Short-Term Outcomes and Risk Factors of In-Hospital Mortality in Patients Suffering Acute Mesenteric Ischemia after Cardiac Surgery: Role of Opioids and Lactic Acid
Abstract
1. Introduction
2. Materials and Methods
2.1. Definition of Gastrointestinal Complications
2.2. Surgical Approach
2.3. Data Collection
2.4. Outcomes
2.5. Predictors of Acute Mesenteric Ischemia after Cardiac Surgery
2.6. Risk Factors of In-Hospital Mortality
2.7. Ethics
2.8. Statistical Analysis
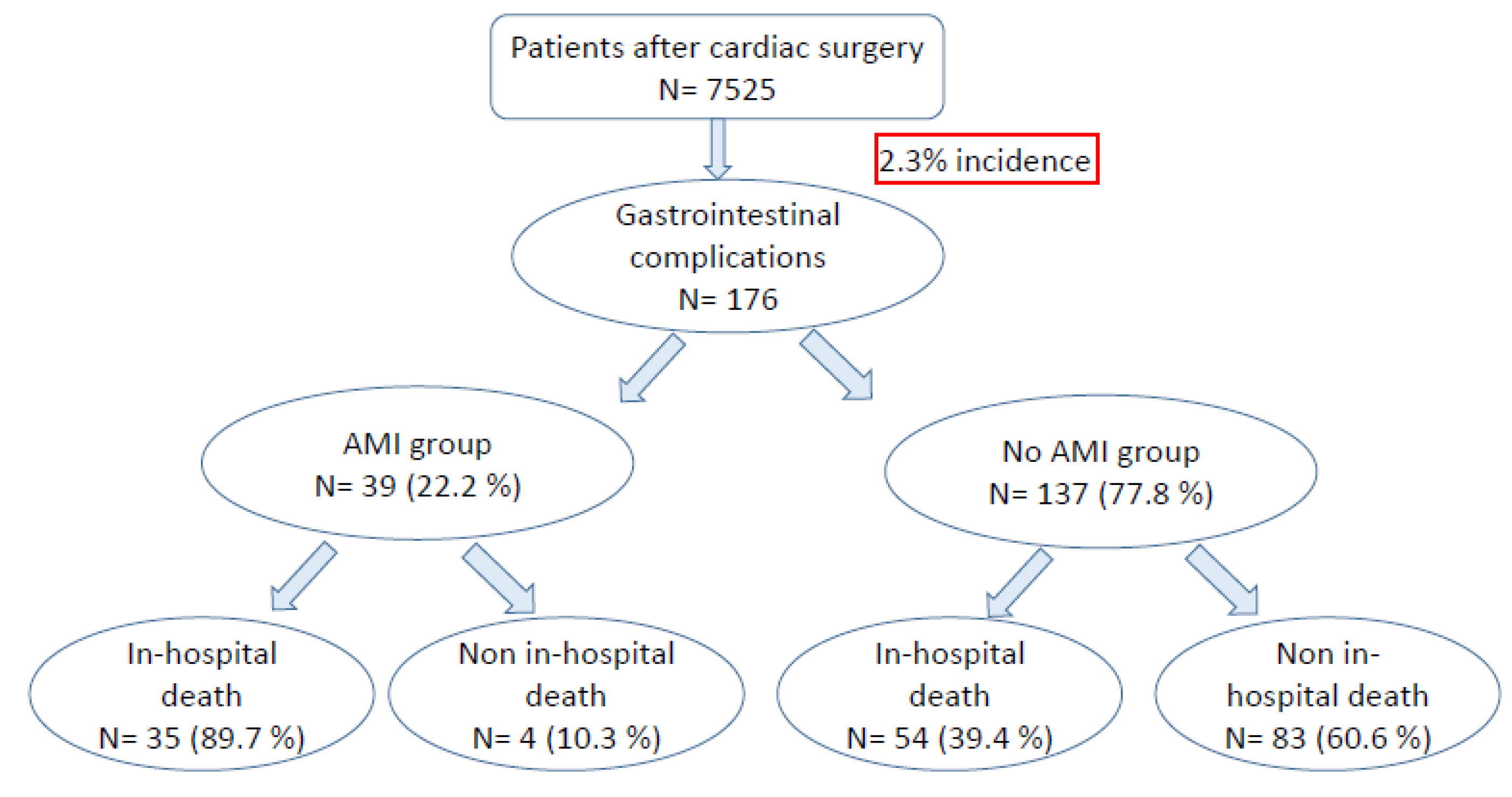
3. Results
3.1. Baseline Data
3.2. Intraoperative Data
3.3. Postoperative Data
3.4. Analysis of Combined Risk Factor: Opioid Infusion and Lactic Acid Elevation
3.5. Combined Risk Factor for In-Hospital Mortality
4. Discussion
5. Conclusions
6. Study Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Viana, F.F.; Chen, Y.; Almeida, A.A.; Baxter, H.D.; Cochrane, A.D.; Smith, J.A. Gastrointestinal complications after cardiac surgery: 10-year experience of a single Australian centre. ANZ J. Surg. 2013, 83, 651–656. [Google Scholar] [CrossRef] [PubMed]
- Mayumi, T.; Yoshida, M.; Tazuma, S.; Furukawa, A.; Nishii, O.; Shigematsu, K.; Azuhata, T.; Itakura, A.; Kamei, S.; Kondo, H.; et al. Practice Guidelines for Primary Care of Acute Abdomen 2015. J. Hepato–Biliary–Biliary Pancreat Sci. 2016, 23, 3–36. [Google Scholar] [CrossRef] [PubMed]
- Luther, B.; Mamopoulos, A.; Lehmann, C.; Klar, E. The Ongoing Challenge of Acute Mesenteric Ischemia. Visc. Med. 2018, 34, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, R.; Zaki, J.; Wegner, R.; Pednekar, G.; Tse, A.; Sheinbaum, R.; Williams, G.W. Gastrointestinal Complications after Cardiac Surgery: A Nationwide Population-Based Analysis of Morbidity and Mortality Predictors. J. Cardiothorac. Vasc. Anesth. 2017, 31, 1268–1274. [Google Scholar] [CrossRef] [PubMed]
- Krämer, S.C.; Görich, J.; Oertel, F.; Scheld, H.; Heindel, W. Non-occlusive mesenteric ischemia. Rofo 2003, 175, 1177–1183. [Google Scholar]
- Mastoraki, A.; Mastoraki, S.; Tziava, E.; Touloumi, S.; Krinos, N.; Danias, N.; Lazaris, A.; Arkadopoulos, N. Mesenteric ischemia: Pathogenesis and challenging diagnostic and therapeutic modalities. World J. Gastrointest. Pathophysiol. 2016, 7, 125. [Google Scholar] [CrossRef]
- Bobadilla, J.L. Mesenteric ischemia. Surg. Clin. N. Am. 2013, 93, 925–940. [Google Scholar] [CrossRef]
- van den Heijkant, T.C.; Aerts, B.A.; Teijink, J.A.; Buurman, W.A.; Luyer, M.D. Challenges in diagnosing mesenteric ischemia. World J. Gastroenterol. 2013, 19, 1338–1341. [Google Scholar] [CrossRef]
- Zachariah, S.K. Adult necrotizing enterocolitis and non occlusive mesenteric ischemia. J. Emergencies Trauma Shock 2011, 4, 430–432. [Google Scholar] [CrossRef]
- Lorusso, R.; Mariscalco, G.; Vizzardi, E.; Bonadei, I.; Renzulli, A.; Gelsomino, S. Acute Bowel Ischemia after Heart Operations. Ann. Thorac. Surg. 2014, 97, 2219–2227. [Google Scholar] [CrossRef]
- Yap, K.H.; Chua, K.; Lim, S.; Sin, Y.K. Is it possible to predict the risk of ischaemic bowel after cardiac surgery? Interact. Cardiovasc. Thorac. Surg. 2014, 19, 494–498. [Google Scholar] [CrossRef]
- Takeyoshi, D.; Shirasaka, T.; Shibagaki, K.; Okubo, R.; Kunioka, S.; Kikuchi, Y.; Kamiya, H. Mesenteric Ischemia after Cardiac Surgery in Dialysis Patients: An Overlooked Risk Factor. Heart Surg. Forum 2022, 25, E732–E738. [Google Scholar] [CrossRef]
- Djordjevic, I.; Eghbalzadeh, K.; Heinen, S.; Schlachtenberger, G.; Gerfer, S.; Sabashnikov, A.; Merkle, J.; Weber, C.; Kuhn, E.; Zeriouh, M.; et al. Risk Factors Associated with In-Hospital Mortality for Patients with Acute Abdomen after Cardiac Surgery. World J. Surg. 2020, 44, 277–284. [Google Scholar] [CrossRef]
- Yilmaz, A.T.; Arslan, M.; Demirkilic, U.; Ozal, E.; Kuralay, E.; Bingol, H.; Oz, B.S.; Tatar, H.; Oztürk, O.Y. Gastrointestinal complications after cardiac surgery. Eur. J. Cardiothorac. Surg. 1996, 10, 763–767. [Google Scholar] [CrossRef]
- Huddy, S.P.J.; Joyce, W.; Pepper, J.R. Gastrointestinal complications in 4473 patients who underwent cardiopulmonary bypass surgery. Br. J. Surg. 1991, 78, 293–296. [Google Scholar] [CrossRef]
- Pang, P.Y.; Sin, Y.K.; Lim, C.H.; Su, J.W.; Chua, Y.L. Outcome and survival analysis of intestinal ischaemia following cardiac surgery. Interact. Cardiovasc. Thorac. Surg. 2012, 15, 215–218. [Google Scholar] [CrossRef]
- Tofukuji, M.; Stahl, G.; Metais, C.; Tomita, M.; Agah, A.; Bianchi, C.; Fink, M.P.; Sellke, F.W. Mesenteric dysfunction after cardiopulmonary bypass: Role of complement C5a. Ann. Thorac. Surg. 2000, 69, 799–807. [Google Scholar] [CrossRef]
- Hecker, A.; Hecker, B.; Kipfmüller, K.; Holler, J.; Schneck, E.; Reichert, M.; Weigand, M.A.; Padberg, W.; Hecker, M. Diagnosis and therapy of an acute abdomen. Med. Klin. Intensivmed. Notfmed. 2014, 109, 445–458. [Google Scholar] [CrossRef]
- Nilsson, J.; Hansson, E.; Andersson, B. Intestinal ischemia after cardiac surgery: Analysis of a large registry. J. Cardiothorac. Surg. 2013, 8, 156. [Google Scholar] [CrossRef]
- Abboud, B.; Daher, R.; Boujaoude, J. Acute mesenteric ischemia after cardiopulmonary bypass surgery. World J. Gastroenterol. 2008, 14, 5361–5370. [Google Scholar] [CrossRef]
- Deng, Q.-W.; Tan, W.-C.; Zhao, B.-C.; Deng, W.-T.; Xu, M.; Liu, W.-F.; Liu, K.-X. Risk factors for postoperative acute mesenteric ischemia among adult patients undergoing cardiac surgery: A systematic review and meta-analysis. J. Crit. Care 2017, 42, 294–303. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, F.; Nguyen, T.C.; Galanko, J.A.; Morton, J. Gastrointestinal Complications after Coronary Artery Bypass Grafting: A National Study of Morbidity and Mortality Predictors. J. Am. Coll. Surg. 2007, 205, 741–747. [Google Scholar] [CrossRef] [PubMed]
- Zacharias, A.; Schwann, T.A.; Parenteau, G.L.; Riordan, C.J.; Durham, S.J.; Engoren, M.; Fenn-Buderer, N.; Habib, R.H. Predictors of gastrointestinal complications in cardiac surgery. Tex. Heart Inst. J. 2000, 27, 93–99. [Google Scholar] [PubMed]
- Bronicki, R.A.; Hall, M. Cardiopulmonary Bypass-Induced Inflammatory Response: Pathophysiology and Treatment. Pediatr. Crit. Care Med. 2016, 17 (Suppl. S1), S272–S278. [Google Scholar] [CrossRef] [PubMed]
- Moneta, G.L.; Misbach, G.A.; Ivey, T.D. Hypoperfusion as a possible factor in the development of gastrointestinal complications after cardiac surgery. Am. J. Surg. 1985, 149, 648–650. [Google Scholar] [CrossRef]
- Sanisoglu, I.; Guden, M.; Bayramoglu, Z.; Sagbas, E.; Dibekoglu, C.; Sanisoglu, S.; Akpinar, B. Does off-pump CABG reduce gastrointestinal complications? Ann. Thorac. Surg. 2004, 77, 619–625. [Google Scholar] [CrossRef]
- Pakula, A.M.; Skinner, R.A. Acute Kidney Injury in the Critically Ill Patient: A Current Review of the Literature. J. Intensive Care Med. 2016, 31, 319–324. [Google Scholar] [CrossRef]
- Bragg, D.; El-Sharkawy, A.; Psaltis, E.; Maxwell-Armstrong, C.; Lobo, D.N. Postoperative ileus: Recent developments in pathophysiology and management. Clin. Nutr. 2015, 34, 367–376. [Google Scholar] [CrossRef]
- Goettsch, W.G.; Sukel, M.P.P.; van der Peet, D.L.; van Riemsdijk, M.M.; Herings, R.M.C. In-hospital use of opioids increases rate of coded postoperative paralytic ileus. Pharmacoepidemiol. Drug Saf. 2007, 16, 668–674. [Google Scholar] [CrossRef]
- Byhahn, C.; Strouhal, U.; Martens, S.; Mierdl, S.; Kessler, P.; Westphal, K. Incidence of gastrointestinal complications in cardiopulmonary bypass patients. World J. Surg. 2001, 25, 1140–1144. [Google Scholar] [CrossRef]
- Saini, H.S.; Alvi, Z.; Singh, B.; Elsharkawy, B.; Yasir, M. Methylnaltrexone and Naloxone for Opioid-induced Constipation in the Critical Care Setting. Cureus 2020, 12, e6829. [Google Scholar] [CrossRef]
- Merchan, C.; Altshuler, D.; Papadopoulos, J. Methylnaltrexone Versus Naloxone for Opioid-Induced Constipation in the Medical Intensive Care Unit. Ann. Pharmacother. 2017, 51, 203–208. [Google Scholar] [CrossRef]
- Patel, P.B.; Brett, S.J.; O’Callaghan, D.; Anjum, A.; Cross, M.; Warwick, J.; Gordon, A.C. Methylnaltrexone for the treatment of opioid-induced constipation and gastrointestinal stasis in intensive care patients. Results from the MOTION trial. Intensive Care Med. 2020, 46, 747–755. [Google Scholar] [CrossRef]
- Verma, I.; Kaur, S.; Goyal, S.; Goyal, S.; Multani, J.S.; Narang, A.P.S. Diagnostic Value of Lactate Levels in Acute Abdomen Disorders. Indian J. Clin. Biochem. 2014, 29, 382–385. [Google Scholar] [CrossRef]
- Dohle, D.-S.; Bestendonk, C.; Petrat, F.; Tsagakis, K.; Wang, M.; Strucksberg, K.-H.; Canbay, A.; Jakob, H.; De Groot, H. Serum markers for early detection of patients with mesenteric ischemia after cardiac surgery. Innov. Surg. Sci. 2018, 3, 277–283. [Google Scholar] [CrossRef]
- Hong, J.; Gilder, E.; Blenkiron, C.; Jiang, Y.; Evennett, N.J.; Petrov, M.S.; Phillips, A.R.; Windsor, J.A.; Gillham, M. Nonocclusive mesenteric infarction after cardiac surgery: Potential biomarkers. J. Surg. Res. 2017, 211, 21–29. [Google Scholar] [CrossRef]
| Non-AMI Group (n = 137) | AMI Group (n = 39) | p-Value | |
|---|---|---|---|
| Age (years), mean ± SD | 71 ± 11 | 73 ± 11 | 0.737 |
| Male gender, n (%) | 105 (76.6%) | 21 (53.8%) | 0.005 |
| Euroscore II, mean ± SD | 7.7 ± 3.7 | 8.0 ± 4.1 | 0.631 |
| Renal insufficiency, n (%) | 60 (43.8%) | 22 (56.4%) | 0.164 |
| PVD, n (%) | 23 (16.8%) | 10 (25.6%) | 0.211 |
| Atrial fibrillation, n (%) | 66 (48.2%) | 13 (33.3%) | 0.123 |
| Previous abdominal surgery, n (%) | 35 (25.5%) | 12 (30.8%) | 0.515 |
| Inotropes before surgery, n (%) | 15 (10.9%) | 5 (12.8%) | 0.776 |
| Non-AMI Group (n = 137) | AMI Group (n = 39) | p-Value | |
|---|---|---|---|
| CABG, n (%) | 76 (55.5%) | 18 (46.2%) | 0.303 |
| Valve surgery, n (%) | 53 (38.7%) | 18 (46.2%) | 0.402 |
| Combined procedure, n (%) | 8 (5.8%) | 3 (7.6%) | 0.462 |
| Urgent procedure, n (%) | 27 (19.7%) | 9 (23.1%) | 0.645 |
| CPB, n (%) | 114 (83.2%) | 33 (84.6%) | 0.835 |
| CPB time (min), mean ± SD | 122 ± 59 | 157 ± 76 | 0.007 |
| Cross clamp time (min), mean ± SD | 66 ± 37 | 96 ± 51 | <0.001 |
| Requirement for MAD, n (%) | 37 (27.0%) | 6 (15.4%) | 0.136 |
| Non-AMI Group (n = 137) | AMI Group (n = 39) | p-Value | |
|---|---|---|---|
| Absolut arrhythmia, n (%) | 76 (55.5%) | 24 (61.5%) | 0.500 |
| Dialysis, n (%) | 56 (40.9%) | 29 (74.4%) | <0.001 |
| CPR, n (%) | 7 (5.1%) | 5 (12.8%) | 0.141 |
| ARDS, n (%) | 46 (33.6%) | 19 (48.7%) | 0.084 |
| Duration of MV, days, mean ± SD | 7 ± 12 | 8 ± 11 | 0.587 |
| Laparotomy, n (%) | 24 (17.5%) | 26 (66.7%) | <0.001 |
| Paralytic ileus, n (%) | 57 (41.6%) | 10 (25.6%) | 0.070 |
| Septic shock, n (%) | 40 (29.2%) | 15 (38.5%) | 0.271 |
| Onset of symptoms, PD, median ± SD | 6 ± 18 | 7 ± 31 | 0.167 |
| Silent abdomen, n (%) | 28 (20.4%) | 12 (30.8%) | 0.174 |
| Abdominal muscular defense, n (%) | 3 (2.2%) | 6 (15.4%) | 0.004 |
| In-hospital stay, days, median ± SD | 17 ± 41 | 16 ± 41 | 0.616 |
| In-hospital mortality, n (%) | 54 (39.4%) | 35 (89.7%) | <0.001 |
| Combined Risk Factor | Total Number of Patients | Mesenteric Ischemia | Univariate Analysis p-Value | Multivariate Analysis p-Value | OR (CI 95%) |
|---|---|---|---|---|---|
| Lactic acid <2 mmol/L −opioids | 43 | 4.7% (n = 2) | 0.001 | 0.160 | 0.280 (0.048–1.651) |
| Lactic acid <2 mmol/L +opioids | 27 | 14.8% (n = 4) | 0.318 | 0.323 | 0.566 (0.183–1.749) |
| Lactic acid >2 mmol/L −opioids | 57 | 22.8% (n = 13) | 0.886 | 0.398 | 1.699 (0.497–5.806) |
| Lactic acid >2 mmol/L +opioids | 49 | 40.8% (n = 20) | <0.001 | 0.025 | 3.966 (1.188–13.231) |
| Combined Risk Factors | Univariate Logistic Regression Model | Multivariate Logistic Regression Model | ||
|---|---|---|---|---|
| OR (CI 95%) | p-Value | OR (CI 95%) | p-Value | |
| Sex | 1.073 (0.876–3.313) | 0.117 | 1.814 (0.823–3.998) | 0.140 |
| PVD | 0.373 (0.165–0.839) | 0.017 | 0.241 (0.091–0.637) | 0.004 |
| Urgent OP | 0.675 (0.322–1.415) | 0.298 | 0.658 (0.275–1.573) | 0.346 |
| Previous abdominal OP | 1.093 (0.560–2132) | 0.794 | 1.378 (0.597–3.179) | 0.452 |
| Requirement for MAD | 0.517 (0.255–1.448) | 0.067 | 0.811 (0.897–0.367) | 0.811 |
| Dialysis | 0.295 (0.159–0.547) | 0.001 | 0.369 (0.173–0.788) | 0.010 |
| Septic shock | 0.255 (0.127–0.512) | 0.001 | 0.297 (0.134–0.657) | 0.003 |
| Duration of MV | 1.030 (0.999–1.061) | 0.057 | 1.015 (0.986–1045) | 0.305 |
| Noradrenaline (HD) | 1.885 (1.411–2.519) | 0.001 | 1.341 (0.939–1.915) | 0.107 |
| CPR | 0.488 (0.141–1.684) | 0.256 | 0.263 (0.064–1.078) | 0.064 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krasivskyi, I.; Djordjevic, I.; Tayeh, M.; Eghbalzadeh, K.; Ivanov, B.; Avgeridou, S.; Gerfer, S.; Gaisendrees, C.; Suhr, L.; Sabashnikov, A.; et al. Short-Term Outcomes and Risk Factors of In-Hospital Mortality in Patients Suffering Acute Mesenteric Ischemia after Cardiac Surgery: Role of Opioids and Lactic Acid. J. Clin. Med. 2023, 12, 857. https://doi.org/10.3390/jcm12030857
Krasivskyi I, Djordjevic I, Tayeh M, Eghbalzadeh K, Ivanov B, Avgeridou S, Gerfer S, Gaisendrees C, Suhr L, Sabashnikov A, et al. Short-Term Outcomes and Risk Factors of In-Hospital Mortality in Patients Suffering Acute Mesenteric Ischemia after Cardiac Surgery: Role of Opioids and Lactic Acid. Journal of Clinical Medicine. 2023; 12(3):857. https://doi.org/10.3390/jcm12030857
Chicago/Turabian StyleKrasivskyi, Ihor, Ilija Djordjevic, Mahmoud Tayeh, Kaveh Eghbalzadeh, Borko Ivanov, Soi Avgeridou, Stephen Gerfer, Christopher Gaisendrees, Laura Suhr, Anton Sabashnikov, and et al. 2023. "Short-Term Outcomes and Risk Factors of In-Hospital Mortality in Patients Suffering Acute Mesenteric Ischemia after Cardiac Surgery: Role of Opioids and Lactic Acid" Journal of Clinical Medicine 12, no. 3: 857. https://doi.org/10.3390/jcm12030857
APA StyleKrasivskyi, I., Djordjevic, I., Tayeh, M., Eghbalzadeh, K., Ivanov, B., Avgeridou, S., Gerfer, S., Gaisendrees, C., Suhr, L., Sabashnikov, A., Rustenbach, C. J., Mader, N., Doerr, F., & Wahlers, T. (2023). Short-Term Outcomes and Risk Factors of In-Hospital Mortality in Patients Suffering Acute Mesenteric Ischemia after Cardiac Surgery: Role of Opioids and Lactic Acid. Journal of Clinical Medicine, 12(3), 857. https://doi.org/10.3390/jcm12030857











