Early Postoperative Weight-Bearing Ability after Total Hip Arthroplasty versus Bipolar Hemiarthroplasty in Elderly Patients with Femoral Neck Fracture
Abstract
1. Introduction
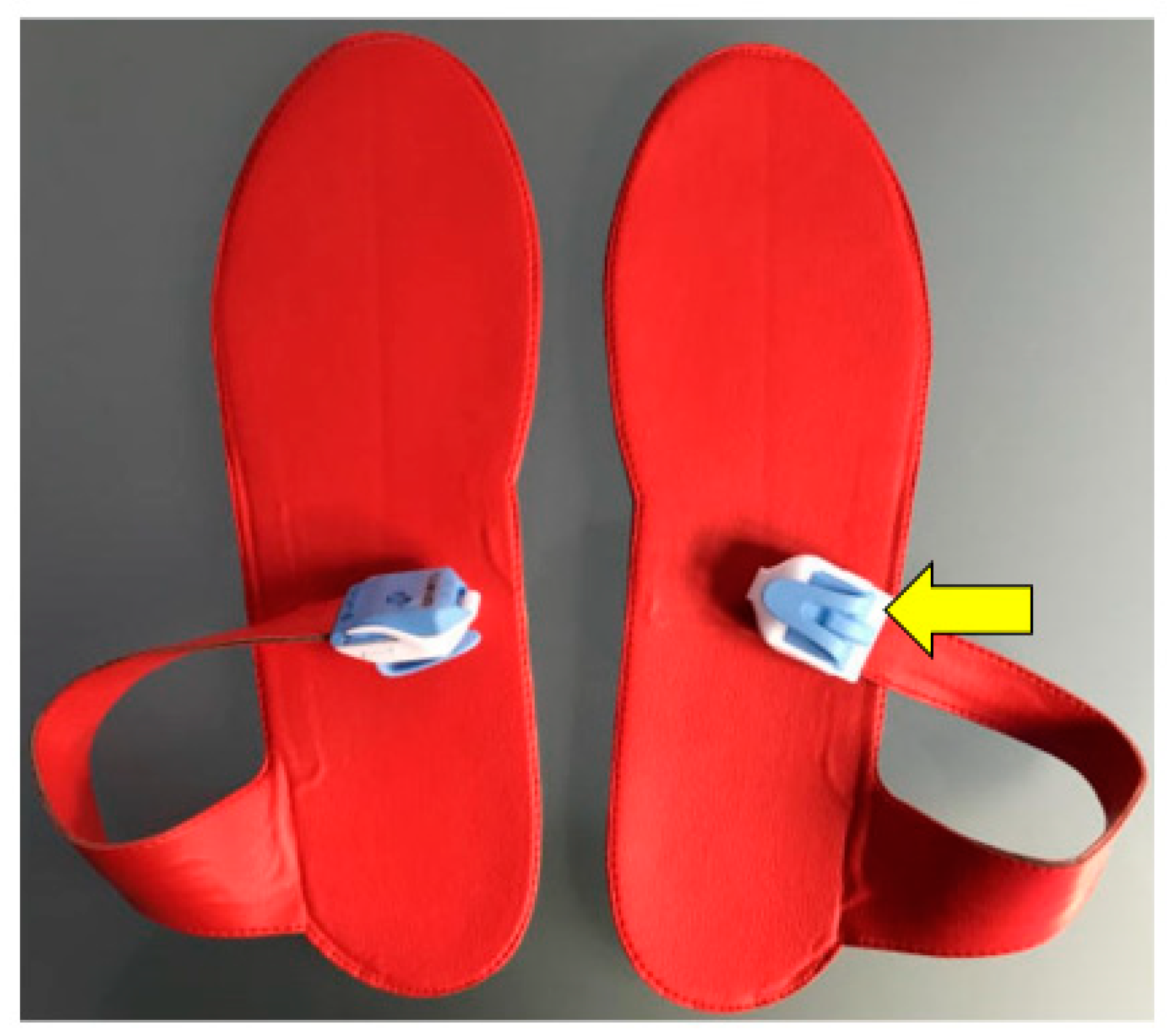
2. Materials and Methods
Statistical Analysis
3. Results
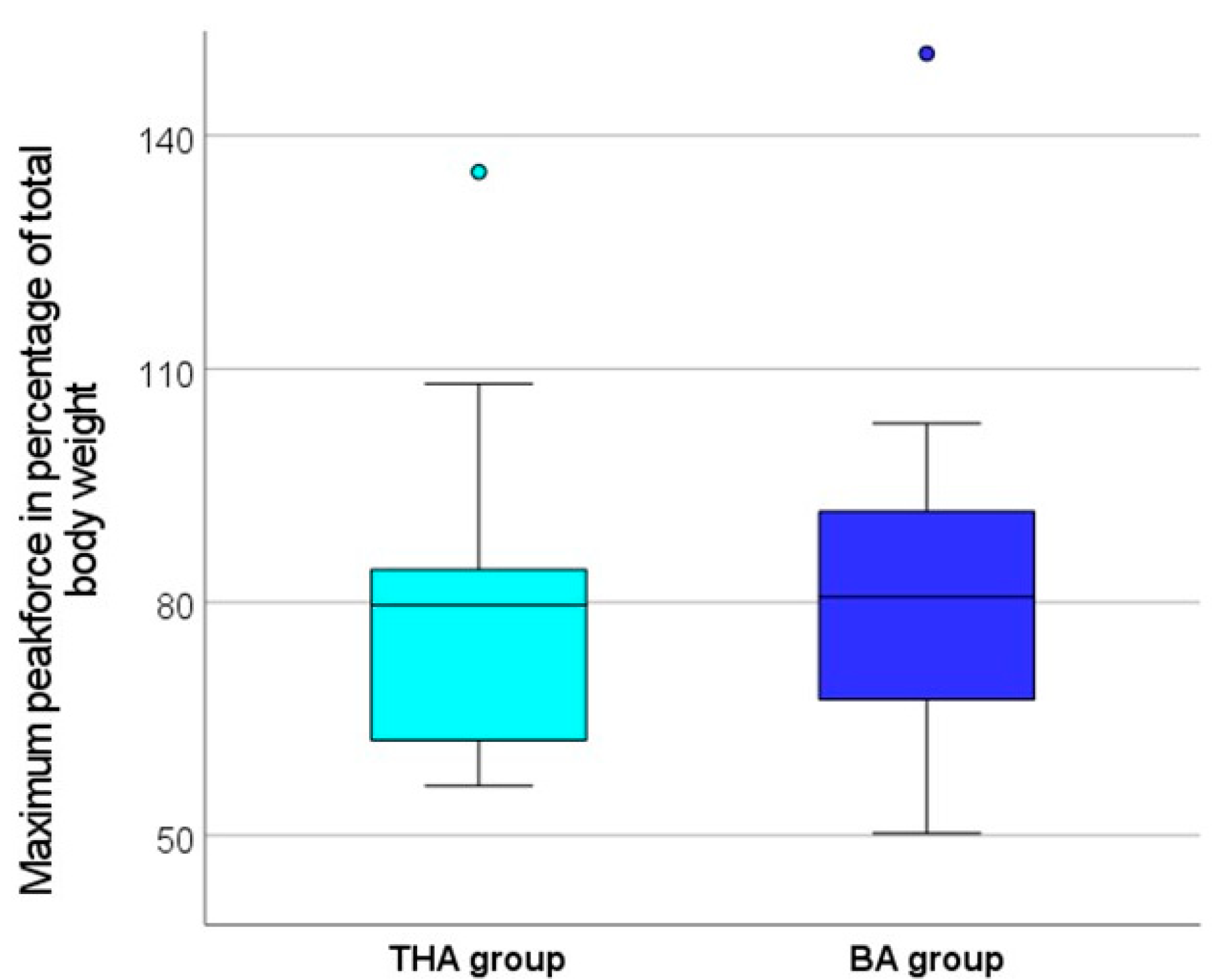
3.1. Postoperative Weight Bearing
3.2. Mobility and Comorbidity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Johnell, O.; Kanis, E.J. Epidemiology of osteoporotic fractures. J. Clin. Orthop. Trauma 2005, 16 (Suppl. 2), S3–S7. [Google Scholar] [CrossRef] [PubMed]
- Lorentzon, M.; Johansson, H.; Harvey, N.C.; Liu, E.; Vandenput, L.; McCloskey, E.V.; Kanis, J.A. Osteoporosis and fractures in women: The burden of disease. Climacteric 2022, 25, 4–10. [Google Scholar] [CrossRef] [PubMed]
- Weyler, E.J.; Gandjour, A. Socioeconomic Burden of Hip Fractures in Germany. Gesundheitswesen 2007, 69, 601–606. [Google Scholar] [CrossRef] [PubMed]
- Greenspan, S.L.; Myers, E.R.; Maitland, L.A.; Resnick, N.M.; Hayes, W.C. Fall Severity and Bone Mineral Density as Risk Factors for Hip Fracture in Ambulatory Elderly. J. Am. Med. Assoc. 1994, 271, 128–133. [Google Scholar] [CrossRef]
- Broos, P.L.; Vecruyssee, R.; Fourneau, I.; Driesen, R.; Stappaerts, K.H. Unstable femoral neck fractures in young adults: Treatment with the AO 130-degree blade plate. J. Orthop. Trauma 1998, 12, 235–239. [Google Scholar] [CrossRef] [PubMed]
- Zetterberg, C.H.; Irstam, L.; Andersson, B.J. Femoral Neck Fractures in Young Adults. Acta Orthop. 1982, 53, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Bales, C.W.; Ritchie, C.S. Sarcopenia, weight loss, and nutritional frailty in the elderly. Annu. Rev. Nutr. 2002, 22, 309–323. [Google Scholar] [CrossRef] [PubMed]
- Karagas, M.R.; Lu-yao, G.L.; Barrett, J.A.; Beach, M.L.; Baron, J.A. Heterogeneity of Hip Fracture: Age, Rac, Sex, and Geographic Patterns of Femoral Neck and Trochanteric Fractures among the US Elderly. Am. J. Epidemiol. 1996, 143, 677–682. [Google Scholar] [CrossRef] [PubMed]
- Girard, J.; Glorion, C. Risk Factors for Revision of Hip Arthroplasties in Patients Younger Than 30 Years. Clin. Orthop. Relat. Res. 2011, 469, 1141–1147. [Google Scholar] [CrossRef]
- Sierra, T.P.; Martín, I.B.; Solís, J.R.; Goitiandia, L.B. Predictive factors of hospital stay, mortality and functional recovery after surgery for hip fracture in elderly patients. Rev. Esp. Cir. Ortop. Traumatol. 2017, 61, 427–435. [Google Scholar] [CrossRef]
- Yoo, J.; Ha, Y.; Lim, J.; Kang, H.; Yoon, B.; Kim, H. Early Rehabilitation in Elderly after Arthroplasty versus Internal Fixation for Unstable Intertrochanteric Fractures of Femur: A Systematic Review and Meta-Analysis. J. Korean Med. Sci. 2017, 32, 858–867. [Google Scholar] [CrossRef] [PubMed]
- Rapp, K.; Rothenbacher, D.; Magaziner, J.; Becker, C.; Benzinger, P.; König, H.-H.; Jaensch, A.; Büchele, G. Risk of Nursing Home Admission after Femoral Fracture Compared with Stroke, Myocardial Infarction, and Pneumonia. J. Am. Med. Dir Assoc. 2015, 16, e7–e715. [Google Scholar] [CrossRef]
- Ariza-vega, P.; Kristensen, T.; Jime, J.; Martı, L. Predictors of Long-Term Mortality in Older People With Hip Fracture. Arch. Phys. Med. Rehabil. 2015, 96, 1215–1221. [Google Scholar] [CrossRef] [PubMed]
- Friedman, S.M.; Mendelson, D.A. Epidemiology of Fragility Fractures. Clin. Geriatr. Med. 2014, 30, 175–181. [Google Scholar] [CrossRef]
- Baer, M.; Neuhaus, V.; Pape, H.C.; Ciritsis, B. Influence of mobilization and weight bearing on in-hospital outcome in geriatric patients with hip fractures. SICOT-J. 2019, 5, 4. [Google Scholar] [CrossRef]
- Pfeufer, D.; Grabmann, C.; Mehaffey, S.; Keppler, A.; Böcker, W.; Kammerlander, C.; Neuerburg, C. Weight bearing in patients with femoral neck fractures compared to pertrochanteric fractures: A postoperative gait analysis. Injury 2019, 50, 1324–1328. [Google Scholar] [CrossRef]
- Blomfeldt, R.; Törnkvist, H.; Ericksson, K.; Söderqvist, A.; Ponzer, S.; Tidermark, J. A randomised controlled trial comparing bipolar hemiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in elderly patients. J. Bone Jt. Surg. Ser. B 2007, 89, 160–165. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, M.; Devereaux, P.; TornettaIII, P.; Swiontkowski, M.F.; Berry, D.J.; Haidukewych, G.; Schemitsch, E.H.; Hanson, B.P.; Koval, K.; Dirschl, D.; et al. Operative Management of displaced femoral neck fractures in elderly patients: An international survey. J. Bone Jt. Surg. Am. 2005, 87, 2122–2131. [Google Scholar] [CrossRef] [PubMed]
- Masson, M.; Parker, M.J.; Schoelzl, S. Internal fixation versus arthroplasty for intracapsular proximal femoral fractures in adults. Cochrane Database Syst. Rev. 2003, CD001708. [Google Scholar] [CrossRef]
- Schleicher, I.; Kordelle, J.; Jürgensen, I.; Haas, H.; Melzer, C. Die schenkelhalsfraktur beim alten menschen—Bipolare hemiendoprothese vs. total-endoprothese. Unfallchirurg 2003, 106, 467–471. [Google Scholar] [CrossRef]
- Sharma, V.; Awasthi, B.; Kumar, K.; Kohli, N.; Katoch, P. Outcome analysis of hemiarthroplasty vs. Total hip replacement in displaced femoral neck fractures in the elderly. J. Clin. Diagn. Res. 2016, 10, RC11–RC13. [Google Scholar] [CrossRef] [PubMed]
- Avery, P.P.; Baker, R.P.; Walton, M.J.; Rooker, J.C.; Squires, B.; Gargan, M.F.; Bannister, G.C. Total hip replacement and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck: A seven- to ten-year follow-up report of a prospective randomised controlled trial. J. Bone Jt. Surg. Ser. B 2011, 93B, 1045–1048. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.P.; Squires, B.; Gargan, M.F.; Bannister, G.C. Total Hip Arthroplasty and Hemiarthroplasty in Mobile, Independent Patients with a Displaced Intracapsular Fracture of the Femoral Neck. J. Bone Jt. Surg. Am. 2006, 88, 2583–2589. [Google Scholar] [CrossRef] [PubMed]
- Squires, B.; Bannister, G. Displaced intracapsular neck of femur fractures in mobile independent patients: Total hip replacement or hemiarthroplasty? Injury 1999, 30, 345–348. [Google Scholar] [CrossRef] [PubMed]
- Apivatthakakul, T.; Oh, J.-K. AO Surgery Reference, Proximal Femur. 2022. Available online: https://surgeryreference.aofoundation.org/orthopedic-trauma/adult-trauma/proximal-femur (accessed on 4 July 2022).
- Tombaugh, T.N.; Mclntyre, N.J. The Mini-Mental State Examination. J. Am. Geriatr. Soc. 1992, 40, 922–935. [Google Scholar] [CrossRef] [PubMed]
- D’Hoore, W.; Sicotte, C.; Tilquin, C. Risk adjustment in outcome assessment: The Charlson comorbidity index. Methods Inf. Med. 1993, 32, 382–387. [Google Scholar] [CrossRef]
- Lübke, N.; Meinck, M.; Von Renteln-Kruse, W. Der Barthel-Index in der geriatrie. Eine kontextanalyse zum Hamburger Einstufungsmanual. Z. Gerontol. Geriatr. 2004, 37, 316–326. [Google Scholar] [CrossRef]
- Parker, M.J.; Palmer, C.R. A new mobility score for predicting mortality after hip fracture. J. Bone Jt. Surg. Ser. B 1993, 75, 797–798. [Google Scholar] [CrossRef]
- Anekar, A.A.; Cascella, M. WHO analgesic ladder. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- Samson, M.M.; Crowe, A.; de Vreede, P.L.; Dessens, J.A.G.; Duursma, S.A.; Verhaar, H.J.J. Differences in gait parameters at a preferred walking speed in healthy subjects due to age, height and body weight. Aging Clin. Exp. Res. 2001, 13, 16–21. [Google Scholar] [CrossRef] [PubMed]
- Mak, J.C.S.; Cameron, I.D.; March, L.M. Evidence-based guidelines for the management of hip fractures in older persons: An update. Med. J. Aust. 2010, 192, 37–41. [Google Scholar] [CrossRef]
- Ftouh, S.; Morga, A.; Swift, C. Management of hip fracture in adults: Summary of NICE guidance. BMJ 2011, 342, d3304. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, R. Australian and New Zealand Hip Fracture Hospitalisation Trends: 2000–2001 to 2011–2012: Informing the Development of the Australian and New Zealand Hip Fracture Registry; Australian & New Zealand Hip Fracture Registry: Sydney, Australia, 2014. [Google Scholar]
- Bonnaire, F.; Weber, A. Schenkelhalsfraktur des Erwachsenen. Leitlinien Unfallchirurgie 2015. Available online: https://www.awmf.org/uploads/tx_szleitlinien/012-001l_S2e_Schenkelhalsfraktur_2015-10-abgelaufen_02.pdf (accessed on 4 July 2022).
- Tidermark, J. Quality of life and femoral neck fractures. Acta Orthop. 2003, 74, 1–42. [Google Scholar] [CrossRef]
- Calder, S.J.; Anderson, G.H.; Jagger, C.; Harper, W.M.; Gregg, P.J. Unipolar or bipolar prosthesis for displaced intracapsular hip fracture in octogenarians: A randomised prospective study. J. Bone Jt. Surg. Ser. B 1996, 78, 391–394. [Google Scholar] [CrossRef]
- Leon, D.A. Trends in European life expectancy: A salutary view. Int. J. Epidemiol. 2011, 40, 271–277. [Google Scholar] [CrossRef] [PubMed]
- Oldmeadow, L.B.; Edwards, E.R.; Kimmel, L.A.; Kipen, E.; Robertson, V.J.; Bailey, M.J. No rest for the wounded: Early ambulation after hip surgery accelerates recovery. ANZ J. Surg. 2006, 76, 607–611. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, M.T.; Bandholm, T.; Bencke, J.; Ekdahl, C.; Kehlet, H. Knee-extension strength, postural control and function are related to fracture type and thigh edema in patients with hip fracture. Clin. Biomech. 2009, 24, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Sherrington, C.; Lord, S.R.; Herbert, R.D. A randomised trial of weight-bearing versus non-weight-bearing exercise for improving physical ability in inpatients after hip fracture. Aust. J. Physiother. 2003, 49, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Kronborg, L.; Bandholm, T.; Palm, H.; Kehlet, H.; Kristensen, M.T. Feasibility of progressive strength training implemented in the acute ward after hip fracture surgery. PLoS ONE 2014, 9, e0093332. [Google Scholar] [CrossRef] [PubMed]
- Lamb, S.E.; Morse, R.E.; Evans, J.G. Mobility after proximal femoral fracture: The relevance of leg extensor power, postural sway and other factors. Age Ageing 1995, 24, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Jagos, H.; Pils, K.; Haller, M.; Wassermann, C.; Chhatwal, C.; Rafolt, D.; Rattay, F. Mobile gait analysis via eSHOEs instrumented shoe insoles: A pilot study for validation against the gold standard GAITRite®. J. Med. Eng. Technol. 2017, 41, 375–386. [Google Scholar] [CrossRef]
- Marin, L.; Vandoni, M.; Zaza, G.; Febbi, M.; Pedrotti, L.; Chiodaroli, M.; Lovecchio, N.; Manzoni, F. The effects of insole-based visual feedback on weight-bearing in patients undergoing total hip replacement. Int. J. Environ. Res. Public Health 2021, 18, 3346. [Google Scholar] [CrossRef] [PubMed]




| THA | BA | |
|---|---|---|
| Number in total | 14 | 25 |
| Age, mean ± SD | 74.0 ± 7.9 years | 82.5 ± 6.9 years |
| Sex | ||
| Male | 6 (43%) | 14 (56%) |
| Female | 8 (57%) | 11 (44%) |
| ASA, mean ± SD | 2.6 ± 0.6 | 2.9 ± 0.5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grabmann, C.; Hussain, I.; Zeller, A.; Kirnaz, S.; Sullivan, V.; Sommer, F. Early Postoperative Weight-Bearing Ability after Total Hip Arthroplasty versus Bipolar Hemiarthroplasty in Elderly Patients with Femoral Neck Fracture. J. Clin. Med. 2024, 13, 3128. https://doi.org/10.3390/jcm13113128
Grabmann C, Hussain I, Zeller A, Kirnaz S, Sullivan V, Sommer F. Early Postoperative Weight-Bearing Ability after Total Hip Arthroplasty versus Bipolar Hemiarthroplasty in Elderly Patients with Femoral Neck Fracture. Journal of Clinical Medicine. 2024; 13(11):3128. https://doi.org/10.3390/jcm13113128
Chicago/Turabian StyleGrabmann, Chiara, Ibrahim Hussain, Anne Zeller, Sertac Kirnaz, Vincent Sullivan, and Fabian Sommer. 2024. "Early Postoperative Weight-Bearing Ability after Total Hip Arthroplasty versus Bipolar Hemiarthroplasty in Elderly Patients with Femoral Neck Fracture" Journal of Clinical Medicine 13, no. 11: 3128. https://doi.org/10.3390/jcm13113128
APA StyleGrabmann, C., Hussain, I., Zeller, A., Kirnaz, S., Sullivan, V., & Sommer, F. (2024). Early Postoperative Weight-Bearing Ability after Total Hip Arthroplasty versus Bipolar Hemiarthroplasty in Elderly Patients with Femoral Neck Fracture. Journal of Clinical Medicine, 13(11), 3128. https://doi.org/10.3390/jcm13113128





