011, 378, 2081–2087. [Google Scholar] [CrossRef]
- Rothwell, P.M.; Wilson, M.; Elwin, C.E.; Norrving, B.; Algra, A.; Warlow, C.P.; Meade, T.W. Long-Term Effect of Aspirin on Colorectal Cancer Incidence and Mortality: 20-Year Follow-up of Five Randomised Trials. Lancet 2010, 376, 1741–1750. [Google Scholar] [CrossRef] [PubMed]
- Rothwell, P.M.; Wilson, M.; Price, J.F.; Belch, J.F.F.; Meade, T.W.; Mehta, Z. Effect of Daily Aspirin on Risk of Cancer Metastasis: A Study of Incident Cancers during Randomised Controlled Trials. Lancet 2012, 379, 1591–1601. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Zhang, R.; Yu, L.; Xiao, J.; Zhou, X.; Li, X.; Song, P.; Li, X. Aspirin Use and Common Cancer Risk: A Meta-Analysis of Cohort Studies and Randomized Controlled Trials. Front. Oncol. 2021, 11, 690219. [Google Scholar] [CrossRef]
- Bibbins-Domingo, K.; Grossman, D.C.; Curry, S.J.; Davidson, K.W.; Epling, J.W.; García, F.A.R.; Gillman, M.; Harper, D.M.; Kemper, A.R.; Krist, A.H.; et al. Aspirin Use for the Primary Prevention of Cardiovascular Disease and Colorectal Cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann. Intern. Med. 2016, 164, 836–845. [Google Scholar] [CrossRef] [PubMed]
- Mcneil, J.J.; Gibbs, P.; Orchard, S.G.; Lockery, J.E.; Bernstein, W.B.; Cao, Y.; Ford, L.; Haydon, A.; Kirpach, B.; Macrae, F.; et al. Effect of Aspirin on Cancer Incidence and Mortality in Older Adults. J. Natl. Cancer Inst. 2021, 113, 258–265. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care. Effectiveness of Aspirin in the Prevention of Colorectal Cancer in People with Lynch Syndrome; National Institute for Health and Care Excellence (NICE): London, UK, 2020. [Google Scholar]
- Di Fusco, S.A.; Cianfrocca, C.; Bisceglia, I.; Spinelli, A.; Alonzo, A.; Mocini, E.; Gulizia, M.M.; Gabrielli, D.; Oliva, F.; Imperoli, G.; et al. Potential Pathophysiologic Mechanisms Underlying the Inherent Risk of Cancer in Patients with Atherosclerotic Cardiovascular Disease. Int. J. Cardiol. 2022, 363, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Giovannucci, E.; Egan, K.M.; Hunter, D.J.; Stampfer, M.J.; Colditz, G.A.; Willett, W.C.; Speizer, F.E. Aspirin and the Risk of Colorectal Cancer in Women. N. Engl. J. Med. 1995, 333, 609–614. [Google Scholar] [CrossRef] [PubMed]
- Giovannucci, E.; Rimm, E.B.; Stampfer, M.J.; Colditz, G.A.; Ascherio, A.; Willett, W.C. Aspirin Use and the Risk for Colorectal Cancer and Adenoma in Male Health Professionals. Ann. Intern. Med. 1994, 121, 241–246. [Google Scholar] [CrossRef]
- Chan, A.T.; Ogino, S.; Fuchs, C.S. Aspirin and the Risk of Colorectal Cancer in Relation to the Expression of COX-2. N. Engl. J. Med. 2007, 356, 2131–2142. [Google Scholar] [CrossRef]
- Shechan, K.M.; Shcahan, K.; O’Donoghue, P.; Imacswecney, F.; Conroy, R.M.; Fitzgerald, D.J.; Murray, F.E. The Relationship Between Cyclooxygenase-2 Expression and Colorectal Cancer. J. Am. Med. Assoc. 1999, 282, 1254–1257. [Google Scholar] [CrossRef]
- Ogino, S.; Kirkner, G.J.; Nosho, K.; Irahara, N.; Kure, S.; Shima, K.; Hazra, A.; Chan, A.T.; Dehari, R.; Giovannucci, E.L.; et al. Cyclooxygenase-2 Expression Is an Independent Predictor of Poor Prognosis in Colon Cancer. Clin. Cancer Res. 2008, 14, 8221–8227. [Google Scholar] [CrossRef] [PubMed]
- González-Pérez, A.; García Rodríguez, L.A.; López-Ridaura, R. Effects of Non-Steroidal Anti-Inflammatory Drugs on Cancer Sites Other than the Colon and Rectum: A Metal-Analysis. BMC Cancer 2003, 3, 1–12. [Google Scholar] [CrossRef]
- Arnett, D.K.; Blumenthal, R.S.; Albert, M.A.; Buroker, A.B.; Goldberger, Z.D.; Hahn, E.J.; Himmelfarb, C.D.; Khera, A.; Lloyd-Jones, D.; McEvoy, J.W.; et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 140, e596–e646. [Google Scholar] [CrossRef]
- Davidson, K.W.; Barry, M.J.; Mangione, C.M.; Cabana, M.; Chelmow, D.; Coker, T.R.; Davis, E.M.; Donahue, K.E.; Jaén, C.R.; Krist, A.H.; et al. Aspirin Use to Prevent Cardiovascular Disease: US Preventive Services Task Force Recommendation Statement. J. Am. Med. Assoc. 2022, 327, 1577–1584. [Google Scholar] [CrossRef] [PubMed]
- Visseren, F.L.J.; MacH, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on Cardiovascular Disease Prevention in Clinical PracticeDeveloped by the Task Force for Cardiovascular Disease Prevention in Clinical Practice with Representatives of the European Society of Cardiology and 12 Medical Societies with the Special Contribution of the European Association of Preventive Cardiology (EAPC). Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association Professional Practice Committee. 10. Cardiovascular Disease and Risk Management: Standards of Medical Care in Diabetes—2022. Diabetes Care 2022, 45, S144–S174. [Google Scholar] [CrossRef]
- Aboyans, V.; Ricco, J.B.; Bartelink, M.L.E.L.; Björck, M.; Brodmann, M.; Cohnert, T.; Collet, J.P.; Czerny, M.; De Carlo, M.; Debus, S.; et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in Collaboration with the European Society for Vascular Surgery (ESVS) Document Covering Atherosclerotic Disease of Extracranial Carotid and Vertebral, Mesenteric, Renal, Upper and Lower Extremity ArteriesEndorsed by: The European Stroke Organization (ESO)The Task Force for the Diagnosis and Treatment of Peripheral Arterial Diseases of the European Society of Cardiology (ESC) and of the European Society for Vascul. Eur. Heart J. 2018, 39, 763–816. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, S.F.; Streja, E.; Zahmatkesh, G.; Streja, D.; Kashyap, M.; Moradi, H.; Molnar, M.Z.; Reddy, U.; Amin, A.N.; Kovesdy, C.P.; et al. Reverse Epidemiology of Traditional Cardiovascular Risk Factors in the Geriatric Population. J. Am. Med. Dir. Assoc. 2015, 16, 933. [Google Scholar] [CrossRef] [PubMed]
- Vaes, B.; Depoortere, D.; Van Pottelbergh, G.; Matheï, C.; Neto, J.; Degryse, J. Association between Traditional Cardiovascular Risk Factors and Mortality in the Oldest Old: Untangling the Role of Frailty. BMC Geriatr. 2017, 17, 1–8. [Google Scholar] [CrossRef] [PubMed]
- SCORE2 working group and ESC Cardiovascular risk collaboration; Hageman, S.; Pennells, L.; Ojeda, F.; Kaptoge, S.; Kuulasmaa, K.; de Vries, T.; Xu, Z.; Kee, F.; Chung, R.; et al. SCORE2 Risk Prediction Algorithms: New Models to Estimate 10-Year Risk of Cardiovascular Disease in Europe. Eur. Heart J. 2021, 42, 2439–2454. [Google Scholar] [CrossRef]
- SCORE2-OP working group and ESC Cardiovascular risk collaboration; de Vries, T.I.; Cooney, M.T.; Selmer, R.M.; Hageman, S.H.J.; Pennells, L.A.; Wood, A.; Kaptoge, S.; Xu, Z.; Westerink, J.; et al. SCORE2-OP Risk Prediction Algorithms: Estimating Incident Cardiovascular Event Risk in Older Persons in Four Geographical Risk Regions. Eur. Heart J. 2021, 42, 2455–2467. [Google Scholar] [CrossRef]
- Pennells, L.; Kaptoge, S.; Østergaard, H.B.; Read, S.H.; Carinci, F.; Franch-Nadal, J.; Petitjean, C.; Taylor, O.; Hageman, S.H.J.; Xu, Z.; et al. SCORE2-Diabetes: 10-Year Cardiovascular Risk Estimation in Type 2 Diabetes in Europe. Eur. Heart J. 2023, 44, 2544–2556. [Google Scholar] [CrossRef]
- Matsushita, K.; Kaptoge, S.; Hageman, S.H.J.; Sang, Y.; Ballew, S.H.; Grams, M.E.; Surapaneni, A.; Sun, L.; Arnlov, J.; Bozic, M.; et al. Including Measures of Chronic Kidney Disease to Improve Cardiovascular Risk Prediction by SCORE2 and SCORE2-OP. Eur. J. Prev. Cardiol. 2023, 30, 8–16. [Google Scholar] [CrossRef]
- Tokgozoglu, L.; Torp-Pedersen, C. Redefining Cardiovascular Risk Prediction: Is the Crystal Ball Clearer Now? Eur. Heart J. 2021, 42, 2468–2471. [Google Scholar] [CrossRef] [PubMed]
- Montone, R.A.; Camilli, M.; Calvieri, C.; Magnani, G.; Bonanni, A.; Bhatt, D.L.; Rajagopalan, S.; Crea, F.; Niccoli, G. Exposome in Ischaemic Heart Disease: Beyond Traditional Risk Factors. Eur. Heart J. 2024, 45, 419–438. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.S.; Coresh, J.; Pencina, M.J.; Ndumele, C.E.; Rangaswami, J.; Chow, S.L.; Palaniappan, L.P.; Sperling, L.S.; Virani, S.S.; Ho, J.E.; et al. Novel Prediction Equations for Absolute Risk Assessment of Total Cardiovascular Disease Incorporating Cardiovascular-Kidney-Metabolic Health: A Scientific Statement From the American Heart Association. Circulation 2023, 148, 1982–2004. [Google Scholar] [CrossRef] [PubMed]
- Di Fusco, S.A.; Arca, M.; Scicchitano, P.; Alonzo, A.; Perone, F.; Gulizia, M.M.; Gabrielli, D.; Oliva, F.; Imperoli, G.; Colivicchi, F. Lipoprotein(a): A Risk Factor for Atherosclerosis and an Emerging Therapeutic Target. Heart 2022, 109, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Reyes-Soffer, G.; Ginsberg, H.N.; Berglund, L.; Duell, P.B.; Heffron, S.P.; Kamstrup, P.R.; Lloyd-Jones, D.M.; Marcovina, S.M.; Yeang, C.; Koschinsky, M.L. Lipoprotein(a): A Genetically Determined, Causal, and Prevalent Risk Factor for Atherosclerotic Cardiovascular Disease: A Scientific Statement From the American Heart Association. Arterioscler. Thromb. Vasc. Biol. 2022, 42, E48–E60. [Google Scholar] [CrossRef] [PubMed]
- Bhatia, H.S.; Trainor, P.; Carlisle, S.; Tsai, M.Y.; Criqui, M.H.; Defilippis, A.; Tsimikas, S. Aspirin and Cardiovascular Risk in Individuals with Elevated Lipoprotein(a): The Multi-Ethnic Study of Atherosclerosis. J. Am. Heart Assoc. 2024, 13, 33562. [Google Scholar] [CrossRef] [PubMed]
- Razavi, A.C.; Richardson, L.C.; Coronado, F.; Dzaye, O.; Bhatia, H.S.; Mehta, A.; Quyyumi, A.A.; Vaccarino, V.; Budoff, M.J.; Nasir, K.; et al. Aspirin Use for Primary Prevention Among US Adults with and without Elevated Lipoprotein(a). Am. J. Prev. Cardiol. 2024, 18, 100674. [Google Scholar] [CrossRef]
- Agatston, A.S.; Janowitz, W.R.; Hildner, F.J.; Zusmer, N.R.; Viamonte, M.; Detrano, R. Quantification of Coronary Artery Calcium Using Ultrafast Computed Tomography. J. Am. Coll. Cardiol. 1990, 15, 827–832. [Google Scholar] [CrossRef] [PubMed]
- Arad, Y.; Spadaro, L.A.; Goodman, K.; Newstein, D.; Guerci, A.D. Prediction of Coronary Events with Electron Beam Computed Tomography. J. Am. Coll. Cardiol. 2000, 36, 1253–1260. [Google Scholar] [CrossRef]
- Detrano, R.; Guerci, A.D.; Carr, J.J.; Bild, D.E.; Burke, G.; Folsom, A.R.; Liu, K.; Shea, S.; Szklo, M.; Bluemke, D.A.; et al. Coronary Calcium as a Predictor of Coronary Events in Four Racial or Ethnic Groups. N. Engl. J. Med. 2008, 358, 1336–1345. [Google Scholar] [CrossRef]
- Razavi, A.C.; Shaw, L.J.; Berman, D.S.; Budoff, M.J.; Wong, N.D.; Vaccarino, V.; van Assen, M.; De Cecco, C.N.; Quyyumi, A.A.; Mehta, A.; et al. Left Main Coronary Artery Calcium and Diabetes Confer Very-High-Risk Equivalence in Coronary Artery Calcium >1,000. Cardiovasc. Imaging 2023, 17, 766–776. [Google Scholar] [CrossRef] [PubMed]
- Miedema, M.D.; Duprez, D.A.; Misialek, J.R.; Blaha, M.J.; Nasir, K.; Silverman, M.G.; Blankstein, R.; Budoff, M.J.; Greenland, P.; Folsom, A.R. Use of Coronary Artery Calcium Testing to Guide Aspirin Utilization for Primary Prevention: Estimates from the Multi-Ethnic Study of Atherosclerosis. Circ. Cardiovasc. Qual. Outcomes 2014, 7, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Nasir, K.; Bittencourt, M.S.; Blaha, M.J.; Blankstein, R.; Agatson, A.S.; Rivera, J.J.; Miemdema, M.D.; Sibley, C.T.; Shaw, L.J.; Blumenthal, R.S.; et al. Implications of Coronary Artery Calcium Testing Among Statin Candidates According to American College of Cardiology/American Heart Association Cholesterol Management Guidelines: MESA (Multi-Ethnic Study of Atherosclerosis). J. Am. Coll. Cardiol. 2015, 66, 1657–1668. [Google Scholar] [CrossRef] [PubMed]
- Cainzos-Achirica, M.; Miedema, M.D.; McEvoy, J.W.; Al Rifai, M.; Greenland, P.; Dardari, Z.; Budoff, M.; Blumenthal, R.S.; Yeboah, J.; Duprez, D.A.; et al. Coronary Artery Calcium for Personalized Allocation of Aspirin in Primary Prevention of Cardiovascular Disease in 2019. Circulation 2020, 141, 1541–1553. [Google Scholar] [CrossRef]
- Mansour, K.; Taher, A.T.; Musallam, K.M.; Alam, S. Aspirin Resistance. Adv. Hematol. 2009, 937352. [Google Scholar] [CrossRef] [PubMed]
- Galli, M.; Benenati, S.; Capodanno, D.; Franchi, F.; Rollini, F.; D’Amario, D.; Porto, I.; Angiolillo, D.J. Guided versus Standard Antiplatelet Therapy in Patients Undergoing Percutaneous Coronary Intervention: A Systematic Review and Meta-Analysis. Lancet 2021, 397, 1470–1483. [Google Scholar] [CrossRef] [PubMed]
- Galli, M.; Benenati, S.; Franchi, F.; Rollini, F.; Capodanno, D.; Biondi-Zoccai, G.; Vescovo, G.M.; Cavallari, L.H.; Bikdeli, B.; Ten Berg, J.; et al. Comparative Effects of Guided vs. Potent P2Y12 Inhibitor Therapy in Acute Coronary Syndrome: A Network Meta-Analysis of 61 898 Patients from 15 Randomized Trials. Eur. Heart J. 2022, 43, 959–967. [Google Scholar] [CrossRef]
- Akintoye, E.; Afonso, L.; Jayanna, M.B.; Bao, W.; Briasoulis, A.; Robinson, J. Prognostic Utility of Risk Enhancers and Coronary Artery Calcium Score Recommended in the 2018 ACC/AHA Multisociety Cholesterol Treatment Guidelines over the Pooled Cohort Equation: Insights from 3 Large Prospective Cohorts. J. Am. Heart Assoc. Cardiovasc. Cerebrovasc. Dis. 2021, 10, 19589. [Google Scholar] [CrossRef]
- Yusuf, S.; Joseph, P.; Dans, A.; Gao, P.; Teo, K.; Xavier, D.; López-Jaramillo, P.; Yusoff, K.; Santoso, A.; Gamra, H.; et al. Polypill with or without Aspirin in Persons without Cardiovascular Disease. N. Engl. J. Med. 2021, 384, 216–228. [Google Scholar] [CrossRef]
- Safi, U.; Khan, M.M.; Ahmad, N.; Lone, M.; Neal, S.; Kleiman, M.; Adeel Arshad, M.; Vardhmaan Jain, M.; Mahmoud Al Rifai, M.M.; Hassaan, B.; et al. Aspirin with or without Statin in Individuals without Atherosclerotic Cardiovascular Disease Across Risk Categories. JACC Adv. 2023, 2, 100197. [Google Scholar] [CrossRef]
- Lanas, A.; Fuentes, J.; Benito, R.; Serrano, P.; Bajador, E.; Sáinz, R. Helicobacter Pylori Increases the Risk of Upper Gastrointestinal Bleeding in Patients Taking Low-Dose Aspirin. Aliment. Pharmacol. Ther. 2002, 16, 779–786. [Google Scholar] [CrossRef] [PubMed]
- Steffel, J.; Eikelboom, J.W.; Anand, S.S.; Shestakovska, O.; Yusuf, S.; Fox, K.A.A. The COMPASS Trial: Net Clinical Benefit of Low-Dose Rivaroxaban plus Aspirin as Compared with Aspirin in Patients with Chronic Vascular Disease. Circulation 2020, 142, 40–48. [Google Scholar] [CrossRef] [PubMed]

| Guidelines | Recommendation | Class | Level |
|---|---|---|---|
| 2019 American College of Cardiology/American Heart Association (ACC/AHA) Guideline on the Primary Prevention of Cardiovascular Disease | Low-dose aspirin (75–100 mg orally daily) might be considered for the primary prevention of ASCVD among select adults 40 to 70 years of age who are at higher ASCVD risk but not at increased bleeding risk. | IIb | A |
| Low-dose aspirin (75–100 mg orally daily) should not be administered on a routine basis for the primary prevention of ASCVD among adults > 70 years of age. | III | B-R | |
| Low-dose aspirin (75–100 mg orally daily) should not be administered for the primary prevention of ASCVD among adults of any age who are at increased risk of bleeding. | III | C-LD | |
| 2023 American Diabetes Association (ADA) “Standards of Medical Care in Diabetes” | Aspirin therapy (75–162 mg/day) may be considered as a primary prevention strategy in those with diabetes who are at increased cardiovascular risk, after a comprehensive discussion with the patient on the benefits versus the comparable increased risk of bleeding. | IIb | A |
| Aspirin is not recommended for those at low risk of ASCVD (such as men and women, aged < 50 years old with diabetes with no other major ASCVD risk factors) as the low benefit is likely to be outweighed by the risks of bleeding. | III | N.A. | |
| 2022 Aspirin Use to Prevent Cardiovascular Disease: US Preventive Services Task Force (USPSTF) Recommendation Statement | The decision to initiate low-dose aspirin use for the primary prevention of CVD in adults aged 40 to 59 years old who have a 10% or greater 10-year CVD risk should be an individual one. Evidence indicates that the net benefit of aspirin use in this group is small. Persons who are not at increased risk for bleeding and are willing to take low-dose aspirin daily are more likely to benefit. | N.A. | C |
| The USPSTF recommends against initiating low-dose aspirin use for the primary prevention of CVD in adults 60 years or older. | III | D | |
| 2021 European Society of Cardiology (ESC) Guidelines on cardiovascular disease prevention in clinical practice | In patients with DM at high or very high CVD risk, low-dose aspirin may be considered for primary prevention in the absence of clear contraindications. | IIb | A |
| Antiplatelet therapy is not recommended in individuals with low/moderate CVD risk due to the increased risk of major bleeding. | III | A | |
| 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS) | In patients with symptomatic carotid stenosis, long-term SAPT is recommended. | I | A |
| In patients with asymptomatic > 50% carotid artery stenosis, long-term antiplatelet therapy (commonly low-dose aspirin) should be considered when the bleeding risk is low. | IIa | C | |
| Long-term SAPT is recommended in symptomatic patients with LEAD. | I | A | |
| Because of a lack of proven benefit, antiplatelet therapy is not routinely indicated in patients with isolated asymptomatic LEAD. | III | A |
| Traditional Cardiovascular Risk Factors | |
|---|---|
| Age | Sex |
| Blood pressure | Blood cholesterol |
| Cigarette smoking | Diabetes Mellitus |
| Adiposity | Lifestyle (nutrition and physical activity) |
| 2019 ACC/AHA risk enhancers | 2021 ESC risk modifiers |
| Family history of premature ASCVD | Family history |
| Primary hypercholesterolemia | Genetics |
| Metabolic syndrome | Body composition |
| Chronic kidney disease | Frailty |
| History of premature menopause and history of pregnancy-associated conditions that increase later ASCVD risk | Imaging (CAC, CCTA, IMT, ABI) |
| High-risk race/ethnicity | Ethnicity |
| Chronic inflammatory conditions (psoriasis, lupus, RA, HIV/AIDS, etc.) | Biomarkers |
| Lipids/biomarkers: associated with increased ASCVD risk | Psychosocial factors |
| Persistently elevated, primary hypertriglyceridemia (≥175 mg/dL) | Socioeconomic determinants |
| Elevated high-sensitivity C-reactive protein (≥2.0 mg/L) | Environmental exposure |
| Elevated Lp(a): ≥50 mg/dL or ≥125 nmol/L constitutes a risk-enhancing factor especially at higher levels of Lp(a) | Clinical conditions (CKD, AF, COPD, Cancer, HF, inflammatory conditions, infections, sleeping and mental disorders) |
| Elevated apoB: ≥130 mg/dL corresponds to an LDL-C ≥ 160 mg/dL and constitutes a risk-enhancing factor | |
| ABI < 0.9 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Della Bona, R.; Giubilato, S.; Palmieri, M.; Benenati, S.; Rossini, R.; Di Fusco, S.A.; Novarese, F.; Mascia, G.; Gasparetto, N.; Di Monaco, A.; et al. Aspirin in Primary Prevention: Looking for Those Who Enjoy It. J. Clin. Med. 2024, 13, 4148. https://doi.org/10.3390/jcm13144148
Della Bona R, Giubilato S, Palmieri M, Benenati S, Rossini R, Di Fusco SA, Novarese F, Mascia G, Gasparetto N, Di Monaco A, et al. Aspirin in Primary Prevention: Looking for Those Who Enjoy It. Journal of Clinical Medicine. 2024; 13(14):4148. https://doi.org/10.3390/jcm13144148
Chicago/Turabian StyleDella Bona, Roberta, Simona Giubilato, Marco Palmieri, Stefano Benenati, Roberta Rossini, Stefania Angela Di Fusco, Filippo Novarese, Giuseppe Mascia, Nicola Gasparetto, Antonio Di Monaco, and et al. 2024. "Aspirin in Primary Prevention: Looking for Those Who Enjoy It" Journal of Clinical Medicine 13, no. 14: 4148. https://doi.org/10.3390/jcm13144148
APA StyleDella Bona, R., Giubilato, S., Palmieri, M., Benenati, S., Rossini, R., Di Fusco, S. A., Novarese, F., Mascia, G., Gasparetto, N., Di Monaco, A., Gatto, L., Zilio, F., Sorini Dini, C., Borrello, F., Geraci, G., Riccio, C., De Luca, L., Colivicchi, F., Grimaldi, M., ... Oliva, F. G. (2024). Aspirin in Primary Prevention: Looking for Those Who Enjoy It. Journal of Clinical Medicine, 13(14), 4148. https://doi.org/10.3390/jcm13144148









