Lapses of the Heart: Frequency and Subjective Salience of Impressions Reported by Patients after Cardiac Arrest
Abstract
1. Introduction
2. Methods
2.1. Project Design
2.2. Patients
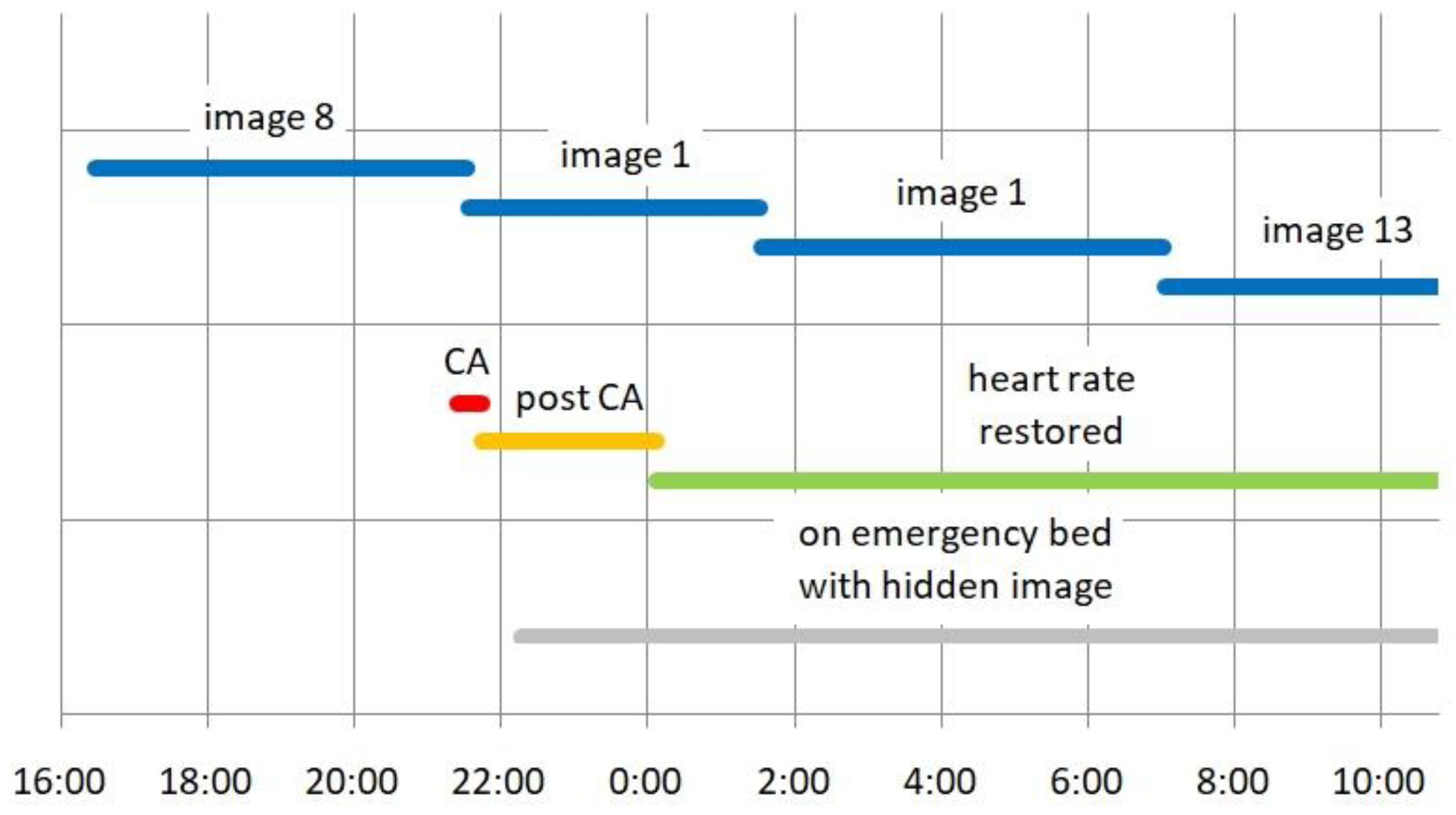
2.3. Hidden Images
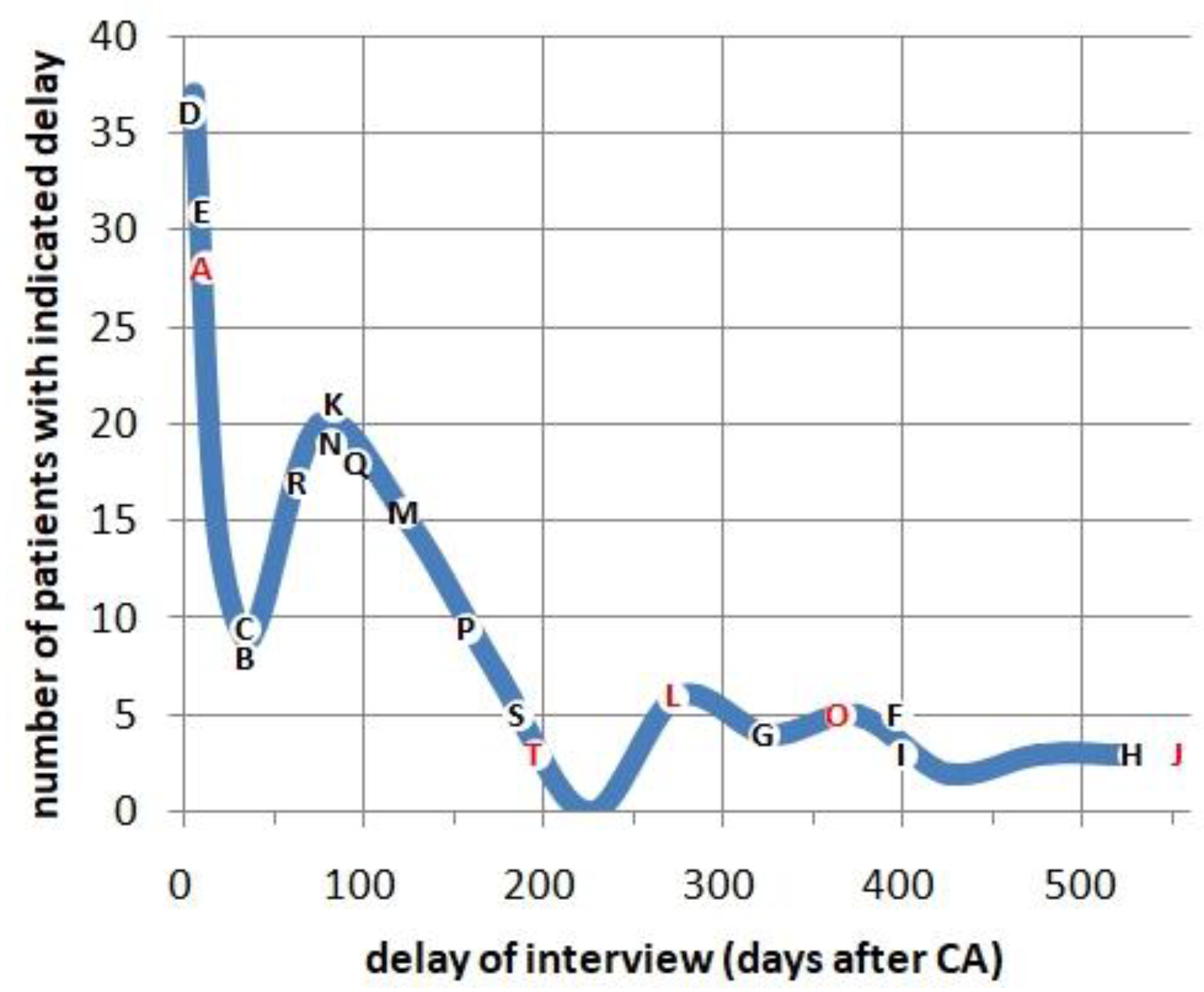
2.4. Interviews
2.5. Patients with Recollections
2.6. Statistics
3. Results
3.1. Compromised Memories
3.2. A First Patient Seems to Comment on a Hidden Image
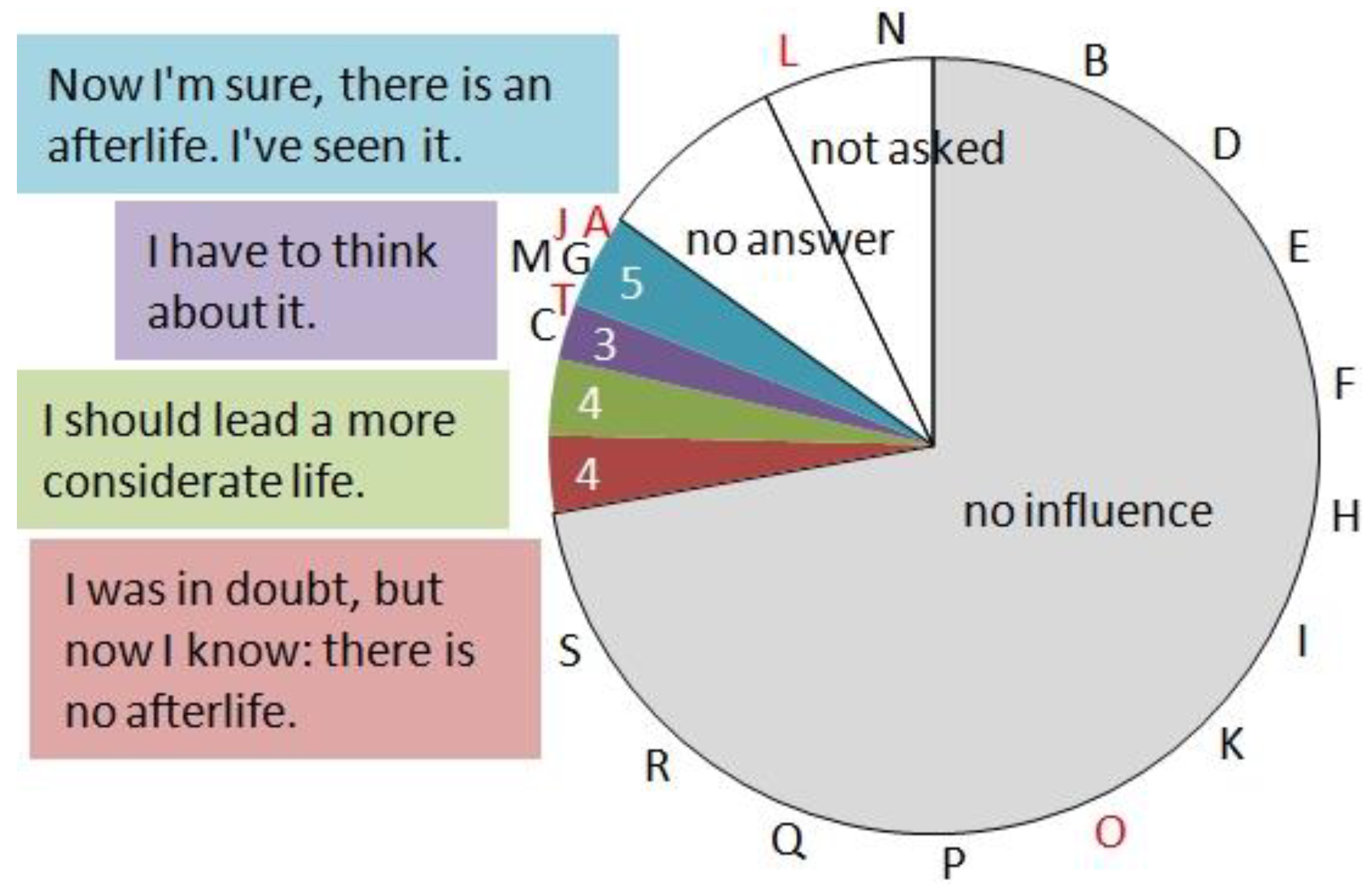
3.3. Influence of Attitude towards Religious Matters
3.4. Did You Notice Anything Similar in the Media?
3.5. Influence of the Duration of Cardiac Arrest
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cipani, S.; Bartolozzi, C.; Ballo, P.; Sarti, A. Blood flow maintenance by cardiac massage during cardiopulmonary resuscitation: Classical theories, newer hypotheses, and clinical utility of mechanical devices. J. Intensive Care Soc. 2019, 20, 2–10. [Google Scholar] [CrossRef] [PubMed]
- Kosmopoulos, M.; Kalra, R.; Bartos, J.A.; Raveendran, G.; Yannopoulos, D. Contemporary approaches to cardiopulmonary resuscitation: Physiology-guided approaches. J. Emerg. Crit. Care Med. 2020, 4, 19. [Google Scholar] [CrossRef]
- Orlando, A. Can Science Explain Near Death Experiences? Discover Magazine 2021, Sept/Oct issue. Available online: https://www.discovermagazine.com/mind/can-science-explain-near-death-experiences (accessed on 15 February 2023).
- Borjigin, J.; Lee, U.C.; Liu, T.; Pal, D.; Huff, S.; Klarr, D.; Sloboda, J.; Hernandez, J.; Wang, M.M.; Mashour, G.A. Surge of neurophysiological coherence and connectivity in the dying brain. Proc. Nat. Acad. Sci. USA 2013, 110, 14432–14437. [Google Scholar] [CrossRef] [PubMed]
- Vicente, R.; Rizzuto, M.; Sarica, C.; Yamamoto, K.; Sadr, M.; Khajuria, T.; Fatehi, M.; Moien-Afshari, F.; Haw, C.S.; Llinas, R.R.; et al. Enhanced interplay of neuronal coherence and coupling in the dying human brain. Front. Aging Neurosci. 2022, 14, 813531. [Google Scholar] [CrossRef]
- Iordanova, B.; Li, L.; Clark, R.S.B.; Manole, M.D. Alterations in cerebral blood flow after resuscitation from cardiac arrest. Front. Pediatr. 2017, 5, 174. [Google Scholar] [CrossRef]
- Greyson, B. The Near-Death Experience Scale: Construction, reliability, and validity. J. Nerv. Ment. Dis. 1983, 171, 369–375. [Google Scholar] [CrossRef]
- Parnia, S.; Post, S.G.; Lee, M.T.; Lyubomirsky, S.; Aufderheide, T.P.; Deakin, C.D.; Greyson, B.; Long, J.; Gonzales, A.M.; Huppert, E.L.; et al. Guidelines and standards for the study of death and recalled experience of death—A multidisciplinary consensus statement and proposed future directions. Ann. N. Y. Acad. Sci. 2022, 1511, 5–21. [Google Scholar] [CrossRef] [PubMed]
- Martial, C.; Cassol, H.; Laureys, S.; Gosseries, O. Near-death experiences as a probe to explore (disconnected) consciousness. Trends Cognit. Sci. 2020, 24, 173–183. [Google Scholar] [CrossRef]
- Parnia, S.; Spearpoint, K.; de Vos, G.; Fenwick, P.; Goldberg, D.; Yang, J.; Zhu, J.; Baker, K.; Killingback, H.; McLean, P.; et al. AWARE – AWAreness during Resuscitation – A prospective study. Resuscitation 2014, 85, 1799–1805. [Google Scholar] [CrossRef]
- Kandel, E.R. A new intellectual framework for psychiatry. Am. J. Psychiatry 1998, 155, 457–469. [Google Scholar] [CrossRef]
- Holzer, M. Targeted temperature management for comatose survivors of cardiac arrest. New Engl. J. Med. 2010, 363, 1256–1264. [Google Scholar] [CrossRef]
- Kelly, G.A. The Psychology of Personal Constructs; Norton: New York, NY, USA; Routledge: London, UK, 1991; Volume 1–2. [Google Scholar]
- Schwanninger, J.; Eisenberg, P.R.; Schechtman, K.B.; Weiss, A.N. A prospective analysis of near-death experiences in cardiac arrest patients. J. Near Death Stud. 2002, 20, 215–232. [Google Scholar] [CrossRef]
- Bailey, N.T.J. Statistical Methods in Biology; The English University Press LTD: London, UK, 1959; pp. 56–58. [Google Scholar]
- Parnia, S.; Waller, D.G.; Yeates, R.; Fenwick, P. A qualitative and quantitative study of the incidence, features and etiology of near death experiences in cardiac arrest survivors. Resuscitation 2001, 48, 149–156. [Google Scholar] [CrossRef]
- Van Lommel, P.; van Wees, R.; Meyers, V.; Elfferich, I. Near-death experience in survivors of cardiac arrest: A prospective study in the Netherlands. Lancet 2001, 358, 2039–2045. [Google Scholar] [CrossRef]
- Knoblauch, H.; Schmied, I.; Schnettler, B. Different kinds of near-death experience: A report on a survey on near-death experiences in Germany. J. Near Death Stud. 2001, 20, 15–29. [Google Scholar] [CrossRef]
- Greyson, B. Incidence and correlates of near-death experiences in a cardiac care unit. Gen. Hosp. Psychiatry 2003, 25, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Klemenc-Ketis, Z.; Kersnik, J.; Grmec, S. The effect of carbon dioxide on near-death experiences in out-of hospital cardiac arrest survivors: A prospective observational study. Crit. Care 2010, 14, R56. [Google Scholar] [CrossRef] [PubMed]
- Berger, M.L.; Sterz, F.; Parnia, S.; Beisteiner, R. Experience during cardiac arrest: Myth or reality? Intrinsic Act. 2013, 1 (Suppl. S1), A1.21. [Google Scholar] [CrossRef]
- Lallier, F.; Velly, G.; Leon, A. Near-death experiences in survivors of cardiac arrest: A study about demographic, medical, pharmacological and psychological context. Crit. Care 2015, 19 (Suppl. S1), P421. [Google Scholar] [CrossRef]
- Kondziella, D.; Dreier, J.P.; Harboe Olsen, M. Prevalence of near-death experiences in people with and without REM sleep intrusion. Peer J. 2019, 7, e7585. [Google Scholar] [CrossRef]
- Parnia, S.; Keshavarz, T.; McMullin, M.; Williams, T. Awareness and cognitive activity during cardiac arrest. Circulation 2019, 140, A387. [Google Scholar] [CrossRef]
- Thonnard, M.; Charland-Verville, V.; Brédart, S.; Dehon, H.; LeDoux, D.; Laureys, S.; Vanhaudenhuyse, A. Characteristics of near-death experience memories as compared to real and imagined event memories. PLoS ONE 2013, 8, e57620. [Google Scholar] [CrossRef] [PubMed]
- Palmieri, A.; Calvo, V.; Kleinbub, J.R.; Meconi, F.; Marangoni, M.; Barilaro, P.; Broggio, A.; Sambin, M.; Sessa, P. “Reality” of near-death-experience memories: Evidence from a psychodynamic and electrophysiological integrated study. Front. Hum. Neurosci. 2014, 8, 429. [Google Scholar] [CrossRef]
- Cassol, H.; Bonin, E.A.C.; Bastin, C.; Puttaert, N.; Charland-Verville, V.; Laureys, S.; Martial, C. Near-Death Experience memories include more episodic components than flashbulb memories. Front. Psychol. 2020, 11, 888. [Google Scholar] [CrossRef]
- Blanke, O.; Landis, T.; Spinelli, L.; Seeck, M. Stimulating illusory own-body perceptions. Nature 2002, 419, 269–270. [Google Scholar] [CrossRef]
- Blanke, O.; Landis, T.; Spinelli, L.; Seeck, M. Out-of-body experience and autoscopy of neurological origin. Brain 2004, 127, 243–258. [Google Scholar] [CrossRef] [PubMed]
- Plato. Apology. 399 BC. 21d. Available online: https://en.wikipedia.org/wiki/I_know_that_I_know_nothing (accessed on 15 February 2023).
- Kant, I. Prolegomena to Any Future Metaphysics; Cambridge University Press: New York, NY, USA, 1783; p. §52c. Available online: https://en.wikipedia.org/wiki/Prolegomena_to_Any_Future_Metaphysics (accessed on 14 February 2023).
- Popper, K. The Logic of Scientific Discovery; Routledge: Abington-on-Thames, UK, 1959; p. 66. Available online: https://en.wikipedia.org/wiki/The_Logic_of_Scientific_Discovery (accessed on 15 February 2023).
- Kuhn, T.S. The Structure of Scientific Revolutions; University of Chicago Press: Chicago, IL, USA, 1962. [Google Scholar]

| № | Location | Age | Delay (d) | Greyson Points | Recollections |
|---|---|---|---|---|---|
| 24, A | at home | 68.1 | 11 | 7 | Encounter with deceased relatives, daughter signs to her she can go back. |
| 41, B | at home | 47.8 | 34 | 2 | He dreams an actor is in danger, not him; a written message says he would not die. |
| 46, C | tram | 67.2 | 33 | 0 | Dream of upper half of a head watching him from behind a screen; running numbers on a clock. |
| 53, D | at home | 52.3 | 4 | 2 | Reports whiteout (no blackout), feels very fine when waking up a few min later. |
| 58, E | hospital | 73.6 | 10 | 2 | Feeling of a “presence” reassuring nothing bad can happen. |
| 71, F | hospital | 69.9 | 396 | 1 | Dream during waking up: a train takes another track at the moment she opens her eyes. |
| 72, G | near home | 55.8 | 322 | 5 | His body cruising extremely fast in futuristic settings. |
| 74, H | at home | 56.3 | 528 | 3 | Several vivid dreams during prolonged critical period, in one of them features a Thai spirit of death. |
| 75, I | at home | 56.3 | 399 | 2 | Warm wellbeing, bright light in the ambulance. |
| 79, J | hospital | 59.2 | 553 | 11 | Point of view near the bed looking at himself; passes by a garden door while hearing behind the surgeon calling, vivid dreams during waking up. |
| 83, K | hospital | 79.2 | 83 | 1 | Agreeable impression of a meadow with large pink flowers indicating she will come back. |
| 87, L | hiking tour | 45.7 | 272 | 9 * | Feels drawn into a tunnel shining in all colors (“Rohrpost”), impression of roofs and blue sky. |
| 101, M | hospital | 67.7 | 122 | 6 | First of four dreams interrupted by reanimating physician’s voice, meets deceased relatives (mother, aunt: “Fine you are here!”). |
| 103, N | subway | 66.1 | 81 | 3 * | Realistic dream of a cemetery with rails branching, heading for life or death. |
| 109, O | at home | 47.4 | 364 | 8 * | She is in paradise with Allah, bright and warm, she is happy. |
| 111, P | ergometer | 54.9 | 157 | 3 | Silhouettes against bright light, for a moment he opens his eyes to witness his own CPR, returns to the bright light, and is finally reanimated. |
| 115, Q | hospital | 52.0 | 95 | 2 | Realistic impression: she sees herself from behind standing in front of a big wooden door, the door remains closed. |
| 122 R | near home | 76.8 | 63 | 1 | Irrational behavior for 2 weeks, joyful, extremely imaginative, joking, singing. |
| 124, S | at work | 39.6 | 185 | 0 | Haunted by nightmare featuring “bone men” with bones in their hands, threatening her with death. |
| 125, T | at home | 46.5 | 195 | 18 | Finds herself in some kind of antechamber to heaven, bright with blue sky, a stairway leading up; from there, she is sent back by her father (deceased 27 years ago), she still has obligations in her life. |
| Total | NDE | ||
|---|---|---|---|
| Parnia et al. [16] | 63 | 4 | 6.3% |
| Van Lommel et al. [17] | 344 | 23 a | 6.7% |
| Knoblauch et al. [18] | 2044 b | 82 | 4.0% |
| Schwaninger et al. [14] | 30 | 7 c | 23% |
| Greyson [19] | 116 | 11 | 9.5% |
| Klemenc-Ketis et al. [20] | 52 | 11 | 21% |
| Berger et al. [21] | 22 | 0 | <5% |
| Parnia et al. [10] | 101 | 9 | 8.9% |
| Lallier et al. [22] | 118 | 18 | 15% |
| Kondziella et al. [23] | 1034 d | 106 | 10.3% |
| Parnia et al. [24] | 21 | 4 e | 19% |
| actual study | 126 | 5 | 4.0% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sterz, F.; Berger, M.L.; Ruzicka, G.; Beisteiner, R. Lapses of the Heart: Frequency and Subjective Salience of Impressions Reported by Patients after Cardiac Arrest. J. Clin. Med. 2023, 12, 1968. https://doi.org/10.3390/jcm12051968
Sterz F, Berger ML, Ruzicka G, Beisteiner R. Lapses of the Heart: Frequency and Subjective Salience of Impressions Reported by Patients after Cardiac Arrest. Journal of Clinical Medicine. 2023; 12(5):1968. https://doi.org/10.3390/jcm12051968
Chicago/Turabian StyleSterz, Fritz, Michael L. Berger, Gerhard Ruzicka, and Roland Beisteiner. 2023. "Lapses of the Heart: Frequency and Subjective Salience of Impressions Reported by Patients after Cardiac Arrest" Journal of Clinical Medicine 12, no. 5: 1968. https://doi.org/10.3390/jcm12051968
APA StyleSterz, F., Berger, M. L., Ruzicka, G., & Beisteiner, R. (2023). Lapses of the Heart: Frequency and Subjective Salience of Impressions Reported by Patients after Cardiac Arrest. Journal of Clinical Medicine, 12(5), 1968. https://doi.org/10.3390/jcm12051968






