Oral Health Statuses of Children and Young Adults with Autism Spectrum Disorder: An Umbrella Review
Abstract
:1. Introduction
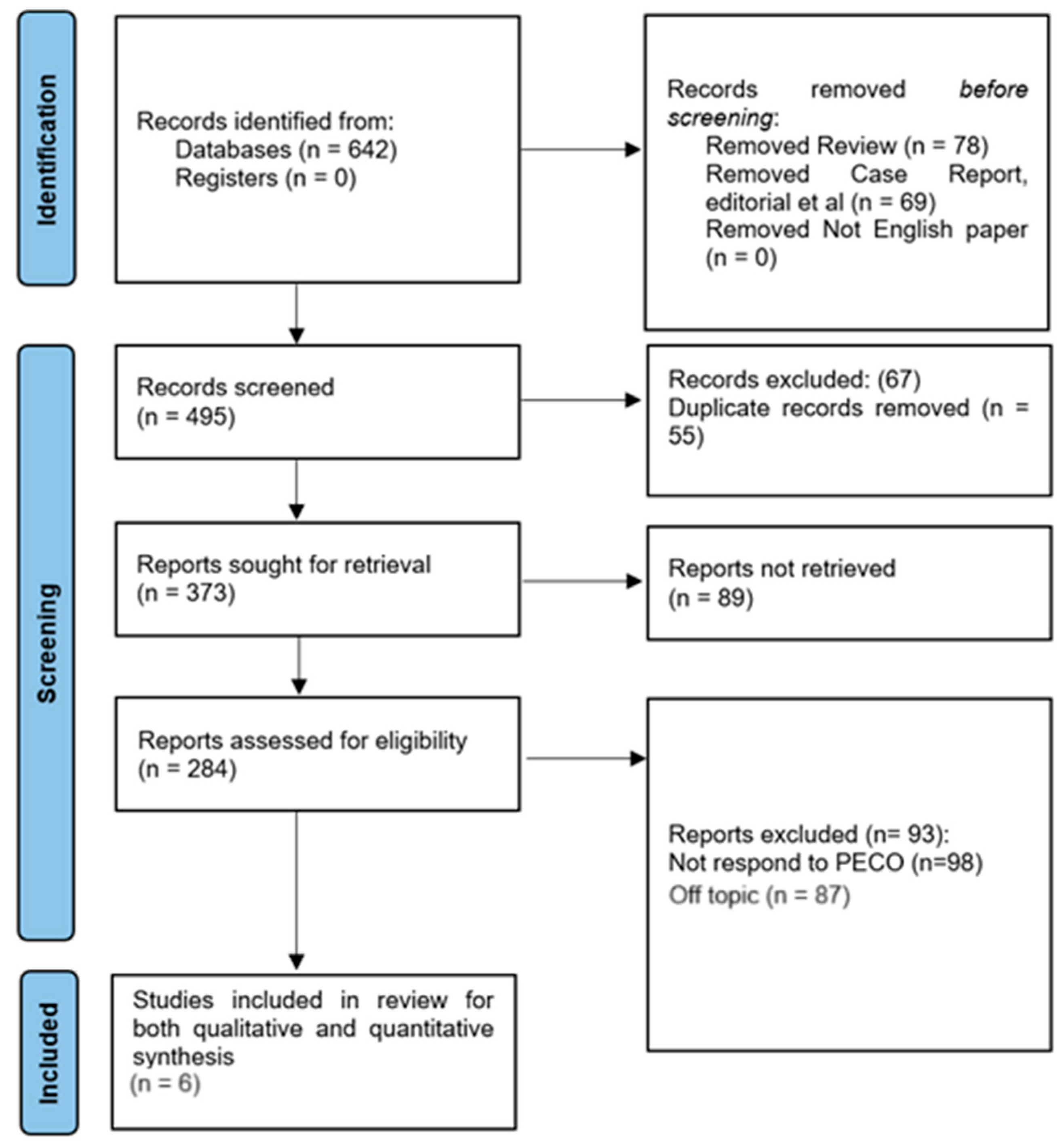
2. Materials and Methods
2.1. Review Protocol
2.2. PICOS Strategy
2.3. Database Search Strategy
2.4. Selection Criterion for the Review
- Population: Research focusing on individuals with autism spectrum disorder (ASD) and in children and young adults was eligible for inclusion.
- Study Focus: Selected papers were required to evaluate the prevalence rates of dental caries, periodontal disease, and related oral hygiene indicators in people with autism spectrum disorder (ASD).
- Peer-reviewed research articles that have been published in scholarly publications were added, encouraging the utilization of reliable and verified research.
- Cross-sectional, cohort, case–control, and clinical trial study types were all taken into consideration, as well as observational and interventional study designs.
- Irrelevant Population: Research on children and young adults with ASD was expressly omitted from the study.
- Relevant Outcome: Studies were excluded if they did not evaluate the prevalence rates of dental caries, periodontal disease, and related oral hygiene indicators, among other oral health indicators.
- Publication Type: In order to preserve the integrity of the research, non-peer-reviewed materials such as conference abstracts, editorials, and letters were disregarded.
- Non-English Language: Studies that were published in tongues other than English were disregarded since there might be difficulties in understanding and interpreting the results owing to language issues.
- Studies involving animals were not included because they did not directly address the oral health status of the ASD community, such as animal models or in vitro trials.
2.5. Data Extraction and Reviewer Protocol
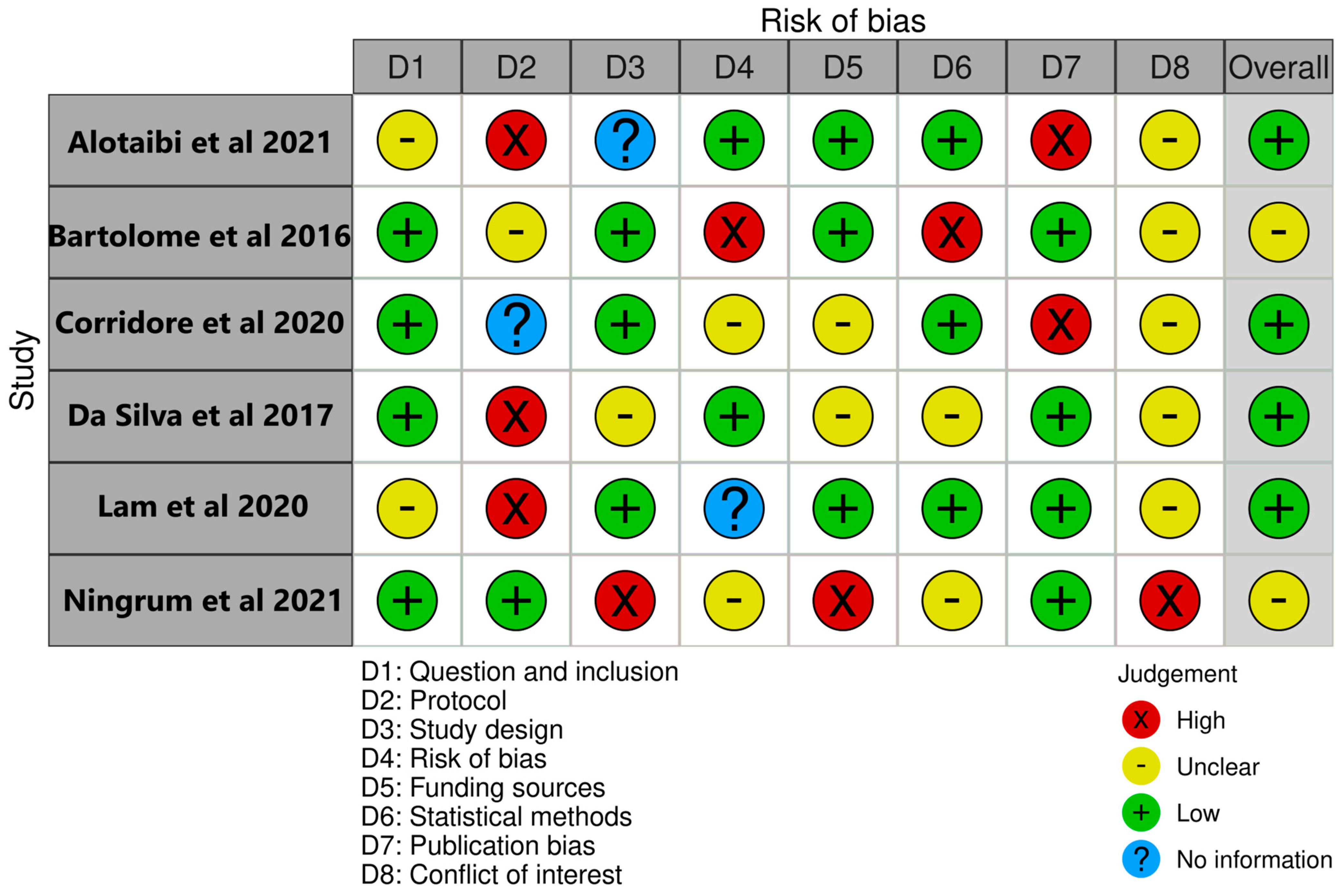
2.6. Bias Assessment of Included Studies
3. Results
3.1. Demographic Characteristics
3.2. Parametrical Assessment of Oral Health Indices
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ferrazzano, G.F.; Salerno, C.; Bravaccio, C.; Ingenito, A.; Sangianantoni, G.; Cantile, T. Autism spectrum disorders and oral health status:review of the literature. Eur. J. Paediatr. Dent. 2020, 21, 9–12. [Google Scholar] [CrossRef] [PubMed]
- El-Yousfi, S.; Jones, K.; White, S.; Marshman, Z. A rapid review of barriers to oral healthcare for vulnerable people. Br. Dent. J. 2019, 227, 143–149. [Google Scholar] [CrossRef] [PubMed]
- Rouleau, T.; Harrington, A.; Brennan, M.; Hammond, F.; Hirsch, M.; Nussbaum, M.; Bockenek, W. Receipt of dental care and barriers encountered by persons with disabilities. Spéc. Care Dent. 2011, 31, 63–67. [Google Scholar] [CrossRef]
- Lord, C.; Elsabbagh, M.; Baird, G.; Veenstra-Vanderweele, J. Autism spectrum disorder. Lancet 2018, 392, 508–520. [Google Scholar] [CrossRef]
- Udhya, J.; Varadharaja, M.M.; Parthiban, J.; Srinivasan, I. Autism disorder (AD): An updated review for paediatric dentists. J. Clin. Diagn. Res. JCDR 2014, 8, 275. [Google Scholar] [CrossRef]
- Alshatrat, S.M.; Al-Bakri, I.A.; Al-Omari, W.M.; Al Mortadi, N.A. Oral health knowledge and dental behavior among individuals with autism in Jordan: A case–control study. BMC Oral Health 2021, 21, 62. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, R.P.; Klein, U. Autism Spectrum Disorders: An Update on Oral Health Management. J. Evid. Based Dent. Pract. 2014, 14, 115–126. [Google Scholar] [CrossRef] [PubMed]
- Bernath, B.; Kanji, Z. Exploring Barriers to Oral Health Care Experienced by Individuals Living with Autism Spectrum Disorder. Can. J. Dent. Hyg. 2021, 55, 160–166. [Google Scholar]
- Fontaine-Sylvestre, C.; Roy, A.; Rizkallah, J.; Dabbagh, B.; Ferraz dos Santos, B. Prevalence of malocclusion in Canadian children with autism spectrum disorder. Am. J. Orthod. Dentofac. Orthop. 2017, 152, 38–41. [Google Scholar] [CrossRef]
- Jaber, M.A. Dental caries experience, oral health status and treatment needs of dental patients with autism. J. Appl. Oral Sci. 2011, 19, 212. [Google Scholar] [CrossRef]
- Zhang, Y.; Lin, L.; Liu, J.; Shi, L.; Lu, J. Dental Caries Status in Autistic Children: A Meta-analysis. J. Autism Dev. Disord. 2020, 50, 1249–1257. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Aromataris, E.; Fernandez, R.; Godfrey, C.; Holly, C.; Khalil, H.; Tungpunkom, P. Chapter 10: Umbrella Reviews. In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JBI: Adelaide, Australia, 2020. [Google Scholar] [CrossRef]
- AlOtaibi, A.; Ben Shaber, S.; AlBatli, A.; AlGhamdi, T.; Murshid, E. A systematic review of population-based gingival health studies among children and adolescents with autism spectrum disorder. Saudi Dent. J. 2021, 33, 370–374. [Google Scholar] [CrossRef] [PubMed]
- Bartolomé-Villar, B.; Mourelle-Martínez, M.R.; Diéguez-Pérez, M.; de Nova-García, M.J. Incidence of oral health in paediatric patients with disabilities: Sensory disorders and autism spectrum disorder. Systematic review II. J. Clin. Exp. Dent. 2016, 8, e344–e351. [Google Scholar] [CrossRef]
- Corridore, D.; Zumbo, G.; Corvino, I.; Guaragna, M.; Bossù, M.; Polimeni, A.; Vozza, I. Prevalence of oral disease and treatment types proposed to children affected by Autistic Spectrum Disorder in Pediatric Dentistry: A Systematic Review. Clin. Ter. 2020, 171, e275–e282. [Google Scholar] [CrossRef]
- da Silva, S.N.; Gimenez, T.; Souza, R.C.; Mello-Moura, A.C.V.; Raggio, D.P.; Morimoto, S.; Lara, J.S.; Soares, G.C.; Tedesco, T.K. Oral health status of children and young adults with autism spectrum disorders: Systematic review and meta-analysis. Int. J. Paediatr. Dent. 2017, 27, 388–398. [Google Scholar] [CrossRef]
- Lam, P.P.; Du, R.; Peng, S.; McGrath, C.P.; Yiu, C.K. Oral health status of children and adolescents with autism spectrum disorder: A systematic review of case-control studies and meta-analysis. Autism 2020, 24, 1047–1066. [Google Scholar] [CrossRef]
- Ningrum, V.; Bakar, A.; Shieh, T.-M.; Shih, Y.-H. The Oral Health Inequities between Special Needs Children and Normal Children in Asia: A Systematic Review and Meta-Analysis. Healthcare 2021, 9, 410. [Google Scholar] [CrossRef]
- Tomazoni, F.; Zanatta, F.B.; Tuchtenhagen, S.; da Rosa, G.N.; Del Fabro, J.P.; Ardenghi, T.M. Association of gingivitis with child oral health-related quality of life. J. Periodontol. 2014, 85, 1557–1565. [Google Scholar] [CrossRef]
- Blomqvist, M.; Bejerot, S.; Dahllöf, G. A cross-sectional study on oral health and dental care in intellectually able adults with autism spectrum disorder. BMC Oral Health 2015, 15, 81. [Google Scholar] [CrossRef]
- Stein, L.I.; Polido, J.C.; Mailloux, Z.; Coleman, G.G.; Cermak, S.A. Oral care and sensory sensitivities in children with autism spectrum disorders. Spec. Care Dentist. 2011, 31, 102–110. [Google Scholar] [CrossRef]
- Rogers, S.J.; Ozonoff, S. Annotation: What do we know about sensory dysfunction in autism? A critical review of the empirical evidence. J. Child Psychol. Psychiatry 2005, 46, 1255–1268. [Google Scholar] [CrossRef] [PubMed]
- Ashburner, J.; Bennett, L.; Rodger, S.; Ziviani, J. Understanding the sensory experiences of young people with autism spectrum disorder: A preliminary investigation. Aust. Occup. Ther. J. 2013, 60, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Subramaniam, P.; Gupta, M. Oral health status of autistic children in India. J. Clin. Pediatr. Dent. 2011, 36, 43–47. [Google Scholar] [CrossRef]
- Rai, K.; Hegde, A.M.; Jose, N. Salivary antioxidants and oral health in children with autism. Arch. Oral Biol. 2012, 57, 1116–1120. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.Y.; Wei, I.H.; Huang, C.C. Dental health—A challenging problem for a patient with autism spectrum disorder. Gen. Hosp. Psychiatry 2013, 35, 214.e1–214.e3. [Google Scholar] [CrossRef]
- Tofani, M.; Galeoto, G.; Cazzetta, D.; Berardi, A.; Sansoni, J.; Valente, D. Validation of the Pediatric Evaluation of Disability Inventory in an Italian Population with Autism Spectrum Disorder: A Cross-Sectional Study. Clin. Ter. 2019, 170, e460–e464. [Google Scholar] [CrossRef]
- Ferrara, R.; Ansermet, F.; Massoni, F.; Petrone, L.; Onofri, E.; Ricci, P.; Archer, T.; Ricci, S. Autism Spectrum Disorder and intact executive functioning. Clin. Ter. 2016, 167, e96–e101. [Google Scholar] [CrossRef]
- Romagnoli, G.; Leone, A.; Romagnoli, G.; Sansoni, J.; Tofani, M.; De Santis, R.; Valente, D.; Galeoto, G. Occupational Therapy’s efficacy in children with Asperger’s syndrome: A systematic review of randomized controlled trials. Clin. Ter. 2019, 170, e382–e387. [Google Scholar] [CrossRef]
- Troili, G.M.; Businaro, R.; Massoni, F.; Ricci, L.; Petrone, L.; Ricci, P.; Ricci, S. Indagine su un gruppo di bambini autistici: Possibili fattori di rischio e considerazioni medico sociali [Investigation on a group of autistic children: Risk factors and medical social considerations]. Clin. Ter. 2013, 164, e273–e278. (In Italian) [Google Scholar] [CrossRef]
- Vozza, I.; Cavallè, E.; Corridore, D.; Ripari, F.; Spota, A.; Brugnoletti, O.; Guerra, F. Preventive strategies in oral health for special needs patients. Ann. Stomatol. 2016, 6, 96–99. [Google Scholar] [CrossRef]
- Barros, A.; Mascarenhas, P.; Botelho, J.; Machado, V.; Balixa, G.; Bandeira Lopes, L. Autism Spectrum Disorders and Malocclusions: Systematic Review and Meta-Analyses. J. Clin. Med. 2022, 11, 2727. [Google Scholar] [CrossRef] [PubMed]
- da Motta, T.P.; Owens, J.; Abreu, L.G.; Debossan, S.A.T.; Vargas-Ferreira, F.; Vettore, M.V. Malocclusion characteristics amongst individuals with autism spectrum disorder: A systematic review and meta-analysis. BMC Oral Health 2022, 22, 341. [Google Scholar] [CrossRef] [PubMed]
- Erwin, J.; Paisi, M.; Neill, S.; Burns, L.; Vassallo, I.; Nelder, A.; Facenfield, J.; Devalia, U.; Vassallo, T.; Witton, R. Factors influencing oral health behaviours, access and delivery of dental care for autistic children and adolescents: A mixed-methods systematic review. Health Expect. 2022, 25, 1269–1318. [Google Scholar] [CrossRef] [PubMed]
| Study | Variables Assessed | Data Sources | Key Findings | Conclusion |
|---|---|---|---|---|
| AlOtaibi et al. [14] | Gingival and plaque indices | MEDLINE, PubMed, the Cochrane Library, Web of Science, Controlled-Trial Database, Clinical Trials-US National Institutes of Health, National Institute for Health and Clinical Excellence, Virtual Health Library, and Saudi Digital Library |
| Individuals with ASD need help and better access to oral healthcare. Further investigation is needed with regard to gingival health in individuals with ASD and caries risk assessment to understand how this disorder affects oral health. |
| Bartolomé et al. [15] | Oral hygiene, dental caries, malocclusion, oral habits, dental trauma, and gingival/periodontal status | PubMed/Medline, Scopus, Cochrane Library |
| A larger number of research studies is needed to corroborate these results. There are discrepancies about the results found in the different studies regarding dental caries and oral hygiene in children with ASD and SD. |
| Corridore et al. [16] |
| Pubmed, Scopus, EMBASE, Science Citation Index, Science Direct, Web of Science |
| Lack of protocols for ASD patients, need for improved collaboration and preventive care. |
| Da Silva et al. [17] |
| MEDLINE/PubMed, Web of Science, Scopus |
| Need for oral health policies targeting high prevalence of dental caries and periodontal disease in ASD individuals. |
| Lam et al. [18] |
| CINAHL, Ovid Embase, Ovid MEDLINE, PsycINFO, Web of Science |
| Limited evidence, high risk of bias, need for further research. |
| Ningrum et al. [19] |
| PubMed, Scopus, Cochrane Library, Web of Science, Wiley Online Library |
| Importance of an integrated and equitable care system to maintain oral health of special needs children, especially in high DMFT countries. |
| Source | Dental Caries | Periodontal Disease | Oral Hygiene |
|---|---|---|---|
| AlOtaibi et al. [14] | Not clearly specified |
|
|
| Bartolomé et al. [15] |
|
|
|
| Corridore et al. [16] |
|
|
|
| Da Silva et al. [17] |
|
| No statistical difference observed between the ASD and control groups |
| Lam et al. [18] | No statistical difference observed between the ASD and control groups |
|
|
| Ningrum et al. [19] |
|
|
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sami, W.; Ahmad, M.S.; Shaik, R.A.; Miraj, M.; Ahmad, S.; Molla, M.H. Oral Health Statuses of Children and Young Adults with Autism Spectrum Disorder: An Umbrella Review. J. Clin. Med. 2024, 13, 59. https://doi.org/10.3390/jcm13010059
Sami W, Ahmad MS, Shaik RA, Miraj M, Ahmad S, Molla MH. Oral Health Statuses of Children and Young Adults with Autism Spectrum Disorder: An Umbrella Review. Journal of Clinical Medicine. 2024; 13(1):59. https://doi.org/10.3390/jcm13010059
Chicago/Turabian StyleSami, Waqas, Mohammad Shakil Ahmad, Riyaz Ahamed Shaik, Mohammad Miraj, Sadiya Ahmad, and Muhammed Hamza Molla. 2024. "Oral Health Statuses of Children and Young Adults with Autism Spectrum Disorder: An Umbrella Review" Journal of Clinical Medicine 13, no. 1: 59. https://doi.org/10.3390/jcm13010059
APA StyleSami, W., Ahmad, M. S., Shaik, R. A., Miraj, M., Ahmad, S., & Molla, M. H. (2024). Oral Health Statuses of Children and Young Adults with Autism Spectrum Disorder: An Umbrella Review. Journal of Clinical Medicine, 13(1), 59. https://doi.org/10.3390/jcm13010059