Can We Improve the Technique of Pelvic Floor Muscle Exercises in Postmenopausal Women Using a Single Electromyography Biofeedback Session? An Experimental Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Assessment of Neuromuscular Activity in Pelvic Floor Muscles and Implementation of a Biofeedback Session
2.3. Assessment of Pelvic Floor Muscle Exercise Techniques
2.4. Assessment of the Impact of Urinary Incontinence on Quality of Life
2.5. Description of Statistics
3. Results
4. Discussion
5. Conclusions
6. Perspective
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bo, K.; Frawley, H.C.; Haylen, B.T.; Abramov, Y.; Almeida, F.G.; Berghmans, B.; Bortolini, M.; Dumoulin, C.; Gomes, M.; McClurg, D.; et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for the conservative and nonpharmacological management of female pelvic floor dysfunction. Int. Urogynecol. J. 2017, 28, 191–213. [Google Scholar] [CrossRef]
- Sam, P.; LaGrange, C. Anatomy, Abdomen and Pelvis, Penis. 2022. Available online: https://www.ncbi.nlm.nih.gov/books/NBK482236/ (accessed on 20 November 2023).
- Forman, M.R.; Mangini, L.D.; Thelus-Jean, R.; Hayward, M.D. Life-course origins of the ages at menarche and menopause. Adolesc. Health Med. Ther. 2013, 4, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Ayten, D.; Urinary Incontinence, M. Recent Studies in Health Sciences 2019 C. Menopause and Urinary Incontinence. In Recent Studies in Health Sciences; Chernopolski, P., Shapekova, N., Sancar, B., Ak, B., Eds.; St. Kliment Ohridski University Press: Sofia, Bulgaria, 2019; pp. 341–351. [Google Scholar]
- El Khoudary, S.R.; Greendale, G.; Crawford, S.L.; Avis, N.E.; Brooks, M.M.; Thurston, R.C.; Karvonen-Gutierrez, C.; Waetjen, L.E.; Matthews, K. The menopause transition and women’s health at midlife: A progress report from the Study of Women’s Health Across the Nation (SWAN). N. Am. Menopause Soc. 2019, 26, 1213–1227. [Google Scholar] [CrossRef]
- Prajapati, M.M. Awareness regarding menopausal symptoms and effect on daily life among postmenopausal women. J. Patan Acad. Health Sci. 2020, 7, 130–136. [Google Scholar] [CrossRef]
- Van der Woude, D.A.A.; Pijnenborg, J.M.A.; de Vries, J. Health status and quality of life in postpartum women: A systematic review of associated factors. Eur. J. Obstet. Gynecol. Reprod. Biol. 2015, 185, 45–52. [Google Scholar] [CrossRef]
- Leong, B.S.; Mok, N.W. Effectiveness of a new standardised Urinary Continence Physiotherapy Programme for community-dwelling older women in Hong Kong. Hong Kong Med. J. 2015, 21, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Opławski, M.; Smoczyńska, M.; Grabarek, B.O.; Boron, D. Assessment of Dysfunction in the Urinary System as Well as Comfort in the Life of Women during and after Combination Therapy Due to Ovarian and Endometrial Cancer Based on the SWL, II-Q7 and UDI-6 Scales. J. Clin. Med. 2021, 10, 1228. [Google Scholar] [CrossRef] [PubMed]
- Castro, R.A.; Arruda, R.M.; Zanetti, M.R.D.; Santos, P.D.; Sartori, M.G.F.; Girao, M. Single-blind, randomized, controlled trial of pelvic floor muscle training, electrical stimulation, vaginal cones, and no active treatment in the management of stress urinary incontinence. Clinics 2008, 63, 465–472. [Google Scholar] [CrossRef]
- Dumoulin, C.; Adewuyi, T.; Booth, J.; Bradley, C.; Burgio, K.; Hagen, S.; Williams, K. Adult conservative management. In Incontinence: 6th International Consultation on Incontinence. Tokyo, 6th ed.; Abrams, P., Cardozo, L., Wagg, A., Wein, A., Eds.; International Continence Society (ICS) and International Consultation on Urological Diseases (ICUD): Bristol, UK, 2017; pp. 1443–1628. [Google Scholar]
- Cho, S.T.; Kim, K.H. Pelvic floor muscle exercise and training for coping with urinary incontinence. J. Exerc. Rehabil. 2021, 17, 379–387. [Google Scholar] [CrossRef]
- Piernicka, M.; Bludnicka, M.; Kortas, J.; Duda-Biernacka, B.; Szumilewicz, A. High-impact aerobics programme supplemented by pelvic floor muscle training does not impair the function of pelvic floor muscles in active nulliparous women A randomized control trial. Medicine 2021, 100, e26989. [Google Scholar] [CrossRef]
- Yang, S.J.; Liu, Y.T.; Lo, S.S.; Tsai, C.C.; Pan, P.J. Effect of a Comprehensive Rehabilitation Program for Community Women with Urinary Incontinence: A Retrospect Cohort Study. Healthcare. 2021, 9, 1686. [Google Scholar] [CrossRef] [PubMed]
- Cacciari, L.P.; Dumoulin, C.; Hay-Smith, E.J. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women: A cochrane systematic review abridged republication. Braz. J. Phys. Ther. 2019, 23, 93–107. [Google Scholar] [CrossRef] [PubMed]
- Alouini, S.; Memic, S.; Couillandre, A. Pelvic Floor Muscle Training for Urinary Incontinence with or without Biofeedback or Electrostimulation in Women: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 2789. [Google Scholar] [CrossRef] [PubMed]
- Zhuo, Z.H.; Wang, C.H.; Yu, H.M.; Li, J. The Relationship Between Pelvic Floor Function and Sexual Function in Perimenopausal Women. Sex. Med. 2021, 9, 100441. [Google Scholar] [CrossRef] [PubMed]
- Vodusek, D.B. Electromyography. In Evidence-Based Physical Therapy for the Pelvic Floor: Bridging Science and Clinical Practice; Bo, K., Berghmans, B., Morkved, S., Van Kampen, M., Eds.; Churchill Livingstone: Edinburgh, UK, 2015. [Google Scholar]
- O’Toole, J. Pelvic floor exercises for women tips and tricks. Aust. Nurs. Midwifery J. 2016, 24, 44. [Google Scholar]
- Vermandel, A.; De Wachter, S.; Beyltjens, T.; D’Hondt, D.; Jacquemyn, Y.; Wyndaele, J.J. Pelvic floor awareness and the positive effect of verbal instructions in 958 women early postdelivery. Int. Urogynecol. J. 2015, 26, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Giggins, O.M.; Persson, U.M.; Caulfield, B. Biofeedback in rehabilitation. J. Neuroeng. Rehabil. 2013, 10, 60. [Google Scholar] [CrossRef] [PubMed]
- Błudnicka, M.; Piernicka, M.; Szumilewicz, A. The characteristics of biofeedback techniques used in pelvic floor muscle training for healthy pregnant women. A narrative review. Balt. J. Health Phys. Act. 2019, 11, 87–95. [Google Scholar] [CrossRef]
- Hagen, S.; Elders, A.; Stratton, S.; Sergenson, N.; Bugge, C.; Dean, S.; Hay-Smith, J.; Kilonzo, M.; Dimitrova, M.; Abdel-Fattah, M.; et al. Effectiveness of pelvic floor muscle training with and without electromyographic biofeedback for urinary incontinence in women: Multicentre randomised controlled trial. BMJ 2020, 371, 3719. [Google Scholar] [CrossRef]
- Błudnicka, M.; Piernicka, M.; Kortas, J.; Biernacka, B.D.; Szumilewicz, A. Effects of a One-Time Biofeedback EMG Session on Neuromuscular Activity of the Pelvic Floor Muscles in Pregnant Women. Neurophysiology 2020, 52, 438–445. [Google Scholar] [CrossRef]
- Błudnicka, M.; Piernicka, M.; Kortas, J.; Bojar, D.; Duda-Biernacka, B.; Szumilewicz, A. The influence of one-time biofeedback electromyography session on the firing order in the pelvic floor muscle contraction in pregnant woman-A randomized controlled trial. Front. Hum. Neurosci. 2022, 16, 944792. [Google Scholar] [CrossRef] [PubMed]
- Halski, T.; Słupska, L.; Dymarek, R.; Bartnicki, J.; Halska, U.; Król, A.; Paprocka-Borowicz, M.; Dembowski, J.; Zdrojowy, R.; Ptaszkowski, K. Evaluation of Bioelectrical Activity of Pelvic Floor Muscles and Synergistic Muscles Depending on Orientation of Pelvis in Menopausal Women with Symptoms of Stress Urinary Incontinence: A Preliminary Observational Study. BioMed Res. Int. 2014, 2014, 274938. [Google Scholar] [CrossRef] [PubMed]
- Glazer, H.I.; Marinoff, S.C.; Sleight, I.J. Web-enabled Glazer surface electromyographic protocol for the remote, real-time assessment and rehabilitation of pelvic floor dysfunction in vulvar vestibulitis syndrome. A case report. J. Reprod. Med. 2002, 47, 728–730. [Google Scholar]
- Woodley, S.J.; Hay-Smith, E.J.C. Narrative review of pelvic floor muscle training for childbearing women-why, when, what, and how. Int. Urogynecol. J. 2021, 32, 1977–1988. [Google Scholar] [CrossRef] [PubMed]
- Hodges, P.W.; Bui, B.H. A comparison of computer-based methods for the determination of onset of muscle contraction using electromyography. Electromyogr. Mot. Control Electroencephalogr. Clin. Neurophysiol. 1996, 101, 511–519. [Google Scholar] [CrossRef] [PubMed]
- Szumilewicz, A.; Hopkins, W.G.; Dornowski, M.; Piernicka, M. Exercise Professionals Improve Their Poor Skills in Contracting Pelvic-Floor Muscles: A Randomized Controlled Trial. Res. Q. Exerc. Sport 2019, 90, 641–650. [Google Scholar] [CrossRef] [PubMed]
- Ghroubi, S.; El Fani, N.; Elarem, S.; Alila, S.; Ben Ayed, H.; Borgi, O.; Chmak, J.; Elleuch, M.H. Arabic (Tunisian) translation and validation of the Urogenital Distress Inventory short form (UDI-6) and Incontinence Impact Questionnaire short form (IIQ-7). Arab. J. Urol. 2020, 18, 27–33. [Google Scholar] [CrossRef]
- Bouallatene-Jaramillo, K.; Bagur-Calafat, M.C.; Girabent-Farres, M. Validation of the Spanish version of the Urogenital Distress Inventory short form and Incontinence Impact Questionnaire short form for women between the ages of 18 and 65. Actas Urol. Esp. 2015, 39, 511–517. [Google Scholar] [CrossRef] [PubMed]
- Vieira, G.F.; Saltiel, F.; Miranda-Gazzola, A.P.G.; Kirkwood, R.N.; Figueiredo, E.M. Pelvic floor muscle function in women with and without urinary incontinence: Are strength and endurance the only relevant functions? a cross-sectional study. Physiotherapy 2020, 109, 85–93. [Google Scholar] [CrossRef]
- Bø, K.; Sherburn, M. Vaginal squeeze pressure measurment. In Evidence-Based Physical Therapy for the Pelvic Floor: Bridging Science and Clinical Practice; Bø, K., Berghmans, B., Mørkved, S., Van Kampen, M., Eds.; Elsevier: London, UK, 2007; pp. 63–68. [Google Scholar]
- Neels, H.; De Wachter, S.; Wyndaele, J.J.; Van Aggelpoel, T.; Vermandel, A. Common errors made in attempt to contract the pelvic floor muscles in women early after delivery: A prospective observational study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018, 220, 113–117. [Google Scholar] [CrossRef]
- Glazer, H.I.; Romanzi, L.; Polaneczky, M. Pelvic floor muscle surface electromyography: Reliability and clinical predictive validity. J. Reprod. Med. 1999, 44, 779–782. [Google Scholar] [PubMed]
- Scharschmidt, R.; Derlien, S.; Siebert, T.; Herbsleb, M.; Stutzig, N. Intraday and interday reliability of pelvic floor muscles electromyography incontinent woman. Neurourol. Urodyn. 2020, 39, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Leitner, M.; Moser, H.; Eichelberger, P.; Kuhn, A.; Radlinger, L. Pelvic floor muscle activity during fast voluntary contractions in continent and incontinent women. Neurourol. Urodyn. 2019, 38, 625–631. [Google Scholar] [CrossRef] [PubMed]
- López-Pérez, M.P.; Afanador-Restrepo, D.F.; Rivas-Campo, Y.; Hita-Contreras, F.; Carcelén-Fraile, M.d.C.; Castellote-Caballero, Y.; Rodríguez-López, C.; Aibar-Almazán, A. Pelvic Floor Muscle Exercises as a Treatment for Urinary Incontinence in Postmenopausal Women: A Systematic Review of Randomized Controlled Trials. Healthcare 2023, 11, 216. [Google Scholar] [CrossRef]
- NICE. NICE Guidance—Urinary incontinence and pelvic organ prolapse in women: Management © NICE (2019) Urinary incontinence and pelvic organ prolapse in women: Management. BJU Int. 2019, 123, 777–803. [Google Scholar] [CrossRef]
| Variables | All Participants (n = 62) | ||
|---|---|---|---|
| Age | 69.23 ± 4.83 | ||
| BMI (kg∙m−2) | 27.37 ± 4.01 | ||
| Parity | 1.60 ± 0.79 | ||
| IIQ score | 17.84 ± 21.43 | ||
| Incorrect technique (n = 20) | Correct technique (n = 42) | p-value | |
| Age | 70.25 ± 3.31 | 68.74 ± 5.37 | 0.252 |
| BMI (kg∙m−2) | 28.39 ± 3.55 | 26.88 ± 4.16 | 0.168 |
| Parity | 2.00 ± 1.12 | 1.93 ± 1.05 | 0.997 |
| IIQ score | 22.12 ± 26.92 | 15.70 ±18.1 | 0.603 |
| Age 60–69 (n = 30) | Age > 70 (n = 32) | p-value | |
| BMI (kg∙m−2) | 26.07 ± 4.07 | 28.59 ± 3.59 | 0.016 * |
| Parity | 1.92 ± 0.86 | 2 ± 1.24 | 0.882 |
| IIQ score | 13.12 ± 14.64 | 22.25 ± 25.72 | 0.284 |
| Asymptomatic group (IIQ = 0); (n = 28) | Symptomatic Group (IIQ > 0); (n = 34) | p-value | |
| Age | 69 ± 5.63 | 69.36 ± 4.13 | 0.552 |
| BMI (kg∙m−2) | 26.2 ± 3.5 | 28.26 ± 4.3 | 0.049 * |
| Parity | 1.44 ± 0.75 | 2.36 ± 1.11 | 0.003 * |
| All Participants (n = 62) | |||
|---|---|---|---|
| Exercise Number | Baseline Assessment | Biofeedback | p-Value |
| Exercise 1 | 2.68 ± 1.38 | 2.61 ± 1.23 | 0.616 |
| Exercise 2 | 2.47 ± 1.57 | 2.63 ± 1.36 | 0.36 |
| Exercise 3 | 2.4 ± 1.55 | 2.65 ± 1.4 | 0.169 |
| Exercise 4 | 2.47 ± 1.61 | 2.53 ± 1.48 | 0.668 |
| Exercise 5 | 2.6 ± 1.45 | 2.71 ± 1.37 | 0.568 |
| Exercise 6 | 2.56 ± 1.07 | 2.61 ± 0.98 | 0.657 |
| Exercise 7 | 2.65 ± 1.24 | 2.73 ± 0.99 | 0.681 |
| Exercise 8 | 2.6 ± 1.19 | 2.66 ± 1.02 | 0.781 |
| Exercise 9 | 2.58 ± 1.15 | 2.52 ± 1.08 | 0.496 |
| Exercise 10 | 2.66 ± 1.17 | 2.63 ± 0.89 | 0.792 |
| Exercise 11 | 2.52 ± 0.82 | 2.61 ± 0.8 | 0.411 |
| Women Presenting Incorrect Technique (n = 20) in the First Exercise at Baseline | |||
|---|---|---|---|
| Exercise Number | Baseline Assessment | Biofeedback | p-Value |
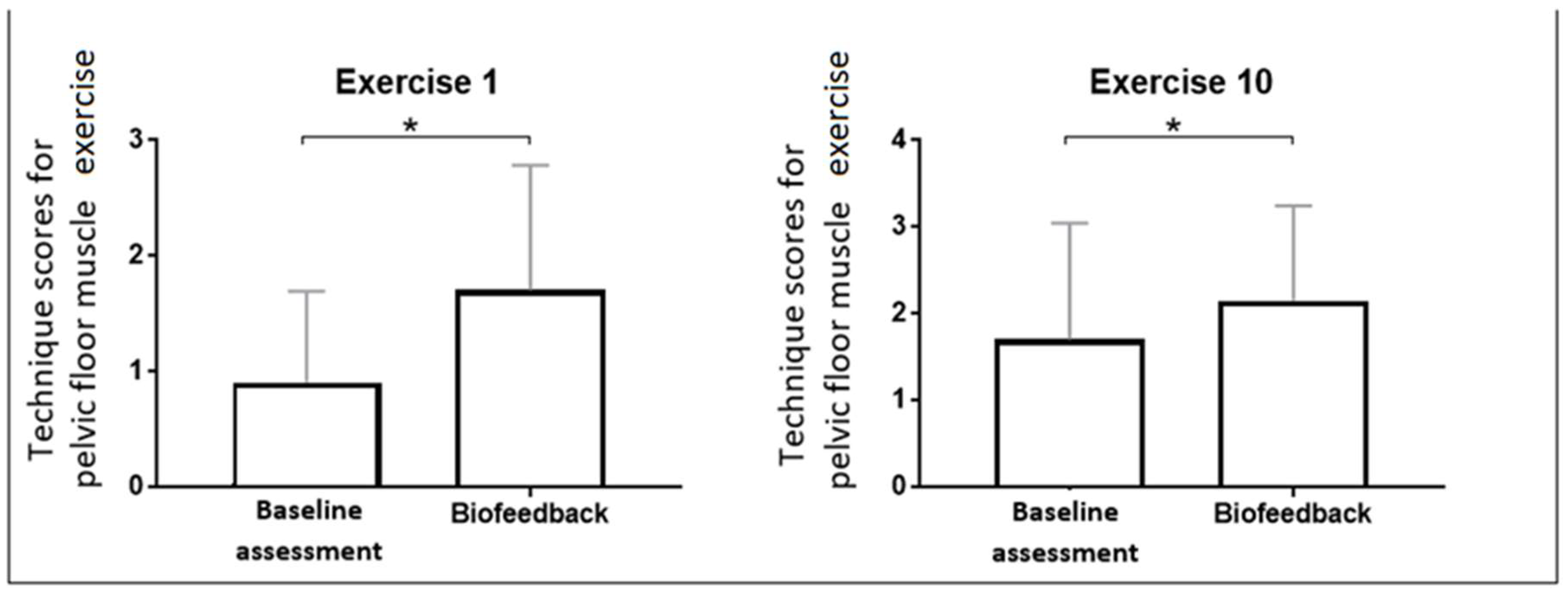
| Exercise 1 | 0.9 ± 0.79 | 1.7 ± 1.08 | 0.003 * |
| Exercise 2 | 1 ± 1.12 | 1.5 ± 1.28 | 0.948 |
| Exercise 3 | 1.05 ± 1.28 | 1.6 ± 1.47 | 0.605 |
| Exercise 4 | 1.05 ± 1.15 | 1.5 ± 1.32 | 0.709 |
| Exercise 5 | 1.6 ± 1.43 | 1.65 ± 1.27 | 0.575 |
| Exercise 6 | 1.8 ± 1.06 | 1.8 ± 1.15 | 0.67 |
| Exercise 7 | 1.55 ± 1.19 | 2.1 ± 1.37 | 0.334 |
| Exercise 8 | 1.6 ± 1.14 | 2.15 ± 1.04 | 0.207 |
| Exercise 9 | 1.55 ± 1.19 | 1.9 ± 1.17 | 0.064 |
| Exercise 10 | 1.7 ± 1.34 | 2.15 ± 1.09 | 0.037 * |
| Exercise 11 | 1.9 ± 0.79 | 2.15 ± 1.14 | 0.814 |
| Exercise Number | Age 60–69 (n = 30) | Age > 70 (n = 32) | ||||
|---|---|---|---|---|---|---|
| Baseline Assessment | Biofeedback | p-Value | Baseline Assessment | Biofeedback | p-Value | |
| Exercise 1 | 2.93 ± 1.23 | 2.83 ± 1.05 | 0.496 | 2.44 ± 1.48 | 2.41 ± 1.36 | 0.888 |
| Exercise 2 | 2.53 ± 1.59 | 2.77 ± 1.3 | 0.394 | 2.41 ± 1.56 | 2.5 ± 1.41 | 0.807 |
| Exercise 3 | 2.57 ± 1.5 | 2.8 ± 1.27 | 0.333 | 2.25 ± 1.61 | 2.5 ± 1.52 | 0.32 |
| Exercise 4 | 2.63 ± 1.59 | 2.7 ± 1.26 | 0.836 | 2.31 ± 1.64 | 2.38 ± 1.66 | 0.704 |
| Exercise 5 | 2.67 ± 1.4 | 2.93 ± 1.11 | 0.345 | 2.53 ± 1.52 | 2.5 ± 1.57 | 0.968 |
| Exercise 6 | 2.67 ± 0.99 | 2.5 ± 1.07 | 0.397 | 2.47 ± 1.14 | 2.72 ± 0.89 | 0.187 |
| Exercise 7 | 2.6 ± 1.3 | 2.73 ± 0.83 | 0.594 | 2.69 ± 1.2 | 2.72 ± 1.14 | 0.979 |
| Exercise 8 | 2.73 ± 1.14 | 2.6 ± 0.97 | 0.46 | 2.47 ± 1.24 | 2.72 ± 1.08 | 0.334 |
| Exercise 9 | 2.63 ± 1.19 | 2.43 ± 1.1 | 0.301 | 2.53 ± 1.14 | 2.59 ± 1.07 | 0.807 |
| Exercise 10 | 2.67 ± 1.27 | 2.5 ± 0.97 | 0.352 | 2.66 ± 1.1 | 2.75 ± 0.8 | 0.529 |
| Exercise 11 | 2.63 ± 0.76 | 2.7 ± 0.53 | 0.575 | 2.41 ± 0.87 | 2.53 ± 0.98 | 0.552 |
| Exercise Number | Asymptomatic Group (IIQ = 0); (n = 28) | Symptomatic group (IIQ > 0); (n = 34) | ||||
|---|---|---|---|---|---|---|
| Baseline Assessment | Biofeedback | p-Value | Baseline Assessment | Biofeedback | p-Value | |
| Exercise 1 | 2.74 ± 1.38 | 2.78 ± 1.05 | 0.859 | 2.61 ± 1.43 | 2.52 ± 1.37 | 0.737 |
| Exercise 2 | 2.41 ± 1.55 | 2.56 ± 1.45 | 0.776 | 2.52 ± 1.64 | 2.67 ± 1.34 | 0.433 |
| Exercise 3 | 2.48 ± 1.53 | 2.59 ± 1.47 | 0.722 | 2.39 ± 1.58 | 2.67 ± 1.41 | 0.248 |
| Exercise 4 | 2.22 ± 1.74 | 2.52 ± 1.58 | 0.272 | 2.7 ± 1.51 | 2.52 ± 1.46 | 0.614 |
| Exercise 5 | 2.41 ± 1.5 | 2.59 ± 1.5 | 0.754 | 2.79 ± 1.43 | 2.76 ± 1.3 | 0.996 |
| Exercise 6 | 2.59 ± 1.12 | 2.63 ± 0.97 | 0.824 | 2.55 ± 1.06 | 2.61 ± 1.03 | 0.629 |
| Exercise 7 | 2.56 ± 1.25 | 2.78 ± 0.89 | 0.48 | 2.76 ± 1.25 | 2.7 ± 1.1 | 0.717 |
| Exercise 8 | 2.59 ± 1.22 | 2.81 ± 0.74 | 0.3 | 2.58 ± 1.23 | 2.64 ± 1.14 | 0.974 |
| Exercise 9 | 2.56 ± 1.19 | 2.33 ± 1.27 | 0.262 | 2.58 ± 1.17 | 2.7 ± 0.88 | 0.695 |
| Exercise 10 | 2.56 ± 1.28 | 2.7 ± 0.82 | 0.507 | 2.73 ± 1.13 | 2.58 ± 0.97 | 0.293 |
| Exercise 11 | 2.56 ± 0.8 | 2.52 ± 0.85 | 0.859 | 2.48 ± 0.87 | 2.7 ± 0.77 | 0.158 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piernicka, M.; Ossowski, Z.; Kortas, J.; Bojar, D.; Labun, J.; Szumilewicz, A. Can We Improve the Technique of Pelvic Floor Muscle Exercises in Postmenopausal Women Using a Single Electromyography Biofeedback Session? An Experimental Study. J. Clin. Med. 2024, 13, 3062. https://doi.org/10.3390/jcm13113062
Piernicka M, Ossowski Z, Kortas J, Bojar D, Labun J, Szumilewicz A. Can We Improve the Technique of Pelvic Floor Muscle Exercises in Postmenopausal Women Using a Single Electromyography Biofeedback Session? An Experimental Study. Journal of Clinical Medicine. 2024; 13(11):3062. https://doi.org/10.3390/jcm13113062
Chicago/Turabian StylePiernicka, Magdalena, Zbigniew Ossowski, Jakub Kortas, Damian Bojar, Justyna Labun, and Anna Szumilewicz. 2024. "Can We Improve the Technique of Pelvic Floor Muscle Exercises in Postmenopausal Women Using a Single Electromyography Biofeedback Session? An Experimental Study" Journal of Clinical Medicine 13, no. 11: 3062. https://doi.org/10.3390/jcm13113062
APA StylePiernicka, M., Ossowski, Z., Kortas, J., Bojar, D., Labun, J., & Szumilewicz, A. (2024). Can We Improve the Technique of Pelvic Floor Muscle Exercises in Postmenopausal Women Using a Single Electromyography Biofeedback Session? An Experimental Study. Journal of Clinical Medicine, 13(11), 3062. https://doi.org/10.3390/jcm13113062







