Potential of Titanium Pins Coated with Fibroblast Growth Factor-2–Calcium Phosphate Composite Layers to Reduce the Risk of Impaired Bone–Pin Interface Strength in the External Fixation of Distal Radius Fractures
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Study Design
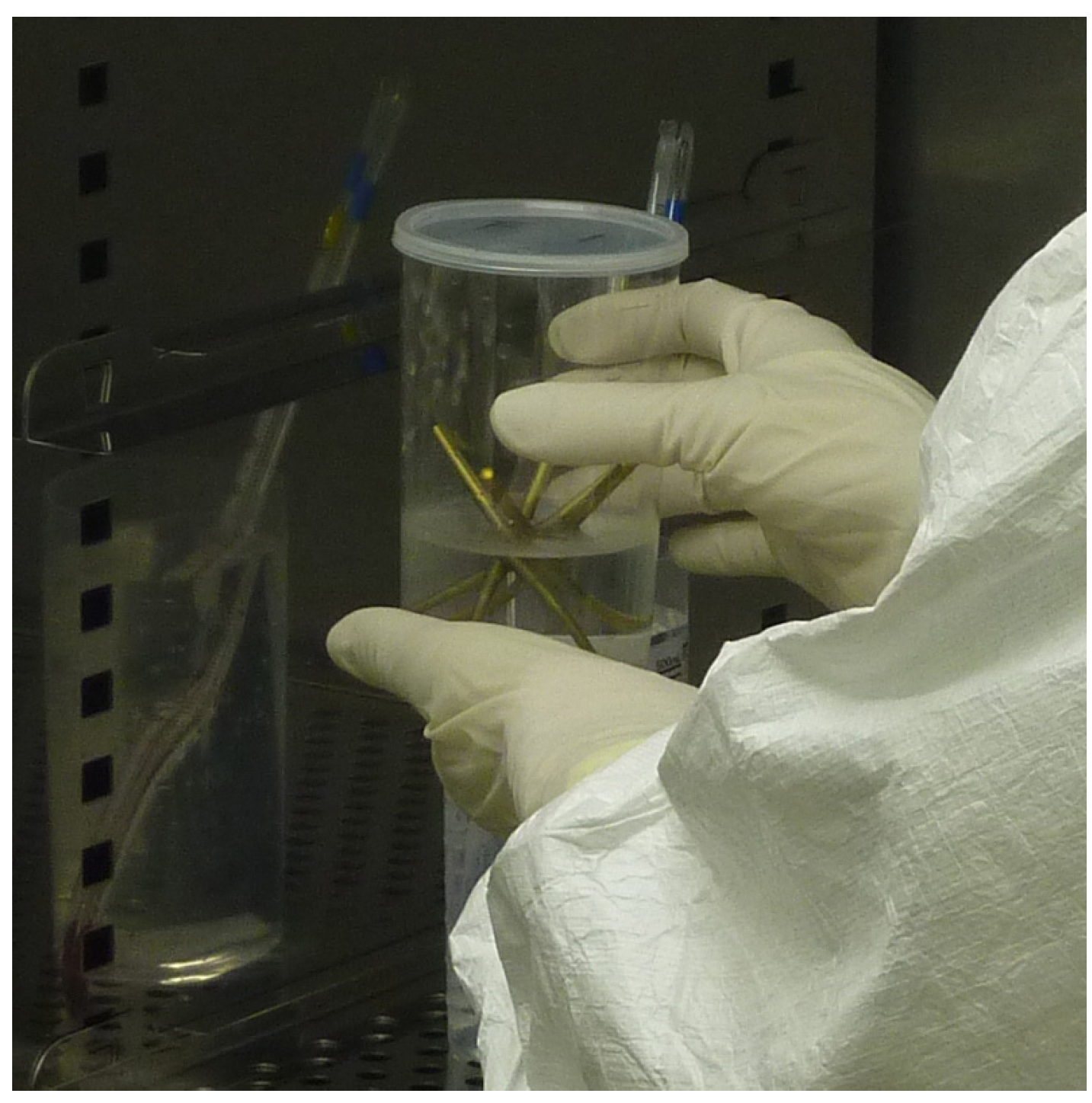
2.3. FGF-CP Coating Technique
2.4. Operation and Measurement Procedures
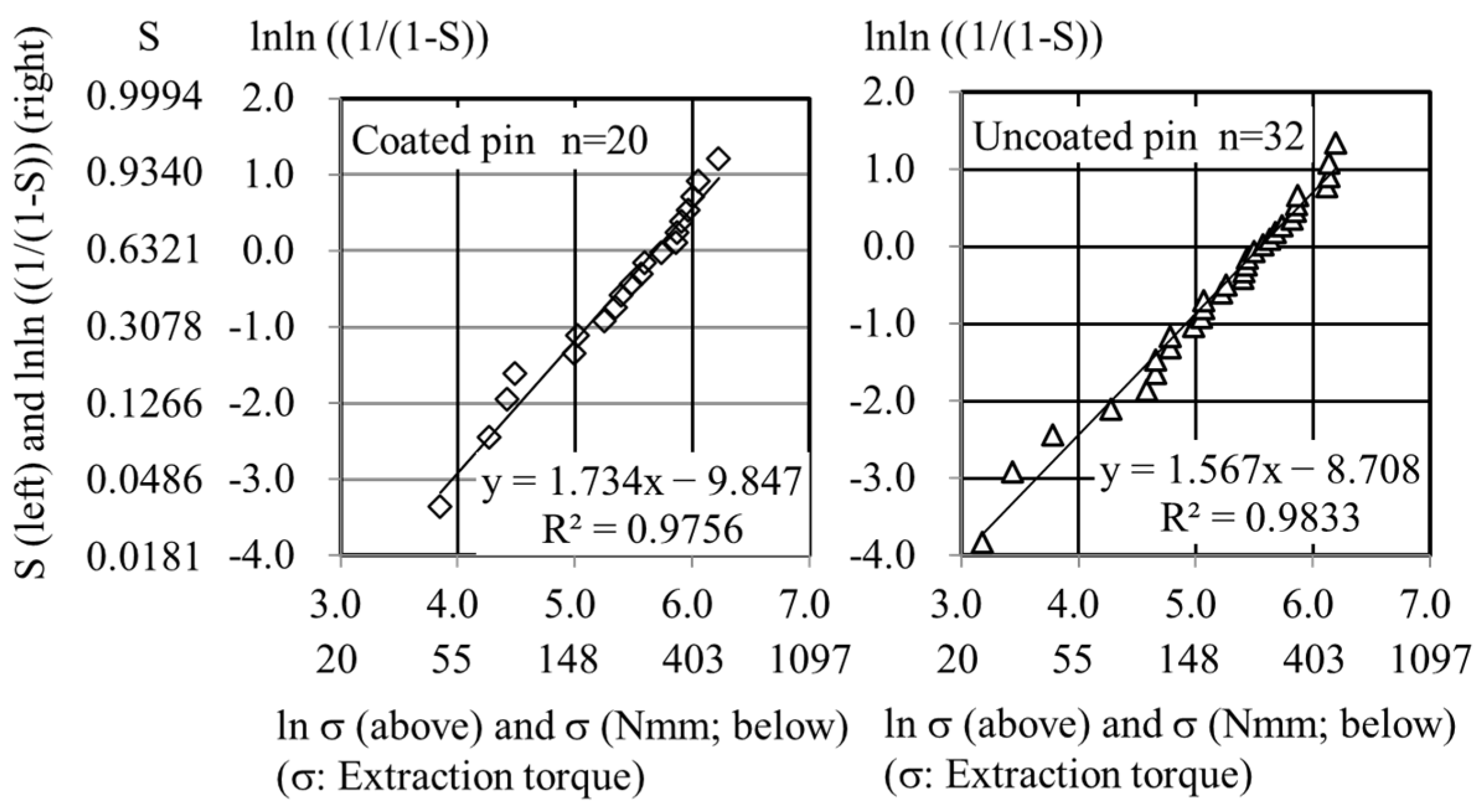
2.5. Weibull Plot Analysis
2.6. Statistical Analysis
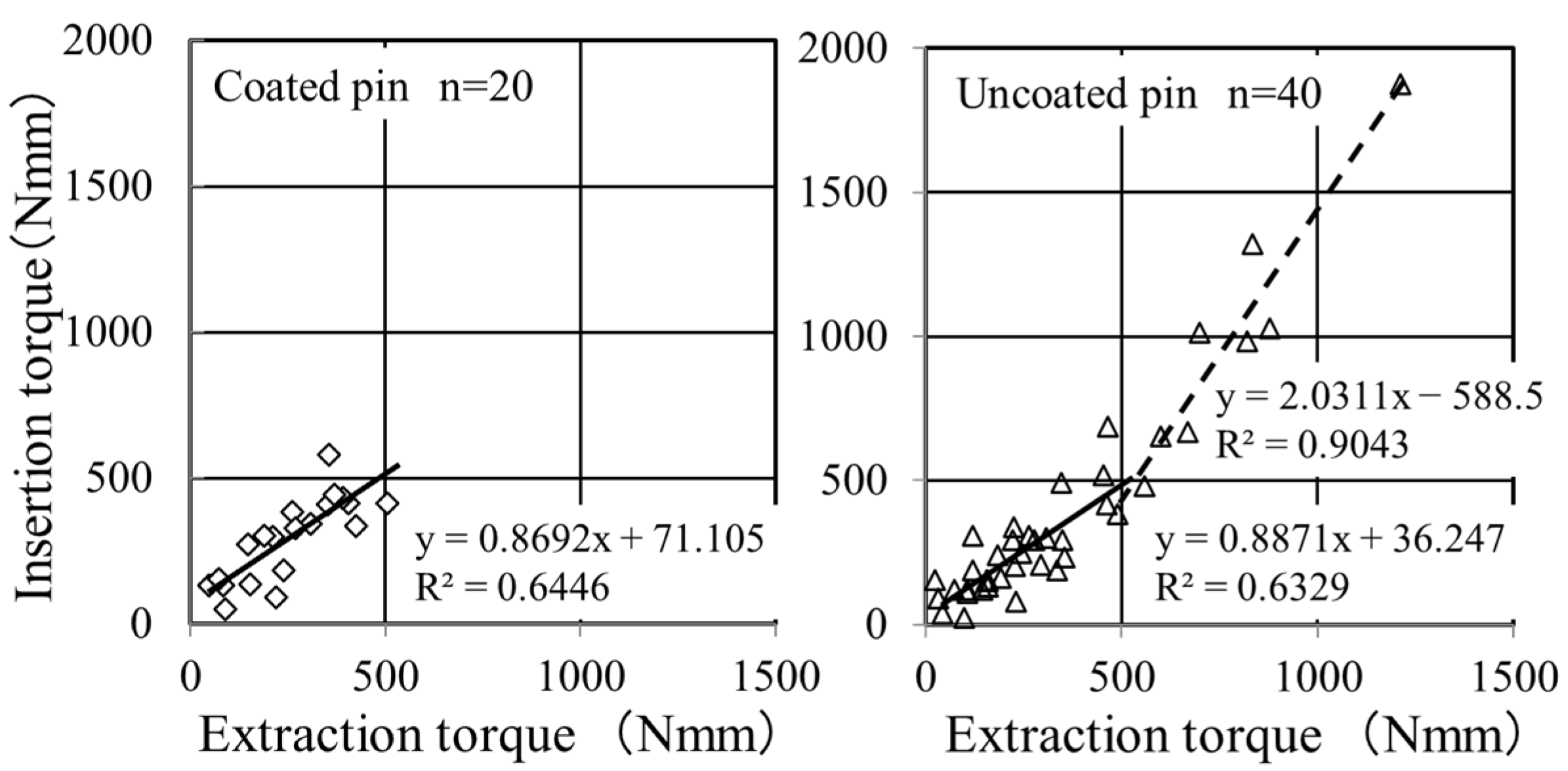
3. Results
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Galbusera, F.; Volkheimer, D.; Reitmaier, S.; Berger-Roscher, N.; Kienle, A.; Wilke, H.J. Pedicle screw loosening: A clinically relevant complication? Eur. Spine J. 2015, 24, 1005–1016. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.C.; Huang, W.C.; Tsai, H.W.; Ko, C.C.; Wu, C.L.; Tu, T.H.; Cheng, H. Pedicle screw loosening in dynamic stabilization: Incidence, risk, and outcome in 126 patients. Neurosurg. Focus 2011, 31, E9. [Google Scholar] [CrossRef] [PubMed]
- Kocak, T.; Cakir, B.; Reichel, H.; Mattes, T. Screw loosening after posterior dynamic stabilization–review of the literature. Acta Chir. Orthop. Traumatol. Cech. 2010, 77, 134–139. [Google Scholar] [CrossRef] [PubMed]
- Moroni, A.; Cadossi, M.; Romagnoli, M.; Faldini, C.; Giannini, S. A biomechanical and histological analysis of standard versus hydroxyApatite-coated pins for external fixation. J. Biomed. Mater. Res. B Appl. Biomater. 2008, 86, 417–421. [Google Scholar] [CrossRef] [PubMed]
- Moroni, A.; Pegreffi, F.; Cadossi, M.; Hoang-Kim, A.; Lio, V.; Giannini, S. Hydroxyapatite-coated external fixation pins. Expert Rev. Med. Devices. 2005, 2, 465–471. [Google Scholar] [CrossRef]
- Gathen, M.; Ploeger, M.M.; Jaenisch, M.; Koob, S.; Cucchi, D.; Kasapovic, A.; Randau, T.; Placzek, R. Outcome evaluation of new calcium titanate schanz-screws for external fixators. First clinical results and cadaver studies. J. Mater. Sci. Mater. Med. 2019, 30, 124. [Google Scholar] [CrossRef] [PubMed]
- Toksvig-Larsen, S.; Aspenberg, P. Bisphosphonate-coated external fixation pins appear similar to hydroxyapatite-coated pins in the tibial metaphysis and to uncoated pins in the shaft. Acta Orthop. 2013, 84, 314–318. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, Y.; Mutsuzaki, H.; Hara, Y.; Nagashima, K.; Okano, E.; Yanagisawa, Y.; Noguchi, H.; Sankai, T.; Yamazaki, M. Safety and osteointegration of titanium screws coated with a fibroblast growth factor-2-calcium phosphate composite layer in non-human primates: A pilot study. J. Funct. Biomater. 2023, 14, 261. [Google Scholar] [CrossRef] [PubMed]
- Weibull, W. A statistical distribution function of wide applicability. J. Appl. Mech. 1951, 18, 293–297. [Google Scholar] [CrossRef]
- Yanagisawa, Y.; Ito, A.; Hara, Y.; Mutsuzaki, H.; Murai, S.; Fujii, K.; Sogo, Y.; Hirose, M.; Oyane, A.; Kobayashi, F.; et al. Initial clinical trial of pins coated with fibroblast growth factor-2-apatite composite layer in external fixation of distal radius fractures. J. Orthop. 2019, 16, 69–73. [Google Scholar] [CrossRef] [PubMed]
- Pieske, O.; Kaltenhauser, F.; Pichlmaier, L.; Schramm, N.; Trentzsch, H.; Löffler, T.; Greiner, A.; Piltz, S. Clinical benefit of hydroxyapatite-coated pins compared with stainless steel pins in external fixation at the wrist: A randomised prospective study. Injury 2010, 41, 1031–1036. [Google Scholar] [CrossRef] [PubMed]
- Pieske, O.; Pichlmaier, L.; Kaltenhauser, F.; Schramm, N.; Rubenbauer, B.; Greiner, A.; Piltz, S. Hydroxyapatite-coated pins versus titanium alloy pins in external fixation at the wrist: A controlled cohort study. J. Trauma. 2011, 70, 845–851. [Google Scholar] [CrossRef]
- Saithna, A. The influence of hydroxyapatite coating of external fixator pins on pin loosening and pin track infection: A systematic review. Injury 2010, 41, 128–132. [Google Scholar] [CrossRef] [PubMed]
- Moroni, A.; Aspenberg, P.; Toksvig-Larsen, S.; Falzarano, G.; Giannini, S. Enhanced fixation with hydroxyapatite coated pins. Clin. Orthop. Relat. Res. 1998, 346, 171–177. [Google Scholar]
- Moroni, A.; Faldini, C.; Marchetti, S.; Manca, M.; Consoli, V.; Giannini, S. Improvement of the bone-pin interface strength in osteoporotic bone with use of hydroxyapatite-coated tapered external-fixation pins. A prospective, randomized clinical study of wrist fracture. J. Bone Joint Surg. Am. 2001, 83, 717–721. [Google Scholar] [CrossRef]
- Pizà, G.; Caja, V.L.; González-Viejo, M.A.; Navarro, A. Hydroxyapatite-coated external-fixation pins. The effect on pin loosening and pin-track infection in leg lengthening for short stature. J. Bone Joint Surg. Br. 2004, 86, 892–897. [Google Scholar] [CrossRef] [PubMed]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mutsuzaki, H.; Yanagisawa, Y.; Noguchi, H.; Ito, A.; Yamazaki, M. Potential of Titanium Pins Coated with Fibroblast Growth Factor-2–Calcium Phosphate Composite Layers to Reduce the Risk of Impaired Bone–Pin Interface Strength in the External Fixation of Distal Radius Fractures. J. Clin. Med. 2024, 13, 3040. https://doi.org/10.3390/jcm13113040
Mutsuzaki H, Yanagisawa Y, Noguchi H, Ito A, Yamazaki M. Potential of Titanium Pins Coated with Fibroblast Growth Factor-2–Calcium Phosphate Composite Layers to Reduce the Risk of Impaired Bone–Pin Interface Strength in the External Fixation of Distal Radius Fractures. Journal of Clinical Medicine. 2024; 13(11):3040. https://doi.org/10.3390/jcm13113040
Chicago/Turabian StyleMutsuzaki, Hirotaka, Yohei Yanagisawa, Hiroshi Noguchi, Atsuo Ito, and Masashi Yamazaki. 2024. "Potential of Titanium Pins Coated with Fibroblast Growth Factor-2–Calcium Phosphate Composite Layers to Reduce the Risk of Impaired Bone–Pin Interface Strength in the External Fixation of Distal Radius Fractures" Journal of Clinical Medicine 13, no. 11: 3040. https://doi.org/10.3390/jcm13113040
APA StyleMutsuzaki, H., Yanagisawa, Y., Noguchi, H., Ito, A., & Yamazaki, M. (2024). Potential of Titanium Pins Coated with Fibroblast Growth Factor-2–Calcium Phosphate Composite Layers to Reduce the Risk of Impaired Bone–Pin Interface Strength in the External Fixation of Distal Radius Fractures. Journal of Clinical Medicine, 13(11), 3040. https://doi.org/10.3390/jcm13113040





