Prevalence of Dental Caries in Patients on Renal Replacement Therapy—A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Focused Question
2.2. Eligibility Criteria
2.3. Search Strategy
2.4. Data Extraction
- year of publication, study type, country
- number of participants, sex, age, type of RRT, duration of treatment
- caries, tooth loss/remaining teeth/dentures, oral hygiene parameters, glomerular filtration rate, laboratory parameters, saliva parameters, bacteria/-metabolism
- presence of a control group, sex, age
2.5. Quality Assessment
3. Results
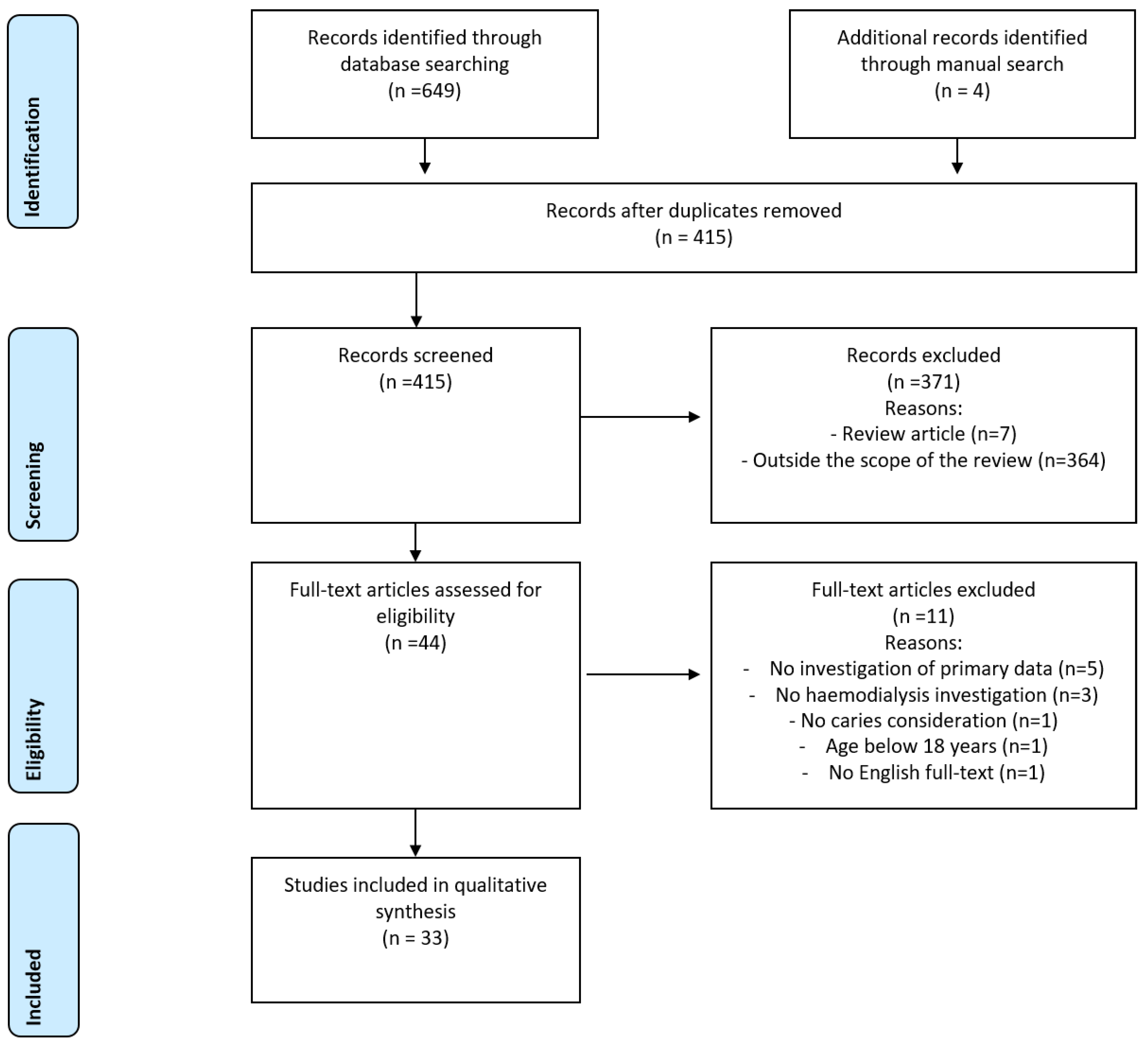
3.1. Search Findings
3.2. Characteristics of Included Studies
3.3. Oral Health Record and Findings
3.4. Quality Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CKD | Chronic kidney disease |
| CPI | community periodontal index |
| CRP | C-reactive protein |
| D-T | number of decayed teeth |
| DMF-T | decayed-, missing- and filled teeth index |
| eGFR | estimated glomerular filtration rate |
| F-T | number of filled teeth |
| GI | gingival index |
| HD | hemodialysis |
| KTx | kidney transplantation |
| M-T | number of missing teeth |
| PI | plaque index |
| RRT | renal replacement therapy |
References
- Kassebaum, N.J.; Bernabe, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.L.; Marcenes, W. Global Burden of Untreated Caries: A Systematic Review and Metaregression. J. Dent. Res. 2015, 94, 650–658. [Google Scholar] [CrossRef]
- Peres, M.A.; Macpherson, L.M.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef] [PubMed]
- Wen, P.; Chen, M.; Zhong, Y.; Dong, Q.; Wong, H. Global Burden and Inequality of Dental Caries, 1990 to 2019. J. Dent. Res. 2022, 101, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Pitts, N.B.; Zero, D.T.; Marsh, P.D.; Ekstrand, K.; Weintraub, J.A.; Ramos-Gomez, F.; Tagami, J.; Twetman, S.; Tsakos, G.; Ismail, A. Dental caries. Nat. Rev. Dis. Primers 2017, 3, 17030. [Google Scholar] [CrossRef]
- Sabharwal, A.; Stellrecht, E.; Scannapieco, F.A. Associations between dental caries and systemic diseases: A scoping review. BMC Oral Health 2021, 21, 472. [Google Scholar] [CrossRef]
- Cassolato, S.F.; Turnbull, R.S. Xerostomia: Clinical Aspects and Treatment. Gerodontology 2003, 20, 64–77. [Google Scholar] [CrossRef]
- Bossola, M. Xerostomia in patients on chronic hemodialysis: An update. Semin. Dial. 2019, 32, 467–474. [Google Scholar] [CrossRef]
- Cengiz, M.; Sümer, P.; Cengiz, S.; Yavuz, U. The effect of the duration of the dialysis in hemodialysis patients on dental and periodontal findings. Oral Dis. 2009, 15, 336–341. [Google Scholar] [CrossRef]
- Rezazadeh, F.; Bazargani, A.; Roozbeh-Shahroodi, J.; Pooladi, A.; Arasteh, P.; Zamani, K. Comparison of oral Lactobacillus and Streptococcus mutans between diabetic dialysis patients with non-diabetic dialysis patients and healthy people. J. Ren. Inj. Prev. 2016, 5, 148–152. [Google Scholar] [CrossRef]
- Mizutani, K.; Mikami, R.; Gohda, T.; Gotoh, H.; Aoyama, N.; Matsuura, T.; Kido, D.; Takeda, K.; Izumi, Y.; Sasaki, Y.; et al. Poor oral hygiene and dental caries predict high mortality rate in hemodialysis: A 3-year cohort study. Sci. Rep. 2020, 10, 21872. [Google Scholar] [CrossRef]
- Schmalz, G.; Patschan, S.; Patschan, D.; Ziebolz, D. Oral health-related quality of life in adult patients with end-stage kidney diseases undergoing renal replacement therapy—A systematic review. BMC Nephrol. 2020, 21, 154. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Rostom, A.; Dube, C.; Cranney, A. Celiac Disease; Evidence Reports/Technology Assessments, No. 104; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2004. Available online: https://www.ncbi.nlm.nih.gov/books/NBK35156/ (accessed on 29 January 2020).
- Yue, Q.; Yin, F.-T.; Zhang, Q.; Yuan, C.; Ye, M.-Y.; Wang, X.-L.; Li, J.-J.; Gan, Y.-H. Carious status and supragingival plaque microbiota in hemodialysis patients. PLoS ONE 2018, 13, e0204674. [Google Scholar] [CrossRef]
- Schmalz, G.; Kollmar, O.; Vasko, R.; Müller, G.; Haak, R.; Ziebolz, D. Oral health-related quality of life in patients on chronic haemodialysis and after kidney transplantation. Oral Dis. 2016, 22, 665–672. [Google Scholar] [CrossRef]
- Gautam, N.R.; Koganti, R.; Rao, T.H.; Agarwal, R.; Alamanda, M. Effect of end-stage renal disease on oral health in patients undergoing renal dialysis: A cross-sectional study. J. Int. Soc. Prev. Community Dent. 2014, 4, 164–169. [Google Scholar] [CrossRef]
- da Cruz, A.J.S.; de Castilho, L.S.; Contarini, L.C.S.; Silva, M.E.D.S.E.; Abreu, M.H.N.G. Dental Findings of Kidney and Liver Transplantation Patients from a Brazilian Oral Health Care Service. Pesqui. Bras. Em Odontopediatria E Clínica Integr. 2021, 21. [Google Scholar] [CrossRef]
- Ziebolz, D.; Fischer, P.; Hornecker, E.; Mausberg, R.F. Oral health of hemodialysis patients: A cross-sectional study at two German dialysis centers. Hemodial. Int. 2012, 16, 69–75. [Google Scholar] [CrossRef]
- Sekiguchi, R.T.; Pannuti, C.M.; Silva, H.T., Jr.; Medina-Pestana, J.O.; Romito, G.A. Decrease in oral health may be associated with length of time since beginning dialysis. Spec. Care Dent. 2012, 32, 6–10. [Google Scholar] [CrossRef]
- Bayraktar, G.; Kurtulus, I.; Duraduryan, A.; Cintan, S.; Kazancıoğlu, R.T.; Yildiz, A.; Bural, C.; Bozfakioglu, S.; Besler, M.; Trablus, S.; et al. Dental and periodontal findings in hemodialysis patients. Oral Dis. 2007, 13, 393–397. [Google Scholar] [CrossRef]
- Tiwari, V.; Saxena, V.; Bhambhal, A.; Tiwari, U.; Singh, A.; Goud, S. The oral health status of patients with renal disease in central india: A preliminary study. J. Ren. Care 2013, 39, 208–213. [Google Scholar] [CrossRef]
- Tadakamadla, J.; Kumar, S.; Mamatha, G.P. Comparative evaluation of oral health status of chronic kidney disease (CKD) patients in various stages and healthy controls. Spec. Care Dent. 2014, 34, 122–126. [Google Scholar] [CrossRef]
- Cunha, F.L.; Tagliaferro, E.P.S.; Pereira, A.C.; Meneghim, M.C.; Hebling, E. Oral health of a Brazilian population on renal dialysis. Spec. Care Dent. 2007, 27, 227–231. [Google Scholar] [CrossRef]
- Chuang, S.-F.; Sung, J.-M.; Kuo, S.-C.; Huang, J.-J.; Lee, S.-Y. Oral and dental manifestations in diabetic and nondiabetic uremic patients receiving hemodialysis. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2005, 99, 689–695. [Google Scholar] [CrossRef]
- Benderli, Y.; Erdilek, D.; Koray, F.; Telci, A.; Turan, N. The relation between salivary IgA and caries in renal transplant patients. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endodontology 2000, 89, 588–593. [Google Scholar] [CrossRef]
- Schmalz, G.; Kauffels, A.; Kollmar, O.; Slotta, J.E.; Vasko, R.; Müller, G.A.; Haak, R.; Ziebolz, D. Oral behavior, dental, periodontal and microbiological findings in patients undergoing hemodialysis and after kidney transplantation. BMC Oral Health 2016, 16, 72. [Google Scholar] [CrossRef]
- Schmalz, G.; Dietl, M.; Vasko, R.; Muller, G.; Rothermund, L.; Keller, F.; Ziebolz, D.; Rasche, F. Dialysis vintage time has the strongest correlation to psychosocial pattern of oral health-related quality of life—A multicentre cross-sectional study. Med. Oral Patol. Oral Y Cirugía Bucal 2018, 23, e698–e706. [Google Scholar] [CrossRef]
- Akça, N.K.; Arslan, D.E.; In, H. Examination of factors affecting oral health in patients receiving haemodialysis. J. Ren. Care 2021, 48, 262–271. [Google Scholar] [CrossRef]
- Ruas, B.M.; Castilho, L.S.; Carneiro, N.C.R.; Cardoso, N.M.D.M.; Reis, A.B.; e Silva, M.E.S.; Borges-Oliveira, A.C. Integrality of care for hemodialysis patient in Brazil: An analysis of access to dental care. Ciência Saúde Coletiva 2020, 25, 533–540. [Google Scholar] [CrossRef]
- Bayraktar, G.; Kazancıoğlu, R.T.; Bozfakioglu, S.; Yildiz, A.; Ark, E. Evaluation of salivary parameters and dental status in adult hemodialysis patients. Clin. Nephrol. 2004, 62, 380–383. [Google Scholar] [CrossRef]
- Buhlin, K.; Bárány, P.; Heimbürger, O.; Stenvinkel, P.; Gustafsson, A. Oral health and pro-inflammatory status in end-stage renal disease patients. Oral Health Prev. Dent. 2007, 5, 235–244. [Google Scholar]
- Al-Wahadni, A.; Al-Omari, M.A. Dental diseases in a Jordanian population on renal dialysis. Quintessence Int. 2003, 34, 343–347. [Google Scholar]
- Pereira-Lopes, O.; Simões-Silva, L.; Araujo, R.; Correia-Sousa, J.; Braga, A.C.; Soares-Silva, I.; Sampaio-Maia, B. Influence of dialysis therapies on oral health: A pilot study. Quintessence Int. 2019, 50, 216–223. [Google Scholar] [CrossRef]
- Bots, C.P.; Brand, H.S.; Poorterman, J.H.G.; Van Amerongen, B.M.; Valentijn-Benz, M.; Veerman, E.C.I.; Ter Wee, P.M.; Amerongen, A.V.N. Oral and salivary changes in patients with end stage renal disease (ESRD): A two year follow-up study. Br. Dent. J. 2007, 202, E7. [Google Scholar] [CrossRef]
- Amaral, M.A.; Miotto, A.M.M.; Moimaz, S.A.S.; Garbin, C.A.S. Self-perception of oral health among tertiary-care users: Quanti-qualitative analysis with chronic kidney disease patients. Acta Sci. Health Sci. 2022, 44, e53802. [Google Scholar] [CrossRef]
- Naugle, K.; Darby, M.L.; Bauman, D.B.; Lineberger, L.T.; Powers, R. The Oral Health Status of Individuals on Renal Dialysis. Ann. Periodontol. 1998, 3, 197–205. [Google Scholar] [CrossRef]
- Souza, C.M.; Braosi, A.P.R.; Luczyszyn, S.M.; Casagrande, R.W.; Pecoits-Filho, R.; Riella, M.C.; Ignácio, S.A.; Trevilatto, P.C. Oral health in Brazilian patients with chronic renal disease. Rev. Med. Chil. 2008, 136, 741–746. [Google Scholar] [CrossRef]
- Menezes, C.; Pereira, A.; Ribeiro, C.; Chaves, C.; Guerra, R.; Thomaz, É.B.; Monteiro-Neto, V.; Alves, C. Is there association between chronic kidney disease and dental caries? A case-controlled study. Med. Oral Patol. Oral Cir. Bucal. 2019, 24, e211–e216. [Google Scholar] [CrossRef]
- Sobrado Marinho, J.S.; Tomás Carmona, I.; Loureiro, A.; Limeres Posse, J.; García Caballero, L.; Diz Dios, P. Oral health status in patients with moderate-severe and terminal renal failure. Med. Oral Patol. Oral Cir. Bucal. 2007, 12, E305–E310. [Google Scholar]
- Misaki, T.; Fukunaga, A.; Shimizu, Y.; Ishikawa, A.; Nakano, K. Possible link between dental diseases and arteriosclerosis in patients on hemodialysis. PLoS ONE 2019, 14, e0225038. [Google Scholar] [CrossRef]
- Pakpour, A.H.; Kumar, S.; Fridlund, B.; Zimmer, S. A case-control study on oral health-related quality of life in kidney disease patients undergoing haemodialysis. Clin. Oral Investig. 2015, 19, 1235–1243. [Google Scholar] [CrossRef]
- Rocha, L.C.B.; Nunes-Dos-Santos, D.L.; Costa, E.M.; Gomes, S.V.; Rodrigues, V.P.; Pereira, A.L.A. A Cross-Sectional Study of the Association Between Chronic Oral Disease Burden and Serum Biomarkers in Kidney Transplant Recipients. Prog. Transplant. 2021, 32, 49–54. [Google Scholar] [CrossRef]
- Jordan, R.A.; Micheelis, W. The Fifth German Oral Health Study (DMS V). Institut der Deutschen Zahnärzte (Hrsg.); (IDZ Materialienreihe Band 35); Deutscher Zahnärzte Verlag DÄV: Köln, Germany, 2016. (In German) [Google Scholar]
- WHO. World Health Organization: Oral Health Surveys, Basic Methods, 4th ed.; WHO Oral Health Unit: Geneva, Switzerland, 1997. [Google Scholar]
- Ismail, A.I.; Pitts, N.B.; Tellez, M.; Authors of the International Caries Classification and Management System (ICCMS). The International Caries Classification and Management System (ICCMS™) An Example of a Caries Management Pathway. BMC Oral Health 2015, 15 Suppl. 1, S9. [Google Scholar] [CrossRef]
- Ekstrand, K.R.; Gimenez, T.; Ferreira, F.R.; Mendes, F.M.; Braga, M.M. The International Caries Detection and Assessment System—ICDAS: A Systematic Review. Caries Res. 2018, 52, 406–419. [Google Scholar] [CrossRef]
- AlQranei, M.S.; Balhaddad, A.A.; Melo, M.A. The burden of root caries: Updated perspectives and advances on management strategies. Gerodontology 2021, 38, 136–153. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Lueckel, H.; Machiulskiene, V.; Giacaman, R.A. How to Intervene in the Root Caries Process? Systematic Review and Meta-Analyses. Caries Res. 2019, 53, 599–608. [Google Scholar] [CrossRef] [PubMed]
- Kreher, D.; Park, K.-J.; Schmalz, G.; Schulz-Kornas, E.; Haak, R.; Ziebolz, D. Evaluation of quantitative light-induced fluorescence to assess lesion depth in cavitated and non-cavitated root caries lesions—An in vitro study. Photodiagnosis Photodyn. Ther. 2022, 37, 102675. [Google Scholar] [CrossRef]
- Litzenburger, F.; Schäfer, G.; Hickel, R.; Kühnisch, J.; Heck, K. Comparison of novel and established caries diagnostic methods: A clinical study on occlusal surfaces. BMC Oral Health 2021, 21, 97. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Tzschoppe, M.; Paris, S. Radiographic caries detection: A systematic review and meta-analysis. J. Dent. 2015, 43, 924–933. [Google Scholar] [CrossRef] [PubMed]
- Janjic Rankovic, M.; Kapor, S.; Khazaei, Y.; Crispin, A.; Schüler, I.; Krause, F.; Ekstrand, K.; Michou, S.; Eggmann, F.; Lussi, A.; et al. Systematic review and meta-analysis of diagnostic studies of proximal surface caries. Clin. Oral Investig. 2021, 25, 6069–6079. [Google Scholar] [CrossRef]
- Brouwer, F.; Askar, H.; Paris, S.; Schwendicke, F. Detecting Secondary Caries Lesions: A Systematic Review and Meta-analysis. J. Dent. Res. 2015, 95, 143–151. [Google Scholar] [CrossRef] [PubMed]
- Misaki, T.; Fukunaga, A.; Nakano, K. Dental caries status is associated with arteriosclerosis in patients on hemodialysis. Clin. Exp. Nephrol. 2020, 25, 87–93. [Google Scholar] [CrossRef]
- Chiu, C.-C.; Chang, Y.-C.; Huang, R.-Y.; Chan, J.-S.; Chung, C.-H.; Chien, W.-C.; Kao, Y.-H.; Hsiao, P.-J. Investigation of the Impact of Endodontic Therapy on Survival among Dialysis Patients in Taiwan: A Nationwide Population-Based Cohort Study. Int. J. Environ. Res. Public Health 2021, 18, 326. [Google Scholar] [CrossRef]
- Ebert, T.; Neytchev, O.; Witasp, A.; Kublickiene, K.; Stenvinkel, P.; Shiels, P.G. Inflammation and Oxidative Stress in Chronic Kidney Disease and Dialysis Patients. Antioxidants Redox Signal. 2021, 35, 1426–1448. [Google Scholar] [CrossRef]
- Ebert, T.; Pawelzik, S.-C.; Witasp, A.; Arefin, S.; Hobson, S.; Kublickiene, K.; Shiels, P.G.; Bäck, M.; Stenvinkel, P. Inflammation and Premature Ageing in Chronic Kidney Disease. Toxins 2020, 12, 227. [Google Scholar] [CrossRef]
- Ebert, T.; Tran, N.; Schurgers, L.; Stenvinkel, P.; Shiels, P.G. Ageing—Oxidative stress, PTMs and disease. Mol. Asp. Med. 2022, 86, 101099. [Google Scholar] [CrossRef]
- Piccoli, G.B.; Lippi, F.; Fois, A.; Gendrot, L.; Nielsen, L.; Vigreux, J.; Chatrenet, A.; D’Alessandro, C.; Cabiddu, G.; Cupisti, A. Intradialytic Nutrition and Hemodialysis Prescriptions: A Personalized Stepwise Approach. Nutrients 2020, 12, 785. [Google Scholar] [CrossRef]
- Ostermann, M.; Lumlertgul, N.; Mehta, R. Nutritional assessment and support during continuous renal replacement therapy. Semin. Dial. 2021, 34, 449–456. [Google Scholar] [CrossRef]
- Bossola, M.; Tazza, L. Xerostomia in patients on chronic hemodialysis. Nat. Rev. Nephrol. 2012, 8, 176–182. [Google Scholar] [CrossRef]
- Syed-Ahmed, M.; Narayanan, M. Immune Dysfunction and Risk of Infection in Chronic Kidney Disease. Adv. Chronic Kidney Dis. 2019, 26, 8–15. [Google Scholar] [CrossRef]
- Schmalz, G.; Schiffers, N.; Schwabe, S.; Vasko, R.; Müller, G.A.; Haak, R.; Mausberg, R.F.; Ziebolz, D. Dental and periodontal health, and microbiological and salivary conditions in patients with or without diabetes undergoing haemodialysis. Int. Dent. J. 2017, 67, 186–193. [Google Scholar] [CrossRef]
- Wilczynska-Borawska, M.; Baginska, J.; Borawski, J. Is xerostomia a risk factor for cardiovascular morbidity and mortality in maintenance hemodialysis patients? Med. Hypotheses 2012, 79, 544–548. [Google Scholar] [CrossRef]

| Author, Year | Form of RRT | Country | No. of Patients | Study Type | Subjects Mean Age in Years | Treatment Time | Male (%) | Control Group | ||
|---|---|---|---|---|---|---|---|---|---|---|
| HD | PD | Tx | ||||||||
| Yue et al. 2018 [14] | HD | China | 30 | monocentric | 48.53 ± 12.69 | >12 month | n/a | n/a | 50 | 30, 46.50 ± 8.83, 53% men |
| Schmalz et al. 2016 [15] | HD, Tx | Germany | 126 (HD: 87; Tx: 39) | clinical multicentre cross-sectional | HD: 60.98 ± 14.01; KTx: 56.51 ± 11.56 | ≥5 years | n/a | ≥5 years | HD: 62.1; KTx: 48.7 | 91, 58.31 ± 9.91, 43.1% men |
| Gautam et al. 2014 [16] | HD | India | 206 | multicentre cross-sectional | 46.79 ± 12.78 | 69%, <1 year, 13.6%, 1–3 years, 16.5% >3 years | n/a | n/a | 81.1 | n/a |
| Cruz et al. 2021 [17] | HD, Tx | Brazil | 46 | descriptive cross-sectional | 18–44: 43.5%; 45–54: 21.7%; 55–80: 34.8% | n/a | n/a | 80.4% pre Tx, 19.6% post Tx | 71.4 | n/a |
| Ziebolz et al. 2012 [18] | HD | Germany | 54 | multicentre clinical cross-sectional | 63.9 ± 13.0 | 4.1 ± 3.4 years | n/a | n/a | 57 | n/a |
| Misaki et al. 2021 [10] | HD | Japan | 80 (13 died during 2 year follow up → 67 surviving) | monocentric | 67.3 ± 12.2 (surviving group: 65.8 ± 11.9) | 7.6 ± 5.9 years | n/a | n/a | 60 (surviving group: 54) | n/a |
| Sekiguchi et al. 2012 [19] | HD | Brazil | 94 | monocentric cross sectional | <3 y HD: 56% 20–39 years, 44% 40–79 years; >3 y HD: 36.32% 20–39 years; 63.68% 40–79 years | 1.: <36 months; 2.: >37 months | n/a | n/a | <3 years HD: 52; >3 years HD: 56.8 | n/a |
| Cengiz et al. 2009 [8] | HD | Turkey | 86 | monocentric cross sectional | 47.85 ± 14.61 | n/a | n/a | n/a | 54 | 41, 44.80 ± 10.22, 52% men |
| Bayraktar et al. 2007 [20] | HD | Turkey | 76 | multicentre cross sectional | 48 ± 15 | 17: HD <3 years, 59: HD >3 years | n/a | n/a | 47 | 61, 36% men, 46 ± 18 |
| Tiwari et al. 2013 [21] | HD | India | 30 | monocentric matched case-control study | 35–44: 23.3%; 45–54: 36.6%; 55–64: 40% | n/a | n/a | n/a | 93.3 | 30, 35–44: 23.3%, 45–54: 36.6%, 55–64: 40%, 93.3% men |
| Tadakamadla et al. 2014 [22] | HD | India | 74 | monocentric cross sectional | 46.27 ± 1.42 | n/a | n/a | n/a | 64.5 | 150, 43.14 ± 2.31 |
| Cunha et al. 2007 [23] | HD | Brazil | 160 | multicentre cross sectional | 59 ± 12 | average time: 2 years (11 months to 11 years) | n/a | n/a | 56.9 | n/a |
| Chuang et al. 2005 [24] | HD | Taiwan | 128 | monocentric cross sectional | 57.5 | mean duration 3.72 years (range of 0.1 to 10 years) | n/a | n/a | 45.3 | n/a |
| Benderli et al. 2000 [25] | Tx | Turkey | 28 (G1: 13, G2: 5, G3: 10) | monocentric cross sectional | 18–54 | n/a | n/a | G1: 0–6 months after transplantation, 6–12 months after transplantation, >12 months after transplantation | n/a | 10 |
| Schmalz et al. 2016 [26] | HD, Tx | Germany | 70 (HD: 35; Tx: 35) | monocentric cross-sectional | HD: 56.4 ± 11.1, Tx: 55.8 ± 10.9 | 5.5 ± 6.4 (<1 year: 13.3%, >1 to 5 years: 38.2%, >5 years: 35.3%) | n/a | >1 to 5 years: 11.4%, <5 years: 88.4% | HD: 60, Tx: 47 | n/a |
| Schmalz et al. 2018 [27] | HD | Germany | 190 | multicentre cross sectional | 64.92 ± 15.7 | 0–2 years (n = 29), 3–5 years (n = 35), 6–8 years (n = 34), 9–12 years (n = 29), 13–20 years (n = 34), >20 years (n = 29) | n/a | n/a | 65 | n/a |
| Akca et al. 2021 [28] | HD | Turkey | 150 | monocentric cross sectional | 58.73 (14.59) | 54.67 (47.73) months (at least 6 month) | n/a | n/a | 54 | n/a |
| Ruas et al. 2018 [29] | HD | Brazil | 567 | multicentre cross sectional | 49.9 ± 13.7 | <5 years: 66%, >5 years 34% | n/a | n/a | 58 | n/a |
| Bayraktar et al. 2004 [30] | HD | Turkey | 72 | monocentric cross sectional | 45.05 ± 14.15 | 32.56 ± 40.17 | n/a | n/a | 53 | 50, 43.92 ± 18.80, 48% men |
| Buhlin et al. 2007 [31] | HD | Sweden | 51 | monocentric cross sectional | 55.3 (13.0) | n/a | n/a | n/a | 65 | n/a |
| Al-Wahadni et al. 2003 [32] | HD | Jordan | 47 | monocentric cross sectional | 42.9 ± 12.5 | 1: HD <1 year, 2: HD 1–3 years, 3: HD >3 year | n/a | n/a | 51.06 | n/a |
| Pereira-Lopes et al. 2019 [33] | HD, PD | Portugal | 63 (17 HD, 35 PD, 11 PD after HD) | Monocentric cross sectional | HD: 53.8 ± 6.8, PD: 46.6 ± 12.3, PD after HD: 45.3 ± 13.6 | 33.5 months | PD: 5.8 months, PD after HD: 79.9 | n/a | HD: 82.4, PD: 48.6, PD after HD: 45.5 | n/a |
| Bots et al. 2007 [34] | HD, Tx | Netherlands | 43 (20 of them Tx during study period | monocentric prospective observation study | men: 54 ± 15.7; women: 48.9 ± 17.2 | 33 ± 28.6 month at baseline | n/a | 13.5 ± 7.1 month before second measurement | 69.3 | n/a |
| Amaral et al. 2022 [35] | HD | Brazil | 60 | monocentric cross sectional | 60.23 ± 10.87 | 41.9 ± 56.57 month (45 pat <48 month, 15 pat >48 month) | n/a | n/a | 73.33 | n/a |
| Naugle et al. 1998 [36] | HD | USA | 45 | multicentre cross sectional | n/a | 1. (N = 9) pat haemodialysis <1 y, 2. (N = 22) 1–3 y, 3. (N = 14) >3y | n/a | n/a | n/a | n/a |
| Schmalz et al. 2017 [27] | HD | Germany | 159 | multicentre clinical cross-sectional study | Without DM: 66.7 ± 13, with DM: 70.5 ± 10.2 | Without DM: 4.4 ± 4.1y; with DM: 3.3 ± 2.7 | n/a | n/a | Without DM: 63, with DM: 65 | n/a |
| Souza et al. 2008 [37] | HD, PD, Tx | Chile | 286 CKD: 13 (4.5%) predialysis, 158 (55%) haemodialysis, 23 (8.4%) peritoneal dialysis, 92 (32.1%) Tx | monocentric cross sectional | 42 ± 13 | n/a | n/a | n/a | 53 | n/a |
| Menezes et al. 2019 [38] | HD | Brazil | 107 | monocentric cross-sectional | 44.64 (20–87) | 36 month | n/a | n/a | 61.7 | 107, 43.97, 55.14% |
| Marinho et al. 2007 [39] | HD | Portugal | 50 pat: 22 pharmacological-dietary treatment pat., 28 haemodialysis pat. | monocentric observational, case-control study | 64 ± 11 | n/a | n/a | n/a | 46 | 64, 60 ± 11 46.9% |
| Misaki et al. 2019 [40] | HD | Japan | 80 | monocentric cross sectional | 67.3 ± 12.2 | n/a | n/a | n/a | 60 | 76, 66.6 ± 12.1, 57.9% men |
| Pakpour et al. 2014 [41] | HD | Iran | 512 | multicentre case-controlled study | 57.7 ± 17.01 | 52.12 ± 29.86 month | n/a | n/a | 62.9 | 255, 55.8 ± 15.9, 62% men |
| Mizutani et al. 2020 [10] | HD | Japan | 207 | monocentric prospective observational study with 3 years follow-up | 65.9 ± 12.1 | 64 (33, 115) month | n/a | n/a | 65.2 | n/a |
| Rocha et al. 2022 [42] | Tx | Brazil | 44 | monocentric cross-sectional comparative study | 45.07 ± 13.87 | n/a | n/a | >6 month | 56.82 | n/a |
| Author, Year | Tooth Loss, Remaining Teeth, Dentures | Caries | Oral Hygiene Parameters | Glomerular Filtration Rate (mL/min/1.73 m2) | Laboratory Parameters | Saliva Parameters (Saliva Flow Rate, pH) | Bacterial-/Metabolism | ||
|---|---|---|---|---|---|---|---|---|---|
| CRP (mg/L) | Serum Creatinine (µmol/L) | Saliva Flow Rate | pH | ||||||
| Yue et al. 2018 [14] | >15 | DMFT: 4.36 ± 3.92; DT: 1.11 ± 1.62 | PI: 2.13 ± 0.45 | <15 | 3.09 ± 5.15 | 1041.76 ± 216.93 | n/a | 8.21 ± 0.44 | Proteobacteria, Firmicutes, Bacteroidetes, Fusobacteria, Actinobacteria; heterogeneity of supragingival plaque in CKD patients was higher than in control group |
| Schmalz et al. 2016 [15] | >6 | HD: DMFT: 20.43 ± 5.85, DT: 2.29 ± 4.13; KTx: 17.41 ± 5.51, 0.74 ± 1.43 | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| Gautam et al. 2014 [16] | n/a | Prevalence: 65.3% | CPI (bleeding 0%, calculus 13.1%, pocket 4–5 mm 44.2%, pocket > 6 mm 39.32) | <15 | n/a | n/a | n/a | n/a | n/a |
| Cruz et al. 2021 [17] | n/a | DMFT median: 20.0, DT median: 1.0 | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| Ziebolz et al. 2012 [18] | 12 patients (22%) of 54 were toothless | DMFT (n = 54) 22.1 ± 6.5, DT (n = 54) 0.7 ± 1.2; DMFT (n = 42) 20.4 ± 6.4, DT (n = 42) 0.9 ± 1.2 | PDI: median 1 | n/a | n/a | n/a | n/a | n/a | n/a |
| Misaki et al. 2021 [10] | n/a | DMFT: 18.5 ± 6.7, DT: 1.7 ± 2.6 | PI and GI; median PI HD: 2.00, PI C: 1.00; GI HD: 0.29, GI C: 0.19 | n/a | 0.4 ± 1.6 | n/a | n/a | n/a | n/a |
| Sekiguchi et al. 2012 [19] | >12 | DMFT group L: 12.14 ± 5.36, group M: 14.34 ± 4.80; DT group L: 2.52 ± 2.22, group M: 4.68 ± 2.60 | PI group L: 1.22 ± 0.56, GI group L: 0.88 ± 0.42; PI group M: 1.17 ± 0.55, GI: 1.00 ± 0.41 | n/a | n/a | n/a | n/a | n/a | n/a |
| Cengiz et al. 2009 [8] | n/a | DMF-T HD: 12.7 ± 8.1; C: 11.7 ± 5.5 | PI and GI; PI HD: 2.1 ± 8.1; C: 1.7 ± 5.5; GI HD: 1.9 ± 0.3, C: 1.1 ± 0.2 | n/a | n/a | n/a | n/a | n/a | n/a |
| Bayraktar et al. 2007 [20] | n/a | DMFT median HD: 12.0, C: 15.00, DT median HD: 2.00, C: 1.00 | PI and GI; median PI HD: 2.00, PI C: 1.00; GI HD: 0.29, GI C: 0.19 | n/a | n/a | n/a | n/a | n/a | n/a |
| Tiwari et al. 2013 [21] | n/a | DMFT HD: 6.37 ± 4.26, C: 2.35 ± 1.28; DT HD: 3.87 ± 4.02, C: 1.63 ± 0.36 | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| Tadakamadla et al. 2014 [22] | n/a | DMFT stage2: 1.64 ± 1.70, stage3: 1.51 ± 1.26, stage4: 1.25 ± 1.58, stage5: 1.37 ± 1.46; DT stage2: 1.32 ± 1.25, stage3: 1.13 ± 0.95, stage4: 1.05 ± 1.35, stage5: 1.05 ± 1.31 | GI: stage 2: 1.26 ± 0.13, stage 3: 1.76 ± 0.16, stage 4: 2.06 ± 0.43, stage 5: 2.40 ± 0.39, controls: 0.92 ± 0.42 | stage1: ≥90, stage2: 60–89, stage3: 30–59, stage4: 15–29, stage5: <15 (or dialysis) | n/a | n/a | n/a | n/a | n/a |
| Cunha et al. 2007 [23] | n/a | DMFT 26.0 ± 7.7, DT 32.9% | CPI (bleeding/ calculus 29.4%, pocket >4 mm 8.8) | n/a | n/a | n/a | n/a | n/a | n/a |
| Chuang et al. 2005 [24] | n/a | DMFT diabetics: 19.93 ± 8.19, DMFT non-diabetics: 14.29 ± 9.19; DT diabetics: 2.00 ± 3.42, DT non-diabetics: 1.94 ± 2.48 | CPI: non-diabetics: Code 0: 1.2%, Code 1: 1.2%, Code 2: 24.7%, Code 3: 45.9%, Code 4: 23.5% CPI: diabetics: Code 0: 0%, Code 1: 2.3%, Code 2: 20.9%, Code 3: 39.5%, Code 4: 16.3% | n/a | n/a | n/a | n/a | diabetics: 7.97 ± 0.67, non-diabetics: 8.22 ± 0.44 | n/a |
| Benderli et al. 2000 [25] | n/a | Incidence: G1: 1.15, G2: 1.4, G3: 4.3 | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| Schmalz et al. 2016 [26] | 5 of 70 were toothless | DMFT HD: 19.47 ± 5.84, DMFT KT: 17.61 ± 5.81; DT HD: 1.13 ± 1.68, DT KT: 0.58 ± 1.15 | PBI: HD: 0.38 ± 0.27, KT: 0.52 ± 0.49 | n/a | n/a | n/a | n/a | n/a | yes: 11 different periodontal pathogenic bacteria) most prevalence: Eikanella corrodens and Parvimonas micra > Fusobacterium nucleatum > Tanerella forsythia |
| Schmalz et al. 2018 [27] | 16.90 ± 8.8 | DMFT: 20.45 ± 6.8 | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| Akca et al. 2021 [28] | n/a | DT: 1.15 ± 2.33 | gum bleeding: 14.0% | n/a | n/a | predialysis: 8.51 ± 2.75, postdialysis: 3.25 ± 1.48 | dryness mouth: 81.3% | n/a | n/a |
| Ruas et al. 2018 [29] | average number 19.3 ± 8.7 | Prevalence: 20.4% | Gingivitis: 20.3% | n/a | n/a | n/a | n/a | n/a | n/a |
| Bayraktar et al. 2004 [30] | n/a | DMFT: HD: 11.91 ± 8.73, controls 13.22 ± 9.68 | n/a | n/a | n/a | n/a | Stimulated saliva HD: 0.69 ± 0.31, controls: 1.64 ± 0.44 | Stimulated saliva HD: 8.15 ± 0.72, controls: 7.16 ± 0.75 | n/a |
| Buhlin et al. 2007 [31] | average: 22.9 (7.3) | DMFT: 20.1 ± 6.6 | oral plaque index: 46 ± 24% | estimated by creatinine clearance from 24h urine samples | 3.58 (0.3–218.0) | 727 (247) | n/a | n/a | n/a |
| Al-Wahadni et al. 2003 [32] | n/a | DMFT: 8.47 ± 2.88, DT: 5.07 ± 1.75 | PI: 1.59 ± 0.60; GI: 2.16 ± 0.87 | n/a | n/a | n/a | n/a | n/a | n/a |
| Pereira-Lopes et al. 2019 [33] | n/a | DMFT HD: 12.0 ± 9.0, PD: 13.0 ± 7.0, PD after HD: 15.0 ± 4.0; DT HD: 3.0 ± 3.0, PD: 3.0 ± 3.0, PD after HD: 4.0 ± 3. | VPI (visible plaque index): HD: 85.0 ± 26.0, PD: 69.0 ± 30.0, PD after HD: 60.0 ± 38.0 | n/a | n/a | HD: 9.2, PD: 7.0, PD after HD: 9.3 | unstimulated HD: 0.3 ± 0.2, PD: 0.4 ± 0.4. PD after HD: 0.4 ± 0.4, stimulated HD: 1.0 ± 0.5, PD: 1.1 ± 1.4, PD after HD: 0.8 ± 0.5 | unstimulated HD: 7.3 ±0.7, PD: 7.6 ± 0.6, PD after HD: 7.4 ± 0.5, stimulated HD: 7.8 ± 0.4, PD: 7.8 ± 0.4, PD after HD: 7.8 ± 0.5 | n/a |
| Bots et al. 2007 [34] | n/a | Dia. Treatment: DIAL-base: DMFS 39.1 (26.9), DMFT 13.6 (8.5) DIAL-2yr: DMFS 41.6 (27.8), DMFT 14.4 (8.8); TX: DIAL-base: DMFS 41.9 (26.6), DMFT 14.9 (8.1) TX-2yr DMFS 43.1 (25.3) DMFT 15.5 (7.8) | SOHI | n/a | n/a | n/a | Dia. Treatment: DIAL-base: UWS 0.31 (0.19), SWS 1.18 (0.8) DIAL-2yr: UWS 0.31 (0.18), SWS 1.09 (0.54); TX: DIAL-base: UWS 0.3 (0.21), SWS 1.12 (0.66) TX-2yr UWS 0.44 (0.29) SWS 1.38 (0.84) | Dia. Treatment: DIAL-base: UWS 7.28 (0.52), SWS 7.44 (0.43) DIAL-2yr: UWS 7.1 (0.71), SWS 7.28 (0.57); TX: DIAL-base: UWS 7.36 (0.49), SWS 7.39 (0.42) TX-2yr UWS 6.74 (0.4) SWS 7.0 (0.24) | n/a |
| Amaral et al. 2022 [35] | n/a | DMFT: 22.55 ± 8.39 (D: 0.86 ± 1.59, M: 18.2 ± 10.99, F: 3.49 ± 4.63) | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| Naugle et al. 1998 [36] | n/a | subgroup: 1: 11.88 ± 8.06, 2: 13.57 ± 9.06, 3: 9.87 ± 5.53; grand totals: 11.77 (D: 1.8 M: 4.9 F: 4.8) | SOHI: subgroup: 1: 3.18 ± 1.13, 2: 3.35 ± 1.42, 3: 3.17 ± 1.21; grand totals: 3.241 ± 1.26 (N = 44) | n/a | n/a | n/a | n/a | n/a | n/a |
| Schmalz et al. 2017 [27] | n/a | DMFT all pat: nDM: 22.3 ± 5.5; DM: 21.9 ± 6.1; DMFT pat with teeth: nDM: 21.2 ± 5.4 (D: 1.4 ± 2.1 M: 12.8 ± 8.6 F: 7 ± 5); DM: 20.4 ± 6 (D: 2.1 ± 3 M: 10.8 ± 7.8 F: 7.7 ± 5.5) | n/a | n/a | n/a | n/a | unstimulated: nDM: 0.23 ± 0.23; DM: 0.16 ± 0.2 stimulated: nDM: 0.5 ± 0.4; DM: 0.42 ± 0.42 | unstimulated: nDM: 7 ± 0.9; DM: 6.7 ± 0.7 | n/a |
| Souza et al. 2008 [37] | n/a | DMFT: all pat.: 20.6; Pre 22; HD 21; PD 24; Tx 20 | presence of Calculus: 86.7% | n/a | n/a | n/a | n/a | n/a | n/a |
| Menezes et al. 2019 [38] | n/a | DMFT CKD pat: 14.8 ± 8 (D: 2.9 ± 2.7, M: 11.4 ± 8.7, F: 0.5 ± 1.5); Controls: 16.4 ± 7.7 (D: 3.2 ± 3.2, M: 11.6 ± 8.5, F: 1.6 ± 2.5) | Plaque index: CKD 1.1 ± 0.6; Controls: 1.2 ± 0.8 | n/a | n/a | n/a | n/a | n/a | n/a |
| Marinho et al. 2007 [39] | n/a | DMFT: Pat 17.14 ± 7.79 (D: 1.68 ± 1.57 M: 14.08 ± 9.12 F: 2.34 ± 2.75); controls 15.23 ± 70.7 (D: 2.58 ± 2.48 M: 9.09 ± 7.95 F: 4.32 ± 2.49) DMFT of pat: CRF pat 20.64 ± 6.19 (D:2.36 ± 1.27); TRF pat 14.39 ± 7.91 (D: 1.29 ± 1.62) | simplified Greene and Vermillion oral hygiene index: Pat 10 (26.3%) Grade 0–1, 28 (73.7%) G2–3 (differences between CRF and TRF!), controls 32 (56.1%), 25 (43.9%); Ramfjord calculus index: Pat 19 (50%) G0–1, 19 (50%) G2–3, controls 24 (42.1%), 33 (57.9%) | <60 | n/a | n/a | n/a | n/a | n/a |
| Misaki et al. 2019 [40] | n/a | DMFT: HD pat 19 ± 6.6 (D: 1.9 ± 2.9, M: 8 ± 8.7 F: 9.1 ± 6.5); controls 17.3 ± 6.7 (D: 1.6 ± 2.2 M: 5.2 ± 7.4 F: 10.6 ± 5.5); total number of C4 teeth: HD pat 0.7 ± 1.5; controls 0.2 ± 0.7 | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| Pakpour et al. 2014 [41] | n/a | DMFT: HD pat 20.06 ± 11.16 (D: 0.91 ± 1.93, M: 11.71 ± 7.68 F: 7.37 ± 8.02); controls 10.57 ± 6.74 (D: 2.51 ± 2.12 M: 6.4 ± 4.21 F: 1.43 ± 1.6) | modified Quigley-Hein index visual plaque index: HD pat 1.92 ± 1.28; controls 1.18 ± 1 | n/a | n/a | n/a | n/a | n/a | n/a |
| Mizutani et al. 2020 [10] | 22 (16, 26) mean 19.9 ± 7.1 | DT: mean D: 1.1 ± 2.0 F: 8.3 ± 5.3 | DI-S: mean 0.99 ± 0.76 | n/a | hsCRP 0.16 (0.05, 0.45) | n/a | n/a | n/a | n/a |
| Rocha et al. 2022 [42] | n/a | DMFT: n/a | n/a | n/a | n/a | n/a | n/a | n/a | n/a |
| Author, Year | Caries Disease Group | Caries Healthy Control Group | Significant Difference between Disease and Control |
|---|---|---|---|
| Yue et al. 2018 [14] | DMFT: 4.36 ± 3.92; DT: 1.11 ± 1.62 | DMFT: 2.28 ± 2.52, DT: 0.10 ± 0.31 | yes |
| Schmalz et al. 2016 [15] | HD: DMFT: 20.43 ± 5.85, DT: 2.29 ± 4.13; KTx: 17.41 ± 5.51, 0.74 ± 1.43 | DMFT: 16.76 ± 6.37, DT: 0.01 ± 0.10 | yes |
| Cengiz et al. 2009 [8] | DMFT: 12.7 ± 8.1 | DMFT: 11.7 ± 5.5 | no |
| Bayraktar et al. 2007 [20] | DMFT median: 12.0 (9.00-18.00), DT median HD: 2.00 (0.25-3.00) | DMFT median: 15.00 (6.50-21.50), DT median: 1.00 (0.00-3.00) | no |
| Tiwari et al. 2013 [21] | DMFT HD: 6.37 ± 4.26, DT HD: 3.87 ± 4.02 | DMFT: 2.35 ± 1.28, DT: 1.63 ± 0.36 | DMFT: yes, DT: no |
| Tadakamadla et al. 2014 [22] | DMFT: 1.37 ± 1.46; DT: 1.05 ± 1.31 | DMFT: 2.24 ± 1.82, DT: 2.19 ± 1.79 | DMFT: no, DT: yes |
| Benderli et al. 2000 [25] | Incidence: G1: 1.15, G2: 1.4, G3: 4.3 | Incidence: 1.1 | G3: yes |
| Bayraktar et al. 2004 [30] | DMFT: HD: 11.91 ± 8.73 | DMFT: 13.22 ± 9.68 | no |
| Marinho et al. 2007 [39] | DMFT: 17.14 ± 7.79 DT: 1.68 ± 1.57 | DMFT: 15.23 ± 7.07, DT: 2.58 ± 2.48 | no |
| Misaki et al. 2019 [40] | DMFT: 19 ± 6.6, DT: 1.9 ± 2.9 | DMFT: 17.3 ± 6.7, DT: 1.6 ± 2.2 | no |
| Pakpour et al. 2014 [41] | DMFT: 20.06 ± 11.16, DT: 0.91 ± 1.93 | DMFT: 10.57 ± 6.74, DT: 2.51 ± 2.12 | yes |
| Item | (1) Define the Source of Information (Survey, Record Review) | (2) List Inclusion and Exclusion Criteria for Exposed and Unexposed Subjects (Cases and Controls) Or Refer to Previous Publications | (3) Indicate Time Period Used for Identifying Patients | (4) Indicate Whether or Not Subjects Were Consecutive If Not Population-Based | (5) Indicate If Evaluators of Subjective Components of Study Were Masked to Other Aspects of the Status of the Participants | (6) Describe any Assessments Undertaken for Quality Assurance Purposes (e.g., Test/Retest of Primary Outcome Measurements) | (7) Explain Any Patient Exclusions from Analysis | (8) Describe How Confounding Was Assessed And/or Controlled | (9) If Applicable, Explain How Missing Data Were Handled in the Analysis | (10) Summarize Patient Response Rates and Completeness of Data Collection | (11) Clarify What Follow-Up, If Any, Was Expected and the Percentage of Patients for Which Incomplete Data or Follow-Up Was Obtained | Total Score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Yue et al. 2018 [14] | Yes | yes | no | yes | no | yes | Yes | no | n/a | yes | n/a | 6 |
| Schmalz et al. 2016 [15] | Yes | yes | no | yes | no | no | Yes | no | n/a | yes | n/a | 5 |
| Gautam et al. 2014 [16] | Yes | yes | yes | yes | no | no | Yes | no | n/a | yes | n/a | 6 |
| Cruz et al. 2021 [17] | Yes | yes | yes | yes | no | no | Yes | no | n/a | yes | n/a | 6 |
| Ziebolz et al. 2012 [18] | yes | yes | no | yes | no | no | n/a | no | n/a | yes | n/a | 4 |
| Misaki et al. 2021 [10] | yes | no | yes | yes | no | no | Yes | yes | n/a | yes | yes | 7 |
| Sekiguchi et al. 2012 [19] | yes | yes | no | yes | yes | yes | Yes | no | n/a | yes | n/a | 7 |
| Cengiz et al. 2009 [8] | yes | no | yes | yes | no | yes | Yes | no | n/a | yes | n/a | 6 |
| Bayraktar et al. 2007 [20] | yes | no | no | yes | no | no | Yes | no | n/a | yes | n/a | 4 |
| Tiwari et al. 2013 [21] | yes | yes | no | yes | no | yes | Yes | no | n/a | yes | n/a | 6 |
| Tadakamadla et al. 2014 [22] | yes | yes | yes | yes | yes | no | Yes | no | n/a | yes | n/a | 7 |
| Cunha et al. 2007 [23] | yes | yes | no | yes | no | yes | Yes | no | n/a | yes | n/a | 6 |
| Chuang et al. 2005 [24] | yes | yes | no | yes | no | yes | Yes | no | n/a | yes | n/a | 6 |
| Benderli et al. 2000 [25] | yes | no | no | no | no | no | Yes | no | n/a | yes | n/a | 3 |
| Schmalz et al. 2016 [26] | yes | yes | yes | yes | no | no | Yes | no | n/a | yes | n/a | 6 |
| Schmalz et al. 2018 [27] | yes | yes | no | yes | no | no | Yes | no | n/a | yes | n/a | 5 |
| Akca et al. 2021 [28] | yes | yes | yes | yes | no | no | Yes | no | n/a | yes | n/a | 6 |
| Ruas et al. 2018 [29] | yes | no | no | yes | no | yes | Yes | no | n/a | yes | n/a | 5 |
| Bayraktar et al. 2004 [30] | yes | no | no | yes | no | no | Yes | no | n/a | yes | n/a | 4 |
| Buhlin et al. 2007 [31] | yes | no | no | yes | no | no | Yes | no | n/a | yes | n/a | 4 |
| Al-Wahadni et al. 2003 [32] | yes | no | no | yes | no | yes | Yes | no | n/a | yes | n/a | 5 |
| Pereira-Lopes et al. 2019 [33] | yes | yes | yes | yes | no | yes | Yes | no | n/a | yes | n/a | 7 |
| Bots et al. 2007 [34] | yes | no | no | yes | no | no | Yes | no | n/a | yes | n/a | 4 |
| Amaral et al. 2022 [35] | yes | yes | yes | yes | no | no | Yes | no | n/a | yes | n/a | 6 |
| Naugle et al. 1998 [36] | yes | yes | no | yes | no | yes | n/a | no | n/a | yes | n/a | 5 |
| Schmalz et al. 2017 [27] | yes | yes | no | yes | no | yes | Yes | no | n/a | yes | n/a | 6 |
| Souza et al. 2008 [37] | yes | no | no | yes | no | no | Yes | no | n/a | yes | n/a | 4 |
| Menezes et al. 2019 [38] | yes | yes | no | yes | no | no | Yes | no | n/a | yes | n/a | 5 |
| Marinho et al. 2007 [39] | yes | yes | no | yes | no | no | Yes | no | n/a | yes | n/a | 5 |
| Misaki et al. 2019 [40] | yes | no | yes | yes | no | no | Yes | no | n/a | yes | n/a | 5 |
| Pakpour et al. 2014 [41] | yes | yes | yes | yes | no | yes | Yes | no | n/a | yes | n/a | 7 |
| Mizutani et al. 2020 [10] | yes | no | yes | yes | no | no | Yes | no | n/a | yes | yes | 6 |
| Rocha et al. 2022 [42] | yes | yes | no | yes | no | yes | Yes | no | n/a | yes | yes | 7 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kreher, D.; Ernst, B.L.V.; Ziebolz, D.; Haak, R.; de Fallois, J.; Ebert, T.; Schmalz, G. Prevalence of Dental Caries in Patients on Renal Replacement Therapy—A Systematic Review. J. Clin. Med. 2023, 12, 1507. https://doi.org/10.3390/jcm12041507
Kreher D, Ernst BLV, Ziebolz D, Haak R, de Fallois J, Ebert T, Schmalz G. Prevalence of Dental Caries in Patients on Renal Replacement Therapy—A Systematic Review. Journal of Clinical Medicine. 2023; 12(4):1507. https://doi.org/10.3390/jcm12041507
Chicago/Turabian StyleKreher, Deborah, Bero Luke Vincent Ernst, Dirk Ziebolz, Rainer Haak, Jonathan de Fallois, Thomas Ebert, and Gerhard Schmalz. 2023. "Prevalence of Dental Caries in Patients on Renal Replacement Therapy—A Systematic Review" Journal of Clinical Medicine 12, no. 4: 1507. https://doi.org/10.3390/jcm12041507
APA StyleKreher, D., Ernst, B. L. V., Ziebolz, D., Haak, R., de Fallois, J., Ebert, T., & Schmalz, G. (2023). Prevalence of Dental Caries in Patients on Renal Replacement Therapy—A Systematic Review. Journal of Clinical Medicine, 12(4), 1507. https://doi.org/10.3390/jcm12041507







