Effect of Preoperative Music Therapy Versus Intravenous Midazolam on Anxiety, Sedation and Stress in Stomatology Surgery: A Randomized Controlled Study
Abstract
1. Introduction
2. Methods
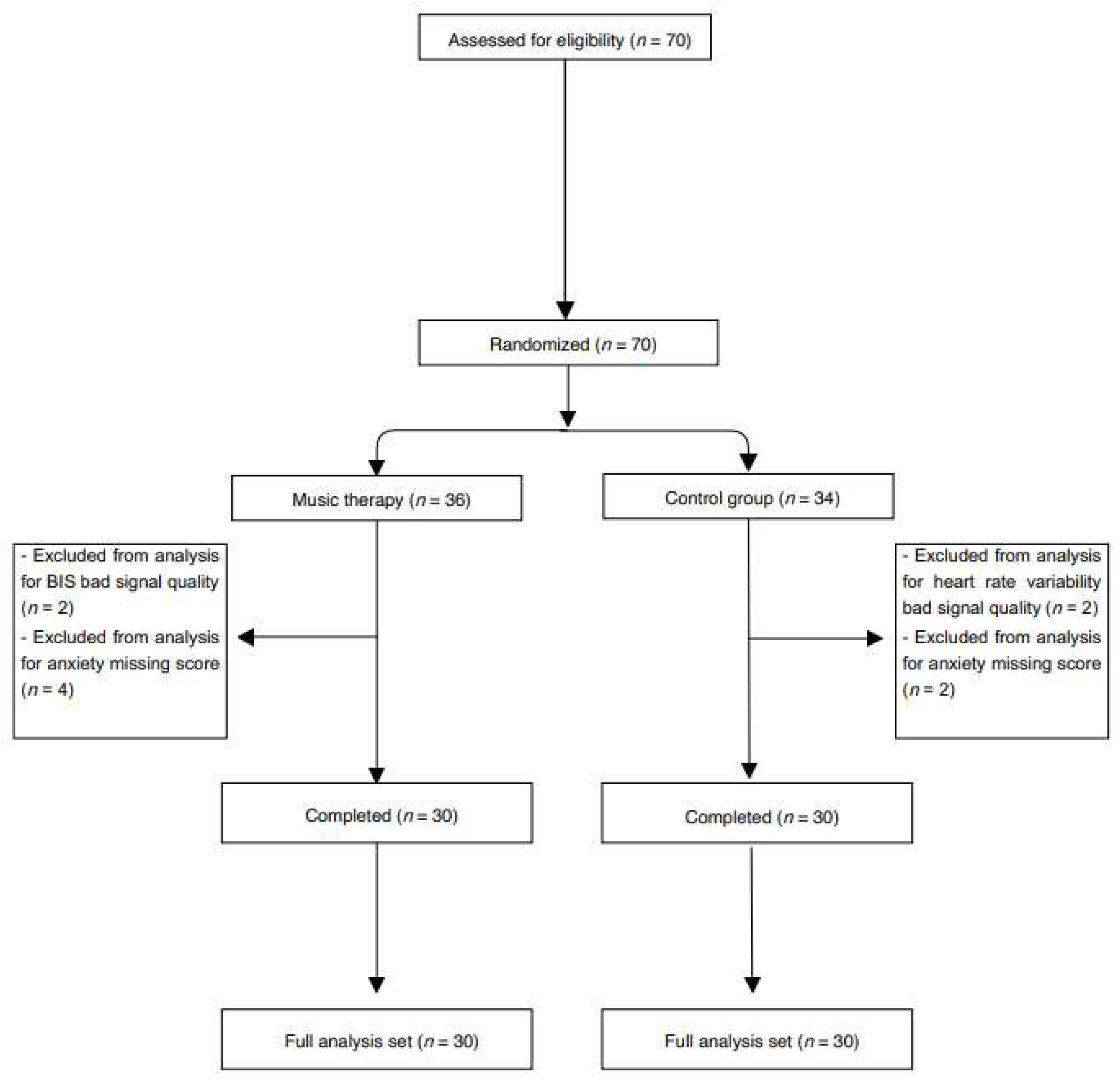
2.1. Participants
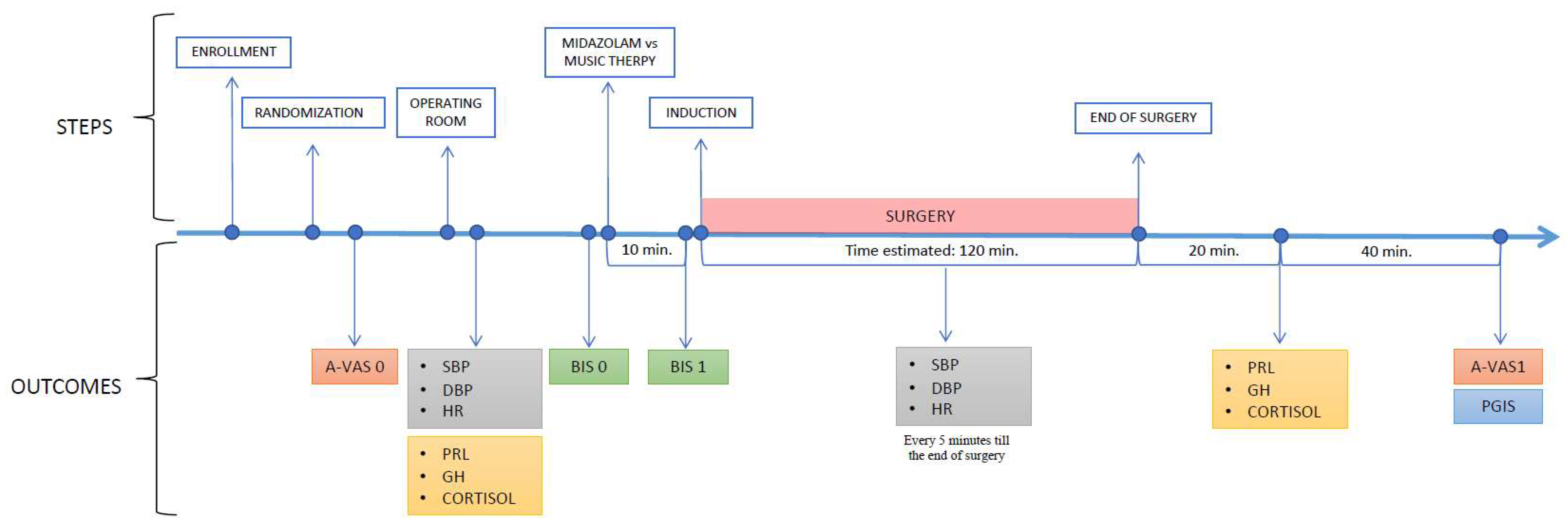
2.2. Procedures
- Firstly, 30 min before surgery, at the bedside, the MTp engaged the patient in an individual brief conversation (10 min) in order to identify their preferred musical genre/songs. Based on both the information collected and specific music elements, the MTp prepared customized playlists to listen to that were tailored to the needs of each patient [26]. The MTp used music that was selected from classical music of the Western tradition, pop, rock, new age, soundtrack and light jazz. A patient-centered approach was employed. Using an interactive relational approach to receptive MT [27,28] that was supplemented by an adaptation of the Bonny method, namely Guided Imagery and Music in the medical setting [29], the MTp tailored the interventions to patients’ individual needs at the time of the surgery.
- After being monitored in the operating room, patients were prepared to listen to the music by the short guided relaxation of the breath (music was matched rhythmically to the rate of breathing, then gradually slowed to encourage slower, deeper breathing) [30], and were invited to find an image with a positive association to focus on. This step took approximately 2 min.
- Music listening, before anesthesia induction, lasted 5 min. Participants listened to music via noise-canceling headphones (BOSE® quiet comfort 35 II) from an iPod®, and the volume was controlled by the MTp.
2.3. Outcomes
2.4. Statistical Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Glossary
| Music therapy | MT |
| Control group | CG |
| Music therapist | MTp |
| Music therapy group | MTG |
| Systolic blood pressure | SBP |
| Diastolic blood pressure | DBP |
| Heart rate | HR |
| Plasma prolactin | PRL |
| Growth hormone | GH |
| Bispectral index | BIS |
| Anxiety visual analogues scale | A-VAS |
| Patient global impression of satisfaction | PGIS |
| Bisphosphonate-related osteonecrosis of the jaws | BRONJI |
References
- Iwasaki, M.; Edmondson, M.; Sakamoto, A.; Ma, D. Anesthesia, surgical stress, and “long-term” outcomes. Acta Anaesthesiol. Taiwanica 2015, 53, 99–104. [Google Scholar] [CrossRef] [PubMed]
- Koelsch, S.; Fuermetz, J.; Sack, U.; Bauer, K.; Hohenadel, M.; Wiegel, M.; Kaisers, U.X.; Heinke, W. Effects of Music Listening on Cortisol Levels and Propofol Consumption during Spinal Anesthesia. Front. Psychol. 2011, 2, 58. [Google Scholar] [CrossRef] [PubMed]
- Cao, X.; Elvir-Lazo, O.L.; White, P.F.; Yumul, R.; Tang, J. An update on pain management for elderly patients undergoing ambulatory surgery. Curr. Opin. Anaesthesiol. 2016, 29, 674–682. [Google Scholar] [CrossRef] [PubMed]
- Brandt, J.; Leong, C. Benzodiazepines and Z-Drugs: An Updated Review of Major Adverse Outcomes Reported on in Epidemiologic Research. Drugs R&D 2017, 17, 493–507. [Google Scholar] [CrossRef]
- Marcantonio, E.R.; Juarez, G.; Goldman, L.; Mangione, C.M.; Ludwig, L.E.; Lind, L.; Katz, N.; Cook, E.F.; Orav, E.J.; Lee, T.H. The relationship of postoperative delirium with psychoactive medications. JAMA 1994, 272, 1518–1522. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, C.P.; Mullins, K.V.; Sidhu, S.S.; Schulman, S.P.; McEvoy, J.W. The on- and off-target effects of morphine in acute coronary syndrome: A narrative review. Am. Heart J. 2016, 176, 114–121. [Google Scholar] [CrossRef]
- Ebrahimi, R.; Shroyer, A.L.; Dennis, P.; Currier, J.; Wischik, D.L. Music Can Reduce the Need for Pharmacologic Conscious Sedation during Invasive Coronary Angiography. J. Invasive Cardiol. 2020, 32, 440–444. [Google Scholar]
- Conway, A.; Rolley, J.; Sutherland, J.R. Midazolam for sedation before procedures. Cochrane Database Syst. Rev. 2016, 2018, CD009491. [Google Scholar] [CrossRef]
- Bradt, J.; Dileo, C. Music interventions for mechanically ventilated patients. Cochrane Database Syst. Rev. 2014, 2018, CD006902. [Google Scholar] [CrossRef] [PubMed]
- Musicoterapia—AIM Musicoterapia. Available online: https://www.aim-musicoterapia.it/musicoterapia/ (accessed on 15 February 2022).
- Stegemann, T.; Geretsegger, M.; Quoc, E.P.; Riedl, H.; Smetana, M. Music Therapy and Other Music-Based Interventions in Pediatric Health Care: An Overview. Medicines 2019, 6, 25. [Google Scholar] [CrossRef] [PubMed]
- Giordano, F.; Zanchi, B.; De Leonardis, F.; Rutigliano, C.; Esposito, F.; Brienza, N.; Santoro, N. The influence of music therapy on preoperative anxiety in pediatric oncology patients undergoing invasive procedures. Arts Psychother. 2020, 68, 101649. [Google Scholar] [CrossRef]
- Chlan, L.L.; Heiderscheit, A.; Skaar, D.J.; Neidecker, M. Economic Evaluation of a Patient-Directed Music Intervention for ICU Patients Receiving Mechanical Ventilatory Support. Crit. Care Med. 2018, 46, 1430–1435. [Google Scholar] [CrossRef]
- Palmer, J.B.; Lane, D.; Mayo, D.; Schluchter, M.; Leeming, R. Effects of Music Therapy on Anesthesia Requirements and Anxiety in Women Undergoing Ambulatory Breast Surgery for Cancer Diagnosis and Treatment: A Randomized Controlled Trial. J. Clin. Oncol. 2015, 33, 3162–3168. [Google Scholar] [CrossRef]
- Fachner, J.C.; Maidhof, C.; Grocke, D.; Pedersen, I.N.; Trondalen, G.; Tucek, G.; Bonde, L.O. “Telling me not to worry…” Hyperscanning and Neural Dynamics of Emotion Processing during Guided Imagery and Music. Front. Psychol. 2019, 10, 1561. [Google Scholar] [CrossRef]
- Lee, J.H. The Effects of Music on Pain: A Meta-Analysis. J. Music Ther. 2016, 53, 430–477. [Google Scholar] [CrossRef] [PubMed]
- Giordano, F.; Messina, R.; Riefolo, A.; Rutigliano, C.; Perillo, T.; Grassi, M.; Santoro, N.; Signorelli, F. Music therapy in children affected by brain tumors. World J. Pediatr. Surg. 2021, 4, e000307. [Google Scholar] [CrossRef]
- Short, A.P.; Gibb, H.P.; Fildes, J.M.; Holmes, C.P. Exploring the Role of Music Therapy in Cardiac Rehabilitation after Cardiothoracic Surgery: A Qualitative Study Using the Bonny Method of Guided Imagery and Music. J. Cardiovasc. Nurs. 2013, 28, E74–E81. [Google Scholar] [CrossRef] [PubMed]
- Bradt, J.; Dileo, C.; Magill, L.; Teague, A. Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst. Rev. 2016, 8, CD006911. [Google Scholar] [CrossRef] [PubMed]
- Bradt, J.; Dileo, C.; Potvin, N. Music for stress and anxiety reduction in coronary heart disease patients. Cochrane Database Syst. Rev. 2013, 2021, CD006577. [Google Scholar] [CrossRef]
- Giordano, F.; Rutigliano, C.; De Leonardis, F.; Rana, R.; Neri, D.; Brienza, N.; Santoro, N. Covid-19 and absence of music therapy: Impact on mother-child dyad during invasive procedures in pediatric oncology. Arts Psychother. 2021, 75, 101839. [Google Scholar] [CrossRef]
- Graff, V.; Cai, L.; Badiola, I.; Elkassabany, N.M. Music versus midazolam during preoperative nerve block placements: A prospective randomized controlled study. Reg. Anesth. Pain Med. 2019, 44, 796–799. [Google Scholar] [CrossRef] [PubMed]
- Fu, V.X.; Oomens, P.; Sneiders, D.; Berg, S.A.V.D.; Feelders, R.A.; Wijnhoven, B.P.; Jeekel, J. The Effect of Perioperative Music on the Stress Response to Surgery: A Meta-analysis. J. Surg. Res. 2019, 244, 444–455. [Google Scholar] [CrossRef]
- Ortega, A.; Gauna, F.; Munoz, D.; Oberreuter, G.; Breinbauer, H.A.; Carrasco, L. Music Therapy for Pain and Anxiety Management in Nasal Bone Fracture Reduction: Randomized Controlled Clinical Trial. Otolaryngol. Neck Surg. 2019, 161, 613–619. [Google Scholar] [CrossRef]
- Dai, W.-S.; Huang, S.-T.; Xu, N.; Chen, Q.; Cao, H. The effect of music therapy on pain, anxiety and depression in patients after coronary artery bypass grafting. J. Cardiothorac. Surg. 2020, 15, 81. [Google Scholar] [CrossRef] [PubMed]
- Robb, S.L.; Carpenter, J.S.; Burns, D.S. Reporting Guidelines for Music-based Interventions. J. Health Psychol. 2011, 16, 342–352. [Google Scholar] [CrossRef]
- Bruscia, K.E.; Grocke, D.E. Guided Imagery and Music: The Bonny Method and Beyond; Barcelona Pub.: New Braunfels, TX, USA, 2002. [Google Scholar]
- Grocke, D.E.; Wigram, T. Receptive Methods in Music Therapy: Techniques and Clinical Applications for Music Therapy Clinicians, Educators and Students, 1st ed.; Jessica Kingsley Publishers: London, UK; Philadelphia, PA, USA, 2007. [Google Scholar]
- Grocke, D.E.; Moe, T. (Eds.) Guided Imagery & Music (GIM) and Music Imagery Methods for Individual and Group Therapy; Jessica Kingsley Publishers: London, UK; Philadelphia, PA, USA, 2015. [Google Scholar]
- Fallek, R.; Corey, K.; Qamar, A.; Vernisie, S.N.; Hoberman, A.; Selwyn, P.A.; Fausto, J.A.; Marcus, P.; Kvetan, V.; Lounsbury, D.W. Soothing the heart with music: A feasibility study of a bedside music therapy intervention for critically ill patients in an urban hospital setting. Palliat. Support. Care 2020, 18, 47–54. [Google Scholar] [CrossRef]
- Bower, A.L.; Ripepi, A.; Dilger, J.; Boparai, N.; Brody, F.J.; Ponsky, J.L. Bispectral index monitoring of sedation during endoscopy. Gastrointest. Endosc. 2000, 52, 192–196. [Google Scholar] [CrossRef] [PubMed]
- Stamenkovic, D.M.; Rancic, N.K.; Latas, M.B.; Neskovic, V.; Rondovic, G.M.; Wu, J.D.; Cattano, D. Preoperative anxiety and implications on postoperative recovery: What can we do to change our history. Minerva Anestesiol. 2018, 84, 1307–1317. [Google Scholar] [CrossRef]
- Bradt, J.; Dileo, C.; Shim, M. Music interventions for preoperative anxiety. Cochrane Database Syst. Rev. 2013, 2013, CD006908. [Google Scholar] [CrossRef]
- Bhakta, P.; Harmon, D. Music therapy as sole anxiolytic may not replace standard pharmaceutical agents, but it is definitely contributory: Our response to article by Graff et al. Reg. Anesth. Pain Med. 2020, 45, 317.1–318. [Google Scholar] [CrossRef]
- Bradt, J.; Teague, A. Music interventions for dental anxiety. Oral Dis. 2018, 24, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.-G.; Cheon, E.-J.; Bai, D.-S.; Lee, Y.H.; Koo, B.-H. Stress and Heart Rate Variability: A Meta-Analysis and Review of the Literature. Psychiatry Investig. 2018, 15, 235–245. [Google Scholar] [CrossRef]
- Ong, W.-Y.; Stohler, C.S.; Herr, D.R. Role of the Prefrontal Cortex in Pain Processing. Mol. Neurobiol. 2019, 56, 1137–1166. [Google Scholar] [CrossRef] [PubMed]
- Salimpoor, V.N.; Benovoy, M.; Larcher, K.; Dagher, A.; Zatorre, R.J. Anatomically distinct dopamine release during anticipation and experience of peak emotion to music. Nat. Neurosci. 2011, 14, 257–262. [Google Scholar] [CrossRef]
- Koelsch, S. Brain correlates of music-evoked emotions. Nat. Rev. Neurosci. 2014, 15, 170–180. [Google Scholar] [CrossRef]
- Ilkkaya, N.K.; Ustun, F.E.; Sener, E.B.; Kaya, C.; Ustun, Y.B.; Koksal, E.; Kocamanoglu, I.S.; Ozkan, F. The Effects of Music, White Noise, and Ambient Noise on Sedation and Anxiety in Patients under Spinal Anesthesia during Surgery. J. Perianesth. Nurs. 2014, 29, 418–426. [Google Scholar] [CrossRef] [PubMed]
- Caponnetto, P.; LaMattina, G.; Quattropani, M.C. Music therapy and psychological-clinical impact in surgery: A systematic review. Health Psychol. Res. 2022, 10, 38615. [Google Scholar] [CrossRef] [PubMed]
- Aitken, J.C.; Wilson, S.; Coury, D.; Moursi, A.M. The effect of music distraction on pain, anxiety and behavior in pediatric dental patients. Pediatr. Dent. 2002, 24, 114–118. [Google Scholar]
- Jacquier, S.; Nay, M.-A.; Muller, G.; Muller, L.; Mathonnet, A.; Lefèvre-Benzekri, D.; Bretagnol, A.; Barbier, F.; Kamel, T.; Runge, I.; et al. Effect of a Musical Intervention during the Implantation of a Central Venous Catheter or a Dialysis Catheter in the Intensive Care Unit: A Prospective Randomized Pilot Study. Anesth. Analg. 2022, 134, 781–790. [Google Scholar] [CrossRef]
- Kühlmann, A.Y.R.; van Rosmalen, J.; Staals, L.M.; Keyzer-Dekker, C.M.G.; Dogger, J.; de Leeuw, T.G.; van der Toorn, F.; Jeekel, J.; Wijnen, R.M.H.; van Dijk, M. Music Interventions in Pediatric Surgery (The Music under Surgery In Children Study): A Randomized Clinical Trial. Anesth. Analg. 2020, 130, 991–1001. [Google Scholar] [CrossRef]
- Thompson, W.F. Music, Thought, and Feeling: Understanding the Psychology of Music; Oxford University Press: Oxford, UK, 2009. [Google Scholar]
- Bradt, J.; Potvin, N.; Kesslick, A.; Shim, M.; Radl, D.; Schriver, E.; Gracely, E.J.; Komarnicky-Kocher, L.T. The impact of music therapy versus music medicine on psychological outcomes and pain in cancer patients: A mixed methods study. Support. Care Cancer 2015, 23, 1261–1271. [Google Scholar] [CrossRef] [PubMed]
- Thaut, M.H.; Davis, W.B. The Influence of Subject-Selected versus Experimenter-Chosen Music on Affect, Anxiety, and Relaxation. J. Music Ther. 1993, 30, 210–223. [Google Scholar] [CrossRef]
- Dahlem, C.; Monteiro, C.; Mendes, E.; Martinho, J.; Oliveira, C.; Bettencourt, M.; Coelho, M.; Neves, P.; Azevedo, L.; Granja, C. Modulating Influence of State Anxiety on the Effect of Midazolam on Postsurgical Pain. J. Clin. Med. 2023, 12, 2669. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Music Therapy (n = 30) | Control (n = 30) |
|---|---|---|
| Age (years) | 61 ± 12 | 61 ± 12 |
| Females, n (%) | 28 (47.5) | 26 (17.5) |
| ASA | ||
| I, N (%) | 4 (13.3) | 3 (10) |
| II, n (%) | 16 (53.4) | 12 (40) |
| III, n (%) | 10 (33.3) | 15 (50) |
| Surgery | ||
| BRONJ, n (%) | 11 (12.5) | 12 (35) |
| Oral cystectomy, n (%) | 1 (45) | 2 (62.5) |
| Carcinoma, n (%) | 9 (20) | 10 (17.5) |
| Others, n (%) | 9 (15) | 6 (15) |
| Time of surgery (min) | 117 ± 22 | 130 ± 23 |
| Outcomes | Music Therapy (n = 30) | Control Group (n = 30) | p-Value |
|---|---|---|---|
| (a) Pre-interventions | |||
| Prolactin (mIU/L) | 355.7 ± 504.5 | 239.76 ± 105.2 | 0.22 |
| GH (ng/mL) | 0.1 ± 1.26 | 1.7 ± 3.12 | 0.24 |
| Cortisol (mcg/L) | 13.7 ± 6 | 14.8 ± 6.5 | 0.77 |
| SBP (mm Hg) | 140.6 ± 14.6 | 137.7 ± 20.6 | 0.53 |
| DBP (mm Hg) | 77.4 ± 8.9 | 77.1 ± 7.1 | 0.85 |
| HR (bpm) | 83.9 ± 9.2 | 82 ± 9.4 | 0.79 |
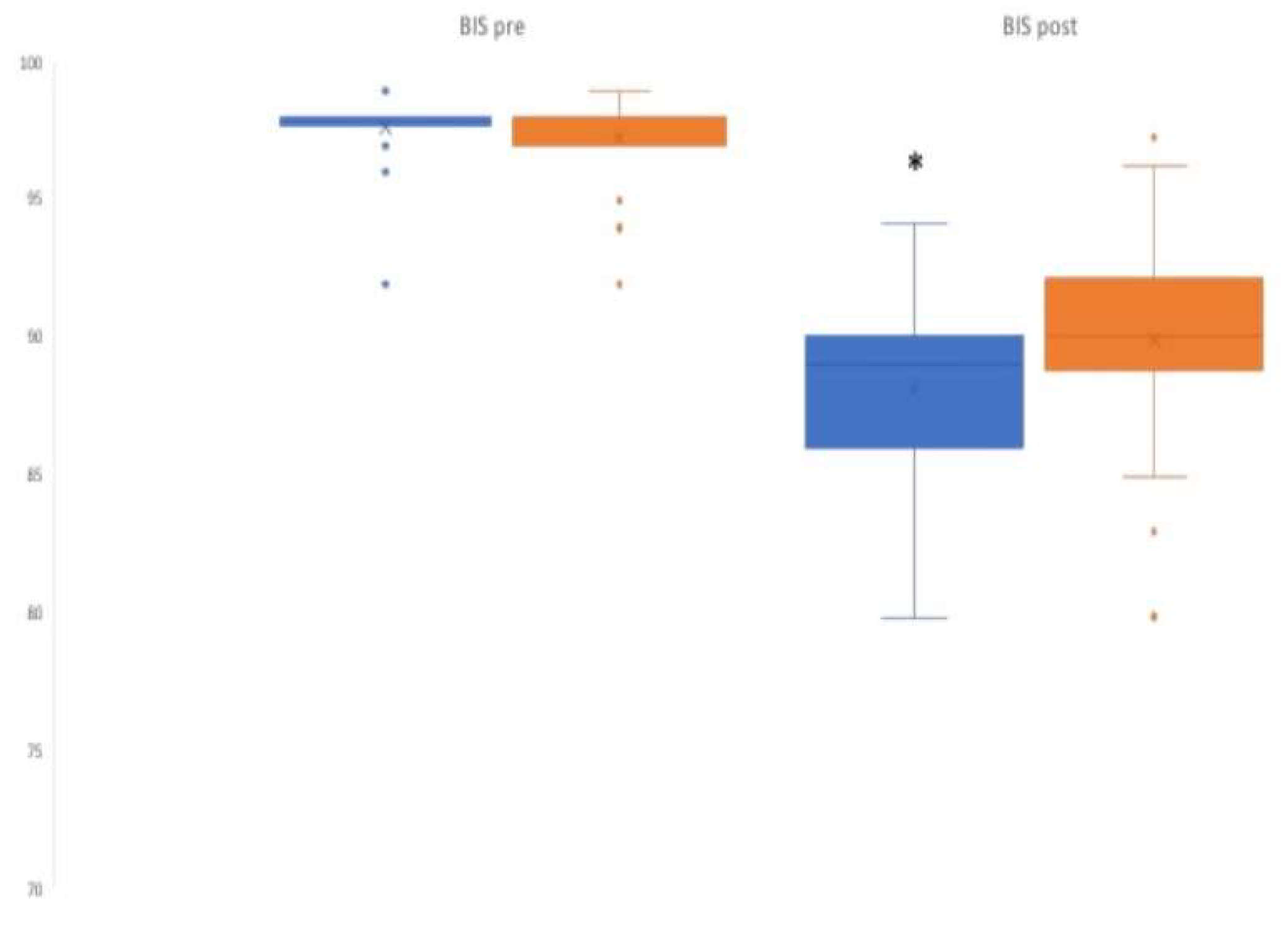
| BIS (median) | 98 | 98 | 0.28 |
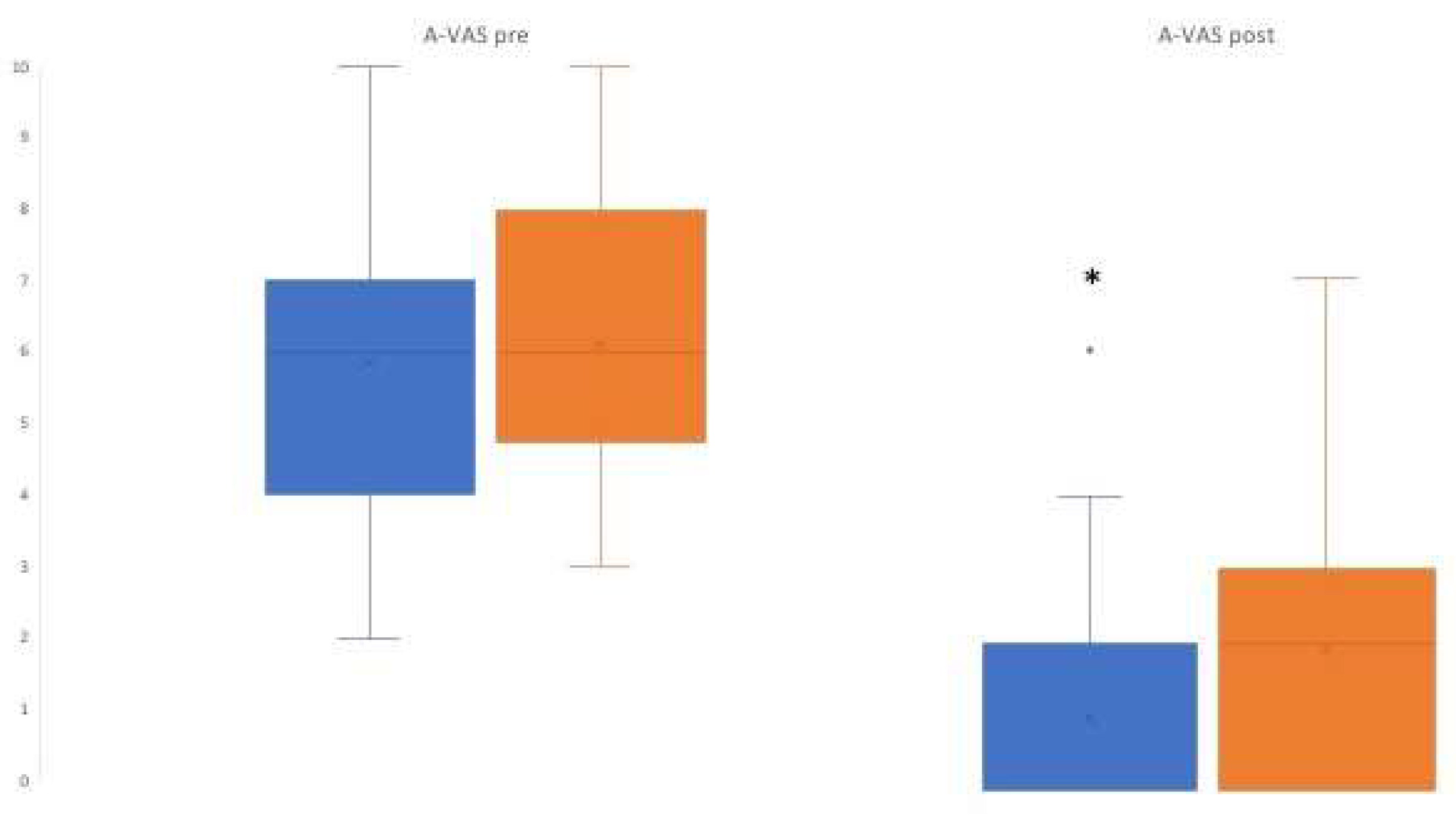
| A-VAS (median) | 6 | 6 | 0.67 |
| (b) Post-interventions | |||
| Prolactin (mIU/L) | 1880 ± 1020 | 1730 ± 0.92 | 0.54 |
| GH (ng/mL) | 1.51 ± 3.93 | 1.10 ± 2.04 | 0.82 |
| Cortisol (mcg/L) | 23.1 ± 20.1 | 20.6 ± 18 | 0.77 |
| SBP (mm Hg) | 124 ± 17 | 122 ± 13 | 0.98 |
| DBP (mm Hg) | 77.4 ± 8.9 | 77.1 ± 7.1 | 0.85 |
| HR (bpm) | 75.5 ± 9.6 | 76.1 ± 7.7 | 0.77 |
| BIS (median) | 89 | 90 | 0.02 * |
| A-VAS (median) | 0 | 2 | 0.01 * |
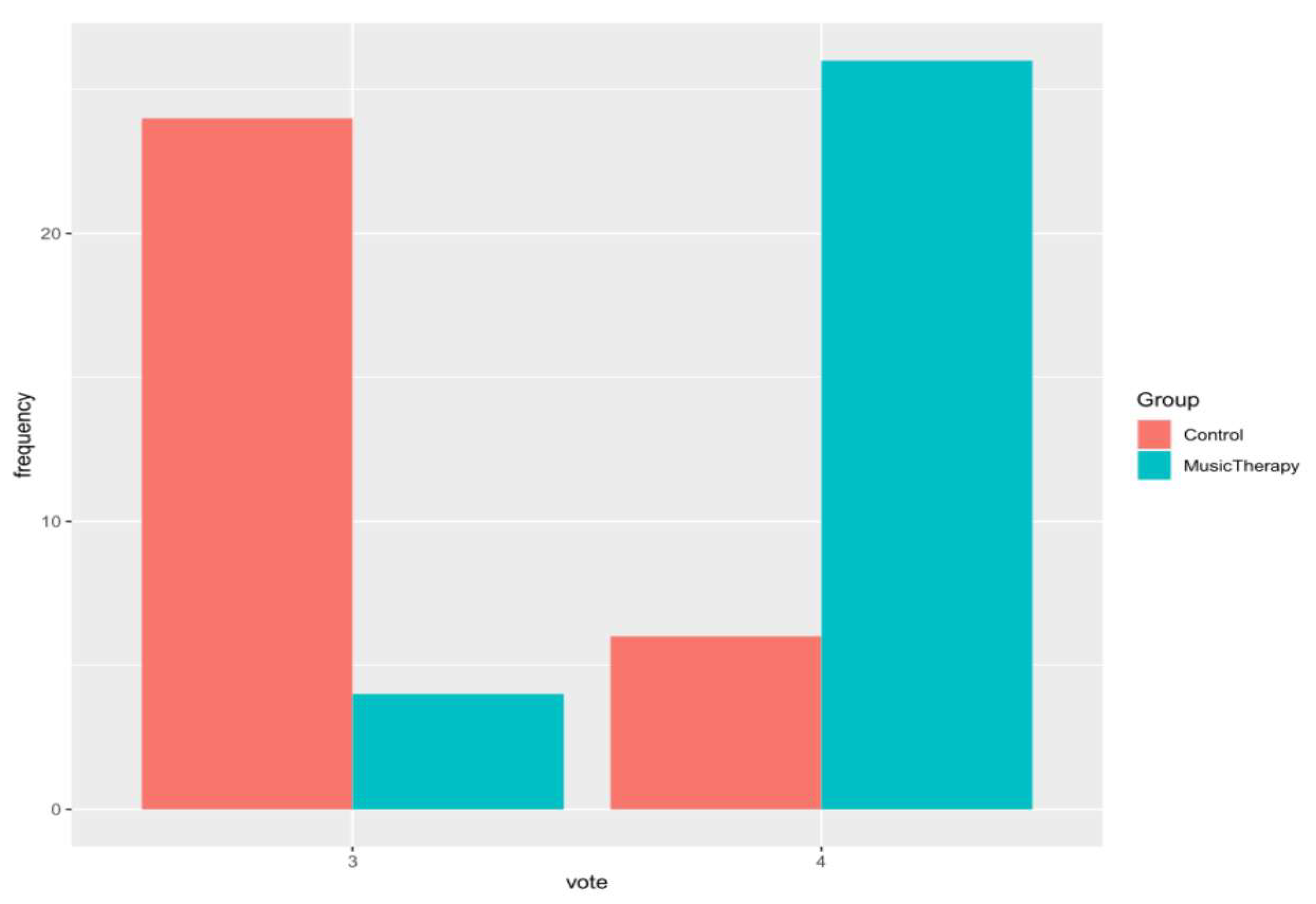
| Satisfaction score 4 (n, %) | 26 (87%) | 6 (20%) | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giordano, F.; Giglio, M.; Sorrentino, I.; Dell’Olio, F.; Lorusso, P.; Massaro, M.; Tempesta, A.; Limongelli, L.; Selicato, L.; Favia, G.; et al. Effect of Preoperative Music Therapy Versus Intravenous Midazolam on Anxiety, Sedation and Stress in Stomatology Surgery: A Randomized Controlled Study. J. Clin. Med. 2023, 12, 3215. https://doi.org/10.3390/jcm12093215
Giordano F, Giglio M, Sorrentino I, Dell’Olio F, Lorusso P, Massaro M, Tempesta A, Limongelli L, Selicato L, Favia G, et al. Effect of Preoperative Music Therapy Versus Intravenous Midazolam on Anxiety, Sedation and Stress in Stomatology Surgery: A Randomized Controlled Study. Journal of Clinical Medicine. 2023; 12(9):3215. https://doi.org/10.3390/jcm12093215
Chicago/Turabian StyleGiordano, Filippo, Mariateresa Giglio, Irene Sorrentino, Fabio Dell’Olio, Pantaleo Lorusso, Maria Massaro, Angela Tempesta, Luisa Limongelli, Laura Selicato, Gianfranco Favia, and et al. 2023. "Effect of Preoperative Music Therapy Versus Intravenous Midazolam on Anxiety, Sedation and Stress in Stomatology Surgery: A Randomized Controlled Study" Journal of Clinical Medicine 12, no. 9: 3215. https://doi.org/10.3390/jcm12093215
APA StyleGiordano, F., Giglio, M., Sorrentino, I., Dell’Olio, F., Lorusso, P., Massaro, M., Tempesta, A., Limongelli, L., Selicato, L., Favia, G., Varrassi, G., & Puntillo, F. (2023). Effect of Preoperative Music Therapy Versus Intravenous Midazolam on Anxiety, Sedation and Stress in Stomatology Surgery: A Randomized Controlled Study. Journal of Clinical Medicine, 12(9), 3215. https://doi.org/10.3390/jcm12093215








