Advanced Paternal Age in Focus: Unraveling Its Influence on Assisted Reproductive Technology Outcomes
Abstract
1. Introduction
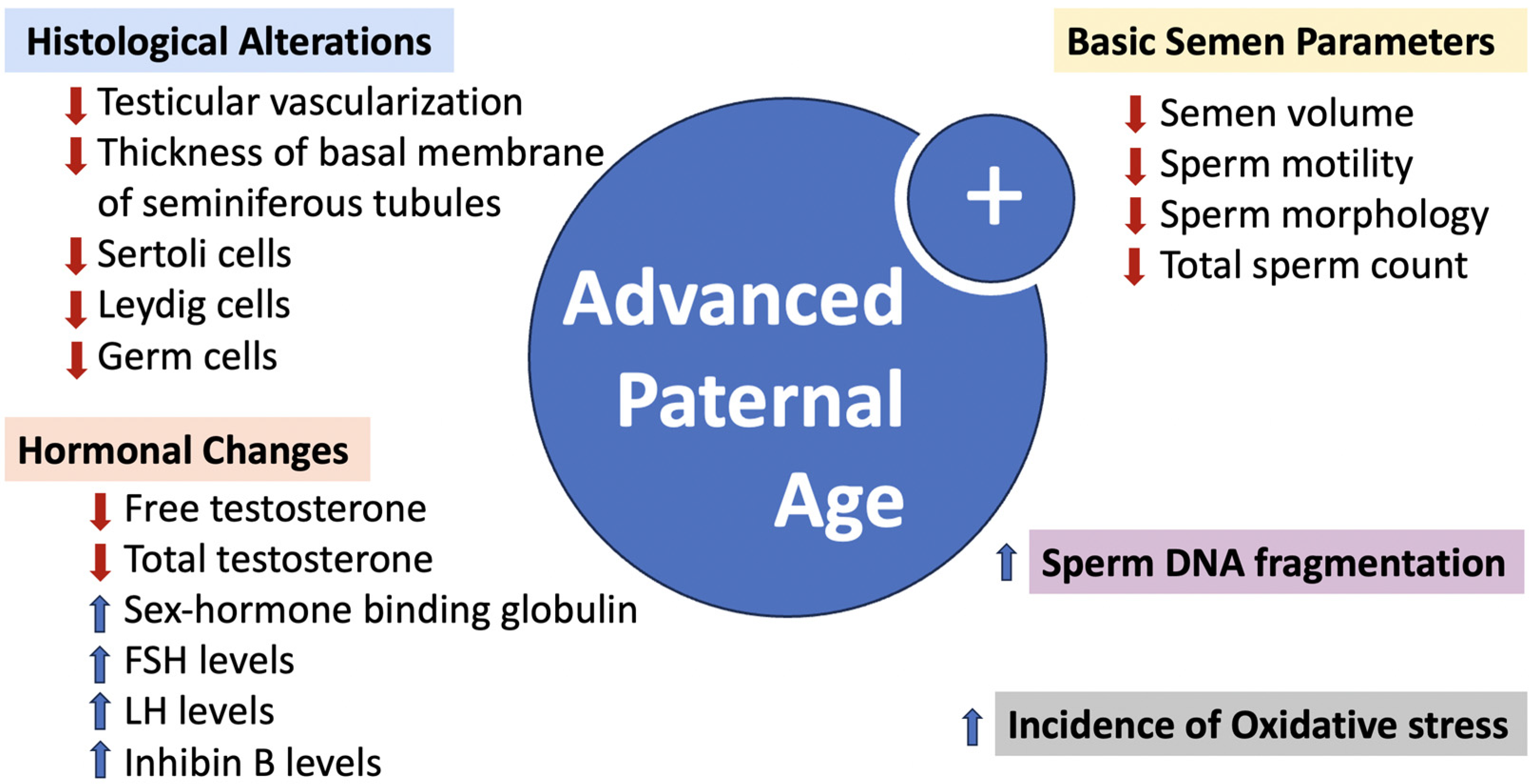
2. Trends in Increasing Paternal Age and ART
3. Aging and Its Impact on Male Reproductive Health: Anatomical, Cellular, and Molecular Perspectives
4. Paternal Aging: Effects on Sperm Integrity, Epigenetics, and Reproductive Health Implications
5. Impact of Advanced Paternal Age on ART Outcomes
5.1. Impact of Paternal Age on Fertilization Rates
5.2. Effect of Paternal Age on Embryo Quality
5.3. Effect of Paternal Age on Implantation
5.4. Effect of Paternal Age on Miscarriages
5.5. Effect of Advanced Paternal Age and Perinatal Risks
5.6. Effect of Paternal Age on Live Birth Rate
6. Strategies for Deferred Fatherhood and Future Research Directions
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sartorius, G.A.; Nieschlag, E. Paternal age and reproduction. Hum. Reprod. Update 2010, 16, 65–79. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, L.; Sobotka, T.; Bentzen, J.G.; Nyboe Andersen, A.; Reproduction, E.; Society Task, F. Demographic and medical consequences of the postponement of parenthood. Hum. Reprod. Update 2012, 18, 29–43. [Google Scholar] [CrossRef] [PubMed]
- Craig, J.R.; Jenkins, T.G.; Carrell, D.T.; Hotaling, J.M. Obesity, male infertility, and the sperm epigenome. Fertil. Steril. 2017, 107, 848–859. [Google Scholar] [CrossRef] [PubMed]
- Campbell, J.M.; Lane, M.; Owens, J.A.; Bakos, H.W. Paternal obesity negatively affects male fertility and assisted reproduction outcomes: A systematic review and meta-analysis. Reprod. Biomed. Online 2015, 31, 593–604. [Google Scholar] [CrossRef] [PubMed]
- Mills, M.; Rindfuss, R.R.; McDonald, P.; te Velde, E.; Reproduction, E.; Society Task, F. Why do people postpone parenthood? Reasons and social policy incentives. Hum. Reprod. Update 2011, 17, 848–860. [Google Scholar] [CrossRef] [PubMed]
- Bray, I.; Gunnell, D.; Davey Smith, G. Advanced paternal age: How old is too old? J. Epidemiol. Community Health 2006, 60, 851–853. [Google Scholar] [CrossRef] [PubMed]
- Sharma, R.; Agarwal, A.; Rohra, V.K.; Assidi, M.; Abu-Elmagd, M.; Turki, R.F. Effects of increased paternal age on sperm quality, reproductive outcome and associated epigenetic risks to offspring. Reprod. Biol. Endocrinol. 2015, 13, 35. [Google Scholar] [CrossRef] [PubMed]
- Kaltsas, A.; Moustakli, E.; Zikopoulos, A.; Georgiou, I.; Dimitriadis, F.; Symeonidis, E.N.; Markou, E.; Michaelidis, T.M.; Tien, D.M.B.; Giannakis, I.; et al. Impact of Advanced Paternal Age on Fertility and Risks of Genetic Disorders in Offspring. Genes 2023, 14, 486. [Google Scholar] [CrossRef] [PubMed]
- Santi, D.; Lotti, F.; Sparano, C.; Rastrelli, G.; Isidori, A.M.; Pivonello, R.; Barbonetti, A.; Salonia, A.; Minhas, S.; Krausz, C.; et al. Does an increase in adipose tissue ‘weight’ affect male fertility? A systematic review and meta-analysis based on semen analysis performed using the WHO 2010 criteria. Andrology 2024, 12, 123–136. [Google Scholar] [CrossRef] [PubMed]
- Du Plessis, S.S.; Cabler, S.; McAlister, D.A.; Sabanegh, E.; Agarwal, A. The effect of obesity on sperm disorders and male infertility. Nat. Rev. Urol. 2010, 7, 153–161. [Google Scholar] [CrossRef]
- Kaltsas, A.; Markou, E.; Zachariou, A.; Dimitriadis, F.; Mamoulakis, C.; Andreadakis, S.; Giannakis, I.; Tsounapi, P.; Takenaka, A.; Sofikitis, N. Varicoceles in Men With Non-obstructive Azoospermia: The Dilemma to Operate or Not. Front. Reprod. Health 2022, 4, 811487. [Google Scholar] [CrossRef] [PubMed]
- Stone, B.A.; Alex, A.; Werlin, L.B.; Marrs, R.P. Age thresholds for changes in semen parameters in men. Fertil. Steril. 2013, 100, 952–958. [Google Scholar] [CrossRef] [PubMed]
- D’Onofrio, B.M.; Rickert, M.E.; Frans, E.; Kuja-Halkola, R.; Almqvist, C.; Sjolander, A.; Larsson, H.; Lichtenstein, P. Paternal age at childbearing and offspring psychiatric and academic morbidity. JAMA Psychiatry 2014, 71, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Halvaei, I.; Litzky, J.; Esfandiari, N. Advanced paternal age: Effects on sperm parameters, assisted reproduction outcomes and offspring health. Reprod. Biol. Endocrinol. 2020, 18, 110. [Google Scholar] [CrossRef] [PubMed]
- Khandwala, Y.S.; Zhang, C.A.; Lu, Y.; Eisenberg, M.L. The age of fathers in the USA is rising: An analysis of 168 867 480 births from 1972 to 2015. Hum. Reprod. 2017, 32, 2110–2116. [Google Scholar] [CrossRef] [PubMed]
- Gourinat, A.; Mazeaud, C.; Hubert, J.; Eschwege, P.; Koscinski, I. Impact of paternal age on assisted reproductive technology outcomes and offspring health: A systematic review. Andrology 2023, 11, 973–986. [Google Scholar] [CrossRef] [PubMed]
- Human, F.; Embryology, A. Code of Practice, 9th ed.; HM Revenue & Customs: Belfast, Ireland, 2023. [Google Scholar]
- Practice Committee of the American Society for Reproductive Medicine; The Practice Committee for the Society for Assisted Reproductive Technology. Guidance regarding gamete and embryo donation. Fertil. Steril. 2021, 115, 1395–1410. [Google Scholar] [CrossRef] [PubMed]
- Fertility Society of Australia & New Zealand. RTAC Code of Practice. Available online: https://www.fertilitysociety.com.au/rtac-australia-new-zealand/ (accessed on 12 April 2021).
- Agence de la biomédecine. Avis du Conseil D’orientation émis à L’initiative de Son Président et Concernant L’âge de Procréer. Available online: https://www.agence-biomedecine.fr/Avis-du-conseil-d-orientation-emis,880 (accessed on 5 July 2017).
- European Society of Human Reproduction and Embryology. Statements by the Task Force Ethics and Law. Available online: https://www.eshre.eu/Specialty-groups/Special-Interest-Groups/Ethics-and-Law/Documents-of-the-Task-Force-Ethics-Law (accessed on 27 April 2021).
- Cavazos-Rehg, P.A.; Krauss, M.J.; Spitznagel, E.L.; Bommarito, K.; Madden, T.; Olsen, M.A.; Subramaniam, H.; Peipert, J.F.; Bierut, L.J. Maternal age and risk of labor and delivery complications. Matern. Child Health J. 2015, 19, 1202–1211. [Google Scholar] [CrossRef] [PubMed]
- Phillips, N.; Taylor, L.; Bachmann, G. Maternal, infant and childhood risks associated with advanced paternal age: The need for comprehensive counseling for men. Maturitas 2019, 125, 81–84. [Google Scholar] [CrossRef]
- Jain, T.; Grainger, D.A.; Ball, G.D.; Gibbons, W.E.; Rebar, R.W.; Robins, J.C.; Leach, R.E. 30 years of data: Impact of the United States in vitro fertilization data registry on advancing fertility care. Fertil. Steril. 2019, 111, 477–488. [Google Scholar] [CrossRef]
- Marsidi, A.M.; Kipling, L.M.; Kawwass, J.F.; Mehta, A. Influence of paternal age on assisted reproductive technology cycles and perinatal outcomes. Fertil. Steril. 2021, 116, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Sampson, N.; Untergasser, G.; Plas, E.; Berger, P. The ageing male reproductive tract. J. Pathol. 2007, 211, 206–218. [Google Scholar] [CrossRef] [PubMed]
- Luna, M.; Finkler, E.; Barritt, J.; Bar-Chama, N.; Sandler, B.; Copperman, A.B.; Grunfeld, L. Paternal age and assisted reproductive technology outcome in ovum recipients. Fertil. Steril. 2009, 92, 1772–1775. [Google Scholar] [CrossRef] [PubMed]
- Bartolacci, A.; Pagliardini, L.; Makieva, S.; Salonia, A.; Papaleo, E.; Vigano, P. Abnormal sperm concentration and motility as well as advanced paternal age compromise early embryonic development but not pregnancy outcomes: A retrospective study of 1266 ICSI cycles. J. Assist. Reprod. Genet. 2018, 35, 1897–1903. [Google Scholar] [CrossRef] [PubMed]
- De La Rochebrochard, E.; Thonneau, P. Paternal age: Are the risks of infecundity and miscarriage higher when the man is aged 40 years or over? Rev. D’épidémiologie Et Santé Publique 2005, 53, 47–55. [Google Scholar] [CrossRef]
- Aboulghar, M.; Mansour, R.; Al-Inany, H.; Abou-Setta, A.M.; Aboulghar, M.; Mourad, L.; Serour, G. Paternal age and outcome of intracytoplasmic sperm injection. Reprod. Biomed. Online 2007, 14, 588–592. [Google Scholar] [CrossRef] [PubMed]
- Horta, F.; Vollenhoven, B.; Healey, M.; Busija, L.; Catt, S.; Temple-Smith, P. Male ageing is negatively associated with the chance of live birth in IVF/ICSI cycles for idiopathic infertility. Hum. Reprod. 2019, 34, 2523–2532. [Google Scholar] [CrossRef]
- Van Opstal, J.; Fieuws, S.; Spiessens, C.; Soubry, A. Male age interferes with embryo growth in IVF treatment. Hum. Reprod. 2021, 36, 107–115. [Google Scholar] [CrossRef]
- Ilacqua, A.; Izzo, G.; Emerenziani, G.P.; Baldari, C.; Aversa, A. Lifestyle and fertility: The influence of stress and quality of life on male fertility. Reprod. Biol. Endocrinol. 2018, 16, 115. [Google Scholar] [CrossRef]
- Laurentino, S.; Cremers, J.F.; Horsthemke, B.; Tuttelmann, F.; Czeloth, K.; Zitzmann, M.; Pohl, E.; Rahmann, S.; Schroder, C.; Berres, S.; et al. A germ cell-specific ageing pattern in otherwise healthy men. Aging Cell 2020, 19, e13242. [Google Scholar] [CrossRef]
- Dain, L.; Auslander, R.; Dirnfeld, M. The effect of paternal age on assisted reproduction outcome. Fertil. Steril. 2011, 95, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Shandley, L.M.; DeSantis, C.E.; Lee, J.C.; Kawwass, J.F.; Hipp, H.S. Trends and Outcomes of Assisted Reproductive Technology Cycles Using a Gestational Carrier Between 2014 and 2020. JAMA 2023, 330, 1691–1694. [Google Scholar] [CrossRef] [PubMed]
- Paavilainen, M.; Bloigu, A.; Hemminki, E.; Gissler, M.; Klemetti, R. Aging fatherhood in Finland—First-time fathers in Finland from 1987 to 2009. Scand. J. Public Health 2016, 44, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Lewington, L.; Lee, J.; Sebar, B. “I’m not Just a Babysitter”: Masculinity and Men’s Experiences of First-Time Fatherhood. Men Masculinities 2021, 24, 571–589. [Google Scholar] [CrossRef]
- Wang, Z.; Liu, X.; Xu, J.; Yang, Q.; Niu, W.; Dai, S.; Hu, L.; Guo, Y. Paternal age, body mass index, and semen volume are associated with chromosomal aberrations-related miscarriages in couples that underwent treatment by assisted reproductive technology. Aging 2020, 12, 8459–8472. [Google Scholar] [CrossRef] [PubMed]
- Reinicke, K. “I thought, Oh shit, because I was 19.” Discourses and practices on young fatherhood in Denmark. Fam. Relatsh. Soc. 2021, 10, 463–478. [Google Scholar] [CrossRef]
- Xi, Y.P.; Nette, E.G.; King, D.W.; Rosen, M. Age-related changes in normal human basement membrane. Mech. Ageing Dev. 1982, 19, 315–324. [Google Scholar] [CrossRef]
- Jiang, H.; Zhu, W.J.; Li, J.; Chen, Q.J.; Liang, W.B.; Gu, Y.Q. Quantitative histological analysis and ultrastructure of the aging human testis. Int. Urol. Nephrol. 2014, 46, 879–885. [Google Scholar] [CrossRef]
- Dong, S.; Chen, C.; Zhang, J.; Gao, Y.; Zeng, X.; Zhang, X. Testicular aging, male fertility and beyond. Front. Endocrinol. 2022, 13, 1012119. [Google Scholar] [CrossRef]
- Nita, M.; Strzalka-Mrozik, B.; Grzybowski, A.; Mazurek, U.; Romaniuk, W. Age-related macular degeneration and changes in the extracellular matrix. Med. Sci. Monit. 2014, 20, 1003–1016. [Google Scholar] [CrossRef]
- Pohl, E.; Gromoll, J.; Wistuba, J.; Laurentino, S. Healthy ageing and spermatogenesis. Reproduction 2021, 161, R89–R101. [Google Scholar] [CrossRef] [PubMed]
- Johnson, S.L.; Dunleavy, J.; Gemmell, N.J.; Nakagawa, S. Consistent age-dependent declines in human semen quality: A systematic review and meta-analysis. Ageing Res. Rev. 2015, 19, 22–33. [Google Scholar] [CrossRef]
- Oliveira, J.B.A.; Petersen, C.G.; Mauri, A.L.; Vagnini, L.D.; Baruffi, R.L.R.; Franco, J.G., Jr. The effects of age on sperm quality: An evaluation of 1,500 semen samples. JBRA Assist. Reprod. 2014, 18, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.X.; Meads, C.; Lu, M.L.; Wu, J.Q.; Zhou, W.J.; Gao, E.S. Turning point of age for semen quality: A population-based study in Chinese men. Fertil. Steril. 2011, 96, 572–576. [Google Scholar] [CrossRef]
- Eskenazi, B.; Wyrobek, A.J.; Sloter, E.; Kidd, S.A.; Moore, L.; Young, S.; Moore, D. The association of age and semen quality in healthy men. Hum. Reprod. 2003, 18, 447–454. [Google Scholar] [CrossRef]
- Plas, E.; Berger, P.; Hermann, M.; Pfluger, H. Effects of aging on male fertility? Exp. Gerontol. 2000, 35, 543–551. [Google Scholar] [CrossRef]
- Frattarelli, J.L.; Miller, K.A.; Miller, B.T.; Elkind-Hirsch, K.; Scott, R.T., Jr. Male age negatively impacts embryo development and reproductive outcome in donor oocyte assisted reproductive technology cycles. Fertil. Steril. 2008, 90, 97–103. [Google Scholar] [CrossRef]
- Bellver, J.; Garrido, N.; Remohi, J.; Pellicer, A.; Meseguer, M. Influence of paternal age on assisted reproduction outcome. Reprod. Biomed. Online 2008, 17, 595–604. [Google Scholar] [CrossRef] [PubMed]
- Duran, E.H.; Dowling-Lacey, D.; Bocca, S.; Stadtmauer, L.; Oehninger, S. Impact of male age on the outcome of assisted reproductive technology cycles using donor oocytes. Reprod. Biomed. Online 2010, 20, 848–856. [Google Scholar] [CrossRef]
- Girsh, E.; Katz, N.; Genkin, L.; Girtler, O.; Bocker, J.; Bezdin, S.; Barr, I. Male age influences oocyte-donor program results. J. Assist. Reprod. Genet. 2008, 25, 137–143. [Google Scholar] [CrossRef]
- Begueria, R.; Garcia, D.; Obradors, A.; Poisot, F.; Vassena, R.; Vernaeve, V. Paternal age and assisted reproductive outcomes in ICSI donor oocytes: Is there an effect of older fathers? Hum. Reprod. 2014, 29, 2114–2122. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, R.C.; Braga, D.P.; Bonetti, T.C.; Pasqualotto, F.F.; Iaconelli, A., Jr.; Borges, E., Jr. Negative influence of paternal age on clinical intracytoplasmic sperm injection cycle outcomes in oligozoospermic patients. Fertil. Steril. 2010, 93, 1870–1874. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.M.; Nazroo, J.; O’Connor, D.B.; Blake, M.; Pendleton, N. Sexual Health and Well-being Among Older Men and Women in England: Findings from the English Longitudinal Study of Ageing. Arch. Sex. Behav. 2016, 45, 133–144. [Google Scholar] [CrossRef] [PubMed]
- Kasman, A.M.; Li, S.; Zhao, Q.; Behr, B.; Eisenberg, M.L. Relationship between male age, semen parameters and assisted reproductive technology outcomes. Andrology 2021, 9, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Lai, S.F.; Li, R.H.; Yeung, W.S.; Ng, E.H. Effect of paternal age on semen parameters and live birth rate of in-vitro fertilisation treatment: A retrospective analysis. Hong Kong Med. J. 2018, 24, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Auger, J.; Kunstmann, J.M.; Czyglik, F.; Jouannet, P. Decline in semen quality among fertile men in Paris during the past 20 years. N. Engl. J. Med. 1995, 332, 281–285. [Google Scholar] [CrossRef]
- Veron, G.L.; Tissera, A.D.; Bello, R.; Beltramone, F.; Estofan, G.; Molina, R.I.; Vazquez-Levin, M.H. Impact of age, clinical conditions, and lifestyle on routine semen parameters and sperm kinematics. Fertil. Steril. 2018, 110, 68–75.e64. [Google Scholar] [CrossRef]
- Freour, T.; Jean, M.; Mirallie, S.; Barriere, P. Computer-assisted sperm analysis parameters in young fertile sperm donors and relationship with age. Syst. Biol. Reprod. Med. 2012, 58, 102–106. [Google Scholar] [CrossRef]
- Sloter, E.; Schmid, T.E.; Marchetti, F.; Eskenazi, B.; Nath, J.; Wyrobek, A.J. Quantitative effects of male age on sperm motion. Hum. Reprod. 2006, 21, 2868–2875. [Google Scholar] [CrossRef]
- Baccetti, B.; Renieri, T.; Selmi, M.G.; Soldani, P. Sperm morphogenesis, structure and function in humans over 70 years old. J. Submicrosc. Cytol. 1984, 16, 585–600. [Google Scholar]
- Bastos, P.; Freitas, M.J.; Gomes, A.; Vitorino, R.; Fardilha, M. Unravelling the Power of Omics for the Infertile Aging Male. Curr. Pharm. Des. 2017, 23, 4451–4469. [Google Scholar] [CrossRef]
- Liu, F.J.; Liu, X.; Han, J.L.; Wang, Y.W.; Jin, S.H.; Liu, X.X.; Liu, J.; Wang, W.T.; Wang, W.J. Aged men share the sperm protein PATE1 defect with young asthenozoospermia patients. Hum. Reprod. 2015, 30, 861–869. [Google Scholar] [CrossRef]
- Guo, Y.; Li, J.; Hao, F.; Yang, Y.; Yang, H.; Chang, Q.; Kong, P.; Liu, W.; Jiao, X.; Teng, X. A new perspective on semen quality of aged male: The characteristics of metabolomics and proteomics. Front. Endocrinol. 2022, 13, 1058250. [Google Scholar] [CrossRef]
- Liochev, S.I. Reactive oxygen species and the free radical theory of aging. Free. Radic. Biol. Med. 2013, 60, 1–4. [Google Scholar] [CrossRef]
- Almeida, S.; Rato, L.; Sousa, M.; Alves, M.G.; Oliveira, P.F. Fertility and Sperm Quality in the Aging Male. Curr. Pharm. Des. 2017, 23, 4429–4437. [Google Scholar] [CrossRef]
- Nago, M.; Arichi, A.; Omura, N.; Iwashita, Y.; Kawamura, T.; Yumura, Y. Aging increases oxidative stress in semen. Investig. Clin. Urol. 2021, 62, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Roque, M.; Esteves, S.C. Effect of varicocele repair on sperm DNA fragmentation: A review. Int. Urol. Nephrol. 2018, 50, 583–603. [Google Scholar] [CrossRef]
- Agarwal, A.; Cho, C.L.; Majzoub, A.; Esteves, S.C. The Society for Translational Medicine: Clinical practice guidelines for sperm DNA fragmentation testing in male infertility. Transl. Androl. Urol. 2017, 6, S720–S733. [Google Scholar] [CrossRef]
- Esteves, S.C.; Roque, M.; Bradley, C.K.; Garrido, N. Reproductive outcomes of testicular versus ejaculated sperm for intracytoplasmic sperm injection among men with high levels of DNA fragmentation in semen: Systematic review and meta-analysis. Fertil. Steril. 2017, 108, 456–467.e451. [Google Scholar] [CrossRef] [PubMed]
- Esteves, S.C.; Roque, M.; Garrido, N. Use of testicular sperm for intracytoplasmic sperm injection in men with high sperm DNA fragmentation: A SWOT analysis. Asian J. Androl. 2018, 20, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Nijs, M.; De Jonge, C.; Cox, A.; Janssen, M.; Bosmans, E.; Ombelet, W. Correlation between male age, WHO sperm parameters, DNA fragmentation, chromatin packaging and outcome in assisted reproduction technology. Andrologia 2011, 43, 174–179. [Google Scholar] [CrossRef]
- Garcia-Ferreyra, J.; Luna, D.; Villegas, L.; Romero, R.; Zavala, P.; Hilario, R.; Duenas-Chacon, J. High Aneuploidy Rates Observed in Embryos Derived from Donated Oocytes are Related to Male Aging and High Percentages of Sperm DNA Fragmentation. Clin. Med. Insights Reprod. Health 2015, 9, 21–27. [Google Scholar] [CrossRef]
- Rosiak-Gill, A.; Gill, K.; Jakubik, J.; Fraczek, M.; Patorski, L.; Gaczarzewicz, D.; Kurzawa, R.; Kurpisz, M.; Piasecka, M. Age-related changes in human sperm DNA integrity. Aging 2019, 11, 5399–5411. [Google Scholar] [CrossRef]
- Gonzalez, D.C.; Ory, J.; Blachman-Braun, R.; Nackeeran, S.; Best, J.C.; Ramasamy, R. Advanced Paternal Age and Sperm DNA Fragmentation: A Systematic Review. World J. Men’s Health 2022, 40, 104–115. [Google Scholar] [CrossRef] [PubMed]
- Nikitaras, V.; Zander-Fox, D.; McPherson, N.O. Improving Sperm Oxidative Stress and Embryo Quality in Advanced Paternal Age Using Idebenone In Vitro-A Proof-of-Concept Study. Antioxidants 2021, 10, 1079. [Google Scholar] [CrossRef]
- Kaltsas, A. Oxidative Stress and Male Infertility: The Protective Role of Antioxidants. Medicina 2023, 59, 1769. [Google Scholar] [CrossRef]
- Mishra, S.; Kumar, R.; Malhotra, N.; Singh, N.; Dada, R. Mild oxidative stress is beneficial for sperm telomere length maintenance. World J. Methodol. 2016, 6, 163–170. [Google Scholar] [CrossRef]
- McNally, E.J.; Luncsford, P.J.; Armanios, M. Long telomeres and cancer risk: The price of cellular immortality. J. Clin. Investig. 2019, 129, 3474–3481. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Zhao, F.; Dai, S.; Zhang, N.; Zhao, W.; Bai, R.; Sun, Y. Sperm telomere length is positively associated with the quality of early embryonic development. Hum. Reprod. 2015, 30, 1876–1881. [Google Scholar] [CrossRef]
- Eisenberg, D.T.A.; Kuzawa, C.W. The paternal age at conception effect on offspring telomere length: Mechanistic, comparative and adaptive perspectives. Philos. Trans. R. Soc. B Biol. Sci. 2018, 373, 20160442. [Google Scholar] [CrossRef]
- Andreescu, N.I.; Cosma, M.; Farcas, S.S.; Stoian, M.; Amzar, D.G.; Puiu, M. Assessment of chromosomal aneuploidies in sperm of infertile males by using FISH technique. Rom. J. Morphol. Embryol. 2016, 57, 173–178. [Google Scholar]
- Yatsenko, A.N.; Turek, P.J. Reproductive genetics and the aging male. J. Assist. Reprod. Genet. 2018, 35, 933–941. [Google Scholar] [CrossRef]
- Gunes, S.; Hekim, G.N.; Arslan, M.A.; Asci, R. Effects of aging on the male reproductive system. J. Assist. Reprod. Genet. 2016, 33, 441–454. [Google Scholar] [CrossRef]
- Gao, Z.; Moorjani, P.; Sasani, T.A.; Pedersen, B.S.; Quinlan, A.R.; Jorde, L.B.; Amster, G.; Przeworski, M. Overlooked roles of DNA damage and maternal age in generating human germline mutations. Proc. Natl. Acad. Sci. USA 2019, 116, 9491–9500. [Google Scholar] [CrossRef]
- Cai, Y.; Cao, H.; Wang, F.; Zhang, Y.; Kapranov, P. Complex genomic patterns of abasic sites in mammalian DNA revealed by a high-resolution SSiNGLe-AP method. Nat. Commun. 2022, 13, 5868. [Google Scholar] [CrossRef]
- Evenson, D.P.; Djira, G.; Kasperson, K.; Christianson, J. Relationships between the age of 25,445 men attending infertility clinics and sperm chromatin structure assay (SCSA®) defined sperm DNA and chromatin integrity. Fertil. Steril. 2020, 114, 311–320. [Google Scholar] [CrossRef]
- Donatti, L.M.; Martello, C.L.; Andrade, G.M.; Oliveira, N.P.; Frantz, N. Advanced Paternal Age Affects the Sperm DNA Fragmentation Index and May Lead to Lower Good-quality Blastocysts. Reprod. Sci. 2023, 30, 2489–2494. [Google Scholar] [CrossRef]
- Brandt, N.B.; Kristensen, M.L.S.; Catalini, L.; Fedder, J. Effect of paternal health on pregnancy loss-A review of current evidence. Andrologia 2022, 54, e14259. [Google Scholar] [CrossRef]
- Punjabi, U.; Goovaerts, I.; Peeters, K.; Van Mulders, H.; De Neubourg, D. Sperm as a Carrier of Genome Instability in Relation to Paternal Lifestyle and Nutritional Conditions. Nutrients 2022, 14, 3155. [Google Scholar] [CrossRef]
- Horta, F.; Catt, S.; Ramachandran, P.; Vollenhoven, B.; Temple-Smith, P. Female ageing affects the DNA repair capacity of oocytes in IVF using a controlled model of sperm DNA damage in mice. Hum. Reprod. 2020, 35, 529–544. [Google Scholar] [CrossRef]
- Aitken, R.J. Role of sperm DNA damage in creating de-novo mutations in human offspring: The ’post-meiotic oocyte collusion’ hypothesis. Reprod. Biomed. Online 2022, 45, 109–124. [Google Scholar] [CrossRef] [PubMed]
- Xavier, M.J.; Nixon, B.; Roman, S.D.; Scott, R.J.; Drevet, J.R.; Aitken, R.J. Paternal impacts on development: Identification of genomic regions vulnerable to oxidative DNA damage in human spermatozoa. Hum. Reprod. 2019, 34, 1876–1890. [Google Scholar] [CrossRef] [PubMed]
- Zweifel, J.E.; Woodward, J.T. The risky business of advanced paternal age: Neurodevelopmental and psychosocial implications for children of older fathers. Fertil. Steril. 2022, 118, 1013–1021. [Google Scholar] [CrossRef] [PubMed]
- Frans, E.M.; Sandin, S.; Reichenberg, A.; Lichtenstein, P.; Langstrom, N.; Hultman, C.M. Advancing paternal age and bipolar disorder. Arch. Gen. Psychiatry 2008, 65, 1034–1040. [Google Scholar] [CrossRef]
- Croen, L.A.; Najjar, D.V.; Fireman, B.; Grether, J.K. Maternal and paternal age and risk of autism spectrum disorders. Arch. Pediatr. Adolesc. Med. 2007, 161, 334–340. [Google Scholar] [CrossRef] [PubMed]
- Malaspina, D.; Corcoran, C.; Fahim, C.; Berman, A.; Harkavy-Friedman, J.; Yale, S.; Goetz, D.; Goetz, R.; Harlap, S.; Gorman, J. Paternal age and sporadic schizophrenia: Evidence for de novo mutations. Am. J. Med. Genet. 2002, 114, 299–303. [Google Scholar] [CrossRef]
- Day, K.; Waite, L.L.; Thalacker-Mercer, A.; West, A.; Bamman, M.M.; Brooks, J.D.; Myers, R.M.; Absher, D. Differential DNA methylation with age displays both common and dynamic features across human tissues that are influenced by CpG landscape. Genome Biol. 2013, 14, R102. [Google Scholar] [CrossRef]
- Milekic, M.H.; Xin, Y.; O’Donnell, A.; Kumar, K.K.; Bradley-Moore, M.; Malaspina, D.; Moore, H.; Brunner, D.; Ge, Y.; Edwards, J.; et al. Age-related sperm DNA methylation changes are transmitted to offspring and associated with abnormal behavior and dysregulated gene expression. Mol. Psychiatry 2015, 20, 995–1001. [Google Scholar] [CrossRef] [PubMed]
- Feinberg, J.I.; Schrott, R.; Ladd-Acosta, C.; Newschaffer, C.J.; Hertz-Picciotto, I.; Croen, L.A.; Daniele Fallin, M.; Feinberg, A.P.; Volk, H.E. Epigenetic changes in sperm are associated with paternal and child quantitative autistic traits in an autism-enriched cohort. Mol. Psychiatry 2023, 1–11. [Google Scholar] [CrossRef]
- Menezo, Y.J.; Silvestris, E.; Dale, B.; Elder, K. Oxidative stress and alterations in DNA methylation: Two sides of the same coin in reproduction. Reprod. Biomed. Online 2016, 33, 668–683. [Google Scholar] [CrossRef]
- Liang, K.; Yao, L.; Wang, S.; Zheng, L.; Qian, Z.; Ge, Y.; Chen, L.; Cheng, X.; Ma, R.; Li, C.; et al. miR-125a-5p increases cellular DNA damage of aging males and perturbs stage-specific embryo development via Rbm38-p53 signaling. Aging Cell 2021, 20, e13508. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.; Ghanghas, P.; Kaushal, N.; Kaur, J.; Kaur, P. Epigenetics and oxidative stress: A twin-edged sword in spermatogenesis. Andrologia 2019, 51, e13432. [Google Scholar] [CrossRef] [PubMed]
- Ashapkin, V.; Suvorov, A.; Pilsner, J.R.; Krawetz, S.A.; Sergeyev, O. Age-associated epigenetic changes in mammalian sperm: Implications for offspring health and development. Hum. Reprod. Update 2023, 29, 24–44. [Google Scholar] [CrossRef] [PubMed]
- Kaarouch, I.; Bouamoud, N.; Madkour, A.; Louanjli, N.; Saadani, B.; Assou, S.; Aboulmaouahib, S.; Amzazi, S.; Copin, H.; Benkhalifa, M.; et al. Paternal age: Negative impact on sperm genome decays and IVF outcomes after 40 years. Mol. Reprod. Dev. 2018, 85, 271–280. [Google Scholar] [CrossRef]
- Ghuman, N.K.; Mair, E.; Pearce, K.; Choudhary, M. Does age of the sperm donor influence live birth outcome in assisted reproduction? Hum. Reprod. 2016, 31, 582–590. [Google Scholar] [CrossRef]
- Robertshaw, I.; Khoury, J.; Abdallah, M.E.; Warikoo, P.; Hofmann, G.E. The effect of paternal age on outcome in assisted reproductive technology using the ovum donation model. Reprod. Sci. 2014, 21, 590–593. [Google Scholar] [CrossRef] [PubMed]
- Campos, I.; Gomez, E.; Fernandez-Valencia, A.L.; Landeras, J.; Gonzalez, R.; Coy, P.; Gadea, J. Effects of men and recipients’ age on the reproductive outcome of an oocyte donation program. J. Assist. Reprod. Genet. 2008, 25, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Tiegs, A.W.; Sachdev, N.M.; Grifo, J.A.; McCulloh, D.H.; Licciardi, F. Paternal Age Is Not Associated With Pregnancy Outcomes After Single Thawed Euploid Blastocyst Transfer. Reprod. Sci. 2017, 24, 1319–1324. [Google Scholar] [CrossRef]
- Johnson, S.L.; Zellhuber-McMillan, S.; Gillum, J.; Dunleavy, J.; Evans, J.P.; Nakagawa, S.; Gemmell, N.J. Evidence that fertility trades off with early offspring fitness as males age. Proc. Biol. Sci. 2018, 285, 20172174. [Google Scholar] [CrossRef]
- Hassan, M.A.; Killick, S.R. Effect of male age on fertility: Evidence for the decline in male fertility with increasing age. Fertil. Steril. 2003, 79 (Suppl. S3), 1520–1527. [Google Scholar] [CrossRef]
- Wu, Y.; Kang, X.; Zheng, H.; Liu, H.; Liu, J. Effect of Paternal Age on Reproductive Outcomes of In Vitro Fertilization. PLoS ONE 2015, 10, e0135734. [Google Scholar] [CrossRef]
- Reichenberg, A.; Gross, R.; Weiser, M.; Bresnahan, M.; Silverman, J.; Harlap, S.; Rabinowitz, J.; Shulman, C.; Malaspina, D.; Lubin, G.; et al. Advancing paternal age and autism. Arch. Gen. Psychiatry 2006, 63, 1026–1032. [Google Scholar] [CrossRef]
- Crosnoe, L.E.; Kim, E.D. Impact of age on male fertility. Curr. Opin. Obstet. Gynecol. 2013, 25, 181–185. [Google Scholar] [CrossRef] [PubMed]
- Malaspina, D. Paternal factors and schizophrenia risk: De novo mutations and imprinting. Schizophr. Bull. 2001, 27, 379–393. [Google Scholar] [CrossRef]
- Chapuis, A.; Gala, A.; Ferrieres-Hoa, A.; Mullet, T.; Bringer-Deutsch, S.; Vintejoux, E.; Torre, A.; Hamamah, S. Sperm quality and paternal age: Effect on blastocyst formation and pregnancy rates. Basic Clin. Androl. 2017, 27, 2. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Ferreyra, J.; Hilario, R.; Duenas, J. High percentages of embryos with 21, 18 or 13 trisomy are related to advanced paternal age in donor egg cycles. JBRA Assist. Reprod. 2018, 22, 26–34. [Google Scholar] [CrossRef]
- Wu, Y.; Kang, X.; Zheng, H.; Liu, H.; Huang, Q.; Liu, J. Effect of Paternal Age on Reproductive Outcomes of Intracytoplasmic Sperm Injection. PLoS ONE 2016, 11, e0149867. [Google Scholar] [CrossRef] [PubMed]
- Murugesu, S.; Kasaven, L.S.; Petrie, A.; Vaseekaran, A.; Jones, B.P.; Bracewell-Milnes, T.; Barcroft, J.F.; Grewal, K.J.; Getreu, N.; Galazis, N.; et al. Does advanced paternal age affect outcomes following assisted reproductive technology? A systematic review and meta-analysis. Reprod. Biomed. Online 2022, 45, 283–331. [Google Scholar] [CrossRef]
- Wyrobek, A.J.; Eskenazi, B.; Young, S.; Arnheim, N.; Tiemann-Boege, I.; Jabs, E.W.; Glaser, R.L.; Pearson, F.S.; Evenson, D. Advancing age has differential effects on DNA damage, chromatin integrity, gene mutations, and aneuploidies in sperm. Proc. Natl. Acad. Sci. USA 2006, 103, 9601–9606. [Google Scholar] [CrossRef]
- Khandwala, Y.S.; Baker, V.L.; Shaw, G.M.; Stevenson, D.K.; Lu, Y.; Eisenberg, M.L. Association of paternal age with perinatal outcomes between 2007 and 2016 in the United States: Population based cohort study. BMJ 2018, 363, k4372. [Google Scholar] [CrossRef]
- Meijerink, A.M.; Ramos, L.; Fleischer, K.; Veltman, J.A.; Hendriks, J.C.; Braat, D.D. Influence of paternal age on ongoing pregnancy rate at eight weeks’ gestation in assisted reproduction. Reprod. Biomed. Online 2016, 32, 96–103. [Google Scholar] [CrossRef]
- Setti, A.S.; Braga, D.; Iaconelli Junior, A.; Borges Junior, E. Increasing paternal age and ejaculatory abstinence length negatively influence the intracytoplasmic sperm injection outcomes from egg-sharing donation cycles. Andrology 2020, 8, 594–601. [Google Scholar] [CrossRef]
- Colaco, S.; Sakkas, D. Paternal factors contributing to embryo quality. J. Assist. Reprod. Genet. 2018, 35, 1953–1968. [Google Scholar] [CrossRef]
- McPherson, N.O.; Zander-Fox, D.; Vincent, A.D.; Lane, M. Combined advanced parental age has an additive negative effect on live birth rates-data from 4057 first IVF/ICSI cycles. J. Assist. Reprod. Genet. 2018, 35, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Klonoff-Cohen, H.S.; Natarajan, L. The effect of advancing paternal age on pregnancy and live birth rates in couples undergoing in vitro fertilization or gamete intrafallopian transfer. Am. J. Obstet. Gynecol. 2004, 191, 507–514. [Google Scholar] [CrossRef]
- Nybo Andersen, A.M.; Hansen, K.D.; Andersen, P.K.; Davey Smith, G. Advanced paternal age and risk of fetal death: A cohort study. Am. J. Epidemiol. 2004, 160, 1214–1222. [Google Scholar] [CrossRef] [PubMed]
- du Fosse, N.A.; van der Hoorn, M.P.; van Lith, J.M.M.; le Cessie, S.; Lashley, E. Advanced paternal age is associated with an increased risk of spontaneous miscarriage: A systematic review and meta-analysis. Hum. Reprod. Update 2020, 26, 650–669. [Google Scholar] [CrossRef] [PubMed]
- Tatsumi, T.; Ishida, E.; Tatsumi, K.; Okada, Y.; Saito, T.; Kubota, T.; Saito, H. Advanced paternal age alone does not adversely affect pregnancy or live-birth rates or sperm parameters following intrauterine insemination. Reprod. Med. Biol. 2018, 17, 459–465. [Google Scholar] [CrossRef]
- Stern, J.E.; Luke, B.; Hornstein, M.D.; Cabral, H.; Gopal, D.; Diop, H.; Kotelchuck, M. The effect of father’s age in fertile, subfertile, and assisted reproductive technology pregnancies: A population based cohort study. J. Assist. Reprod. Genet. 2014, 31, 1437–1444. [Google Scholar] [CrossRef]
- Bronet, F.; Martinez, E.; Gaytan, M.; Linan, A.; Cernuda, D.; Ariza, M.; Nogales, M.; Pacheco, A.; San Celestino, M.; Garcia-Velasco, J.A. Sperm DNA fragmentation index does not correlate with the sperm or embryo aneuploidy rate in recurrent miscarriage or implantation failure patients. Hum. Reprod. 2012, 27, 1922–1929. [Google Scholar] [CrossRef]
- Slama, R.; Bouyer, J.; Windham, G.; Fenster, L.; Werwatz, A.; Swan, S.H. Influence of paternal age on the risk of spontaneous abortion. Am. J. Epidemiol. 2005, 161, 816–823. [Google Scholar] [CrossRef] [PubMed]
- Pritts, E.A.; Parker, W.H.; Olive, D.L. Fibroids and infertility: An updated systematic review of the evidence. Fertil. Steril. 2009, 91, 1215–1223. [Google Scholar] [CrossRef] [PubMed]
- Coban, O.; Serdarogullari, M.; Pervaiz, R.; Soykok, A.; Yarkiner, Z.; Bankeroglu, H. Effect of paternal age on assisted reproductive outcomes in ICSI donor cycles. Andrology 2023, 11, 515–522. [Google Scholar] [CrossRef] [PubMed]
- Stabile, L.A.; Mendes, C.M.; Goissis, M.D.; Sousa, R.G.B.; Nichi, M.; Visintin, J.A.; Hamilton, T.; Assumpcao, M. Paternal age impairs in vitro embryo and in vivo fetal development in murine. Sci. Rep. 2022, 12, 13031. [Google Scholar] [CrossRef] [PubMed]
- Setti, A.S.; Braga, D.; Provenza, R.R.; Iaconelli, A., Jr.; Borges, E., Jr. Oocyte ability to repair sperm DNA fragmentation: The impact of maternal age on intracytoplasmic sperm injection outcomes. Fertil. Steril. 2021, 116, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Green, R.F.; Devine, O.; Crider, K.S.; Olney, R.S.; Archer, N.; Olshan, A.F.; Shapira, S.K.; The National Birth Defects Prevention Study. Association of paternal age and risk for major congenital anomalies from the National Birth Defects Prevention Study, 1997 to 2004. Ann. Epidemiol. 2010, 20, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Basso, O.; Wilcox, A.J. Paternal age and delivery before 32 weeks. Epidemiology 2006, 17, 475–478. [Google Scholar] [CrossRef] [PubMed]
- El Rafei, R.; Ghandour, L.; Assaf, G.; Charafeddine, L.; Al Bizri, A.; Alameh, M.; Yunis, K.; National Collaborative Perinatal National Collaborative Perinatal Neonatal Network, American University of Beirut, Lebanon. Children born to mothers in their 20s and fathers in their 40s: Evidence for an increased low birth weight and Cesarean Section deliveries in Lebanon. Ann. Epidemiol. 2018, 28, 368–371. [Google Scholar] [CrossRef] [PubMed]
- Urhoj, S.K.; Andersen, P.K.; Mortensen, L.H.; Davey Smith, G.; Nybo Andersen, A.M. Advanced paternal age and stillbirth rate: A nationwide register-based cohort study of 944,031 pregnancies in Denmark. Eur. J. Epidemiol. 2017, 32, 227–234. [Google Scholar] [CrossRef]
- Mayo, J.A.; Lu, Y.; Stevenson, D.K.; Shaw, G.M.; Eisenberg, M.L. Parental age and stillbirth: A population-based cohort of nearly 10 million California deliveries from 1991 to 2011. Ann. Epidemiol. 2019, 31, 32–37.e32. [Google Scholar] [CrossRef]
- Alio, A.P.; Salihu, H.M.; McIntosh, C.; August, E.M.; Weldeselasse, H.; Sanchez, E.; Mbah, A.K. The effect of paternal age on fetal birth outcomes. Am. J. Men’s Health 2012, 6, 427–435. [Google Scholar] [CrossRef]
- Rossen, J.; Klungsoyr, K.; Albrechtsen, S.; Lokkegard, E.; Rasmussen, S.; Bergholt, T.; Skjeldestad, F.E. Can oxytocin augmentation modify the risk of epidural analgesia by maternal age in cesarean sections? Acta Obstet Gynecol. Scand. 2018, 97, 872–879. [Google Scholar] [CrossRef] [PubMed]
- Bernhardt, L.; Dittrich, M.; Prell, A.; Potabattula, R.; Drummer, C.; Behr, R.; Hahn, T.; Schorsch, M.; Muller, T.; Haaf, T. Age-related methylation changes in the human sperm epigenome. Aging 2023, 15, 1257–1278. [Google Scholar] [CrossRef]
- Park, Y.S.; Lee, S.H.; Lim, C.K.; Choi, H.W.; An, J.H.; Park, C.W.; Lee, H.S.; Lee, J.S.; Seo, J.T. Paternal age as an independent factor does not affect embryo quality and pregnancy outcomes of testicular sperm extraction-intracytoplasmic sperm injection in azoospermia. Andrologia 2018, 50, e12864. [Google Scholar] [CrossRef]
- Mathieu, C.; Ecochard, R.; Bied, V.; Lornage, J.; Czyba, J.C. Cumulative conception rate following intrauterine artificial insemination with husband’s spermatozoa: Influence of husband’s age. Hum. Reprod. 1995, 10, 1090–1097. [Google Scholar] [CrossRef]
- Gu, L.; Zhang, H.; Yin, L.; Bu, Z.; Zhu, G. Effect of male age on the outcome of in vitro fertilization: Oocyte donation as a model. J. Assist. Reprod. Genet. 2012, 29, 331–334. [Google Scholar] [CrossRef]
- Tsai, Y.R.; Lan, K.C.; Kung, F.T.; Lin, P.Y.; Chiang, H.J.; Lin, Y.J.; Huang, F.J. The effect of advanced paternal age on the outcomes of assisted reproductive techniques among patients with azoospermia using cryopreserved testicular spermatozoa. Taiwan J. Obstet. Gynecol. 2013, 52, 351–355. [Google Scholar] [CrossRef] [PubMed]
- Whitcomb, B.W.; Turzanski-Fortner, R.; Richter, K.S.; Kipersztok, S.; Stillman, R.J.; Levy, M.J.; Levens, E.D. Contribution of male age to outcomes in assisted reproductive technologies. Fertil. Steril. 2011, 95, 147–151. [Google Scholar] [CrossRef]
- Tesarik, J.; Greco, E.; Mendoza, C. Late, but not early, paternal effect on human embryo development is related to sperm DNA fragmentation. Hum. Reprod. 2004, 19, 611–615. [Google Scholar] [CrossRef]
- Kim, S.; Kim, M.; Oh, M.Y.; Seo, Y.; Yum, S.K. Impact of increased paternal age on neonatal outcomes in very-low-birth-weight infants. J. Matern.-Fetal Neonatal Med. 2023, 36, 2257836. [Google Scholar] [CrossRef]
- Bu, X.; Ye, W.; Zhou, J. Paternal age, risk of congenital anomalies, and birth outcomes: A population-based cohort study. Eur. J. Pediatr. 2023, 182, 3519–3526. [Google Scholar] [CrossRef] [PubMed]
- Liu, K.; Case, A.; Cheung, A.P.; Sierra, S.; AlAsiri, S.; Carranza-Mamane, B.; Dwyer, C.; Graham, J.; Havelock, J.; Hemmings, R.; et al. RETIRED: Advanced reproductive age and fertility. J. Obstet. Gynaecol. Can. 2011, 33, 1165–1175. [Google Scholar] [CrossRef]
- Toriello, H.V.; Meck, J.M.; Professional Practice and Guidelines Committee. Statement on guidance for genetic counseling in advanced paternal age. Genet. Med. 2008, 10, 457–460. [Google Scholar] [CrossRef] [PubMed]
- Kaltsas, A.; Zikopoulos, A.; Moustakli, E.; Zachariou, A.; Tsirka, G.; Tsiampali, C.; Palapela, N.; Sofikitis, N.; Dimitriadis, F. The Silent Threat to Women’s Fertility: Uncovering the Devastating Effects of Oxidative Stress. Antioxidants 2023, 12, 1490. [Google Scholar] [CrossRef] [PubMed]
- Halliwell, B. The antioxidant paradox. Lancet 2000, 355, 1179–1180. [Google Scholar] [CrossRef] [PubMed]
- Symeonidis, E.N.; Evgeni, E.; Palapelas, V.; Koumasi, D.; Pyrgidis, N.; Sokolakis, I.; Hatzichristodoulou, G.; Tsiampali, C.; Mykoniatis, I.; Zachariou, A.; et al. Redox Balance in Male Infertility: Excellence through Moderation—“Muepsilontaurhoomicronnu ἄrhoiotasigmatauomicronnu”. Antioxidants 2021, 10, 1534. [Google Scholar] [CrossRef]
- Bertoncelli Tanaka, M.; Agarwal, A.; Esteves, S.C. Paternal age and assisted reproductive technology: Problem solver or trouble maker? Panminerva Medica 2019, 61, 138–151. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, E.T.; Steele, E.K.; McClure, N.; Lewis, S.E. Assessment of DNA integrity and morphology of ejaculated spermatozoa from fertile and infertile men before and after cryopreservation. Hum. Reprod. 2001, 16, 1191–1199. [Google Scholar] [CrossRef]
- Jennings, M.O.; Owen, R.C.; Keefe, D.; Kim, E.D. Management and counseling of the male with advanced paternal age. Fertil. Steril. 2017, 107, 324–328. [Google Scholar] [CrossRef]
- Munne, S.; Sandalinas, M.; Escudero, T.; Velilla, E.; Walmsley, R.; Sadowy, S.; Cohen, J.; Sable, D. Improved implantation after preimplantation genetic diagnosis of aneuploidy. Reprod. Biomed. Online 2003, 7, 91–97. [Google Scholar] [CrossRef]
- Staessen, C.; Verpoest, W.; Donoso, P.; Haentjens, P.; Van der Elst, J.; Liebaers, I.; Devroey, P. Preimplantation genetic screening does not improve delivery rate in women under the age of 36 following single-embryo transfer. Hum. Reprod. 2008, 23, 2818–2825. [Google Scholar] [CrossRef] [PubMed]
- Kaltsas, A.; Dimitriadis, F.; Zachariou, D.; Zikopoulos, A.; Symeonidis, E.N.; Markou, E.; Tien, D.M.B.; Takenaka, A.; Sofikitis, N.; Zachariou, A. From Diagnosis to Treatment: Comprehensive Care by Reproductive Urologists in Assisted Reproductive Technology. Medicina 2023, 59, 1835. [Google Scholar] [CrossRef] [PubMed]
- Marinaro, J.; Goldstein, M. Microsurgical Management of Male Infertility: Compelling Evidence That Collaboration with Qualified Male Reproductive Urologists Enhances Assisted Reproductive Technology (ART) Outcomes. J. Clin. Med. 2022, 11, 4593. [Google Scholar] [CrossRef] [PubMed]
- Stein, L.J.; Rosner, S.; Lo Giudice, A.; Ditzen, B.; Wischmann, T. Analysing medical predictors for the outcome of infertility treatment: A 5-year follow-up survey. Arch. Gynecol. Obstet. 2023, 308, 1007–1014. [Google Scholar] [CrossRef] [PubMed]
- Atsem, S.; Reichenbach, J.; Potabattula, R.; Dittrich, M.; Nava, C.; Depienne, C.; Bohm, L.; Rost, S.; Hahn, T.; Schorsch, M.; et al. Paternal age effects on sperm FOXK1 and KCNA7 methylation and transmission into the next generation. Hum. Mol. Genet. 2016, 25, 4996–5005. [Google Scholar] [CrossRef]
- Yi, H.; Yang, M.; Tang, H.; Lin, M. Risk Factors of Pregnancy Failure in Infertile Patients Undergoing Assisted Reproductive Technology. Int. J. Gen. Med. 2022, 15, 8807–8817. [Google Scholar] [CrossRef]
| Aspects of Paternal Aging | Impact on ART Outcomes | Mitigation Strategies |
|---|---|---|
| Semen Quality |
|
|
| Genetic Risks |
|
|
| Epigenetic Shifts |
|
|
| Psychological Aspects |
|
|
| Impact on Embryo and Birth Outcomes |
|
|
| Long-Term Offspring Health |
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaltsas, A.; Zikopoulos, A.; Vrachnis, D.; Skentou, C.; Symeonidis, E.N.; Dimitriadis, F.; Stavros, S.; Chrisofos, M.; Sofikitis, N.; Vrachnis, N.; et al. Advanced Paternal Age in Focus: Unraveling Its Influence on Assisted Reproductive Technology Outcomes. J. Clin. Med. 2024, 13, 2731. https://doi.org/10.3390/jcm13102731
Kaltsas A, Zikopoulos A, Vrachnis D, Skentou C, Symeonidis EN, Dimitriadis F, Stavros S, Chrisofos M, Sofikitis N, Vrachnis N, et al. Advanced Paternal Age in Focus: Unraveling Its Influence on Assisted Reproductive Technology Outcomes. Journal of Clinical Medicine. 2024; 13(10):2731. https://doi.org/10.3390/jcm13102731
Chicago/Turabian StyleKaltsas, Aris, Athanasios Zikopoulos, Dionysios Vrachnis, Chara Skentou, Evangelos N. Symeonidis, Fotios Dimitriadis, Sofoklis Stavros, Michael Chrisofos, Nikolaos Sofikitis, Nikolaos Vrachnis, and et al. 2024. "Advanced Paternal Age in Focus: Unraveling Its Influence on Assisted Reproductive Technology Outcomes" Journal of Clinical Medicine 13, no. 10: 2731. https://doi.org/10.3390/jcm13102731
APA StyleKaltsas, A., Zikopoulos, A., Vrachnis, D., Skentou, C., Symeonidis, E. N., Dimitriadis, F., Stavros, S., Chrisofos, M., Sofikitis, N., Vrachnis, N., & Zachariou, A. (2024). Advanced Paternal Age in Focus: Unraveling Its Influence on Assisted Reproductive Technology Outcomes. Journal of Clinical Medicine, 13(10), 2731. https://doi.org/10.3390/jcm13102731









