Advances in the Treatment of Implant-Associated Infections of the Pelvis: Eradication Rates, Recurrence of Infection, and Outcome
Abstract
1. Introduction
2. Material and Methods
2.1. Surgical Procedure
2.2. Microbiological Examination
2.3. Follow-Up
2.4. Statistical Analysis
3. Results
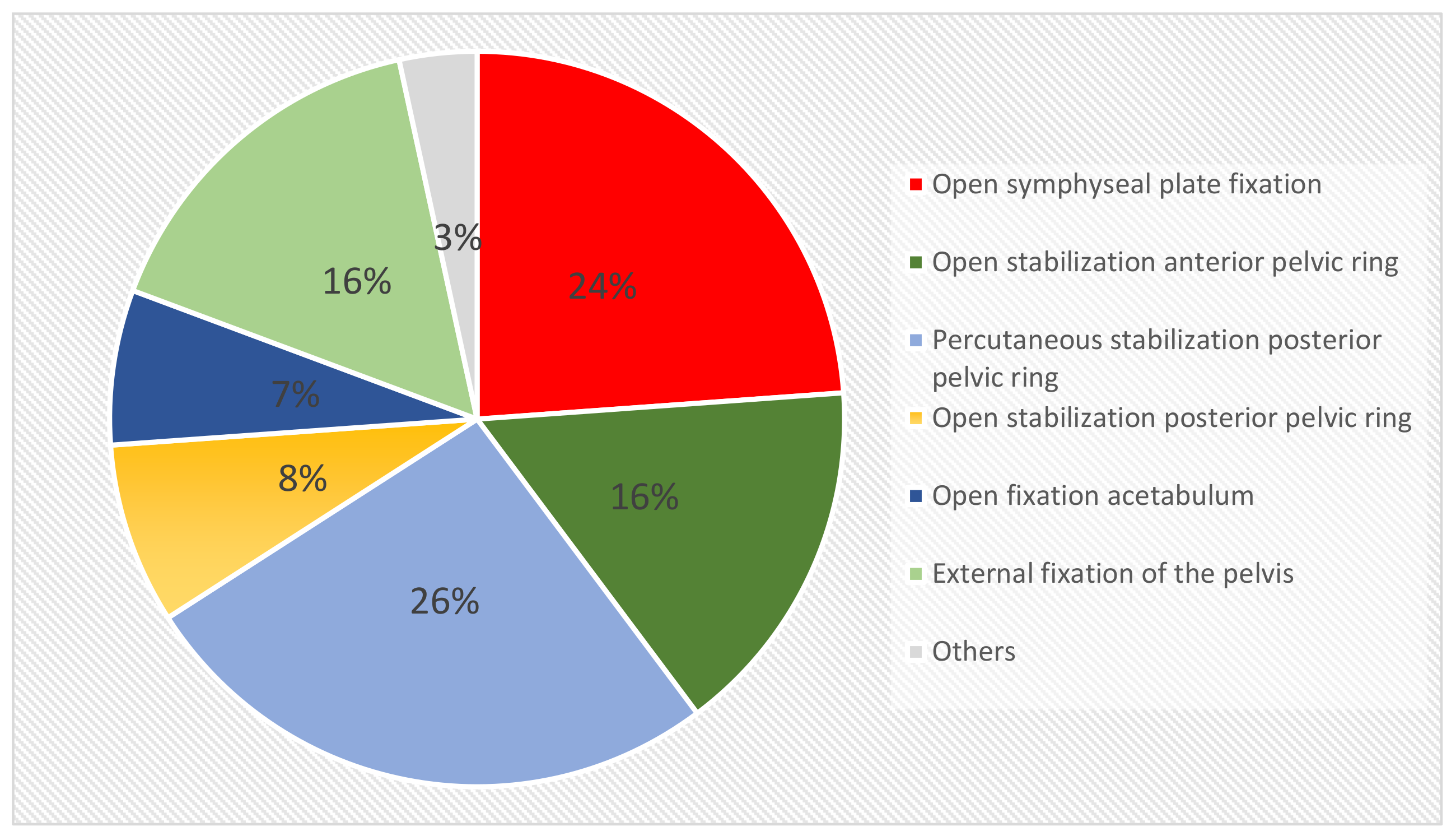
3.1. Epidemiology and Initial Surgical Approach
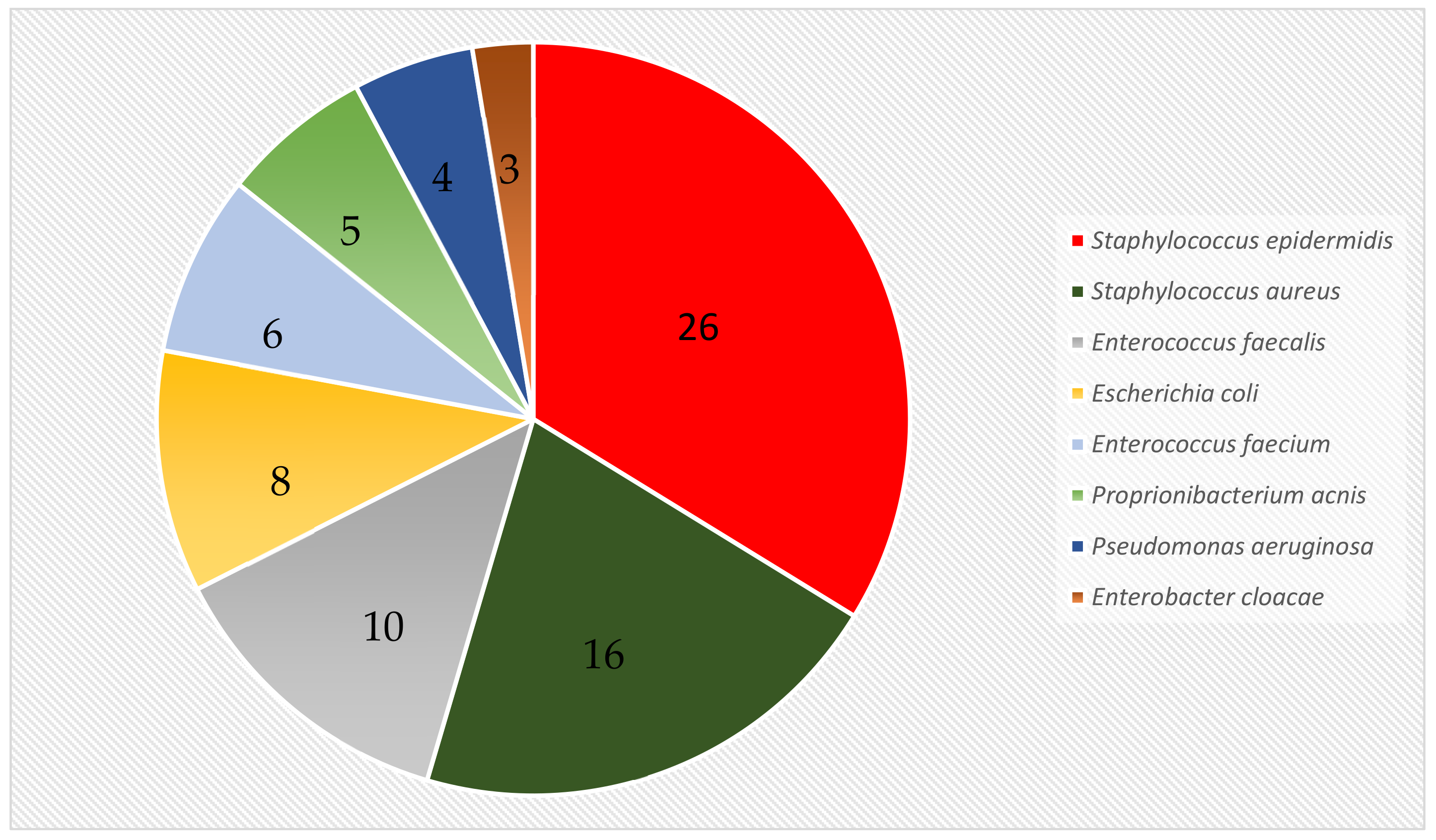
3.2. Microbiology
3.3. Eradication Rate and Recurrence of Infection
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stover, M.D.; Sims, S.; Matta, J. What is the infection rate of the posterior approach to type C pelvic injuries? Clin. Orthop. Relat. Res. 2012, 470, 2142–2147. [Google Scholar] [CrossRef] [PubMed]
- Kellam, J.F.; McMurtry, R.Y.; Paley, D.; Tile, M. The unstable pelvic fracture. Operative treatment. Orthop. Clin. North Am. 1987, 18, 25–41. [Google Scholar] [PubMed]
- Vaidya, R.; Kubiak, I.N.; Bergin, P.F.; Dombroski, D.G.; Critchlow, R.J.; Sethi, A.; Starr, A.J. Complications of anterior subcutaneous internal fixation for unstable pelvis fractures: A multicenter study. Clin. Orthop. Relat. Res. 2012, 470, 2124–2131. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, A.; Phillips, T.; Sclafani, S.J.; Scalea, T.; Duncan, A.; Goldstein, J.; Panetta, T.; Shaftan, G. Early open reduction and internal fixation of the disrupted pelvic ring. J. Trauma. Inj. Infect. Crit. Care. 1986, 26, 325–333. [Google Scholar] [CrossRef] [PubMed]
- Morris, S.A.C.; Loveridge, J.; Smart, D.K.A.; Ward, A.J.; Chesser, T.J.S. Is fixation failure after plate fixation of the symphysis pubis clinically important? Clin. Orthop. Relat. Res. 2012, 470, 2154–2160. [Google Scholar] [CrossRef] [PubMed]
- Ding, A.; O’Toole, R.V.; Castillo, R.; Reahl, B.; Montalvo, R.; Nascone, J.W.; Sciadini, M.F.; Carlini, A.R.; Manson, T.T. Risk Factors for early reoperation after operative treatment of Acetabular Fractures. J. Orthop. Trauma 2018, 32, 251–257. [Google Scholar] [CrossRef] [PubMed]
- Song, W.; Zhou, D.; Xu, W.; Zhang, G.; Wang, C.; Qiu, D.; Dong, J. Factors of pelvic infection and death in patients with open pelvic fractures and rectal injuries. Surg. Infect. 2017, 18, 711–715. [Google Scholar] [CrossRef] [PubMed]
- Yao, H.H.; Esser, M.; Grummet, J.; Atkins, C.; Royce, P.; Hanegbi, U. Lower risk of pelvic metalware infection with operative repair of concurrent bladder rupture. ANZ J. Surg. 2018, 88, 560–564. [Google Scholar]
- Kanakaris, N.K.; Ciriello, V.; Stavrou, P.Z.; West, R.M.; Giannoudis, P.V. Deep infection following reconstruction of pelvic fractures: Prevalence, characteristics and predisposing risk factors. Eur. J. Trauma Emerg. Surg. 2021, 48, 3701–3709. [Google Scholar] [CrossRef] [PubMed]
- Whitehouse, J.D.; Friedman, N.D.; Kirkland, K.B.; Richardson, W.J.; Sexton, D.J. The impact of surgical-site infections following orthopedic surgery at a community hospital and a university hospital: Adverse quality of life, excess length of stay and extra cost. Infect Control Hosp. Epidemiol. 2002, 23, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Manson, T.T.; Perdue, P.W.; Pollack, A.N.; O’Toole, R.V. Embolization of pelvic arterial injury is a risk factor for deep infection after acetabular fracture surgery. J. Orthop. Trauma 2012, 27, 11–15. [Google Scholar] [CrossRef] [PubMed]
- Papakostidis, C.; Giannoudis, P.V. Pelvic ring injuries with haemodynamic instability: Efficacy of pelvic packing, a systematic review. Injury 2009, 40, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Vaidya, R.; Amar, K.; Woodburry, D.; Washington, A. Infection after the use of INFIX in pelvic ring injuries. SICOT J. 2021, 7, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Brown, D.F.; Wootton, M.; Howe, R.A. Antimicrobial susceptibility testing break-points and methods from BSAC to EUCAST. J. Antimicrob. Chemother. 2016, 71, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Sagi, C.H.; Dziadosz, D.; Mir, H.; Virani, N.; Olson, C. Obesity, Leukocytosis, Embolization, and Injury Severity increase the risk for deep postoperative Wound Infection after Pelvic and Acetabular Surgery. J. Orthop. Trauma 2013, 27, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Iqbal, F.; Younus, S.; Asmatullah; Bin Zia, O.; Khan, N. Surgical Site Infection following fixation of acetabular fractures. Hip. Pelvis. 2017, 29, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, T.; Morgan, S.J.; Smith, W.R.; Stahel, P.F.; Gillani, S.A.; Hak, D.J. Postoperative surgical site infection following acetabular fracture fixation. Injury 2010, 41, 396–399. [Google Scholar] [CrossRef] [PubMed]
- Torbert, J.T.; Joshi, M.; Moraff, A.; Matuszewski, P.E.; Holmes, A.; Pollak, A.M.; O’Toole, O.V. Current bacterial speciation and antibiotic resistance in deep infection after operative fixation of fractures. J. Orthop. Trauma 2015, 29, 7–17. [Google Scholar] [CrossRef] [PubMed]
- Letournel, E.; Judet, R. Fractures of the Acetabulum; Springer: Berlin, Germany, 1993. [Google Scholar]
- Hak, D.J.; Olson, S.A.; Matta, J.M. Diagnosis and management of closed internal degloving injuries associated with pelvic and acetabular fractures: The Morel-Lavallée lesion. J. Trauma 1997, 42, 1046–1051. [Google Scholar] [CrossRef] [PubMed]
- Tseng, S.; Tornetta, P., 3rd. Percutaneous management of Morel-Lavallée lesions. J. Bone Joint Surg. Am. 2006, 88, 92–96. [Google Scholar] [PubMed]
| Age (years) | 45.4 (±15.4) |
| Male | 32 (74.4%) |
| Female | 11 (25.6%) |
| Early infection (<6 weeks) | 24 (56%) |
| Late infection >6 weeks) | 19 (44%) |
| Days in hospital (median) | 45 (7–330) |
| Number of operations (average) | 5.7 (±5.4) |
| Follow-up (median, months) | 98.2 (24–226) |
| Recurrent Infection | Non-Recurrent Infection |
|---|---|
| n = 7 (16%) | 27 (63%) |
| Staphylococcus epidermidis (57%) | Staphylococcus epidermidis (67%) |
| Enterococcus faecalis (43%) | Staphylococcus aureus (39%) |
| Staphylococcus aureus (29%) | Enterococcus faecalis (19%) |
| Escherichia coli (19%) | |
| Enterococcus faecium (17%) | |
| Pseudomonas aeruginosa (8%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kellermann, F.; Hackl, S.; Leister, I.; Hungerer, S.; Militz, M.; Stuby, F.; Holzmann, B.; Friederichs, J. Advances in the Treatment of Implant-Associated Infections of the Pelvis: Eradication Rates, Recurrence of Infection, and Outcome. J. Clin. Med. 2023, 12, 2854. https://doi.org/10.3390/jcm12082854
Kellermann F, Hackl S, Leister I, Hungerer S, Militz M, Stuby F, Holzmann B, Friederichs J. Advances in the Treatment of Implant-Associated Infections of the Pelvis: Eradication Rates, Recurrence of Infection, and Outcome. Journal of Clinical Medicine. 2023; 12(8):2854. https://doi.org/10.3390/jcm12082854
Chicago/Turabian StyleKellermann, Florian, Simon Hackl, Iris Leister, Sven Hungerer, Matthias Militz, Fabian Stuby, Bernhard Holzmann, and Jan Friederichs. 2023. "Advances in the Treatment of Implant-Associated Infections of the Pelvis: Eradication Rates, Recurrence of Infection, and Outcome" Journal of Clinical Medicine 12, no. 8: 2854. https://doi.org/10.3390/jcm12082854
APA StyleKellermann, F., Hackl, S., Leister, I., Hungerer, S., Militz, M., Stuby, F., Holzmann, B., & Friederichs, J. (2023). Advances in the Treatment of Implant-Associated Infections of the Pelvis: Eradication Rates, Recurrence of Infection, and Outcome. Journal of Clinical Medicine, 12(8), 2854. https://doi.org/10.3390/jcm12082854






