Protein Deposition on Sport Mouthguards and the Effectiveness of Two Different Cleaning Protocols
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Sample Collection
2.2. Protein Elution and Gel Electrophoresis
2.3. Western Blotting
2.4. Gel Analysis and Quantification
2.5. Amylase Biological Activity
2.6. Statistical Analysis
3. Results
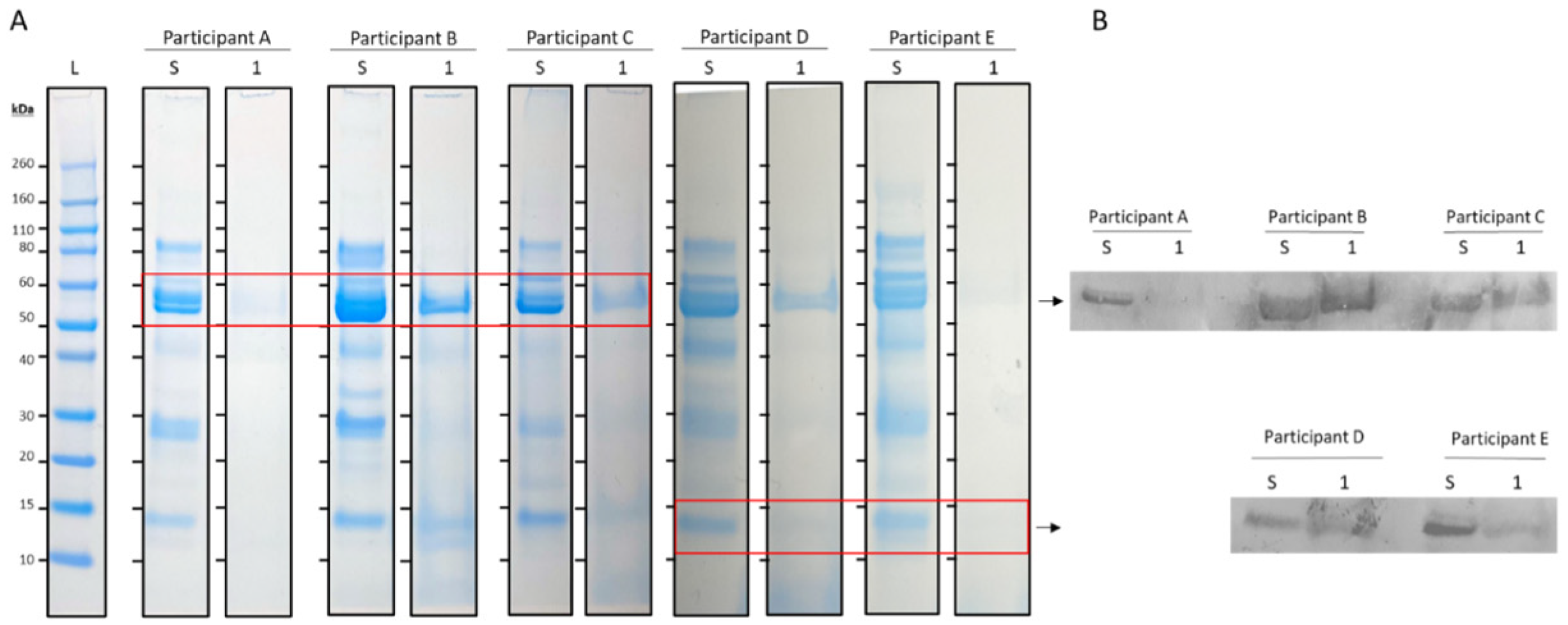
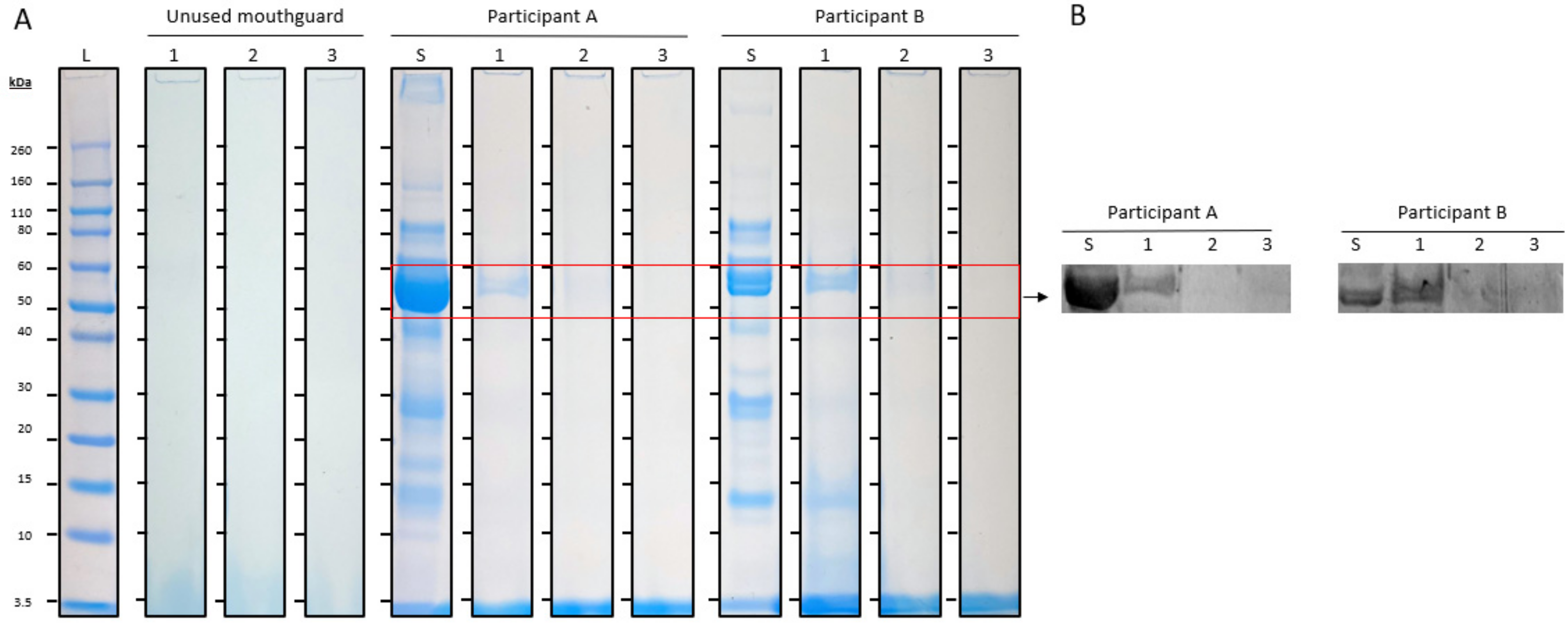
3.1. SDS-PAGE and Western Blotting
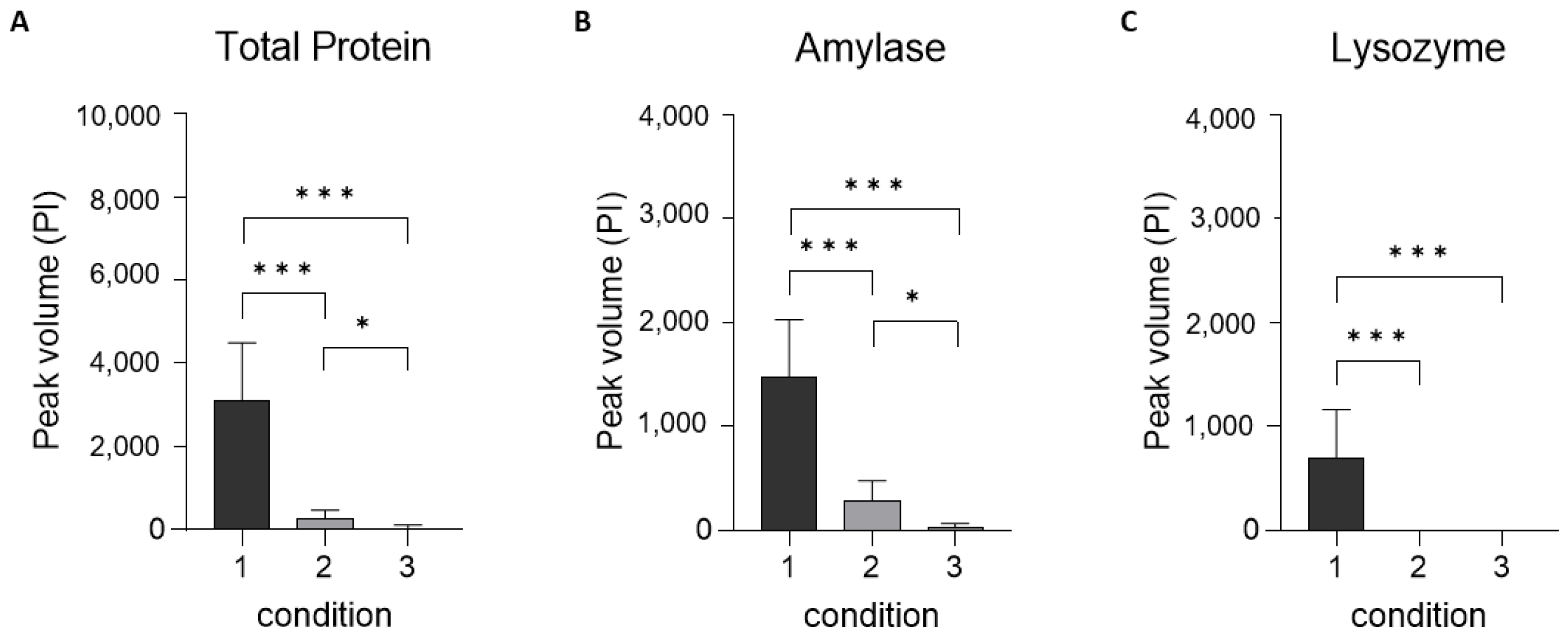
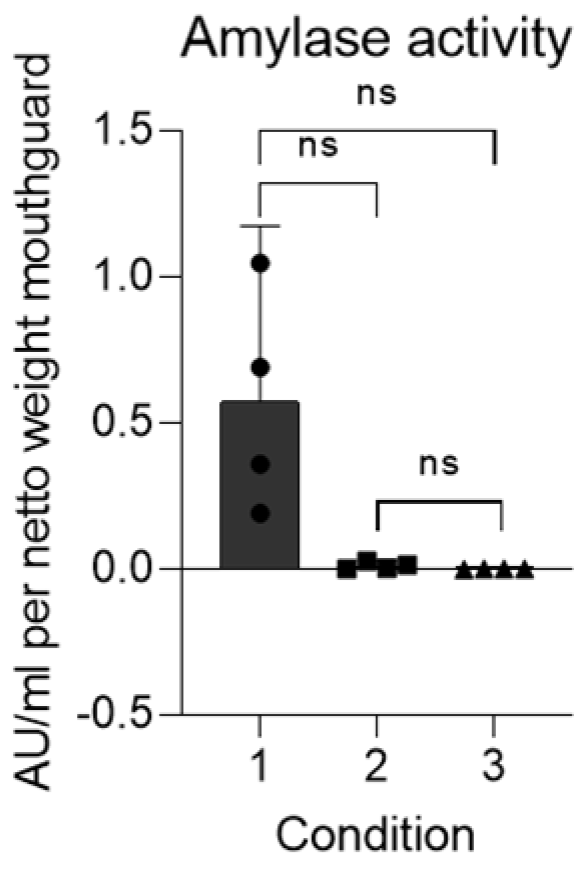
3.2. Gel Analysis and Quantification
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Spinas, E.; Mameli, A.; Giannetti, L. Traumatic Dental Injuries Resulting from Sports Activities; Immediate Treatment and Five Years Follow-Up: An Observational Study. Open Dent. J. 2018, 12, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Spinas, E.; Giannetti, L.; Mameli, A.; Re, D. Dental injuries in young athletes, a five-year follow-up study. Eur. J. Paediatr. Dent. 2018, 19, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Lam, R. Epidemiology and outcomes of traumatic dental injuries: A review of the literature. Aust. Dent. J. 2016, 61 (Suppl. S1), 4–20. [Google Scholar] [CrossRef] [PubMed]
- Newsome, P.R.; Tran, D.C.; Cooke, M.S. The role of the mouthguard in the prevention of sports-related dental injuries: A review. Int. J. Paediatr. Dent. 2001, 11, 396–404. [Google Scholar] [CrossRef] [PubMed]
- Knapik, J.J.; Marshall, S.W.; Lee, R.B.; Darakjy, S.S.; Jones, S.B.; Mitchener, T.A.; delaCruz, G.G.; Jones, B.H. Mouthguards in sport activities: History, physical properties and injury prevention effectiveness. Sports Med. 2007, 37, 117–144. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, L.M.; Neto, J.C.L.; Lima, T.F.R.; Magno, M.B.; Santiago, B.M.; Cavalcanti, Y.W.; de Almeida, L.F.D. The use of mouthguards and prevalence of dento-alveolar trauma among athletes: A systematic review and meta-analysis. Dent. Traumatol. 2019, 35, 54–72. [Google Scholar] [CrossRef] [PubMed]
- Vucic, S.; Drost, R.W.; Ongkosuwito, E.M.; Wolvius, E.B. Dentofacial trauma and players’ attitude towards mouthguard use in field hockey: A systematic review and meta-analysis. Br. J. Sports Med. 2016, 50, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Vucic, S.; Drost, R.W.; van Wijk, A.J.; Wesselink, P.R.; Wolvius, E.B. Patterns of orodental injury and mouthguard use in Dutch field hockey. Br. J. Sports Med. 2016, 50, 661–668. [Google Scholar] [CrossRef] [PubMed]
- Bolhuis, J.H.; Baarda, D.B.; Leurs, J.M.M.; Flogel, G.E. Incidentie en preventie van tandtraumata bij de hockeysport. Ned. Tijdschr. Tandheelkd. 1986, 92, 283. [Google Scholar]
- Bolhuis, J.H.; Leurs, J.M.; Flogel, G.E.; Lam, R. Dental and facial injuries in international field hockey. Br. J. Sports Med. 1987, 21, 174–177. [Google Scholar] [CrossRef]
- Bolhuis, J.H.; Baarda, D.B.; Leurs, J.M.; Stokhuyzen, Y.L.M.; Flogel, G.E. Factoren die het gebruik van gebitsbeschermers beïnvloeden. Ned. Tijdschr. Tandheelkd. 1988, 95, 393–397. [Google Scholar] [PubMed]
- Hendrick, K.; Farrelly, P.; Jagger, R. Oro-facial injuries and mouthguard use in elite female field hockey players. Dent. Traumatol. 2008, 24, 189–192. [Google Scholar] [CrossRef] [PubMed]
- Glass, R.T.; Wood, C.R.; Bullard, J.W.; Conrad, R.S. Possible disease transmission by contaminated mouthguards in two young football players. Gen. Dent. 2007, 55, 436–440. [Google Scholar]
- Glass, R.T.; Bullard, J.W.; Conrad, R.S. The contamination of protective mouth-guards: A characterization of the microbiota found in football players’ protective mouth-guards as compared to the oral microbiotica found in first-year medical students. Am. Dent. Inst. Cont. Educ. J. 2006, 93, 23–38. [Google Scholar]
- Glass, R.T.; Conrad, R.S.; Wood, C.R.; Warren, A.J.; Kohler, G.A.; Bullard, J.W.; Benson, G.; Gulden, J.M. Protective athletic mouthguards: Do they cause harm? Sports Health 2009, 1, 411–415. [Google Scholar] [CrossRef] [PubMed]
- D’Ercole, S.; Martinelli, D.; Tripodi, D. Influence of sport mouthguards on the ecological factors of the children oral cavity. BMC Oral Health 2014, 14, 97. [Google Scholar] [CrossRef] [PubMed]
- D’Ercole, S.; Tieri, M.; Fulco, D.; Martinelli, D.; Tripodi, D. The use of chlorhexidine in mouthguards. J. Biol. Regul. Homeost. Agents 2017, 31, 487–493. [Google Scholar] [PubMed]
- Glass, R.T.; Conrad, R.S.; Kohler, G.A.; Warren, A.J.; Bullard, J.W. Microbiota found in protective athletic mouthguards. Sports Health 2011, 3, 244–248. [Google Scholar] [CrossRef]
- Nagai, K.; Domon, H.; Oda, M.; Shirai, T.; Ohsumi, T.; Terao, Y.; Arai, Y. Antimicrobial activity of ethylene-vinyl acetate containing bioactive filler against oral bacteria. Dent. Mater. J. 2017, 36, 784–790. [Google Scholar] [CrossRef]
- Tripodi, D.; Martinelli, D.; Ciaravino, C.; Fulco, D.; Tieri, M.; D’Ercole, S. The use of casein in sport mouthguards: Microbiological and ecological variations in oral cavity. J. Biol. Regul. Homeost. Agents 2018, 32, 1045–1049. [Google Scholar]
- Heo, S.M.; Ruhl, S.; Scannapieco, F.A. Implications of salivary protein binding to commensal and pathogenic bacteria. J. Oral Biosci. 2013, 55, 169–174. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Baker, O.J.; Edgerton, M.; Kramer, J.M.; Ruhl, S. Saliva-microbe interactions and salivary gland dysfunction. Adv. Dent. Res. 2014, 26, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Han, A.; Tsoi, J.K.H.; Flavia Rodrigues, F.; Leprince, J.G.; Palin, W.M. Bacterial adhesion mechanisms on dental implant surfaces and the influencing factors. Int. J. Adhes. Adhes. 2016, 69, 58–71. [Google Scholar] [CrossRef]
- Iorgulescu, G. Saliva between normal and pathological. Important factors in determining systemic and oral health. J. Med. Life 2009, 2, 303–307. [Google Scholar] [PubMed]
- Lynge Pedersen, A.M.; Belstrøm, D. The role of natural salivary defences in maintaining a healthy oral microbiota. J. Dent. 2019, 80 (Suppl. S1), S3–S12. [Google Scholar] [CrossRef] [PubMed]
- van ’t Hof, W.; Veerman, E.C.; Nieuw Amerongen, A.V.; Ligtenberg, A.J. Antimicrobial defense systems in saliva. Monogr. Oral Sci. 2014, 24, 40–51. [Google Scholar] [CrossRef] [PubMed]
- Nawaz, N.; Wen, S.; Wang, F.; Nawaz, S.; Raza, J.; Iftikhar, M.; Usman, M. Lysozyme and its application as bacterial agent in food industry. Molecules 2022, 27, 6305. [Google Scholar] [CrossRef] [PubMed]
- Gibbons, R.J.; Hay, D.I. Human salivary acidic proline-rich proteins and statherin promote the attachment of Actinomyces viscosus LY7 to apatite surfaces. Infect. Immun. 1988, 56, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Jesse Joel, T.; Suguna, S.; Stef, S.R. Antimicrobial Activity of Lysozyme Against Oral Pathogens. Asian J. Pharm. Res. Health Care 2016, 8, 42–46. [Google Scholar] [CrossRef]
- Kurtzman, G.M.; Horowitz, R.A.; Johnson, R.; Prestiano, R.A.; Klein, B.I. The systemic oral health connection: Biofilms. Medicine 2022, 101, e30517. [Google Scholar] [CrossRef]
- Peyrot des Gachons, C.; Breslin, P.A.S. Salivary amylase: Digestion and metabolic syndrome. Curr. Diabetes Rep. 2016, 16, 102. [Google Scholar] [CrossRef] [PubMed]
- Abranches, J.; Zeng, L.; Kajfasz, J.K.; Palmer, S.R.; Chakraborty, B.; Wen, Z.T.; Richards, V.P.; Brady, L.J.; Lemos, J.A. Biology of Oral Streptococci. Microbiol. Spectr. 2018, 6. [Google Scholar] [CrossRef] [PubMed]
- Mandel, A.L.; Peyrot des Gachons, C.; Plank, K.L.; Alarcon, S.; Breslin, P.A.S. Individual differences in AMY1 gene copy number, salivary α-amylase levels, and the perception of oral starch. PLoS ONE 2010, 5, e13352. [Google Scholar] [CrossRef] [PubMed]
- Bosch, J.A.; Brand, H.S.; Ligtenberg, T.J.; Bermond, B.; Hoogstraten, J.; Nieuw Amerongen, A.V. Psychological stress as a determinant of protein levels and salivary-induced aggregation of Streptococcus gordonii in human whole saliva. Psychosom. Med. 1996, 58, 374–382. [Google Scholar] [CrossRef]
- Prodan, A.; Brand, H.S.; Ligtenberg, A.J.M.; Imangaliyev, S.; Tsivtsivadze, E.; van der Weijden, G.A.; Crielaard, W.; Keijser, B.J.F.; Veerman, E.C.I. Interindividual variation, correlations, and sex-related differences in the salivary biochemistry of young healthy adults. Eur. J. Oral Sci. 2015, 123, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Ntovas, P.; Loumprinis, N.; Maniatakos, P.; Margaritidi, L.; Rahiotis, C. The effects of physical exercise on saliva composition: A comprehensive review. Dent. J. 2022, 10, 7. [Google Scholar] [CrossRef]
- Gillum, T.L.; Kuennen, M.R.; Gourley, C.; Schneider, S.; Dokladny, K.; Moseley, P. Salivary antimicrobial protein response to prolonged running. Biol. Sport 2013, 30, 3–8. [Google Scholar] [CrossRef] [PubMed]
- Gillum, T.; Kuennen, M.; McKenna, Z.; Castillo, M.; Jordan-Patterson, A.; Bohnert, C. Exercise does not increase salivary lymphocytes. monocytes, or granulocytes, but does increase salivary lysozyme. J. Sports Sci. 2017, 35, 1294–1299. [Google Scholar] [CrossRef] [PubMed]
- Ligtenberg, A.J.M.; Brand, H.S.; van den Keijbus, P.A.M.; Veerman, E.C.I. The effect of physical exercise on salivary secretion of MUC5B, amylase and lysozyme. Arch. Oral Biol. 2015, 60, 1639–1644. [Google Scholar] [CrossRef]
- Bishop, N.C.; Gleeson, M. Acute and chronic effects of exercise on markers of mucosal immunity. Front. Biosci. 2009, 14, 4444–4456. [Google Scholar] [CrossRef]
- Yasuda, N.; Yamamoto, K.; Iwashita, N. Concurrent evaluation of salivary and urinary α-amylase activity following prolonged exercise with or without carbohydrate solution in aerobically active men. Neuro Endocrinol. Lett. 2021, 42, 265–276. [Google Scholar] [PubMed]
- Teughels, W.; Van Assche, N.; Sliepen, I.; Quirynen, M. Effect of material characteristics and/or surface topography on biofilm development. Clin. Oral Implant. Res. 2006, 17 (Suppl. S2), 68–81. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Vliet, K.; van Splunter, A.; de Lange, J.; Lobbezoo, F.; Brand, H. Protein Deposition on Sport Mouthguards and the Effectiveness of Two Different Cleaning Protocols. J. Clin. Med. 2024, 13, 3023. https://doi.org/10.3390/jcm13113023
van Vliet K, van Splunter A, de Lange J, Lobbezoo F, Brand H. Protein Deposition on Sport Mouthguards and the Effectiveness of Two Different Cleaning Protocols. Journal of Clinical Medicine. 2024; 13(11):3023. https://doi.org/10.3390/jcm13113023
Chicago/Turabian Stylevan Vliet, Kirsten, Annina van Splunter, Jan de Lange, Frank Lobbezoo, and Henk Brand. 2024. "Protein Deposition on Sport Mouthguards and the Effectiveness of Two Different Cleaning Protocols" Journal of Clinical Medicine 13, no. 11: 3023. https://doi.org/10.3390/jcm13113023
APA Stylevan Vliet, K., van Splunter, A., de Lange, J., Lobbezoo, F., & Brand, H. (2024). Protein Deposition on Sport Mouthguards and the Effectiveness of Two Different Cleaning Protocols. Journal of Clinical Medicine, 13(11), 3023. https://doi.org/10.3390/jcm13113023






