Accuracy Analysis of the Multiparametric Acoustic Voice Indices, the VWI, AVQI, ABI, and DSI Measures, in Differentiating between Normal and Dysphonic Voices
Abstract
:1. Introduction
2. Materials and Methods
2.1. Glottal Function Index Questionnaire
2.2. Voice Recordings
2.3. DSI Estimation
2.4. AVQI Estimation
2.5. ABI Estimation
2.6. VWI Estimation
2.7. Statistical Analysis
3. Results
3.1. Study Group
3.2. MAVI Evaluation Outcomes
3.3. Normal vs. Pathological Voice Diagnostic Accuracy of the Investigated MAVI
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lechien, J.R.; Geneid, A.; Bohlender, J.E.; Cantarella, G.; Avellaneda, J.C.; Desuter, G.; Sjogren, E.V.; Finck, C.; Hans, S.; Hess, M.; et al. Consensus for voice quality assessment in clinical practice: Guidelines of the European Laryngological Society and Union of the European Phoniatricians. Eur. Arch. Otorhinolaryngol. 2023, 280, 5459–5473. [Google Scholar] [CrossRef] [PubMed]
- Patel, R.R.; Awan, S.N.; Barkmeier-Kraemer, J.; Courey, M.; Deliyski, D.; Eadie, T.; Paul, D.; Švec, J.G.; Hillman, R. Recommended Protocols for Instrumental Assessment of Voice: American Speech-Language-Hearing Association Expert Panel to Develop a Protocol for Instrumental Assessment of Vocal Function. Am. J. Speech Lang. Pathol. 2018, 27, 887–905. [Google Scholar] [CrossRef] [PubMed]
- Maryn, Y.; Roy, N.; De Bodt, M.; Van Cauwenberge, P.; Corthals, P. Acoustic measurement of overall voice quality: A meta-analysis. J. Acoust. Soc. Am. 2009, 126, 2619–2634. [Google Scholar] [CrossRef] [PubMed]
- Latoszek, B.B.V.; Maryn, Y.; Gerrits, E.; De Bodt, M. A Meta-Analysis: Acoustic Measurement of Roughness and Breathiness. J. Speech Lang. Hear. Res. 2018, 61, 298–323. [Google Scholar] [CrossRef] [PubMed]
- Narasimhan, S.V.; Rashmi, R. Multiparameter Voice Assessment in Dysphonics: Correlation Between Objective and Perceptual Parameters. J. Voice 2022, 36, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Maryn, Y.; Weenink, D. Objective dysphonia measures in the program Praat: Smoothed cepstral peak prominence and acoustic voice quality index. J. Voice 2015, 29, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Awan, S.N.; Roy, N.; Zhang, D.; Cohen, S.M. Validation of the Cepstral Spectral Index of Dysphonia (CSID) as a Screening Tool for Voice Disorders: Development of Clinical Cutoff Scores. J. Voice 2016, 30, 130–144. [Google Scholar] [CrossRef] [PubMed]
- Murton, O.; Hillman, R.; Mehta, D. Cepstral Peak Prominence Values for Clinical Voice Evaluation. Am. J. Speech Lang. Pathol. 2020, 29, 1596–1607. [Google Scholar] [CrossRef]
- Wuyts, F.L.; De Bodt, M.S.; Molenberghs, G.; Remacle, M.; Heylen, L.; Millet, B.; Van Lierde, K.; Raes, J.; Van de Heyning, P.H. The dysphonia severity index: An objective measure of vocal quality based on a multiparameter approach. J. Speech Lang. Hear. Res. 2000, 43, 796–809. [Google Scholar] [CrossRef]
- Salmen, T.; Ermakova, T.; Möller, A.; Seipelt, M.; Weikert, S.; Rummich, J.; Gross, M.; Nawka, T.; Caffier, P.P. The Value of Vocal Extent Measure (VEM) Assessing Phonomicrosurgical Outcomes in Vocal Fold Polyps. J. Voice 2017, 31, 114.e7–114.e15. [Google Scholar] [CrossRef]
- Song, W.; Caffier, F.; Nawka, T.; Ermakova, T.; Martin, A.; Mürbe, D.; Caffier, P.P. T1a Glottic Cancer: Advances in Vocal Outcome Assessment after Transoral CO2-Laser Microsurgery Using the VEM. J. Clin. Med. 2021, 10, 1250. [Google Scholar] [CrossRef]
- Wu, P.; Klein, L.; Rozema, Z.; Haderlein, N.; Cai, J.; Scholp, A.; Xu, X.; Jiang, J.J.; Zhuang, P. The Influence of Voice Training on Vocal Learner’s Objective Acoustic Voice Components. J. Voice 2023, 37, 355–361. [Google Scholar] [CrossRef]
- Aghadoost, S.; Jalaie, S.; Dabirmoghaddam, P.; Khoddami, S.M. Effect of Muscle Tension Dysphonia on Self-perceived Voice Handicap and Multiparametric Measurement and Their Relation in Female Teachers. J. Voice 2022, 36, 68–75. [Google Scholar] [CrossRef]
- Ataee, E.; Khoramshahi, H.; Naderifar, E.; Dastoorpour, M. Relation Between Dysphonia Severity Index (DSI) and Consensus Auditory-Perceptual Evaluation of Voice (CAPE-V). J. Voice 2022, 36, 435.e1–435.e14. [Google Scholar] [CrossRef]
- Graf, S.; Kirschstein, L.; Knopf, A.; Mansour, N.; Jeleff-Wölfler, O.; Buchberger, A.M.S.; Hofauer, B. Systematic evaluation of laryngeal impairment in Sjögren’s syndrome. Eur. Arch. Otorhinolaryngol. 2021, 278, 2421–2428. [Google Scholar] [CrossRef]
- Nasrin, S.; Ali, D.; Jamshid, J.; Hamed, G.; Bashir, R.; Hamide, G. The effects of Cricothyroid Visor Maneuver (CVM) therapy on the voice characteristics of patients with muscular tension dysphonia: A Case Series Study. J. Voice 2022, in press. [Google Scholar] [CrossRef]
- D’haeseleer, E.; Papeleu, T.; Leyns, C.; Adriaansen, A.; Meerschman, I.; Tomassen, P. Voice Outcome of Glottoplasty in Trans Women. J. Voice 2023, in press. [Google Scholar] [CrossRef]
- Hussein Gaber, A.G.; Liang, F.; Yang, J.; Wang, Y.; Zheng, Y. Correlation among the dysphonia severity index (DSI), the RBH voice perceptual evaluation, and minimum glottal area in female patients with vocal fold nodules. J. Voice 2014, 28, 20–23. [Google Scholar] [CrossRef]
- Nemr, K.; Simões-Zenari, M.; de Souza, G.S.; Hachiya, A.; Tsuji, D.H. Correlation of the Dysphonia Severity Index (DSI), Consensus Auditory-Perceptual Evaluation of Voice (CAPE-V), and Gender in Brazilians with and Without Voice Disorders. J. Voice 2016, 30, 765.e7–765.e11. [Google Scholar] [CrossRef]
- Mansouri, Y.; Naderifar, E.; Hajiyakhchali, A.; Moradi, N. The Relationship Between Dysphonia Severity Index and Voice-Related Quality of Life in the Elementary School Teachers with Voice Complaint. J. Voice 2023, 37, 466.e35–466.e39. [Google Scholar] [CrossRef]
- Uloza, V.; Barsties VL, B.; Ulozaite, N.; Petrauskas, T.; Maryn, Y. A comparison of Dysphonia Severity Index and Acoustic Voice Quality Index measures in differentiating normal and dysphonic voices. Eur. Arch. Otorhinolaryngol. 2018, 275, 949–958. [Google Scholar] [CrossRef]
- Goy, H.; Fernandes, D.N.; Pichora-Fuller, M.K.; van Lieshout, P. Normative voice data for younger and older adults. J. Voice 2013, 27, 545–555. [Google Scholar] [CrossRef] [PubMed]
- Maruthy, S.; Ravibabu, P. Comparison of dysphonia severity index between younger and older carnatic classical singers and nonsingers. J. Voice 2015, 29, 65–70. [Google Scholar] [CrossRef] [PubMed]
- Barsties V Latoszek, B.; Ulozaitė-Stanienė, N.; Maryn, Y.; Petrauskas, T.; Uloza, V. The Influence of Gender and Age on the Acoustic Voice Quality Index and Dysphonia Severity Index: A Normative Study. J. Voice 2019, 33, 340–345. [Google Scholar] [CrossRef] [PubMed]
- Sobol, M.; Sielska-Badurek, E.M. The Dysphonia Severity Index (DSI)-Normative Values. Systematic Review and Meta-Analysis. J. Voice 2022, 36, 143.e9–143.e13. [Google Scholar] [CrossRef]
- Maryn, Y.; De Bodt, M.; Roy, N. The Acoustic Voice Quality Index: Toward improved treatment outcomes assessment in voice disorders. J. Commun. Disord. 2010, 43, 161–174. [Google Scholar] [CrossRef]
- Kankare, E.; Barsties V Latoszek, B.; Maryn, Y.; Asikainen, M.; Rorarius, E.; Vilpas, S.; Ilomäki, I.; Tyrmi, J.; Rantala, L.; Laukkanen, A. The acoustic voice quality index version 02.02 in the Finnish-speaking population. Logoped. Phoniatr. Vocol. 2020, 45, 49–56. [Google Scholar] [CrossRef]
- Lehnert, B.; Herold, J.; Blaurock, M.; Busch, C. Reliability of the Acoustic Voice Quality Index AVQI and the Acoustic Breathiness Index (ABI) when wearing CoViD-19 protective masks. Eur. Arch. Otorhinolaryngol. 2022, 279, 4617–4621. [Google Scholar] [CrossRef]
- Shabnam, S.; Pushpavathi, M.; Gopi Sankar, R.; Sridharan, K.V.; Vasanthalakshmi, M.S. A Comprehensive Application for Grading Severity of Voice Based on Acoustic Voice Quality Index v.02.03. J. Voice 2022, in press. [Google Scholar] [CrossRef]
- Penido, F.A.; Gama, A.C.C. Accuracy Analysis of the Multiparametric Acoustic Indices AVQI, ABI, and DSI for Speech-Language Pathologist Decision-Making. J. Voice 2023, in press. [Google Scholar] [CrossRef]
- Jayakumar, T.; Benoy, J.J.; Yasin, H.M. Effect of Age and Gender on Acoustic Voice Quality Index Across Lifespan: A Cross-sectional Study in Indian Population. J. Voice 2022, 36, 436.e1–436.e8. [Google Scholar] [CrossRef]
- Batthyany, C.; Latoszek, B.B.V.; Maryn, Y. Meta-Analysis on the Validity of the Acoustic Voice Quality Index. J. Voice 2022, in press. [Google Scholar] [CrossRef] [PubMed]
- Saeedi, S.; Aghajanzadeh, M.; Khatoonabadi, A.R. A Literature Review of Voice Indices Available for Voice Assessment. J. Rehabil. Sci. Res. 2022, 9, 151–155. [Google Scholar] [CrossRef]
- Barsties V Latoszek, B.; Maryn, Y.; Gerrits, E.; De Bodt, M. The Acoustic Breathiness Index (ABI): A Multivariate Acoustic Model for Breathiness. J. Voice 2017, 31, 511.e11–511.e27. [Google Scholar] [CrossRef] [PubMed]
- Gierlich, J.; Latoszek, B.B.V. Test-Retest Reliability of the Acoustic Voice Quality Index and the Acoustic Breathiness Index. J. Voice 2023, in press. [Google Scholar] [CrossRef] [PubMed]
- Hosokawa, K.; Barsties, V.; Latoszek, B.; Ferrer-Riesgo, C.A.; Iwahashi, M.; Iwaki, S.; Kato, C.; Yoshida, M.; Umatani, M.; Miyauchi, A.; et al. Acoustic Breathiness Index for the Japanese-Speaking Population: Validation Study and Exploration of Affecting Factors. J. Speech Lang. Hear. Res. 2019, 62, 2617–2631. [Google Scholar] [CrossRef] [PubMed]
- Latoszek, B.B.V.; Mathmann, P.; Neumann, K. The cepstral spectral index of dysphonia, the acoustic voice quality index and the acoustic breathiness index as novel multiparametric indices for acoustic assessment of voice quality. Curr. Opin. Otolaryngol. Head Neck Surg. 2021, 29, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Barsties V Latoszek, B.; Kim, G.; Delgado Hernández, J.; Hosokawa, K.; Englert, M.; Neumann, K.; Hetjens, S. The validity of the Acoustic Breathiness Index in the evaluation of breathy voice quality: A Meta-Analysis. Clin. Otolaryngol. 2021, 46, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Uloza, V.; Ulozaite-Staniene, N.; Pertrauskas, T.; Uloziene, I.; Pribuisis, K.; Blažauskas, T.; Damaševičius, R.; Maskeliūnas, R. Smartphone-based Voice Wellness Index application for dysphonia screening and assessment: Development and reliability. J. Voice 2023, in press. [Google Scholar] [CrossRef]
- Bach, K.K.; Belafsky, P.C.; Wasylik, K.; Postma, G.N.; Koufman, J.A. Validity and reliability of the glottal function index. Arch. Otolaryngol. Head Neck Surg. 2005, 131, 961–964. [Google Scholar] [CrossRef]
- Cohen, J.T.; Oestreicher-Kedem, Y.; Fliss, D.M.; DeRowe, A. Glottal function index: A predictor of glottal disorders in children. Ann. Otol. Rhinol. Laryngol. 2007, 116, 81–84. [Google Scholar] [CrossRef]
- Ulozaite-Staniene, N.; Petrauskas, T.; Šaferis, V.; Uloza, V. Exploring the feasibility of the combination of acoustic voice quality index and glottal function index for voice pathology screening. Eur. Arch. Otorhinolaryngol. 2019, 276, 1737–1745. [Google Scholar] [CrossRef]
- Barsties V Latoszek, B.; Ulozaitė-Stanienė, N.; Petrauskas, T.; Uloza, V.; Maryn, Y. Diagnostic Accuracy of Dysphonia Classification of DSI and AVQI. Laryngoscope 2019, 129, 692–698. [Google Scholar] [CrossRef]
- McHugh, M.L. Multiple comparison analysis testing in ANOVA. Biochem. Med. 2011, 21, 203–209. [Google Scholar] [CrossRef]
- Hanley, J.A.; McNeil, B.J. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 1982, 143, 29–36. [Google Scholar] [CrossRef]
- Dollaghan, C.A. The Handbook for Evidence-Based Practice in Communication Disorders; Paul H. Brookes Pub.: Baltimore, MD, USA, 2007; Available online: https://worldcat.org/title/608392915 (accessed on 11 October 2023).
- Lopes, L.W.; da Silva, J.D.; Simões, L.B.; Evangelista, D.d.S.; Silva, P.O.C.; Almeida, A.A.; de Lima-Silva, M.F.B. Relationship Between Acoustic Measurements and Self-evaluation in Patients with Voice Disorders. J. Voice 2017, 31, 119.e1–119.e10. [Google Scholar] [CrossRef]
- Grillo, E.U.; Wolfberg, J. An Assessment of Different Praat Versions for Acoustic Measures Analyzed Automatically by VoiceEvalU8 and Manually by Two Raters. J. Voice 2023, 37, 17–25. [Google Scholar] [CrossRef]
- Uloza, V.; Ulozaite-Staniene, N.; Petrauskas, T. An iOS-based VoiceScreen application: Feasibility for use in clinical settings-a pilot study. Eur. Arch. Otorhinolaryngol. 2023, 280, 277–284. [Google Scholar] [CrossRef]
- Barsties V Latoszek, B.; Mayer, J.; Watts, C.R.; Lehnert, B. Advances in Clinical Voice Quality Analysis with VOXplot. J. Clin. Med. 2023, 12, 4644. [Google Scholar] [CrossRef]
| Diagnosis | n | Age | |
|---|---|---|---|
| Mean | SD | ||
| Normal voice | 49 | 31.69 | 9.89 |
| Mass lesions of the vocal folds (vocal fold polyp, nodules, cyst, granuloma) | 49 | 44.39 | 12.4 |
| Vocal fold cancer (T1-2N0M0) | 11 | 65.09 | 7.71 |
| Chronic hyperplastic laryngitis | 10 | 55.9 | 7.34 |
| Unilateral vocal fold paralysis | 6 | 40.83 | 12.77 |
| Bilateral vocal fold paralysis | 4 | 52.75 | 12.61 |
| Total | 129 | 42.32 | 14.83 |
| MAVI | Voice Group | n | F | Mean | Std. Deviation | p |
|---|---|---|---|---|---|---|
| Acoustic Breathiness Index | Normal voice | 49 | 18.59 | 3.28 | 1.17 | 0.01 |
| Pathological | 80 | 5.33 | 2.08 | |||
| Dysphonia Severity Index | Normal | 49 | 0.03 | 6.28 | 2.22 | 0.01 |
| Pathological | 80 | −0.49 | 5.83 | |||
| Acoustic Voice Quality Index | Normal | 49 | 30.78 | 2.09 | 0.77 | 0.01 |
| Pathological | 80 | 4.26 | 1.80 | |||
| Voice Wellness Index | Normal | 49 | 35.41 | 2.53 | 1.14 | 0.01 |
| Pathological | 80 | 9.29 | 3.01 |
| MAVI | Acoustic Breathiness Index | Dysphonia Severity Index | Acoustic Voice Quality Index | Voice Wellness Index |
|---|---|---|---|---|
| Acoustic Breathiness Index | 1 | 0.45 * | 0.88 * | 0.72 * |
| Dysphonia Severity Index | 0.45 * | 1 | 0.56 * | 0.54 * |
| Acoustic Voice Quality Index | 0.88 * | 0.56 * | 1 | 0.76 * |
| Voice Wellness Index | 0.72 * | 0.54 * | 0.76 * | 1 |
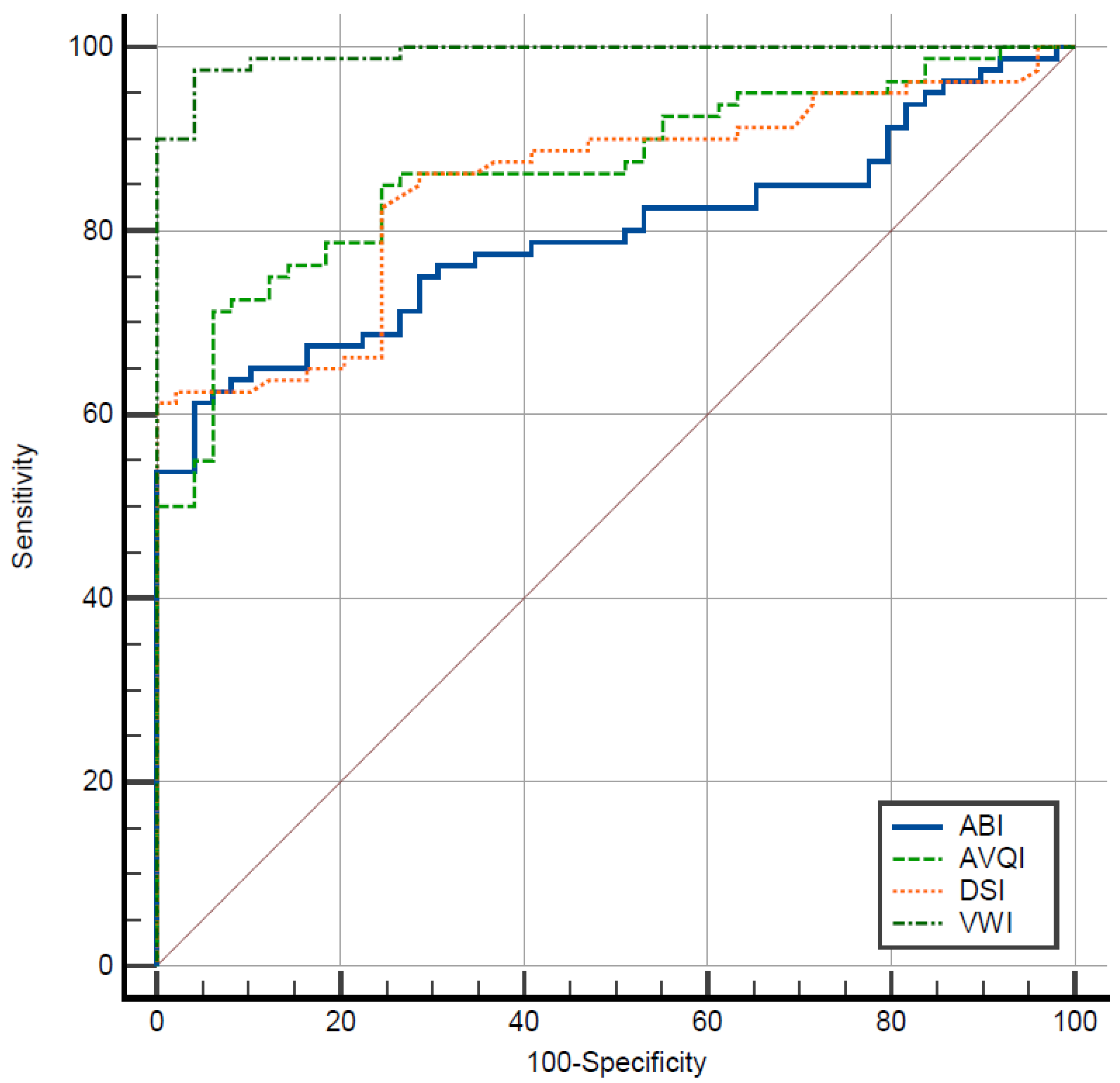
| MAVI | AUC | Cut-off | Sensitivity % | Specificity % | Youden-Index J |
|---|---|---|---|---|---|
| Acoustic Breathiness Index | 0.80 | 4.87 | 61.25 | 95.92 | 0.57 |
| Dysphonia Severity Index | 0.85 | −4.3 | 61.25 | 100 | 0.61 |
| Acoustic Voice Quality Index | 0.87 | 3.27 | 71.25 | 93.88 | 0.65 |
| Voice Wellness Index | 0.99 | 4.45 | 97.50 | 95.92 | 0.93 |
| MAVI | Acoustic Breathiness Index | Dysphonia Severity Index | Acoustic Voice Quality Index | Voice Wellness Index |
|---|---|---|---|---|
| Acoustic Breathiness Index | - | 0.053 | 0.073 * | 0.198 * |
| Dysphonia Severity Index | 0.053 | - | 0.02 | 0.145 * |
| Acoustic Voice Quality Index | 0.073 * | 0.02 | - | 0.125 * |
| Voice Wellness Index | 0.198 * | 0.145 * | 0.125 * | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Uloza, V.; Pribuišis, K.; Ulozaite-Staniene, N.; Petrauskas, T.; Damaševičius, R.; Maskeliūnas, R. Accuracy Analysis of the Multiparametric Acoustic Voice Indices, the VWI, AVQI, ABI, and DSI Measures, in Differentiating between Normal and Dysphonic Voices. J. Clin. Med. 2024, 13, 99. https://doi.org/10.3390/jcm13010099
Uloza V, Pribuišis K, Ulozaite-Staniene N, Petrauskas T, Damaševičius R, Maskeliūnas R. Accuracy Analysis of the Multiparametric Acoustic Voice Indices, the VWI, AVQI, ABI, and DSI Measures, in Differentiating between Normal and Dysphonic Voices. Journal of Clinical Medicine. 2024; 13(1):99. https://doi.org/10.3390/jcm13010099
Chicago/Turabian StyleUloza, Virgilijus, Kipras Pribuišis, Nora Ulozaite-Staniene, Tadas Petrauskas, Robertas Damaševičius, and Rytis Maskeliūnas. 2024. "Accuracy Analysis of the Multiparametric Acoustic Voice Indices, the VWI, AVQI, ABI, and DSI Measures, in Differentiating between Normal and Dysphonic Voices" Journal of Clinical Medicine 13, no. 1: 99. https://doi.org/10.3390/jcm13010099
APA StyleUloza, V., Pribuišis, K., Ulozaite-Staniene, N., Petrauskas, T., Damaševičius, R., & Maskeliūnas, R. (2024). Accuracy Analysis of the Multiparametric Acoustic Voice Indices, the VWI, AVQI, ABI, and DSI Measures, in Differentiating between Normal and Dysphonic Voices. Journal of Clinical Medicine, 13(1), 99. https://doi.org/10.3390/jcm13010099






