Pelvic Fixation for Non-Ambulatory Patients with Neuromuscular Scoliosis Treated with Magnetically Controlled Growing Rods—A 4-Year Comparison of Two Different Fixation Methods
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Data Collection
- Preoperative data: demographics [age, sex, body mass index, American Society of Anesthesiologists class, neuromuscular disease type], ambulatory status, and preoperative hemoglobin value.
- Surgical details: type of pelvic fixation, duration of surgery, intraoperative blood loss, use of intraoperative neurophysiological monitoring, use of cell salvage device, red blood cell (auto-) transfusion, use of rib cradles or thoracic screw placement, pedicle screw placement at the lumbar spine and sacrum, number of pedicle screws used, vancomycin use, hemoglobin low point, and postoperative hemoglobin value.
- Radiographic data: severity of NMS measured by Cobb angle, side of convexity, pelvic horizontal obliquity (PO), lumbar lordosis (LL), highest instrumented vertebra, and corresponding follow-up measurements at each time point.
- Postoperative data: In-hospital and complications throughout the follow-up period, follow-up duration, and BMI change.
2.3. Operative Technique
2.4. In-Hospital Care
2.5. Follow-Up Care
2.6. Statistical Analysis
3. Results
3.1. Patient Demographics
3.2. Operative Data
3.3. Radiological Follow-Up
3.4. Mechanical Complications
4. Discussion
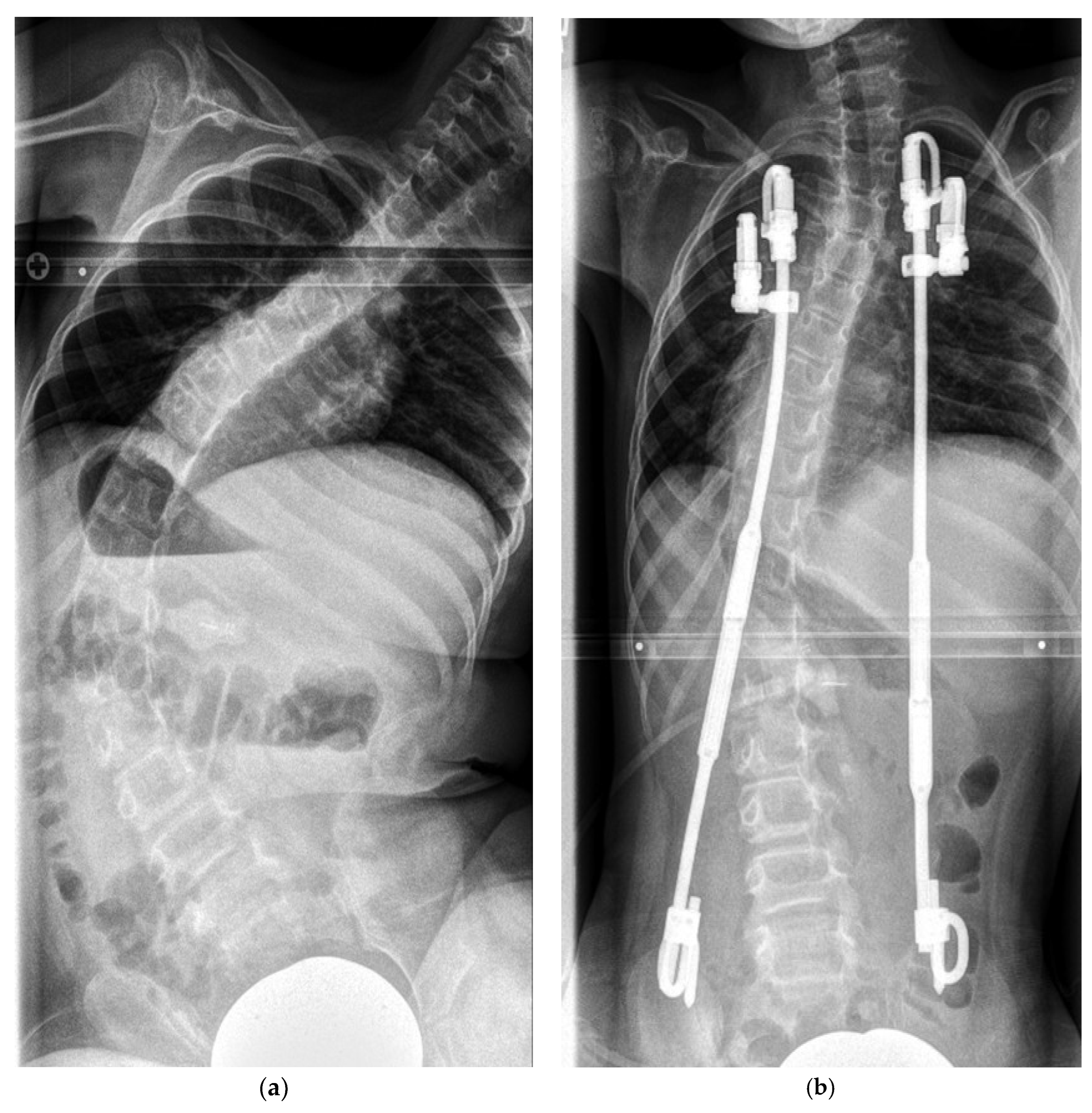
- (A)
- Horizontal PO correction was successfully achieved and maintained over the mean duration of 55 months. This result was independent of the pelvic fixation method.
- (B)
- The S-hook subgroup presented with more severe scoliosis at baseline and experienced a significant higher rate of UPROR.
- (C)
- SAI screw fixation led to a substantially greater initial correction of scoliosis, which was effectively maintained throughout the treatment period.
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ruiz, G.; Torres-Lugo, N.J.; Marrero-Ortiz, P.; Guzmán, H.; Olivella, G.; Ramírez, N. Early-onset scoliosis: A narrative review. EFORT Open Rev. 2022, 7, 599–610. [Google Scholar] [CrossRef] [PubMed]
- De Salvatore, S.; Oggiano, L.; Sessa, S.; Curri, C.; Fumo, C.; Costici, P.F.; Ruzzini, L. Patients treated by magnetic growing rods for early-onset scoliosis reach the expected average growth. Spine Deform. 2024, 12, 843–851. [Google Scholar] [CrossRef] [PubMed]
- Mehta, J.S.; Tognini, M.; Hothi, H. Growing rods in Early Onset Scoliosis: The current scenario. J. Orthop. 2023, 42, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Stücker, R.; Mladenov, K.; Stücker, S. Mitwachsende Korrektursysteme bei Early-Onset-Skoliosen. Oper. Orthopädie Traumatol. 2024, 36, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Bess, S.; Akbarnia, B.A.; Thompson, G.H.; Sponseller, P.D.; A Shah, S.; El Sebaie, H.; Boachie-Adjei, O.; Karlin, L.I.; Canale, S.; Poe-Kochert, C.; et al. Complications of growing-rod treatment for early-onset scoliosis: Analysis of one hundred and forty patients. J. Bone Jt. Surg. Am. 2010, 92, 2533–2543. [Google Scholar] [CrossRef] [PubMed]
- Takaso, M.; Moriya, H.; Kitahara, H.; Minami, S.; Takahashi, K.; Isobe, K.; Yamagata, M.; Otsuka, Y.; Nakata, Y.; Inoue, M. New remote-controlled growing-rod spinal instrumentation possibly applicable for scoliosis in young children. J. Orthop. Sci. 1998, 3, 336–340. [Google Scholar] [CrossRef] [PubMed]
- Gaumé, M.; Saghbiny, E.; Richard, L.; Thouement, C.; Vialle, R.; Miladi, L. Pelvic Fixation Technique Using the Ilio-Sacral Screw for 173 Neuromuscular Scoliosis Patients. Children 2024, 11, 199. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, H.; Fano, A.N.; Ball, J.; Roye, B.D.; George, A.; Garg, S.; Erickson, M.; Samdani, A.; Skaggs, D.; Roye, D.P.; et al. Uncorrected Pelvic Obliquity Is Associated with Worse Health-related Quality of Life (HRQoL) in Children and Their Caregivers at the End of Surgical Treatment for Early Onset Scoliosis (EOS). J. Pediatr. Orthop. 2022, 42, e390–e396. [Google Scholar] [CrossRef]
- Douleh, D.G.; Greig, D.; Thompson, R.; Garg, S. When Should Instrumentation to the Pelvis be Considered in Minimally Ambulatory Adolescents with Neuromuscular Scoliosis? J. Pediatr. Orthop. 2021, 41 (Suppl. S1), S53–S58. [Google Scholar] [CrossRef]
- Alexander, M.S.; Anderson, K.D.; Biering-Sorensen, F.; Blight, A.R.; Brannon, R.; Bryce, T.N.; Creasey, G.; Catz, A.; Curt, A.; Donovan, W.; et al. Outcome measures in spinal cord injury: Recent assessments and recommendations for future directions. Spinal Cord 2009, 47, 582–591. [Google Scholar] [CrossRef]
- Ramirez, N.; Flynn, J.M.; Smith, J.T.; Vitale, M.; Sturm, P.F.; D’amato, C.; Samdani, A.; Machiavelli, R.; El-Hawary, R. Use of the S-hook for Pelvic Fixation in Rib-Based Treatment of Early-Onset Scoliosis: A Multicenter Study. Spine 2015, 40, 816–822. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [PubMed]
- Sponseller, P.D.; Zimmerman, R.M.; Ko, P.S.; ter Gunne, A.F.P.; Mohamed, A.S.; Chang, T.-L.; Kebaish, K.M. Low profile pelvic fixation with the sacral alar iliac technique in the pediatric population improves results at two-year minimum follow-up. Spine 2010, 35, 1887–1892. [Google Scholar] [CrossRef] [PubMed]
- Smith, J.T. Bilateral rib-to-pelvis technique for managing early-onset scoliosis. Clin. Orthop. Relat. Res. 2011, 469, 1349–1355. [Google Scholar] [CrossRef] [PubMed]
- Cobb, J. Outline for the study of scoliosis. Instr. Course Lect. 1948, 5, 261–275. [Google Scholar]
- Osebold, W.R.; Mayfield, J.K.; Winter, R.B.; Moe, J.H. Surgical treatment of paralytic scoliosis associated with myelomeningocele. J. Bone Jt. Surg. Am. 1982, 64, 841–856. [Google Scholar] [CrossRef]
- Thakar, C.; Kieser, D.C.; Mardare, M.; Haleem, S.; Fairbank, J.; Nnadi, C. Systematic review of the complications associated with magnetically controlled growing rods for the treatment of early onset scoliosis. Eur. Spine J. 2018, 27, 2062–2071. [Google Scholar] [CrossRef] [PubMed]
- Grabala, P.; Gupta, M.C.; Pereira, D.E.; Latalski, M.; Danielewicz, A.; Glowka, P.; Grabala, M. Radiological Outcomes of Magnetically Controlled Growing Rods for the Treatment of Children with Various Etiologies of Early-Onset Scoliosis—A Multicenter Study. J. Clin. Med. 2024, 13, 1529. [Google Scholar] [CrossRef] [PubMed]
- Welborn, M.C.; Bouton, D. Outcomes of MCGR at >3 year average follow-up in severe scoliosis: Who undergoes elective revision vs UPROR? Spine Deform. 2022, 10, 457–463. [Google Scholar] [CrossRef]
- Urbański, W.; Tucker, S.; Ember, T.; Nadarajah, R. Single vs dual rod constructs in early onset scoliosis treated with magnetically controlled growing rods. Adv. Clin. Exp. Med. 2020, 29, 1169–1174. [Google Scholar] [CrossRef]
- Lebel, D.E.; Rocos, B.; Helenius, I.; Sigal, A.; Struder, D.; Yazici, M.; Bekmez, S.; Hasler, C.-C.; Pesenti, S.; Jouve, J.-L.; et al. Magnetically Controlled Growing Rods Graduation: Deformity Control with High Complication Rate. Spine 2021, 46, E1105–E1112. [Google Scholar] [CrossRef] [PubMed]
- Ilharreborde, B.; Ponchelet, L.; de Gauzy, J.S.; Choufani, E.; Baudoux, M.; Pesenti, S.; Simon, A.-L. How does magnetically controlled growing rods insertion affect sagittal alignment in ambulatory early onset scoliosis patients? Eur. Spine J. 2022, 31, 1036–1044. [Google Scholar] [CrossRef] [PubMed]
- Buckland, A.J.; Woo, D.; Graham, H.K.; Vasquez-Montes, D.; Cahill, P.; Errico, T.J.; Sponseller, P.D.; Harms Study Group. Residual lumbar hyperlordosis is associated with worsened hip status 5 years after scoliosis correction in non-ambulant patients with cerebral palsy. Spine Deform. 2021, 9, 1125–1136. [Google Scholar] [CrossRef] [PubMed]
- Murphy, R.F.; Mooney, J.F., 3rd. The Crankshaft Phenomenon. J. Am. Acad. Orthop. Surg. 2017, 25, e185–e193. [Google Scholar] [CrossRef] [PubMed]
- Roberts, S.B.; Tsirikos, A.I. Paediatric Spinal Deformity Surgery: Complications and Their Management. Healthcare 2022, 10, 2519. [Google Scholar] [CrossRef] [PubMed]
- Okuwaki, S.; Kotani, T.; Taniguchi, Y.; Suzuki, T.; Yamaguchi, T.; Demura, S.; Wada, K.; Sugawara, R.; Takeshita, K.; Watanabe, K.; et al. Evaluation of crankshaft phenomenon after posterior fusion for early onset scoliosis using an inverse trigonometric function: A multicenter retrospective cohort study. Spine Deform. 2024. [Google Scholar] [CrossRef]
- Upasani, V.V.; Hedequist, D.J.; Hresko, M.T.; Karlin, L.I.; Emans, J.B.; Glotzbecker, M.P. Spinal deformity progression after posterior segmental instrumentation and fusion for idiopathic scoliosis. J. Child. Orthop. 2015, 9, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Kioschos, H.C.; Asher, M.A.; Lark, R.G.; Harner, E.J. Overpowering the crankshaft mechanism. The effect of posterior spinal fusion with and without stiff transpedicular fixation on anterior spinal column growth in immature canines. Spine 1996, 21, 1168–1173. [Google Scholar] [CrossRef]
- Lemans, J.V.; Tabeling, C.S.; Scholten, E.P.; Stempels, H.W.; Miladi, L.; Castelein, R.M.; Kruyt, M.C. Surgical treatment of neuromuscular Early Onset Scoliosis with a bilateral posterior one-way rod compared to the Spring Distraction System: Study protocol for a limited-efficacy Randomized Controlled Trial (BiPOWR). BMC Musculoskelet. Disord. 2023, 24, 20. [Google Scholar] [CrossRef]
- Yang, M.J.; Rompala, A.; Samuel, S.P.; Samdani, A.; Pahys, J.; Hwang, S. Autofusion with Magnetically Controlled Growing Rods: A Case Report. Cureus 2023, 15, e36638. [Google Scholar] [CrossRef]
- Li, Y.; Swallow, J.; Gagnier, J.; Smith, J.T.; Murphy, R.F.; Sponseller, P.D.; Cahill, P.J.; Pediatric Spine Study Group. Pelvic fixation is not always necessary in children with cerebral palsy scoliosis treated with growth-friendly instrumentation. Spine Deform. 2022, 10, 925–932. [Google Scholar] [CrossRef] [PubMed]
- Sponseller, P.D.; Yang, J.S.; Thompson, G.H.; McCarthy, R.E.; Emans, J.B.; Skaggs, D.L.; Asher, M.A.; Yazici, M.; Poe-Kochert, C.; Akbarnia, B.A.; et al. Pelvic Fixation of Growing Rods: Comparison of Constructs. Spine 2009, 34, 1706–1710. [Google Scholar] [CrossRef]
- Tøndevold, N.; Lastikka, M.; Andersen, T.; Gehrchen, M.; Helenius, I. Should instrumented spinal fusion in nonambulatory children with neuromuscular scoliosis be extended to L5 or the pelvis? Bone Jt. J. 2020, 102-B, 261–267. [Google Scholar] [CrossRef]
- Nielsen, E.; Andras, L.M.; Bellaire, L.L.; Fletcher, N.D.; Minkara, A.; Vitale, M.G.; Troy, M.; Glotzbecker, M.; Skaggs, D.L. Don’t You Wish You Had Fused to the Pelvis the First Time: A Comparison of Reoperation Rate and Correction of Pelvic Obliquity. Spine 2019, 44, E465–E469. [Google Scholar] [CrossRef] [PubMed]
- Cottrill, E.; Margalit, A.; Brucker, C.; Sponseller, P.D. Comparison of Sacral-Alar-Iliac and Iliac-Only Methods of Pelvic Fixation in Early-Onset Scoliosis at 5.8 Years’ Mean Follow-up. Spine Deform. 2019, 7, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Brooks, J.T.; Jain, A.; Sanchez-Perez-Grueso, F.; Skaggs, D.L.; Thompson, G.H.; Akbarnia, B.A.; Sponseller, P.D. Outcomes of Pelvic Fixation in Growing Rod Constructs: An Analysis of Patients with a Minimum of 4 Years of Follow-up. Spine Deform. 2016, 4, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Schur, M.; Andras, L.M.; Murgai, R.; Siddiqui, A.A.; Gonsalves, N.R.; Sponseller, P.D.; Emans, J.B.; Vitale, M.G.; Skaggs, D.L. Pelvic Obliquity Correction in Distraction-Based Growth Friendly Implants. Spine Deform. 2019, 7, 985–991. [Google Scholar] [CrossRef]
- Abol Oyoun, N.; Stuecker, R. Bilateral rib-to-pelvis Eiffel Tower VEPTR construct for children with neuromuscular scoliosis: A preliminary report. Spine J. 2014, 14, 1183–1191. [Google Scholar] [CrossRef]



| Variables | All | SH | SAI | p-Value |
|---|---|---|---|---|
| Female (%, n) | 54% (22) | 66.7% (14) | 40% (8) | 0.087 |
| Age (years; mean ± SD) | 9.4 ± 1.9 | 9.3 ± 2 | 9.5 ± 1.8 | 0.734 |
| BMI (kg/mL; mean ± SD) | 14.8 ± 3.7 | 15.3 ± 4 | 14.2 ± 3.1 | 0.338 |
| BMI Z-score (mean ± SD) | −3.3 ± 3.6 | −2.8 ± 3.7 | −3.7 ± 3.5 | 0.446 |
| Neuromuscular disease | 0.325 | |||
| ICP V (%, n) | 31.7% (13) | 38.1% (8) | 25% (5) | |
| SMA 2 (%, n) | 29.3% (12) | 28.6% (6) | 30% (6) | |
| Myopathy (%, n) | 12.2% (5) | 9.5% (2) | 15% (3) | |
| AMC (%, n) | 7.3% (3) | 1, 4.8% (1) | 10% (2) | |
| MMC (%, n) | 4.9% (2) | 9.5% (2) | 0% (0) | |
| Chromosomal (%, n) | 4.9% (2) | 0% (0) | 10% (2) | |
| Flaccid paraplegia (%, n) | 4.9% (2) | 9.5% (2) | 0% (0) | |
| Rett syndrome (%, n) | 2.4% (1) | 0% (0) | 5% (1) | |
| MCD1A (%, n) | 2.4% (1) | 0% (0) | 5% (1) | |
| Operative time (min, mean ± SD) | 159 ± 58 | 116 ± 31 | 204 ± 43 | <0.001 |
| Unplanned revision surgery (%, n) | 22% (9) | 38.1% (8) | 5% (1) | 0.010 |
| Blood (Re-)transfusion (%, n) | 41.5% (17) | 0% (0) | 85% (17) | <0.001 |
| Hb low point (mean ± SD) | 8.9 ± 1.5 | 9.9 ± 1 | 7.8 ± 1.2 | <0.001 |
| Hb change pre- to postoperative (mean ± SD) | −2.8 ± 2.1 | −1.7 ± 1.2 | −3.9 ± 2.3 | <0.001 |
| Follow-up (month, mean ± SD) | 54.6 ± 17.5 | 59.3 ± 19.6 | 49.7 ± 13.8 | 0.079 |
| SH Subgroup | SAI Subgroup | ||||||
|---|---|---|---|---|---|---|---|
| Patient No. | Convex Side | Curve Degree | Horizontal Pelvic Obliquity | Patient No. | Convex Side | Curve Degree | Horizontal Pelvic Obliquity |
| 1 | Left | 109 | 26 | 1 | Right | 68 | 17 |
| 2 | Left | 84 | 5 | 2 | Left | 60 | 19 |
| 3 | Left | 87 | 15 | 3 | Left | 53 | 10 |
| 4 | Right | 96 | 8 | 4 | Right | 90 | 7 |
| 5 | Left | 94 | 9 | 5 | Right | 62 | 22 |
| 6 | Right | 68 | 11 | 6 | Left | 100 | 30 |
| 7 | Left | 85 | 60 | 7 | Right | 72 | 12 |
| 8 | Right | 81 | 13 | 8 | Right | 57 | 32 |
| 9 | Left | 102 | 34 | 9 | Right | 96 | 14 |
| 10 | Right | 81 | 33 | 10 | Right | 70 | 30 |
| 11 | Right | 110 | 32 | 11 | Right | 109 | 37 |
| 12 | Left | 105 | 25 | 12 | Right | 35 | 18 |
| 13 | Left | 82 | 15 | 13 | Left | 56 | 16 |
| 14 | Right | 98 | 25 | 14 | Left | 85 | 35 |
| 15 | Left | 88 | 8 | 15 | Right | 62 | 7 |
| 16 | Left | 57 | 10 | 16 | Left | 55 | 27 |
| 17 | Right | 68 | 11 | 17 | Left | 70 | 20 |
| 18 | Left | 83 | 34 | 18 | Left | 78 | 30 |
| 19 | Right | 81 | 20 | 19 | Right | 98 | 51 |
| 20 | Left | 98 | 20 | 20 | Right | 82 | 26 |
| 21 | Left | 116 | 27 | ||||
| Variable | All Subjects | SH Subgroup | SAI Subgroup | p-Value | |||
|---|---|---|---|---|---|---|---|
| Mean | ±SD | Mean | ±SD | Mean | ±SD | ||
| Preoperatively | |||||||
| Main curve | 81.2 | 18.8 | 89.2 | 14.9 | 72.9 | 19.0 | 0.008 |
| Pelvic obliquity | 22.0 | 12.1 | 21.0 | 13.1 | 23.0 | 11.2 | 0.603 |
| Postoperatively | |||||||
| Main curve | 36.1 | 19.7 | 44.2 | 19.3 | 27.7 | 16.7 | 0.007 |
| Curve correction (%) | 56.6 | 18.6 | 41.7 | 16.4 | 63.0 | 18.3 | 0.045 |
| Pelvic obliquity | 6.4 | 5.8 | 7.43 | 5.6 | 5.4 | 5.8 | 0.266 |
| Short Term (ST) Follow-up | |||||||
| Main curve | 41.1 | 19.7 | 51.1 | 15.2 | 30.7 | 17.5 | 0.001 |
| Curve correction (%) | 48.9 | 20.1 | 43.7 | 15.6 | 58.5 | 19.2 | 0.038 |
| Pelvic obliquity | 6.4 | 6.3 | 7.2 | 5.0 | 6.0 | 5.6 | 0.494 |
| Mid Term (MT) Follow-up | |||||||
| Main curve | 72.4 | 15.8 | 51.5 | 14.1 | 32.6 | 20.3 | 0.003 |
| Curve correction (%) | 48.8 | 20.1 | 41.4 | 16.4 | 56.6 | 21.1 | 0.047 |
| Pelvic obliquity | 5.5 | 4.4 | 6.7 | 5.0 | 6.1 | 3.8 | 0.648 |
| Long Term (LT) Follow-up | |||||||
| Main curve | 48.2 | 19.8 | 59.4 | 14.9 | 38.2 | 17.9 | <0.001 |
| Curve correction (%) | 40.9 | 21.4 | 32.4 | 18.2 | 49.7 | 21.2 | 0.007 |
| Pelvic obliquity | 6.2 | 3.3 | 6.2 | 3.5 | 6.2 | 3.1 | 1.00 |
| Growth at Last Follow-up | |||||||
| Last BMI (kg/mL) | 16.1 | 4.2 | 16.1 | 4.0 | 16.1 | 4.5 | 0.990 |
| Last BMI Z-score | −2.9 | 4.1 | −2.1 | 2.6 | −3.7 | 5.2 | 0.241 |
| Z-score change from preop | 0.4 | 3.9 | 0.7 | 3.9 | 0.04 | 3.9 | 0.584 |
| Variable | All Subjects | SH Subgroup | SAI Subgroup | p-Value | |||
|---|---|---|---|---|---|---|---|
| Mean | ±SD | Mean | ±SD | Mean | ±SD | ||
| Preoperatively | |||||||
| LL | 25 | 29 | 25 | 25.0 | 26 | 33.0 | 0.754 |
| Postoperatively | |||||||
| LL | 36 | 15 | 34 | 16.0 | 35 | 14.0 | 0.855 |
| Delta PräOP-PostOP | 10 | 25 | 11.0 | 20.0 | 11.0 | 31.0 | 0.933 |
| Short Term (ST) Follow-up | |||||||
| LL | 35 | 14 | 34 | 16.0 | 36 | 14.0 | 0.865 |
| Delta PostOP-ST | −0.5 | 5 | −2 | 6.0 | 0.9 | 4.0 | 0.215 |
| Mid Term (MT) Follow-up | |||||||
| LL | 35 | 9 | 34 | 13.0 | 36 | 14.0 | 0.865 |
| Delta ST-MT | −0.5 | 16 | −0.3 | 8.0 | 0.8 | 11.0 | 0.098 |
| Long Term (LT) Follow-up | |||||||
| LL | 36 | 18 | 34 | 19.0 | 38 | 17.0 | 0.348 |
| Delta MT-LT | 0.7 | 11 | 0.1 | 12.0 | 2.4 | 10.0 | 0.705 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heuer, A.; Stuecker, S.; Stuecker, R.; Mladenov, K. Pelvic Fixation for Non-Ambulatory Patients with Neuromuscular Scoliosis Treated with Magnetically Controlled Growing Rods—A 4-Year Comparison of Two Different Fixation Methods. J. Clin. Med. 2024, 13, 3845. https://doi.org/10.3390/jcm13133845
Heuer A, Stuecker S, Stuecker R, Mladenov K. Pelvic Fixation for Non-Ambulatory Patients with Neuromuscular Scoliosis Treated with Magnetically Controlled Growing Rods—A 4-Year Comparison of Two Different Fixation Methods. Journal of Clinical Medicine. 2024; 13(13):3845. https://doi.org/10.3390/jcm13133845
Chicago/Turabian StyleHeuer, Annika, Sebastian Stuecker, Ralf Stuecker, and Kiril Mladenov. 2024. "Pelvic Fixation for Non-Ambulatory Patients with Neuromuscular Scoliosis Treated with Magnetically Controlled Growing Rods—A 4-Year Comparison of Two Different Fixation Methods" Journal of Clinical Medicine 13, no. 13: 3845. https://doi.org/10.3390/jcm13133845
APA StyleHeuer, A., Stuecker, S., Stuecker, R., & Mladenov, K. (2024). Pelvic Fixation for Non-Ambulatory Patients with Neuromuscular Scoliosis Treated with Magnetically Controlled Growing Rods—A 4-Year Comparison of Two Different Fixation Methods. Journal of Clinical Medicine, 13(13), 3845. https://doi.org/10.3390/jcm13133845






