Acceptance of Assistive Technology by Users with Motor Disabilities Due to Spinal Cord or Acquired Brain Injuries: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Study Selection Criteria
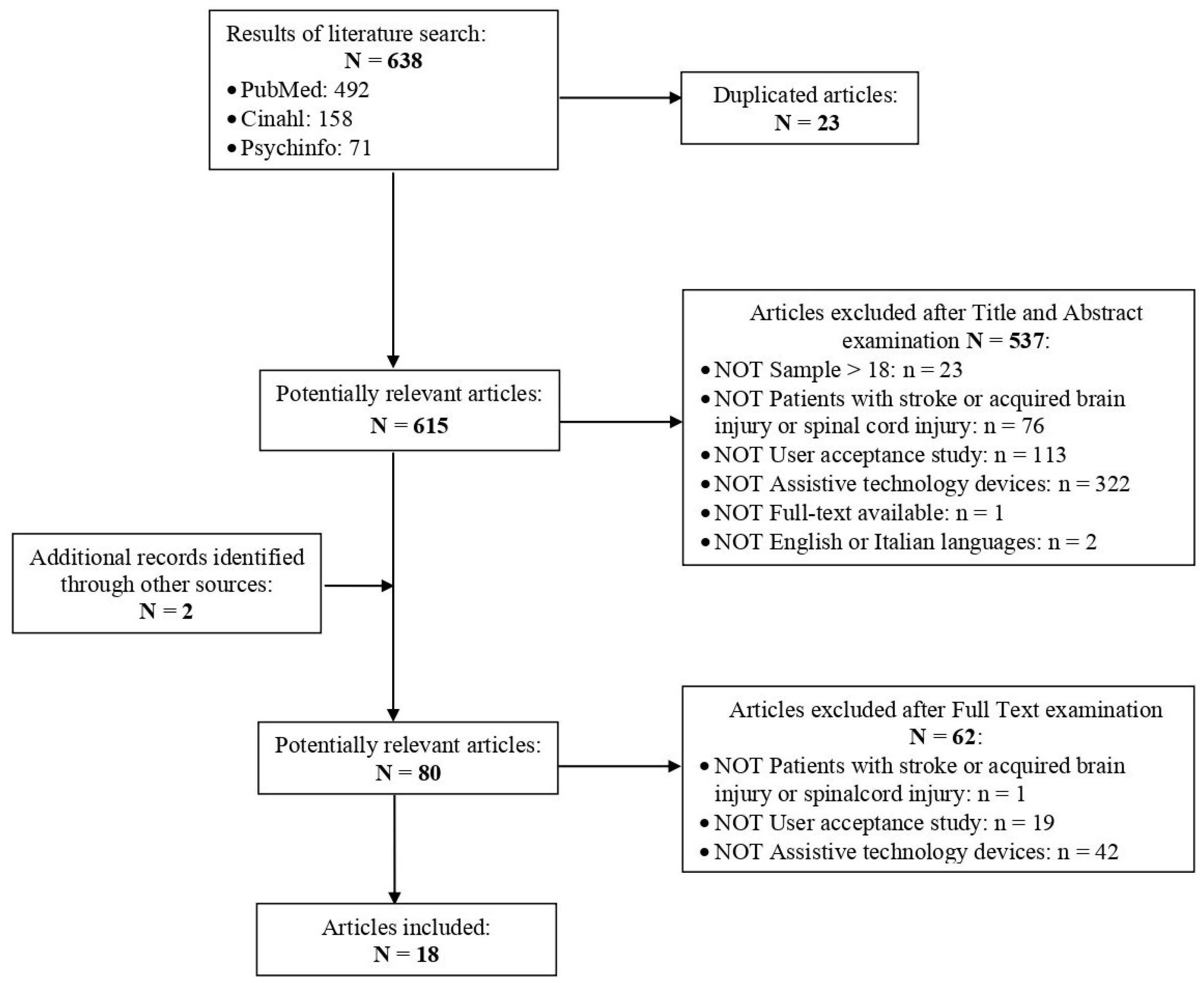
2.2. Search Strategy
2.3. Search Outcome
2.4. Methodological Research Quality Assessment
3. Results
3.1. Research Quality Assessment
3.2. Sample Characteristics
| Study | Sample (N) | Type of Injury | Type of Assistive Technology: Allocentric vs. Egocentric | Measures | Outcomes | Quality Assessment |
|---|---|---|---|---|---|---|
| [30] | 9 | Spinal cord injury | Egocentric—Hand exoskeleton (HX). | Ah-hoc test: comfort, safety, ease to use (6-point Likert). | Comfort (M = 4.17 SD = 4.92) Safety (M = 4.35 SD = 1.38) Ease of use (M = 3.12 SD = 1.81). Qualitative: modify the size and weight. | 0.53 |
| [31] | 19 | Spinal cord injury | Egocentric—REX walking aid. | Ad-hoc test: comfort, safety, ease to use, engagement (7-point Likert). | Total: M = 5.86 SD = 1.20 | 0.42 |
| [32] | 29 | Tetraplegic: Spinal cord injury (n = 23), stroke (n = 2), cerebral palsy (n = 1), arthrogryposis (n = 1), quadruple amputee (n = 1), spinal muscular atrophy (n = 1). | Allocentric—Synthetic autonomous Majordomo robot (SAM). | Ad-hoc test: satisfaction, learnability, confidence in the system, ease to use (5-point Likert). | Satisfaction (M = 3.97 SD = 1.03), learnability (M = 4.21 SD = 0.7), Trust (M = 3.31 SD = 1.69), ease to use (M = 4.62 SD = 0.3). | 0.5 |
| [27] | 262 | * Multiple sclerosis (n = 73), cerebral palsy (n = 37), and spinal cord injury (n = 31) | Allocentric—Electrically powered wheelchairs (EPWs). | Ad-hoc test: usability, safety, reliability, and satisfaction (5-point Likert). | Usability: (M = 4.16 SD = 0.95), safety (M = 4.3 SD = 0.9), reliability (M = 4.3 SD = 0.8), and overall satisfaction (M = 4.2 SD = 0.8). | 0.5 |
| [20] | 13 | Stroke (n = 7), spinal cord injury (n = 6) | Egocentric—mobile, patient-adapted, robot-assisted gait rehabilitation system (MOPASS). | SUS scale, Ad-hoc test: acceptance (score 0–100). | Usability: M = 54 | 0.35 |
| [33] | 17 | Spinal cord injury | Allocentric—SAM. | Ad-hoc test: usability, (a) success rate for achieving the task, (b) success rate for completing the task without mistakes, (c) Success rate for completing the task on time (score 0–100). | Usability: M = 82. 94.1% were satisfied with the control mode, 76.5% were confident, 70.6% were interest in using it at home. | 0.4 |
| [34] | 14 | Spinal cord injury | Egocentric—EKSO or OEAGT robotic exoskeleton. | Ad-hoc test: satisfaction, learnability, usefulness, safety, and motivation to use (score 0–100). | Satisfaction (M = 81.2 SD = 20.1), learnability (M = 76,61 SD = 19.07), usefulness (M = 94.3 SD = 27.93); safety (M = 26 SD = 40.9); motivation (M = 91.2 SD= 15.6). | 0.4 |
| [39] | 46 | Stroke | EKSO or OEAGT. | Technology acceptance model test (7-point Likert). | Total: M = 4.85 SD = 1.71 | 0.42 |
| [26] | 6 | Spinal cord injury | Allocentric—Adaptive head motion control for user-friendly support (AMiCUS). | Ad-hoc test: ease to use (5-point Likert). | Total: M = 4.21 SD = 0.91 | 0.42 |
| [23] | 6 | Spinal cord injury | Allocentric—ASIBOT. | Quebec user evaluation of satisfaction test (5-point Likert) | Average for drinking action 0.91, brushing teeth 0.49. | 0.5 |
| [22] | 28 | Spinal cord injury | Allocentric—Robotic locomotor exoskeleton. | Focus group: experiences and perspectives, benefits and barriers, concerns and limitations, and suggestions. | Robotic exoskeletons were useful in therapy settings but not for daily life activities. Dissatisfaction with the devices due to an inability to use them in autonomy and safely. | 0.8 |
| [21] | 20 | Stroke (n = 10), multiple sclerosis (n = 10) | Egocentric—SEM™ Glove. | Semi-structured interview: usability. | Difficult to use due to the complexity of everyday life where a single activity may involve grasp, grip, and pinch. Limited ability to coordinate finger movements. | 0.8 |
| [38] | 1 | Stroke | Egocentric—Proof-of-concept glove. | Semi-structured interview: usability, acceptability, satisfaction. | Patients are motivated to use for training purpose, but they feel quite uncomfortable. The grasp and velocity must be adjustable to be appropriate for each patient’s needs. | 0.7 |
| [37] | 7 | Spinal cord injury (n = 4), Multiple sclerosis (n = 3). | Egocentric—REX walking aid. | Ad-hoc test: satisfaction (5-point Likert). | High satisfaction with ease of transferring in and out of the REX (M = 1.86; SD = 1.46) and with itsappearance (M = 1.83; SD = 0.98). Low satisfied with the ability to carry an item while using the Ekso (M = 4; SD = 0.71), but more satisfied with its transportability (M = 2.8; SD = 0.84). | 0.5 |
| [25] | 1 | Spinal cord injury | EKSO or OEAGT robotic exoskeleton. | Quebec user evaluation of satisfaction test (5-point Likert—adaptation) | Total: M = 3.8; SD = 1 | 0.4 |
| [35] | 21 | Spinal cord injury | Egocentric—H2 exoskeleton. | Ad-hoc test: comfort, fatigue, enjoyment, motivation. | Median results: comfort = 6, fatigue = 3, enjoyment = 6, advantages = 5, motivation = 6 | 0.42 |
| [24] | 37 | Stroke | EKSO or OEAGT robotic exoskeleton. | Intrinsic motivation inventory (IMI) (7-point Likert), credibility/expectancy questionnaire (CEQ) (score 0–100) | IMI (M = 74% SD = 17.16%), CEQ (M = 75% SD = 18.5). | 0.5 |
| [36] | 5 | Spinal cord injury | Egocentric—driven gait orthosis (DGO). | Intrinsic motivation inventory (IMI) (7-point Likert), credibility/expectancy questionnaire (CEQ) (score 0–100) (score 0–100). | IMI (M = 65% SD = 3.25%), CEQ (M = 60.7% SD = 20.6). | 0.53 |
3.3. Assistive Technologies Characteristics
Assistive Technologies Testing Setting
3.4. Method to Evaluate Users’ Acceptance
3.4.1. Quantitative Measures
| Construct | Items | Reference |
|---|---|---|
| Comfort |
| [30] |
| [31] | |
| Safety |
| [30] |
| [31] | |
| [27] | |
| [34] | |
| Ease to use |
| [30] |
| [31] | |
| [32] | |
| [27] | |
| [26] | |
| Engagement |
| [31] |
| Size, sound, speed |
| [31] |
| Satisfaction |
| [31] |
| [32] | |
| [27] | |
| [34] | |
| [25] | |
| [37] | |
| Learnability |
| [32] |
| [34] | |
| Trust |
| [32] |
| Usefulness (Perceived health benefits) |
| [34] |
| [26] | |
| Motivation |
| [34] |
| Others ad-hoc measures | ||
| [33] | |
| [35] | |
3.4.2. Qualitative Measures
3.5. Main Constructs Outcomes
3.5.1. Satisfaction
3.5.2. Ease to Use
3.5.3. Comfort
3.5.4. Safety
3.5.5. Learnability
3.5.6. Usefulness
3.5.7. Motivation
4. Discussion
5. Critical Aspects
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization; World Bank (Eds.) World Report on Disability; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Strandberg, T. Adults with acquired traumatic brain injury: Experiences of a changeover process and consequences in everyday life. Soc. Work Health Care 2009, 48, 276–297. [Google Scholar] [CrossRef]
- Barrett, D.; Kamenov, K.; Pearce, E.; Cieza, A. Global Report on Health Equity for Persons with Disabilities; World Health Organization: Geneva, Switzerland, 2022. [Google Scholar]
- Kauhanen, M.-L.; Korpelainen, J.T.; Hiltunen, P.; Nieminen, P.; Sotaniemi, K.A.; Myllylä, V. Domains and determinants of quality of life after stroke caused by brain infarction. Arch. Phys. Med. Rehabil. 2000, 81, 1541–1546. [Google Scholar] [CrossRef] [PubMed]
- Plaza, I.; Martín, L.; Martin, S.; Medrano, C. Mobile applications in an aging society: Status and trends. J. Syst. Softw. 2011, 84, 1977–1988. [Google Scholar] [CrossRef]
- Darcy, S.; Green, J.; Maxwell, H. I’ve got a mobile phone too! Hard and soft assistive technology customization and supportive call centres for people with disability. Disabil. Rehabil. Assist. Technol. 2017, 12, 341–351. [Google Scholar] [CrossRef] [PubMed]
- Cook, A.M.; Polgar, J.M. Cook and Hussey’s Assistive Technologies-E-Book: Principles and Practice; Elsevier Health Sciences: Amsterdam, The Netherlands, 2013. [Google Scholar]
- Madara Marasinghe, K. Assistive technologies in reducing caregiver burden among informal caregivers of older adults: A systematic review. Disabil. Rehabil. Assist. Technol. 2016, 11, 353–360. [Google Scholar] [CrossRef]
- Mirza, M.; Gossett, A.Z.; Borsci, S.; Federici, S.; Scherer, M.J.; Federici, S.; Scherer, M.J. The assessment of the environments of use: Accessibility, sustainability, and universal design. In Assistive Technology Assessment Handbook; CRC: Boca Raton, FL, USA, 2012; pp. 67–81. [Google Scholar]
- Yousafzai, S.Y.; Foxall, G.R.; Pallister, J.G. Technology acceptance: A meta-analysis of the TAM: Part 1. J. Model. Manag. 2007, 2, 251–280. [Google Scholar] [CrossRef]
- van Ommeren, A.L.; Smulders, L.C.; Prange-Lasonder, G.B.; Buurke, J.H.; Veltink, P.H.; Rietman, J.S. Assistive Technology for the Upper Extremities After Stroke: Systematic Review of Users’ Needs. JMIR Rehabil. Assist. Technol. 2018, 5, e10510. [Google Scholar] [CrossRef]
- Federici, S.; Artegiani, F.; Pigliautile, M.; Antonelli, P.; Diotallevi, D.; Ritacco, I.; Maschke, R. Enhancing psychological sexual health of people with spinal cord injury and their partners in an Italian Unipolar Spinal Unit: A pilot data study. Front. Psychol. 2019, 10, 754. [Google Scholar] [CrossRef]
- Giesbrecht, E.D. Application of the Human Activity Assistive Technology model for occupational therapy research. Aust. Occup. Ther. J. 2013, 60, 230–240. [Google Scholar] [CrossRef]
- Federici, S.; Scherer, M. Assistive Technology Assessment Handbook; CRC Press: Boca Raton, FL, USA, 2012. [Google Scholar]
- Heerink, M.; Kröse, B.; Evers, V.; Wielinga, B. Assessing acceptance of assistive social agent technology by older adults: The almere model. Int. J. Soc. Robot. 2010, 2, 361–375. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Methley, A.M.; Campbell, S.; Chew-Graham, C.; McNally, R.; Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv. Res. 2014, 14, 579. [Google Scholar] [CrossRef] [PubMed]
- Bramer, W.M.; Rethlefsen, M.L.; Kleijnen, J.; Franco, O.H. Optimal database combinations for literature searches in systematic reviews: A prospective exploratory study. Syst. Rev. 2017, 6, 245. [Google Scholar] [CrossRef] [PubMed]
- Kmet, L.M.; Cook, L.S.; Lee, R.C. Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields; Alberta Heritage Foundation for Medical Research: Edmonton, AB, Canada, 2004. [Google Scholar]
- Eicher, C.; Haesner, M.; Spranger, M.; Kuzmicheva, O.; Gräser, A.; Steinhagen-Thiessen, E. Usability and acceptability by a younger and older user group regarding a mobile robot-supported gait rehabilitation system. Assist. Technol. 2019, 31, 25–33. [Google Scholar] [CrossRef]
- Palmcrantz, S.; Plantin, J.; Borg, J. Factors affecting the usability of an assistive soft robotic glove after stroke or multiple sclerosis. J. Rehabil. Med. (Stift. Rehabiliteringsinform.) 2020, 52, 1–12. [Google Scholar] [CrossRef]
- Kinnett-Hopkins, D.; Mummidisetty, C.K.; Ehrlich-Jones, L.; Crown, D.; Bond, R.A.; Applebaum, M.H.; Jayaraman, A.; Furbish, C.; Forrest, G.; Field-Fote, E.; et al. Users with spinal cord injury experience of robotic Locomotor exoskeletons: A qualitative study of the benefits, limitations, and recommendations. J. Neuroeng. Rehabil. 2020, 17, 124. [Google Scholar] [CrossRef]
- Jardón, A.; Gil, Á.M.; de la Peña, A.I.; Monje, C.A.; Balaguer, C. Usability assessment of ASIBOT: A portable robot to aid patients with spinal cord injury. Disabil. Rehabil. Assist. Technol. 2011, 6, 320–330. [Google Scholar] [CrossRef]
- Swinnen, E.; Lefeber, N.; Willaert, W.; De Neef, F.; Bruyndonckx, L.; Spooren, A.; Michielsen, M.; Ramon, T.; Kerckhofs, E. Motivation, expectations, and usability of a driven gait orthosis in stroke patients and their therapists. Top. Stroke Rehabil. 2017, 24, 299–308. [Google Scholar] [CrossRef]
- Quiles, V.; Ferrero, L.; Ianez, E.; Ortiz, M.; Megia, A.; Comino, N.; Gil-Agudo, A.M.; Azorin, J.M. Usability and acceptance of using a lower-limb exoskeleton controlled by a BMI in incomplete spinal cord injury patients: A case study. In Proceedings of the 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 20–24 July 2020. [Google Scholar] [CrossRef]
- Jackowski, A.; Gebhard, M.; Thietje, R. Head Motion and Head Gesture-Based Robot Control: A Usability Study. IEEE Trans. Neural. Syst. Rehabil. Eng. A Publ. IEEE Eng. Med. Biol. Soc. 2018, 26, 161–170. [Google Scholar] [CrossRef]
- Dolan, M.J.; Henderson, G.I. Control devices for electrically powered wheelchairs: Prevalence, defining characteristics and user perspectives. Disabil. Rehabil. Assist. Technol. 2017, 12, 618–624. [Google Scholar] [CrossRef]
- Devine, P.G.; Baker, S.M. Measurement of racial stereotype subtyping. Personal. Soc. Psychol. Bull. 1991, 17, 44–50. [Google Scholar] [CrossRef]
- Bangor, A.; Kortum, P.T.; Miller, J.T. An empirical evaluation of the system usability scale. Int. J. Hum.—Comput. Interact. 2008, 24, 574–594. [Google Scholar] [CrossRef]
- Almenara, M.; Cempini, M.; Gómez, C.; Cortese, M.; Martín, C.; Medina, J.; Vitiello, N.; Opisso, E. Usability test of a hand exoskeleton for activities of daily living: An example of user-centered design. Disabil. Rehabil. Assist. Technol. 2017, 12, 84–96. [Google Scholar] [CrossRef] [PubMed]
- Birch, N.; Graham, J.; Priestley, T.; Heywood, C.; Sakel, M.; Gall, A.; Nunn, A.; Signal, N. Results of the first interim analysis of the RAPPER II trial in patients with spinal cord injury: Ambulation and functional exercise programs in the REX powered walking aid. J. Neuroeng. Rehabil. 2017, 14, 60. [Google Scholar] [CrossRef] [PubMed]
- Coignard, P.; Departe, J.P.; Remy Neris, O.; Baillet, A.; Bar, A.; Drean, D.; Verier, A.; Leroux, C.; Belletante, P.; Le Guiet, J.L. ANSO study: Evaluation in an indoor environment of a mobile assistance robotic grasping arm. Ann. Phys. Rehabil. Med. 2013, 56, 621–633. [Google Scholar] [CrossRef] [PubMed]
- Fattal, C.; Leynaert, V.; Laffont, I.; Baillet, A.; Enjalbert, M.; Leroux, C. SAM, an assistive robotic device dedicated to helping persons with quadriplegia: Usability study. Int. J. Soc. Robot. 2019, 11, 89–103. [Google Scholar] [CrossRef]
- Gagnon, D.H.; Vermette, M.; Duclos, C.; Aubertin-Leheudre, M.; Ahmed, S.; Kairy, D. Satisfaction and perceptions of long-term manual wheelchair users with a spinal cord injury upon completion of a locomotor training program with an overground robotic exoskeleton. Disabil. Rehabil. Assist. Technol. 2019, 14, 138–145. [Google Scholar] [CrossRef]
- Stampacchia, G.; Rustici, A.; Bigazzi, S.; Gerini, A.; Tombini, T.; Mazzoleni, S. Walking with a powered robotic exoskeleton: Subjective experience, spasticity and pain in spinal cord injured persons. NeuroRehabilitation 2016, 39, 277–283. [Google Scholar] [CrossRef]
- Vanmulken DA, M.M.; Spooren AI, F.; Bongers HM, H.; Seelen HA, M. Robot-assisted task-oriented upper extremity skill training in cervical spinal cord injury: A feasibility study. Spinal Cord 2015, 53, 547–551. [Google Scholar] [CrossRef]
- Poritz, J.M.P.; Taylor, H.B.; Francisco, G.; Chang, S.-H. User satisfaction with lower limb wearable robotic exoskeletons. Disabil. Rehabil. Assist. Technol. 2019, 15, 322–327. [Google Scholar] [CrossRef]
- Park, W.; Jeong, W.; Kwon, G.-H.; Kim, Y.-H.; Kim, L. A rehabilitation device to improve the hand grasp function of stroke patients using a patient-driven approach. In Proceedings of the 2013 IEEE 13th International Conference on Rehabilitation Robotics (ICORR), Seattle, WA, USA, 24–26 June 2013. [Google Scholar] [CrossRef]
- Goffredo, M.; Guanziroli, E.; Pournajaf, S.; Gaffuri, M.; Gasperini, G.; Filoni, S.; Baratta, S.; Damiani, C.; Franceschini, M.; Molteni, F. Overground wearable powered exoskeleton for gait training in subacute stroke subjects: Clinical and gait assessments. Eur. J. Phys. Rehabil. Med. 2019, 55, 710–721. [Google Scholar] [CrossRef] [PubMed]
- Dishaw, M.T.; Strong, D.M. Extending the technology acceptance model with task–technology fit constructs. Inf. Manag. 1999, 36, 9–21. [Google Scholar] [CrossRef]
- Markland, D.; Hardy, L. On the factorial and construct validity of the Intrinsic Motivation Inventory: Conceptual and operational concerns. Res. Q. Exerc. Sport 1997, 68, 20–32. [Google Scholar] [CrossRef] [PubMed]
- Malhotra, Y.; Galletta, D.F. Extending the technology acceptance model to account for social influence: Theoretical bases and empirical validation. In Proceedings of the 32nd Annual Hawaii International Conference on Systems Sciences, 1999, HICSS-32, Abstracts and CD-ROM of Full Papers, Maui, HI, USA, 5–8 January 1999. [Google Scholar]
- Demers, L.; Weiss-Lambrou, R.; Ska, B. The Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST 2.0): An overview and recent progress. Technol. Disabil. 2002, 14, 101–105. [Google Scholar] [CrossRef]
- Rybicka, J.; Tiwari, A.; Leeke, G.A. Technology readiness level assessment of composites recycling technologies. J. Clean. Prod. 2016, 112, 1001–1012. [Google Scholar] [CrossRef]
- Ottoboni, G.; Gallelli, T.; Mariani, E.; Rebecca Soluri, V.; Nunziata, S.; Tessari, A.; Savary, J.P.; Chattat, R. Remote home physical training for seniors: Guidelines from the AAL-supported MOTION project. Eur. J. Ageing 2018, 16, 25–37. [Google Scholar] [CrossRef]
- Ottoboni, G.; Porta, F.L.; Piperno, R.; Bosco, A.; Fattori, P.; Tessari, A. A Multifunctional Adaptive and Interactive AI system to support people living with stroke, acquired brain or spinal cord injuries: A study protocol. PLoS ONE 2022, 17, e0266702. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ventura, S.; Ottoboni, G.; Pappadà, A.; Tessari, A. Acceptance of Assistive Technology by Users with Motor Disabilities Due to Spinal Cord or Acquired Brain Injuries: A Systematic Review. J. Clin. Med. 2023, 12, 2962. https://doi.org/10.3390/jcm12082962
Ventura S, Ottoboni G, Pappadà A, Tessari A. Acceptance of Assistive Technology by Users with Motor Disabilities Due to Spinal Cord or Acquired Brain Injuries: A Systematic Review. Journal of Clinical Medicine. 2023; 12(8):2962. https://doi.org/10.3390/jcm12082962
Chicago/Turabian StyleVentura, Sara, Giovanni Ottoboni, Alessandro Pappadà, and Alessia Tessari. 2023. "Acceptance of Assistive Technology by Users with Motor Disabilities Due to Spinal Cord or Acquired Brain Injuries: A Systematic Review" Journal of Clinical Medicine 12, no. 8: 2962. https://doi.org/10.3390/jcm12082962
APA StyleVentura, S., Ottoboni, G., Pappadà, A., & Tessari, A. (2023). Acceptance of Assistive Technology by Users with Motor Disabilities Due to Spinal Cord or Acquired Brain Injuries: A Systematic Review. Journal of Clinical Medicine, 12(8), 2962. https://doi.org/10.3390/jcm12082962






