Digital Application for Promoting Evidence-Based Children’s Oral Health to Control Early Childhood Caries: Randomized Control Trial on Parental Acceptance and Efficacy
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval
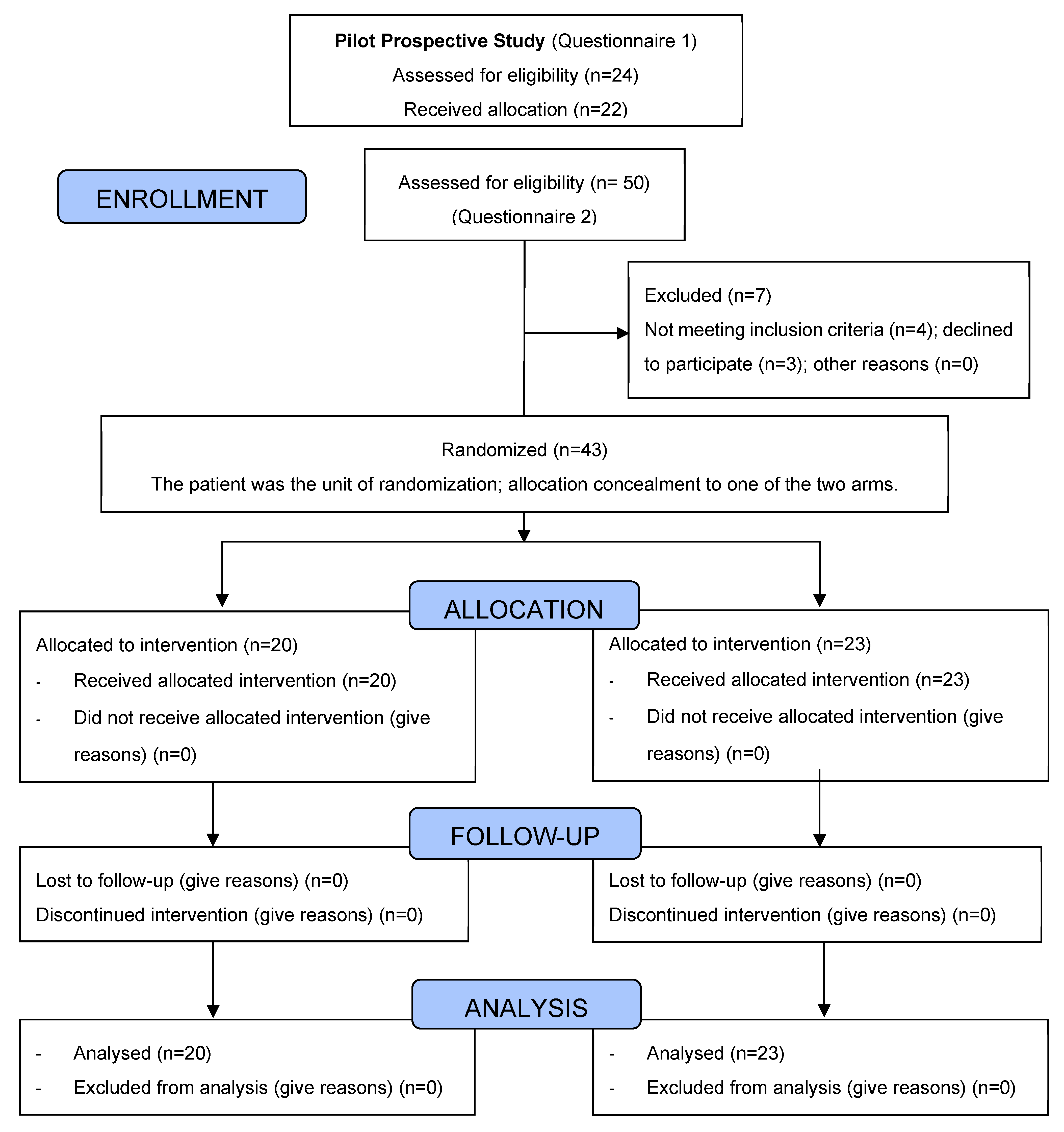
2.2. Study Design
2.3. Sample Size Calculation
2.4. Application Development
2.5. Questionnaires and Data Sheets
2.6. Intervention
2.7. Outcomes
2.7.1. Primary Outcomes
2.7.2. Secondary Outcome and Assessment
2.8. Statistical Analysis
3. Results
3.1. Part 1: Acceptance, Usability, and Parental Perception of the Digital Application (FU-APP)
3.1.1. Baseline Characteristics
3.1.2. Outcomes
- Usage of FU-APP: All participants completely agreed that the FU-APP was easy to use (n = 22; 100%). Almost all (n = 19, 86.4%) completely agreed that the FU-APP was easy to understand, that they liked the usage of the FU-APP, and that the usage time of FU-APP was also reasonable.
- Acceptance of FU-APP: Almost 91% of participants (n = 20) completely agreed that FU-APP provides interactive insight to oral health, whereas 4.5% (n = 1) partially agreed with this statement.
- Content and information of FU-APP: Of the 22 participants, 90.9% (n = 20) completely agreed that the information in FU-APP was clear, understandable, and easy to follow, and 95.5% (n = 21) completely agreed that the navigation was uniform.
- Usefulness of FU-APP: 90.9% of the participants (n = 20) completely agreed that FU-APP can be useful for their child’s caries prevention, 86.4% (n = 19) completely agreed that FU-APP was useful to improve their child’s knowledge of oral hygiene, and 90.9% (n = 20) considered FU-APP as a helpful motivational oral hygiene tool.
- Satisfaction regarding FU-APP: About 90.9% (n = 20) completely agreed that they would use this application again and recommend it to others. In addition, 86.4% (n = 19) of participants were overall satisfied with FU-APP.
- Relationship between outcomes and assessed variables: There was a strong positive correlation between several variables—usage (understandability r = 0.630, p = 0.002), acceptance (interactive insight r = 0.817, p = 0.001), content and information (information clear, understandable, easy to follow r = 0.817, p = 0.001), and usefulness (knowledge r = 0.643, p = 0.001, and motivation improvement r = 0.815, p = 0.001). Description of all correlations are presented in Table 1.
3.2. Part 2: Randomized Controlled Trial
3.2.1. Baseline Characteristics
3.2.2. Reasons of the Dental Visit
3.2.3. Knowledge Comparison about the Best Oral Hygiene Practices
3.2.4. Knowledge Comparison about Nutritional Behavioral Practices
3.2.5. Attitude and Motivation Comparison
3.2.6. Caries Index, API and PBI Baseline, and Follow-Up Comparison
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Group, O.; Council, R. Policy on early childhood caries (ECC): Classifications, consequences, and preventive strategies. Pediatr. Dent. 2014, 30, 40–43. [Google Scholar]
- Meyer, F.; Enax, J. Early Childhood Caries: Epidemiology, Aetiology, and Prevention. Int. J. Dent. 2018, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.J.; Gao, S.S.; Duangthip, D.; Lo, E.C.M.; Chu, C.H. Prevalence of early childhood caries among 5-year-old children: A systematic review. J. Investig. Clin. Dent. 2019, 10, e12376. [Google Scholar] [CrossRef] [PubMed]
- DAJ Epidemiologische Begleituntersuchungen zur Gruppenprophylaxe 2016; Arb. f. Jugendzahnpflege (DAJ): Bonn, Germany, 2017; ISBN 9783926228307.
- Rai, N.K.; Tiwari, T. Parental factors influencing the development of early childhood caries in developing nations: A systematic review. Front. Public Health 2018, 6, 1–8. [Google Scholar] [CrossRef]
- Suma Sogi, H.; Hugar, S.; Nalawade, T.; Sinha, A.; Hugar, S.; Mallikarjuna, R. Knowledge, attitude, and practices of oral health care in prevention of early childhood caries among parents of children in Belagavi city: A Questionnaire study. J. Fam. Med. Prim. Care 2016, 5, 286. [Google Scholar] [CrossRef]
- Bundeszahnärztekammer, K.B. Praktischer Ratgeber für die zahnärztliche Praxis. Frühkindliche Karies Vermeiden 2019, 53, 1–58. [Google Scholar] [CrossRef]
- Winter, J.; Bartsch, B.; Schütz, C.; Jablonski-Momeni, A.; Pieper, K. Implementation and evaluation of an interdisciplinary preventive program to prevent early childhood caries. Clin. Oral Investig. 2019, 23, 187–197. [Google Scholar] [CrossRef]
- Santamaria, R.M.; Schmoeckel, J.; Basner, R.; Schüler, E.; Splieth, C.H. Caries Trends in the Primary Dentition of 6- to 7-Year-old Schoolchildren in Germany from 1994 to 2016: Results from the German National Oral Health Surveys in Children. Caries Res. 2019, 53, 659–666. [Google Scholar] [CrossRef]
- Mohamadkhah, F.; Shokravi, F.A.; Faghihzadeh, S.; Ghaffarifar, S. The effect of digital media programs on the oral health promotion in the health office: A quasi-experimental study. Shiraz E-Med. J. 2013, 14, 2–12. [Google Scholar]
- Ganavadiya, R.; Goel, P.; Hongal, S.; Jain, M.; Chandrashekar, B. Mobile and portable dental services catering to the basic oral health needs of the underserved population in developing countries: A proposed model. Ann. Med. Health Sci. Res. 2014, 4, 293. [Google Scholar] [CrossRef]
- Scheerman, J.F.M.; van Meijel, B.; van Empelen, P.; Kramer, G.J.C.; Verrips, G.H.W.; Pakpour, A.H.; Van den Braak, M.C.T.; van Loveren, C. Study protocol of a randomized controlled trial to test the effect of a smartphone application on oral-health behavior and oral hygiene in adolescents with fixed orthodontic appliances. BMC Oral. Health 2018, 18, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Toniazzo, M.P.; Nodari, D.; Muniz, F.W.M.G.; Weidlich, P. Effect of mHealth in improving oral hygiene: A systematic review with meta-analysis. J. Clin. Periodontol. 2019, 46, 297–309. [Google Scholar] [CrossRef] [PubMed]
- Estai, M.; Kanagasingam, Y.; Mehdizadeh, M.; Vignarajan, J.; Norman, R.; Huang, B.; Spallek, H.; Irving, M.; Arora, A.; Kruger, E.; et al. Teledentistry as a novel pathway to improve dental health in school children: A research protocol for a randomised controlled trial. BMC Oral. Health 2020, 20, 11. [Google Scholar] [CrossRef] [PubMed]
- Braz, M.A.; Rivaldo, E.G.; De Moura, F.R.R.; Cruz, R.A.; Brew, M.C.; Haddad, A.E.; Bavaresco, C.S. Mobile applications for dental education and assistance: An integrative review. Rev. ABENO 2018, 18, 181–190. [Google Scholar] [CrossRef]
- Tiffany, B.; Blasi, P.; Catz, S.L.; McClure, J.B. Mobile apps for oral health promotion: Content review and heuristic usability analysis. JMIR mHealth uHealth 2018, 6, 1–12. [Google Scholar] [CrossRef]
- Kassebaum, N.J.; Smith, A.G.C.; Bernabé, E.; Fleming, T.D.; Reynolds, A.E.; Vos, T.; Murray, C.J.L.; Marcenes, W. Global, Regional, and National Prevalence, Incidence, and Disability-Adjusted Life Years for Oral Conditions for 195 Countries, 1990-2015: A Systematic Analysis for the Global Burden of Diseases, Injuries, and Risk Factors. J. Dent. Res. 2017, 96, 380–387. [Google Scholar] [CrossRef]
- Coughlin, S.S.; Hardy, D.; Caplan, L.S. The need for culturally-tailored smartphone applications for weight control. J. Georg. Public Health Assoc. 2016, 5, 228. [Google Scholar] [CrossRef]
- Ahsan, G.M.T.; Tumpa, J.F.; Adib, R.; Ahamed, S.I.; Petereit, D.; Burhansstipanov, L.; Krebs, L.U.; Dignan, M. A Culturally Tailored Intervention System for Cancer Survivors to Motivate Physical Activity. In Proceedings of the International Computer Software and Applications Conference, Tokyo, Japan, 23–27 July 2018. [Google Scholar]
- Ryan, K.; Dockray, S.; Linehan, C. A systematic review of tailored eHealth interventions for weight loss. Digit. Health 2019, 5, 2055207619826685. [Google Scholar] [CrossRef]
- Moses, J.; Arunachalam, S.K. Knowledge, Attitude, and Practice of Mothers regarding Oral Hygiene of Primary School children in Chennai, Tamil Nadu, India. Int. J. Clin. Pediatr. Dent. 2018, 11, 338. [Google Scholar] [CrossRef]
- Hiratsuka, V.Y.; Robinson, J.M.; Greenlee, R.; Refaat, A. Oral health beliefs and oral hygiene behaviours among parents of urban Alaska Native children. Int. J. Circumpolar Health 2019, 78, 1586274. [Google Scholar] [CrossRef]
- Chen, L.; Hong, J.; Xiong, D.; Zhang, L.; Li, Y.; Huang, S.; Hua, F. Are parents’ education levels associated with either their oral health knowledge or their children’s oral health behaviors? A survey of 8446 families in Wuhan. BMC Oral. Health 2020, 20, 1–12. [Google Scholar] [CrossRef]
- Naidu, R.; Nunn, J.; Irwin, J.D. The effect of motivational interviewing on oral healthcare knowledge, attitudes and behaviour of parents and caregivers of preschool children: An exploratory cluster randomised controlled study. BMC Oral Health 2015, 15, 1–15. [Google Scholar] [CrossRef]
- Naidu, R.S.; Nunn, J.H. Oral Health Knowledge, Attitudes and Behaviour of Parents and Caregivers of Preschool Children: Implications for Oral Health Promotion. Oral Health Prev. Dent. 2020, 18, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Dahlan, R.; Bohlouli, B.; Salami, B.; Saltaji, H.; Amin, M. Parental acculturation and oral health of children among immigrants. J. Public Health Dent. 2021, 82, 426–436. [Google Scholar] [CrossRef]
- Al-Jaber, A.S.; Al-Qatami, H.M.; Abed Al Jawad, F.H. Knowledge, Attitudes, and Practices of Parents on Early Childhood Caries in Qatar-A Questionnaire Study. Eur. J. Dent. 2022, 16, 669–679. [Google Scholar] [CrossRef]
- Dagon, N.; Ratson, T.; Peretz, B.; Blumer, S. Maternal knowledge of oral health of children aged 1-4 years. J. Clin. Pediatr. Dent. 2019, 43, 116–120. [Google Scholar] [CrossRef]
- Nguyen, U.N.; Rowe, D.J.; Barker, J.C. Survey of Knowledge, Beliefs, and Behaviors of Migrant Vietnamese Parents Regarding Young Children’s Oral Health. J. Dent. Hyg. JDH 2017, 91, 45–53. [Google Scholar]
- Walsh, T.; Worthington, H.V.; Glenny, A.M.; Marinho, V.C.C.; Jeroncic, A. Fluoride toothpastes of different concentrations for preventing dental caries: A Cochrane review. Dent. Cadmos 2020. [Google Scholar] [CrossRef]
- Toumba, K.J.; Twetman, S.; Splieth, C.; Parnell, C.; van Loveren, C.; Lygidakis, N. Guidelines on the use of fluoride for caries prevention in children: An updated EAPD policy document. Eur. Arch. Paediatr. Dent. 2019, 20, 507–516. [Google Scholar] [CrossRef]
- Splieth, C.H.; Banerjee, A.; Bottenberg, P.; Breschi, L.; Campus, G.; Ekstrand, K.R.; Giacaman, R.A.; Haak, R.; Hannig, M.; Hickel, R.; et al. How to intervene in the caries process in children: A joint ORCA and EFCD expert delphi consensus statement. Caries Res. 2020, 54, 297–305. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Splieth, C.H.; Bottenberg, P.; Breschi, L.; Campus, G.; Doméjean, S.; Ekstrand, K.; Giacaman, R.A.; Haak, R.; Hannig, M.; et al. How to intervene in the caries process in adults: Proximal and secondary caries? An EFCD-ORCA-DGZ expert Delphi consensus statement. Clin. Oral Investig. 2020, 24, 3315–3321. [Google Scholar] [CrossRef] [PubMed]
- Scheerman, J.F.M.; van Meijel, B.; van Empelen, P.; Verrips, G.H.W.; van Loveren, C.; Twisk, J.W.R.; Pakpour, A.H.; van den Braak, M.C.T.; Kramer, G.J.C. The effect of using a mobile application (“WhiteTeeth”) on improving oral hygiene: A randomized controlled trial. Int. J. Dent. Hyg. 2020, 18, 73–83. [Google Scholar] [CrossRef]
- Banskota, S.; Healy, M.; Goldberg, E.M. 15 smartphone apps for older adults to use while in isolation during the COVID-19 pandemic. West. J. Emerg. Med. 2020, 21, 514–525. [Google Scholar] [CrossRef] [PubMed]
- Ming, L.C.; Untong, N.; Aliudin, N.A.; Osili, N.; Kifli, N.; Tan, C.S.; Goh, K.W.; Ng, P.W.; Al-Worafi, Y.M.; Lee, K.S.; et al. Mobile health apps on COVID-19 launched in the early days of the pandemic: Content analysis and review. JMIR mHealth uHealth 2020, 8, e19796. [Google Scholar] [CrossRef] [PubMed]
- John Leon Singh, H.; Couch, D.; Yap, K. Mobile Health Apps That Help With COVID-19 Management: Scoping Review. JMIR Nurs. 2020, 3, e20596. [Google Scholar] [CrossRef]
| Questionnaire Items | Overall Satisfaction | |
|---|---|---|
| Usage | r | p-Value |
| 0.630 | 0.002 * |
| 0.263 | 0.238 |
| 0.210 | 0.348 |
| Acceptance | ||
| 0.817 | 0.001 * |
| Content and information | ||
| 0.817 | 0.001 * |
| 0.087 | 0.702 |
| Usefulness | ||
| 0.313 | 0.156 |
| 0.643 | 0.001 * |
| 0.815 | 0.001 * |
| Demographic Characteristics | Test (n = 20) | Control (n = 23) | p-Value | |
|---|---|---|---|---|
| Age in years | Mean (SD) (a) | 2.75 (1.97) | 3.35 (1.30) | 0.26 |
| Age in months | 36.10 (22.59) | 44.13 (15.38) | 0.19 | |
| Age category * (b) | 6–9 months | 2 (10%) | 0 (0%) | PMC: 0.18 |
| 10–20 months | 5 (25%) | 2 (8.7%) | ||
| 21–33 months | 2 (10%) | 3 (13%) | ||
| 34–72 months | 11 (55%) | 18 (78.3%) | ||
| Child’s sex (b) | Female | 10 (50%) | 11 (47.8%) | 0.89 |
| Male | 10 (50%) | 12 (52.2%) | ||
| Parent’s sex (b) | Female | 13 (65%) | 15 (65.2%) | 0.99 |
| Male | 7 (35%) | 8 (34.8%) | ||
| Mother’s education (b) | No degree | 0 (0%) | 1 (4.3%) | PMC: 0.57 |
| Elementary school | 0 (0%) | 4 (17.4%) | ||
| Middle/secondary school | 4 (20%) | 2 (8.7%) | ||
| Vocational training | 5 (25%) | 7 (30.4%) | ||
| Technical college/diploma | 1 (5%) | 1 (4.3%) | ||
| Academic/university education | 6 (30%) | 5 (21.7%) | ||
| Higher education | 4 (20%) | 3 (13%) | ||
| Father’s education (b) | No degree | 0 (0%) | 1 (4.3%) | PMC: 0.87 |
| Elementary school | 1 (5%) | 2 (8.7%) | ||
| Middle/secondary school | 3 (15%) | 2 (8.7%) | ||
| Vocational training | 9 (45%) | 9 (39.1%) | ||
| Technical college/diploma | 0 (0%) | 0 (0%) | ||
| Academic/university education | 6 (30%) | 5 (21.7%) | ||
| Higher education | 1 (5%) | 4 (17.4%) | ||
| Oral Hygiene Practices | Test (n = 20) | Control (n = 23) | p-Value | |||
|---|---|---|---|---|---|---|
| Baseline | Follow-Up | Baseline | Follow-Up | PMC | ||
| Who cleans the child’s teeth? | Child alone | 2 (10%) | 2 (10%) | 8 (34.8%) | 10 (43.5%) | Baseline 0.02 * Follow-up 0.02 * |
| Parents alone | 6 (30%) | 6 (30%) | 1 (4.3%) | 1 (4.3%) | ||
| Child and parents | 10 (50%) | 12 (60%) | 13 (56.5%) | 11 (47.8%) | ||
| No one | 2 (10%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Someone else (Nursery) | 0 (0%) | 0 (0%) | 1 (4.3%) | 1 (4.3%) | ||
| p-value | 0.60 | 0.16 | ||||
| With what do you brush your child’s teeth? | Toothbrush | 2 (10%) | 1 (5%) | 2 (9.1%) | 2 (8.7%) | Baseline 0.85 Follow-up 0.85 |
| Toothbrush and toothpaste without fluoride | 1 (5%) | 1 (5%) | 3 (13.6%) | 4 (17.4%) | ||
| Toothbrush and toothpaste with fluoride | 17 (85%) | 18 (90%) | 17 (77.3%) | 17 (73.9%) | ||
| p-value | 0.41 | 0.66 | ||||
| How often are your child’s teeth brushed? | 1 time a day | 7 (35%) | 3 (15%) | 7 (30.4%) | 5 (21.7%) | Baseline 0.31 Follow-up 0.31 |
| 2 or more times a day | 11 (55%) | 17 (85%) | 16 (69.6%) | 18 (78.3%) | ||
| Less than 1 time a week | 2 (10%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| p-value | 0.86 | 0.32 | ||||
| Knowledge about Best Oral Hygiene Practices | Test (n = 20) | Control (n = 23) | p-Value | |||
|---|---|---|---|---|---|---|
| Baseline | Follow-Up | Baseline | Follow-Up | PMC | ||
| When should we begin with cleaning the teeth? | Less than 6 months | 4 (20%) | 7 (35%) | 5 (21.7%) | 5 (21.7%) | Baseline 0.42 Follow-up 0.053 |
| 6–12 months | 11 (55%) | 13 (65%) | 10 (43.5%) | 11 (47.8%) | ||
| 12–24 months | 2 (10%) | 0 (0%) | 5 (21.7%) | 5 (21.7%) | ||
| >24 months | 1 (5%) | 0 (0%) | 3 (13%) | 2 (8.7%) | ||
| Not started yet | 2 (10%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| p-value | 0.02 * | 0.56 | ||||
| What is the right order to brush? | COI brushing technique | 14 (70%) | 20 (100%) | 14 (60.9%) | 19 (82.6%) | Baseline 0.80 Follow-up 0.24 |
| Horizontal vertical | 4 (20%) | 0 (0%) | 7 (30.4%) | 3 (13%) | ||
| The direction does not matter | 2 (10%) | 0 (0%) | 2 (7.7%) | 1 (4.3%) | ||
| p value | 0.02 * | 0.03 * | ||||
| What should be the fluoride content? + | No fluoride | 0 (0%) | 1 (5%) | 0 (0%) | 0 (0%) | Baseline 0.56 Follow-up 0.39 |
| 500 ppm fluoride | 1 (5%) | 2 (10%) | 2 (9.1%) | 4 (17.4%) | ||
| 1000 ppm fluoride | 9 (45%) | 16 (80%) | 12 (54.5%) | 14 (60.9%) | ||
| >than 1400 ppm fluoride | 0 (0%) | 0 (0%) | 1 (4.5%) | 1 (4.3%) | ||
| I don’t know | 10 (50%) | 1 (5%) | 7 (31.8%) | 1 (4.3%) | ||
| p-value | 0.001 * | 0.10 | ||||
| Knowledge about Nutritional and Habitual Practices | Test (n = 20) | Control (n = 23) | p-Value | |||
|---|---|---|---|---|---|---|
| Baseline | Follow-Up | Baseline | Follow-Up | PMC | ||
| By which nutrition modifications can we avoid ECC? | Decreasing sugary food/ beverages | 15 (75%) | 20 (100%) | 19 (82.6%) | 22 (95.7%) | Baseline 0.14 Follow-up 0.22 |
| Avoiding bottle feeding | 5 (25%) | 0 (0%) | 1 (4.3%) | 0 (0%) | ||
| Diet has no effect | 0 (0%) | 0 (0%) | 2 (8.7%) | 0 (0%) | ||
| I don’t know | 0 (0%) | 0 (0%) | 1 (4.3%) | 1 (4.3%) | ||
| p-value | 0.23 | 0.43 | ||||
| Which behavioral habits do you think can damage your child’s dentition? | Thumb sucking | 7 (35%) | 9 (45%) | 15 (65.2%) | 20 (86.9%) | Baseline 0.28 Follow-up 0.01 * |
| Nail biting | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | ||
| Thumb sucking + nail biting | 11 (55%) | 11 (55%) | 7 (30.4%) | 2 (8.7%) | ||
| Behavioral habits have no effect | 0 (0%) | 0 (0%) | 0 (0%) | 1 (4.4%) | ||
| I don’t know | 2 (10%) | 0 (0%) | 1 (4.4%) | 0 (0%) | ||
| p-value | 0.41 | 0.18 | ||||
| Attitude and Motivation | Test (n = 20) | Control (n = 23) | p-Value | |||
|---|---|---|---|---|---|---|
| Baseline | Follow-Up | Baseline | Follow-Up | PMC | ||
| How would you have recommendations? | Only through the dentist | 7 (35%) | 6 (30%) | 12 (52.2%) | 15 (65.2%) | Baseline 0.22 Follow-up 0.06 |
| Via apps only | 0 (0%) | 0 (0%) | 1 (4.3%) | 1 (4.3%) | ||
| Through the dentist and digital apps | 13 (65%) | 12 (60%) | 9 (39.1%) | 6 (26.1%) | ||
| This makes no difference | 0 (0%) | 2 (10%) | 1 (4.3%) | 1 (4.5%) | ||
| p-value | 0.64 | 0.28 | ||||
| Do you feel this appointment influences your motivation to brush your children’s teeth? + | Yes | 12 (63.2%) | 16 (80%) | 0 (0%) | 1 (6.7%) | Baseline <0.001 * Follow-up <0.001* |
| No | 2 (10.5%) | 0 (0%) | 15 (100%) | 14 (93.3%) | ||
| It doesn’t make a difference | 5 (26.3%) | 4 (20%) | 0 (0%) | 0 (0%) | ||
| p-value | 0.10 | 0.32 | ||||
| Test (n = 20) Mean (SD) | Control (n = 23) Mean (SD) | Mann-Whitney U p-Value | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-Up | Baseline | Follow-Up | Baseline | Follow-Up | |
| API | 29.00 (23.37) | 20.50 (15.72) | 30.22 (15.41) | 33.91 (24.63) | 0.32 | 0.03 * |
| p-value: 0.01 * | p-value: 0.72 | |||||
| PBI | 1.00 (3.08) | 0.50 (2.24) | 0.44 (2.09) | 0.87 (4.17) | 0.47 | 0.95 |
| p-value: 0.32 | p-value: 0.66 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdul Haq, J.; Splieth, C.H.; Mourad, M.S.; Vielhauer, A.; Abdulrahim, R.; Khole, M.R.; Santamaría, R.M. Digital Application for Promoting Evidence-Based Children’s Oral Health to Control Early Childhood Caries: Randomized Control Trial on Parental Acceptance and Efficacy. J. Clin. Med. 2023, 12, 2680. https://doi.org/10.3390/jcm12072680
Abdul Haq J, Splieth CH, Mourad MS, Vielhauer A, Abdulrahim R, Khole MR, Santamaría RM. Digital Application for Promoting Evidence-Based Children’s Oral Health to Control Early Childhood Caries: Randomized Control Trial on Parental Acceptance and Efficacy. Journal of Clinical Medicine. 2023; 12(7):2680. https://doi.org/10.3390/jcm12072680
Chicago/Turabian StyleAbdul Haq, Jameela, Christian H. Splieth, Mhd Said Mourad, Annina Vielhauer, Ruba Abdulrahim, Manasi R. Khole, and Ruth M. Santamaría. 2023. "Digital Application for Promoting Evidence-Based Children’s Oral Health to Control Early Childhood Caries: Randomized Control Trial on Parental Acceptance and Efficacy" Journal of Clinical Medicine 12, no. 7: 2680. https://doi.org/10.3390/jcm12072680
APA StyleAbdul Haq, J., Splieth, C. H., Mourad, M. S., Vielhauer, A., Abdulrahim, R., Khole, M. R., & Santamaría, R. M. (2023). Digital Application for Promoting Evidence-Based Children’s Oral Health to Control Early Childhood Caries: Randomized Control Trial on Parental Acceptance and Efficacy. Journal of Clinical Medicine, 12(7), 2680. https://doi.org/10.3390/jcm12072680








