Evaluation of Self-Management Behaviors and Its Correlation with the Metabolic Syndrome among the Type 2 Diabetes Mellitus Patients of Northern Saudi Arabia
Abstract
:1. Introduction
2. Participants and Methods
2.1. Study Design
2.2. Study Setting
2.3. Sampling Method
2.4. Data Collection Steps
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Reed, J.; Bain, S.; Kanamarlapudi, V. A Review of Current Trends with Type 2 Diabetes Epidemiology, Aetiology, Pathogenesis, Treatments and Future Perspectives. Diabetes Metab. Syndr. Obes. 2021, 14, 3567–3602. [Google Scholar] [CrossRef] [PubMed]
- Goyal, R.; Singhal, M.; Jialal, I. Type 2 Diabetes. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. [Google Scholar]
- IDF. Diabetes: Facts and Figures. Available online: https://idf.org/about-diabetes/diabetes-facts-figures/ (accessed on 15 October 2023).
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res. Clin. Pract. 2019, 157, 107843. [Google Scholar] [CrossRef] [PubMed]
- Jarrar, M.; Abusalah, M.A.H.; Albaker, W.; Al-Bsheish, M.; Alsyouf, A.; Al-Mugheed, K.; Issa, M.R.; Alumran, A. Prevalence of Type 2 Diabetes Mellitus in the General Population of Saudi Arabia, 2000–2020: A Systematic Review and Meta-Analysis of Observational Studies. Saudi J. Med. Med. Sci. 2023, 11, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Aljulifi, M.Z. Prevalence and reasons of increased type 2 diabetes in Gulf Cooperation Council Countries. Saudi Med. J. 2021, 42, 481–490. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Patterson, C.C.; Zhang, X.; Ghani, R.B.A.; Magliano, D.J.; Boyko, E.J.; Ogle, G.D.; Luk, A.O.Y. Worldwide estimates of incidence of type 2 diabetes in children and adolescents in 2021. Diabetes Res. Clin. Pract. 2022, 185, 109785. [Google Scholar] [CrossRef] [PubMed]
- Perng, W.; Conway, R.; Mayer-Davis, E.; Dabelea, D. Youth-Onset Type 2 Diabetes: The Epidemiology of an Awakening Epidemic. Diabetes Care 2023, 46, 490–499. [Google Scholar] [CrossRef]
- Powers, M.A.; Bardsley, J.; Cypress, M.; Duker, P.; Funnell, M.M.; Fischl, A.H.; Maryniuk, M.D.; Siminerio, L.; Vivian, E. Diabetes Self-management Education and Support in Type 2 Diabetes: A Joint Position Statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Clin. Diabetes 2016, 34, 70–80. [Google Scholar] [CrossRef] [PubMed]
- Babazadeh, T.; Dianatinasab, M.; Daemi, A.; Nikbakht, H.A.; Moradi, F.; Ghaffari-Fam, S. Association of Self-Care Behaviors and Quality of Life among Patients with Type 2 Diabetes Mellitus: Chaldoran County, Iran. Diabetes Metab. J. 2017, 41, 449–456. [Google Scholar] [CrossRef]
- Lin, H.C.; Tseng, C.W.; Hsieh, P.J.; Liang, H.L.; Sue, S.P.; Huang, C.Y.; Lee, M.Y. Efficacy of Self-Management on Glucose Control in Type 2 Diabetes Mellitus Patients Treated with Insulin. Healthcare 2022, 10, 2080. [Google Scholar] [CrossRef]
- Shrivastava, S.R.; Shrivastava, P.S.; Ramasamy, J. Role of self-care in management of diabetes mellitus. J. Diabetes Metab. Disord. 2013, 12, 14. [Google Scholar] [CrossRef]
- Matpady, P.; Maiya, A.G.; Saraswat, P.P.; Mayya, S.S.; Pai, M.S.; Anupama, D.S.; Umakanth, S. Dietary self-management practices among persons with T2DM: An exploratory qualitative study from western-coast of India. Diabetes Metab. Syndr. 2020, 14, 2161–2167. [Google Scholar] [CrossRef] [PubMed]
- Gray, A.; Threlkeld, R.J. Nutritional Recommendations for Individuals with Diabetes. In Endotext; Feingold, K.R., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatariya, K., Dungan, K., Hofland, J., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. [Google Scholar]
- Petroni, M.L.; Brodosi, L.; Marchignoli, F.; Sasdelli, A.S.; Caraceni, P.; Marchesini, G.; Ravaioli, F. Nutrition in Patients with Type 2 Diabetes: Present Knowledge and Remaining Challenges. Nutrients 2021, 13, 2748. [Google Scholar] [CrossRef] [PubMed]
- Pan, L.; Zhang, X.; Wang, S.; Zhao, N.; Zhao, R.; Ding, B.; Li, Y.; Miao, W.; Fan, H. Determinants associated with self-management behavior among type 2 diabetes patients in China: A structural equation model based on the theory of planned behavior. Int. J. Clin. Health Psychol. 2023, 23, 100332. [Google Scholar] [CrossRef] [PubMed]
- Regufe, V.M.G.; Pinto, C.; Perez, P. Metabolic syndrome in type 2 diabetic patients: A review of current evidence. Porto Biomed. J. 2020, 5, e101. [Google Scholar] [CrossRef] [PubMed]
- Hayden, M.R. Overview and New Insights into the Metabolic Syndrome: Risk Factors and Emerging Variables in the Development of Type 2 Diabetes and Cerebrocardiovascular Disease. Medicina 2023, 59, 561. [Google Scholar] [CrossRef] [PubMed]
- Ji, M.; Ren, D.; Dunbar-Jacob, J.; Gary-Webb, T.L.; Erlen, J.A. Self-Management Behaviors, Glycemic Control, and Metabolic Syndrome in Type 2 Diabetes. Nurs. Res. 2020, 69, E9–E17. [Google Scholar] [CrossRef] [PubMed]
- Alodhayani, A.; Almutairi, K.M.; Vinluan, J.M.; Almigbal, T.H.; Alonazi, W.B.; Ali Batais, M.; Mohammed Alnassar, M. Association between self-care management practices and glycemic control of patients with type 2 diabetes mellitus in Saud Arabia: A cross -sectional study. Saudi J. Biol. Sci. 2021, 28, 2460–2465. [Google Scholar] [CrossRef]
- Almomani, M.H.; Al-Tawalbeh, S. Glycemic Control and Its Relationship with Diabetes Self-Care Behaviors among Patients with Type 2 Diabetes in Northern Jordan: A Cross-Sectional Study. Patient Prefer. Adherence 2022, 16, 449–465. [Google Scholar] [CrossRef]
- Ghamri, R.A.; Alamri, S.H. Metabolic syndrome among adults with type 2 diabetes in a Saudi teaching hospital: A comparative prevalence study using WHO and ATP III definitions. Pak. J. Med. Sci. 2019, 35, 1087–1092. [Google Scholar] [CrossRef]
- Raosoft. Sample Size Calculator by Raosoft, Inc. Available online: http://www.raosoft.com/samplesize.html (accessed on 12 February 2023).
- Grundy, S.M.; Cleeman, J.I.; Daniels, S.R.; Donato, K.A.; Eckel, R.H.; Franklin, B.A.; Gordon, D.J.; Krauss, R.M.; Savage, P.J.; Smith, S.C., Jr.; et al. Diagnosis and management of the metabolic syndrome: An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005, 112, 2735–2752. [Google Scholar] [CrossRef]
- WHO. Body Mass Index (BMI). Available online: https://www.who.int/data/gho/data/themes/topics/topic-details/GHO/body-mass-index (accessed on 18 August 2023).
- Ross, R.; Neeland, I.J.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; Cuevas, A.; Hu, F.B.; et al. Waist circumference as a vital sign in clinical practice: A Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 2020, 16, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Ma, W.Y.; Yang, C.Y.; Shih, S.R.; Hsieh, H.J.; Hung, C.S.; Chiu, F.C.; Lin, M.S.; Liu, P.H.; Hua, C.H.; Hsein, Y.C.; et al. Measurement of Waist Circumference: Midabdominal or iliac crest? Diabetes Care 2013, 36, 1660–1666. [Google Scholar] [CrossRef] [PubMed]
- Toobert, D.J.; Hampson, S.E.; Glasgow, R.E. The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care 2000, 23, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Sukkarieh-Haraty, O.; Howard, E. Psychometric Properties of the Arabic Version of the Summary of Diabetes Self-Care Activities Instrument. Res. Theory Nurs. Pract. 2016, 30, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Alhaiti, A.H.; Senitan, M.; Dator, W.L.T.; Sankarapandian, C.; Baghdadi, N.A.; Jones, L.K.; Da Costa, C.; Lenon, G.B. Adherence of Type 2 Diabetic Patients to Self-Care Activity: Tertiary Care Setting in Saudi Arabia. J. Diabetes Res. 2020, 2020, 4817637. [Google Scholar] [CrossRef]
- Chandrika, K.; Das, B.N.; Syed, S.; Challa, S. Diabetes Self-Care Activities: A Community-Based Survey in an Urban Slum in Hyderabad, India. Indian J. Community Med. 2020, 45, 307–310. [Google Scholar] [CrossRef] [PubMed]
- Shah, S.Z.A.; Karam, J.A.; Zeb, A.; Ullah, R.; Shah, A.; Haq, I.U.; Ali, I.; Darain, H.; Chen, H. Movement is Improvement: The Therapeutic Effects of Exercise and General Physical Activity on Glycemic Control in Patients with Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Diabetes Ther. 2021, 12, 707–732. [Google Scholar] [CrossRef]
- Cannata, F.; Vadalà, G.; Russo, F.; Papalia, R.; Napoli, N.; Pozzilli, P. Beneficial Effects of Physical Activity in Diabetic Patients. J. Funct. Morphol. Kinesiol. 2020, 5, 70. [Google Scholar] [CrossRef]
- Alanazi, M.; Alatawi, A.M. Adherence to Diabetes Mellitus Treatment Regimen among Patients with Diabetes in the Tabuk Region of Saudi Arabia. Cureus 2022, 14, e30688. [Google Scholar] [CrossRef]
- Alsaidan, A.A.; Alotaibi, S.F.; Thirunavukkarasu, A.; BF, A.L.; Alharbi, R.H.; Arnous, M.M.; Alsaidan, O.A.; Alduraywish, A.S.; Alwushayh, Y.A. Medication Adherence and Its Associated Factors among Patients with Type 2 Diabetes Mellitus Attending Primary Health Centers of Eastern Province, Saudi Arabia. Medicina 2023, 59, 989. [Google Scholar] [CrossRef]
- AlShayban, D.M.; Naqvi, A.A.; Alhumaid, O.; AlQahtani, A.S.; Islam, M.A.; Ghori, S.A.; Haseeb, A.; Ali, M.; Iqbal, M.S.; Elrggal, M.E.; et al. Association of Disease Knowledge and Medication Adherence among Out-Patients with Type 2 Diabetes Mellitus in Khobar, Saudi Arabia. Front. Pharmacol. 2020, 11, 60. [Google Scholar] [CrossRef] [PubMed]
- Maina, P.M.; Pienaar, M.; Reid, M. Self-management practices for preventing complications of type II diabetes mellitus in low and middle-income countries: A scoping review. Int. J. Nurs. Stud. Adv. 2023, 5, 100136. [Google Scholar] [CrossRef]
- Peng, X.; Guo, X.; Li, H.; Wang, D.; Liu, C.; Du, Y. A Qualitative Exploration of Self-Management Behaviors and Influencing Factors in Patients with Type 2 Diabetes. Front. Endocrinol. 2022, 13, 771293. [Google Scholar] [CrossRef] [PubMed]
- Ravi, S.; Kumar, S.; Gopichandran, V. Do supportive family behaviors promote diabetes self-management in resource limited urban settings? A cross sectional study. BMC Public Health 2018, 18, 826. [Google Scholar] [CrossRef]
- Asghar, S.; Asghar, S.; Shahid, S.; Fatima, M.; Bukhari, S.M.H.; Nadeem Siddiqui, S. Metabolic Syndrome in Type 2 Diabetes Mellitus Patients: Prevalence, Risk Factors, and Associated Microvascular Complications. Cureus 2023, 15, e39076. [Google Scholar] [CrossRef]
- Gemeda, D.; Abebe, E.; Duguma, A. Metabolic Syndrome and Its Associated Factors among Type 2 Diabetic Patients in Southwest Ethiopia, 2021/2022. J. Diabetes Res. 2022, 2022, 8162342. [Google Scholar] [CrossRef]
- do Vale Moreira, N.C.; Hussain, A.; Bhowmik, B.; Mdala, I.; Siddiquee, T.; Fernandes, V.O.; Montenegro Júnior, R.M.; Meyer, H.E. Prevalence of Metabolic Syndrome by different definitions, and its association with type 2 diabetes, pre-diabetes, and cardiovascular disease risk in Brazil. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 1217–1224. [Google Scholar] [CrossRef]
- James, M.; Varghese, T.P.; Sharma, R.; Chand, S. Association between Metabolic Syndrome and Diabetes Mellitus According to International Diabetic Federation and National Cholesterol Education Program Adult Treatment Panel III Criteria: A Cross-sectional Study. J. Diabetes Metab. Disord. 2020, 19, 437–443. [Google Scholar] [CrossRef]
- Grabia, M.; Markiewicz-Żukowska, R.; Socha, K.; Polkowska, A.; Zasim, A.; Boruch, K.; Bossowski, A. Prevalence of Metabolic Syndrome in Relation to Cardiovascular Biomarkers and Dietary Factors among Adolescents with Type 1 Diabetes Mellitus. Nutrients 2022, 14, 2435. [Google Scholar] [CrossRef]
- Kim, H.-B.; Wolf, B.J.; Kim, J.-H. Association of metabolic syndrome and its components with the risk of depressive symptoms: A systematic review and meta-analysis of cohort studies. J. Affect. Disord. 2023, 323, 46–54. [Google Scholar] [CrossRef]
- Ghanei Gheshlagh, R.; Parizad, N.; Sayehmiri, K. The Relationship between Depression and Metabolic Syndrome: Systematic Review and Meta-Analysis Study. Iran. Red. Crescent Med. J. 2016, 18, e26523. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Lee, K.H.; Kim, H.J.; Youk, H.; Lee, H.Y. Effective Prevention and Management Tools for Metabolic Syndrome Based on Digital Health-Based Lifestyle Interventions Using Healthcare Devices. Diagnostics 2022, 12, 1730. [Google Scholar] [CrossRef] [PubMed]
- Cohen, E.; Margalit, I.; Goldberg, E.; Krause, I. Gender as an Independent Risk Factor for the Components of Metabolic Syndrome among Individuals within the Normal Range of Body Mass Index. Metab. Syndr. Relat. Disord. 2018, 16, 537–542. [Google Scholar] [CrossRef] [PubMed]
- Ramezankhani, A.; Azizi, F.; Hadaegh, F. Gender differences in changes in metabolic syndrome status and its components and risk of cardiovascular disease: A longitudinal cohort study. Cardiovasc. Diabetol. 2022, 21, 227. [Google Scholar] [CrossRef] [PubMed]
- Du, S.; Zhang, H.; Wu, H.; Ye, S.; Li, W.; Su, Q. Prevalence and Gender Differences of Metabolic Syndrome in Young Ketosis-Prone Type 2 Diabetic Individuals: A Retrospective Study. Diabetes Metab. Syndr. Obes. 2020, 13, 2719–2727. [Google Scholar] [CrossRef] [PubMed]
- Arnlöv, J.; Sundström, J.; Ingelsson, E.; Lind, L. Impact of BMI and the metabolic syndrome on the risk of diabetes in middle-aged men. Diabetes Care 2011, 34, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Alegría Ezquerra, E.; Castellano Vázquez, J.M.; Alegría Barrero, A. Obesity, Metabolic Syndrome and Diabetes: Cardiovascular Implications and Therapy. Rev. Esp. Cardiol. Engl. Ed. 2008, 61, 752–764. [Google Scholar] [CrossRef]
- Kobo, O.; Leiba, R.; Avizohar, O.; Karban, A. Normal body mass index (BMI) can rule out metabolic syndrome: An Israeli cohort study. Medicine 2019, 98, e14712. [Google Scholar] [CrossRef]
- Ernawati, U.; Wihastuti, T.A.; Utami, Y.W. Effectiveness of diabetes self-management education (DSME) in type 2 diabetes mellitus (T2DM) patients: Systematic literature review. J. Public Health Res. 2021, 10, jphr-2021. [Google Scholar] [CrossRef]
- Araújo-Soares, V.; Hankonen, N.; Presseau, J.; Rodrigues, A.; Sniehotta, F.F. Developing Behavior Change Interventions for Self-Management in Chronic Illness: An Integrative Overview. Eur. Psychol. 2019, 24, 7–25. [Google Scholar] [CrossRef]
- Cardoso Barbosa, H.; de Queiroz Oliveira, J.A.; Moreira da Costa, J.; de Melo Santos, R.P.; Gonçalves Miranda, L.; de Carvalho Torres, H.; Pagano, A.S.; Parreiras Martins, M.A. Empowerment-oriented strategies to identify behavior change in patients with chronic diseases: An integrative review of the literature. Patient Educ. Couns. 2021, 104, 689–702. [Google Scholar] [CrossRef] [PubMed]
| Variables | Frequency (n) | Proportion (%) |
|---|---|---|
| Age (mean ± SD) | 55.50 ± 11.06 | |
| Less than 50 years | 91 | 29.4 |
| From 50 to 60 years | 126 | 40.6 |
| More than 61 years | 93 | 30.0 |
| Gender | ||
| Male | 163 | 52.6 |
| Female | 147 | 47.4 |
| Educational qualification | ||
| No formal education. | 46 | 14.8 |
| Primary/Preparatory/Secondary | 173 | 55.8 |
| University/Graduate Studies | 91 | 29.4 |
| Occupation | ||
| Employee in a government sector | 87 | 28.1 |
| Employee in the private sector | 18 | 5.8 |
| Unemployed | 111 | 35.8 |
| Retired | 94 | 30.3 |
| Married status | ||
| Single | 75 | 24.2 |
| Currently married | 235 | 75.8 |
| Monthly income in SAR (1 USD = 3.75 SAR) | ||
| Less than 5000 SAR | 100 | 32.2 |
| From 5000 to 1000 SAR | 104 | 33.5 |
| More than 10,000 SAR | 106 | 34.3 |
| Smoking status | ||
| No | 247 | 79.7 |
| Yes | 63 | 20.3 |
| Duration of T2DM (mean ± SD) | 9.84 ± 5.23 | |
| Type (s) of anti-diabetes treatment | ||
| Insulin only | 82 | 26.5 |
| Oral hypoglycemic agents (OHA) only | 204 | 65.8 |
| Both | 24 | 7.7 |
| Presence of comorbid condition | ||
| No | 208 | 67.1 |
| Yes | 102 | 32.9 |
| Parameters | Mean | SD |
|---|---|---|
| BMI (kg/m2) | 32.02 | 13.06 |
| Waist circumference (cms) | 105.75 | 16.22 |
| Systolic BP (mmHg) | 132.95 | 14.41 |
| Diastolic BP (mmHg) | 79.88 | 9.65 |
| FBS (mmol/L) | 8.56 | 6.96 |
| LDL ((mmol/L) | 2.85 | 0.93 |
| HDL (mmol/L) | 1.24 | 0.68 |
| Total Cholesterol (mmol/L) | 4.65 | 1.09 |
| TGL (mmol/L) | 1.68 | 0.78 |
| Subscales/Items | Mean | SD |
|---|---|---|
| Diet (general and special) | ||
| 2.80 | 2.59 |
| 2.81 | 2.62 |
| 3.67 | 2.45 |
| 3.65 | 2.52 |
| 3.83 | 2.30 |
| Physical activities | ||
| 2.65 | 2.64 |
| 1.84 | 2.37 |
| Blood sugar testing | ||
| 3.78 | 2.76 |
| 3.20 | 2.88 |
| Footcare (how many days in a week) | ||
| 1.66 | 2.55 |
| 1.42 | 2.47 |
| 4.99 | 2.92 |
| 2.82 | 2.97 |
| Medication | ||
| 5.93 | 2.05 |
| 5.72 | 2.17 |
| Overall (mean ± SD) | 3.98 | 1.26 |
| Unsatisfactory (<4) = 68.39% | ||
| Satisfactory (from 4 to 7) = 31.61% |
| SDSCA Items | BMI (kg/m2) | Waist Circumference (cms) | Total Cholesterol (mmol/L) | Triglycerides (mmol/L) | LDL (mmol/L) | HDL (mmol/L) | Fasting Blood Sugar (mmol/L) |
|---|---|---|---|---|---|---|---|
| Healthy diet plan | −0.160/0.005 | −0.252/0.001 | −0.071/0.212 | −0.172/0.002 | −0.069/0.227 | 0.168/0.003 | −0.260/0.001 |
| Specific diet plan | −0.125/0.027 | −0.196/0.001 | −0.035/0.545 | −0.172/0.002 | −0.008/0.882 | 0.176/0.002 | −0.248/0.001 |
| Fruits and vegetables intake | 0.063/0.266 | −0.012/0.839 | −0.013/0.816 | −0.077/0.175 | −0.038/0.507 | 0.107/0.61 | −0.133/0.019 |
| Evenly distribution of carbohydrates in food | 0.037/0.521 | −0.013/0.824 | −0.048/0.396 | −0.115/0.044 | −0.044/0.441 | 0.103/0.069 | −0.151/0.008 |
| High fat intake | 0.001/0.996 | 0.013/0.813 | 0.038/0.502 | 0.169/0.029 | 0.180/0.013 | −0.004/0.943 | 0.021/0.712 |
| Physical activity | −0.206/0.001 | −0.229/0.001 | −0.031/0.586 | −0.075/0.188 | 0.019/0.734 | 0.139/0.014 | −0.152/0.008 |
| Specific exercise session | −0.236/0.001 | −0.230/0.001 | 0.032/0.574 | −0.137/0.016 | 0.050/0.378 | 0.159/0.005 | −0.199/0.001 |
| Testing for blood sugar | 0.064/0.261 | 0.009/0.877 | −0.009/0.870 | −0.010/0.858 | −0.035/0.541 | 0.124/0.029 | 0.031/0.582 |
| Number of times testing blood sugar | 0.051/0.374 | 0.017/0.772 | −0.062/0.278 | 0.030/0.605 | −0.100/0.077 | 0.100/0.079 | 0.001/0.984 |
| Checked the feet | 0.019/0.739 | −0.048/0.399 | −0.041/0.476 | −0.196/0.001 | −0.018/0.752 | 0.021/0.710 | 0.007/0.905 |
| Inspect the inside of your shoes | −0.002/0.967 | 0.025/0.662 | −0.075/0.187 | −0.209/0.001 | −0.059/0.297 | 0.093/0.102 | −0.033/0.562 |
| Washed with the soap | 0.005/0.930 | 0.025/0.667 | −0.145/0.011 | 0.013/0.817 | −0.164/0.004 | 0.035/0.544 | 0.045/0.425 |
| Dry between your toes after washing | 0.026/0.644 | −0.015/0.788 | −0.145/0.426 | −0.012/0.835 | −0.031/0.592 | 0.052/0.365 | −0.092/0.106 |
| Adherence to insulin | 0.073/0.198 | 0.002/0.973 | −0.143/0.012 | 0.068/0.233 | −0.209/0.001 | 0.080/0.161 | −0.311/0.001 |
| Adherence to OHA | 0.161/0.004 | 0.117/0.040 | −0.134/0.018 | 0.113/0.047 | −0.177/0.002 | 0.071/0.215 | −0.250/0.006 |
| Characteristics | Total Participants (n = 310) | MS | Univariate Analysis No vs. Yes | Regression Analysis * No vs. Yes | |||
|---|---|---|---|---|---|---|---|
| No (%) n = 197 | Yes (%) n = 113 | Unadjusted Odds Ratio (OR) (95% CI) | p Value ** | Adjusted OR (AOR) (95% CI) | p Value ** | ||
| Age | |||||||
| Less than 50 years | 91 | 56 | 35 | Ref | Ref | ||
| From 50 to 60 years | 126 | 85 | 41 | 0.77 (0.44–1.36) | 0.367 | 0.79 (0.40–1.52) | 0.482 |
| More than 61 years | 93 | 56 | 37 | 1.06 (0.59–1.91) | 0.854 | 1.04 (0.46–2.35) | 0.929 |
| Gender | |||||||
| Male | 163 | 110 | 53 | Ref | Ref | ||
| Female | 147 | 87 | 60 | 2.37 (1.50–3.18) | 0.026 | 1.89 (1.17–2.95) | 0.007 |
| Educational Qualification | |||||||
| No formal education. | 46 | 27 | 19 | Ref | Ref | ||
| Primary/Preparatory/Secondary | 173 | 106 | 67 | 0.87 (0.46–1.74) | 0.375 | 0.89 (0.41–1.92) | 0.766 |
| University/Graduate Studies | 91 | 64 | 27 | 0.60 (0.29–1.26) | 0.839 | 0.63 (0.24–1.71) | 0.365 |
| Occupation | |||||||
| Government sector | 87 | 59 | 28 | Ref | Ref | ||
| Private sector | 18 | 7 | 11 | 3.31 (1.16–5.45) | 0.025 | 2.75 (0.90–5.23) | 0.075 |
| Unemployed | 111 | 68 | 43 | 1.33 (0.74–2.40) | 0.34 | 1.12 (0.43–2.89) | 0.815 |
| Retired | 94 | 63 | 31 | 1.04 (0.56–1.93) | 0.909 | 0.96 (0.43–2.15) | 0.921 |
| Married status | |||||||
| Single | 75 | 42 | 33 | Ref | Ref | ||
| Currently married | 235 | 155 | 80 | 0.66 (0.39–1.12) | 0.12 | 0.71 (0.39–1.28) | 0.229 |
| Monthly income in SAR (1 USD = 3.75 SAR) | |||||||
| Less than 5000 SAR | 100 | 64 | 36 | Ref | Ref | ||
| From 5000 to 1000 SAR | 104 | 60 | 44 | 1.30 (0.74–2.29) | 0.357 | 1.59 (0.79–3.17) | 0.186 |
| More than 10000 SAR | 106 | 73 | 33 | 0.80 (0.45–1.44) | 0.46 | 1.11 (0.47–2.60) | 0.807 |
| Smoking status | |||||||
| Yes | 63 | 35 | 28 | Ref | Ref | ||
| No | 247 | 162 | 85 | 1.35 (0.94–1.79) | 0.068 | 1.56 (1.17–2.41) | 0.016 |
| Duration of T2DM | 9.84 ± 5.23 | 2.19 (0.69–4.34) | 0.699 | 1.93 (0.65–4.31) | 0.742 | ||
| Type (s) of anti-diabetes treatment | |||||||
| Insulin | 82 | 47 | 35 | Ref | Ref | ||
| OHA | 204 | 134 | 70 | 2.05 (0.69–4.19) | 0.517 | 1.95 (0.83–3.14) | 0.091 |
| Both | 24 | 16 | 8 | 0.89 (0.45–3.77) | 0.864 | 1.22 (0.65–2.28) | 0.112 |
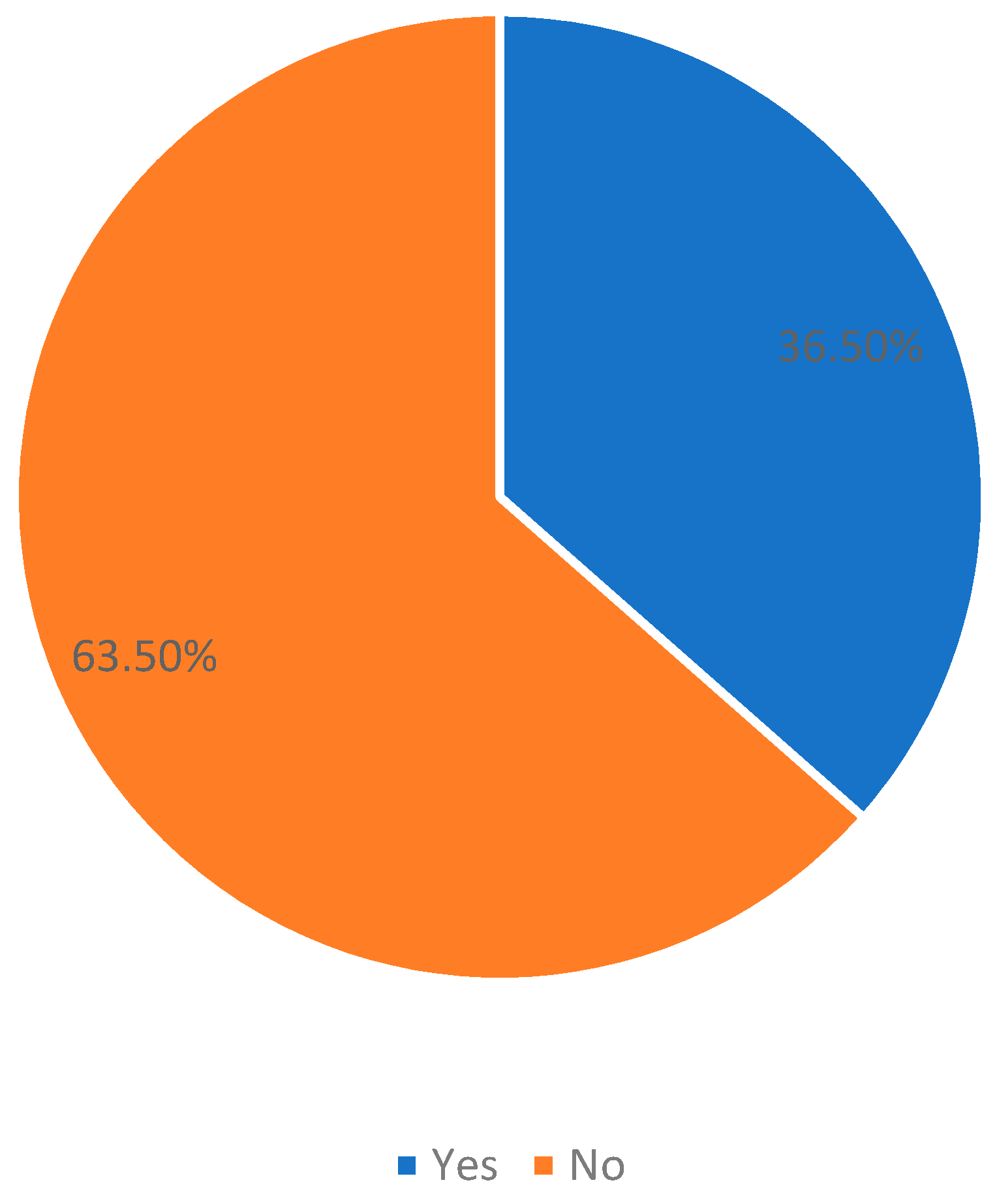
| Self-management behavior | |||||||
| Satisfactory | 98 | 66 | 32 | Ref | Ref | ||
| Unsatisfactory | 212 | 131 | 81 | 1.73 (1.03–3.17) | 0.008 | 1.55 (1.11–2.87) | 0.027 |
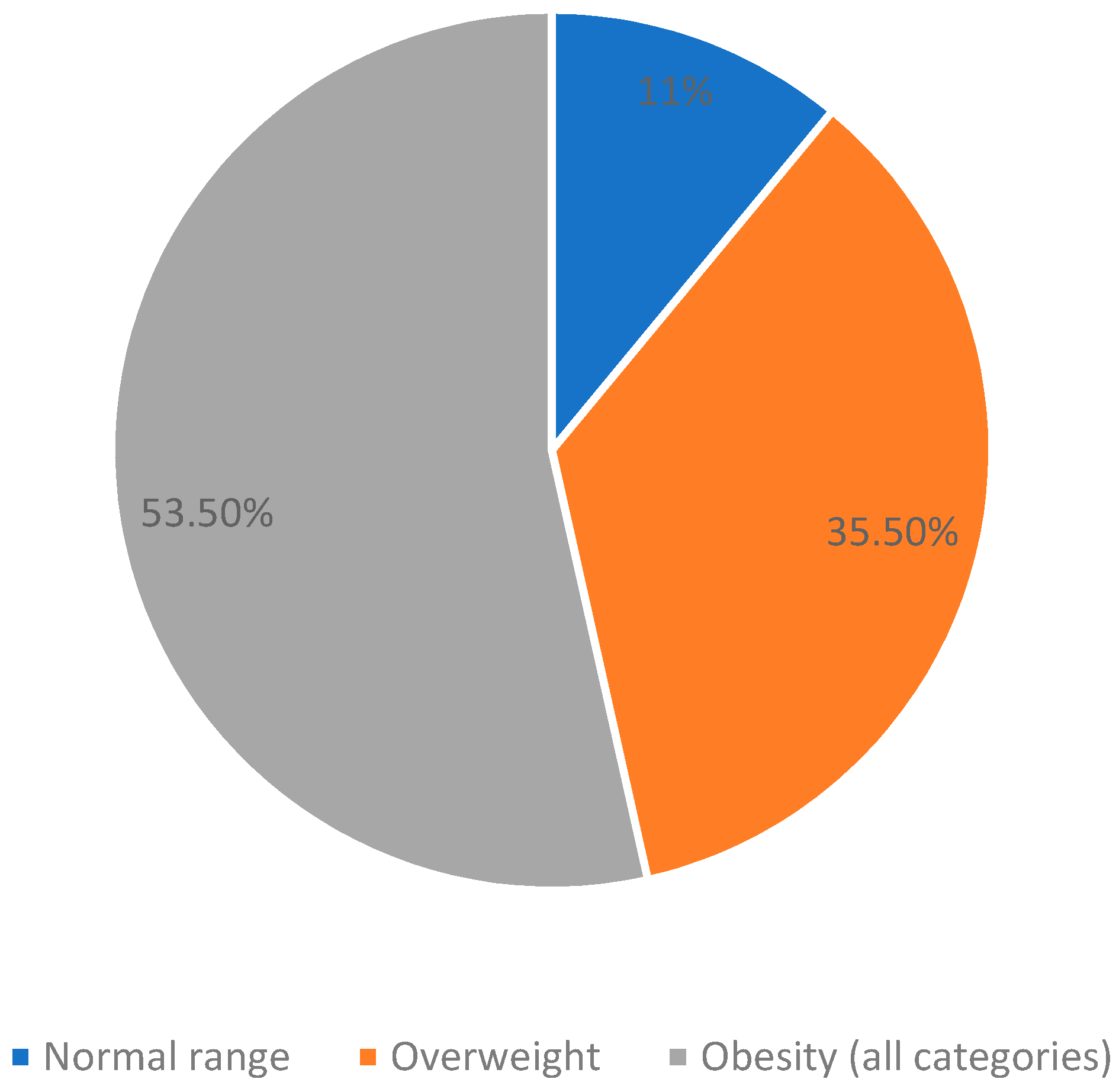
| Body mass index | |||||||
| Normal | 34 | 27 | 7 | Ref | Ref | ||
| Overweight | 110 | 71 | 32 | 1.64 (0.81–2.67) | 0.073 | 1.08 (0.71–1.96) | 0.063 |
| Obesity (all categories) | 166 | 109 | 74 | 2.03 (1.21–3.71) | 2.98 (1.31–5.07) | 0.003 | |
| Presence of other chronic conditions | |||||||
| No | 208 | 130 | 78 | Ref | Ref | ||
| Yes | 102 | 67 | 35 | 2.21 (1.35–3.60) | 0.002 | 1.74 (1.11–2.67) | 0.006 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsaidan, A.A.; Thirunavukkarasu, A.; Alhassan, H.H.; Bin Ahmed, I.A.; Alnasiri, A.S.; Alhirsan, W.M.; Alazmi, N.N.M.; Alkhlaf, A.K.; Alderbas, J.M.; Alkhaldi, M.A. Evaluation of Self-Management Behaviors and Its Correlation with the Metabolic Syndrome among the Type 2 Diabetes Mellitus Patients of Northern Saudi Arabia. J. Clin. Med. 2024, 13, 118. https://doi.org/10.3390/jcm13010118
Alsaidan AA, Thirunavukkarasu A, Alhassan HH, Bin Ahmed IA, Alnasiri AS, Alhirsan WM, Alazmi NNM, Alkhlaf AK, Alderbas JM, Alkhaldi MA. Evaluation of Self-Management Behaviors and Its Correlation with the Metabolic Syndrome among the Type 2 Diabetes Mellitus Patients of Northern Saudi Arabia. Journal of Clinical Medicine. 2024; 13(1):118. https://doi.org/10.3390/jcm13010118
Chicago/Turabian StyleAlsaidan, Aseel Awad, Ashokkumar Thirunavukkarasu, Hassan H. Alhassan, Ibrahim Abdullah Bin Ahmed, Anas Salem Alnasiri, Wejdan Madallah Alhirsan, Nouf Nashmi M. Alazmi, Abdalaziz Khaled Alkhlaf, Jumanah Mohammed Alderbas, and Motaz Abdulsalam Alkhaldi. 2024. "Evaluation of Self-Management Behaviors and Its Correlation with the Metabolic Syndrome among the Type 2 Diabetes Mellitus Patients of Northern Saudi Arabia" Journal of Clinical Medicine 13, no. 1: 118. https://doi.org/10.3390/jcm13010118
APA StyleAlsaidan, A. A., Thirunavukkarasu, A., Alhassan, H. H., Bin Ahmed, I. A., Alnasiri, A. S., Alhirsan, W. M., Alazmi, N. N. M., Alkhlaf, A. K., Alderbas, J. M., & Alkhaldi, M. A. (2024). Evaluation of Self-Management Behaviors and Its Correlation with the Metabolic Syndrome among the Type 2 Diabetes Mellitus Patients of Northern Saudi Arabia. Journal of Clinical Medicine, 13(1), 118. https://doi.org/10.3390/jcm13010118





