Comparative Study of Proximal Femur Bone Tumor Patients Undergoing Hemiarthroplasty versus Total Hip Arthroplasty: A Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Literature Search
2.2. Included Studies
2.2.1. Inclusion Criteria
- English language studies including patients diagnosed with primary bone tumors located in the proximal femur;
- Studies comparing patients who had undergone THA and HA;
- Studies that presented comparative data in the respective outcomes of our study.
2.2.2. Exclusion Criteria
- 4.
- Non-English and unpublished studies;
- 5.
- Non-comparative studies in patients undergoing THA and HA with primary bone tumor;
- 6.
- Case reports, reviews, and letters to editors;
- 7.
- Studies that lacked adequate clinical data;
2.3. Study Selection and Data Extraction
2.4. Quality Assessment and Outcome Measurement
2.5. Statistical Analysis
3. Results
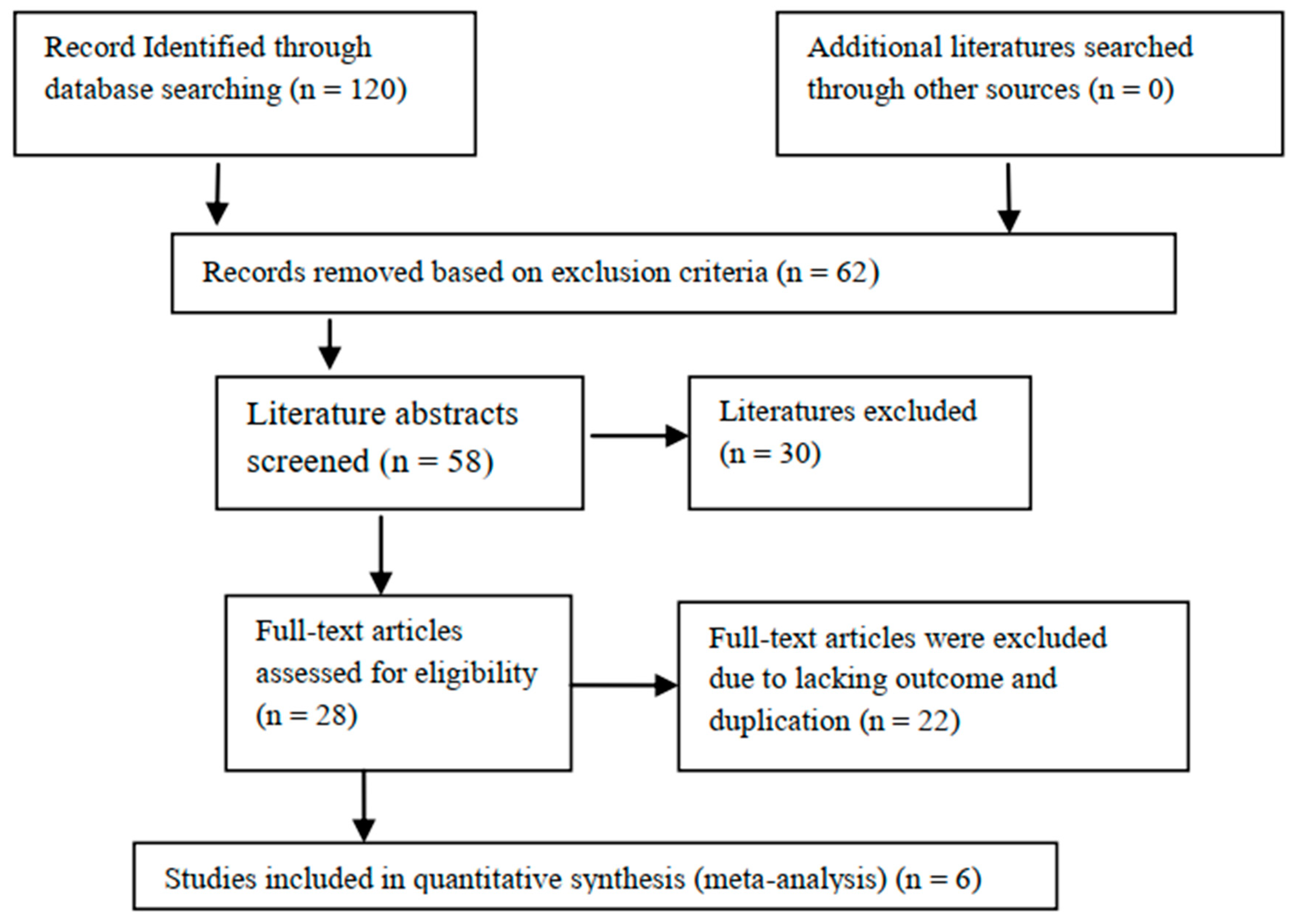
3.1. Study Selection
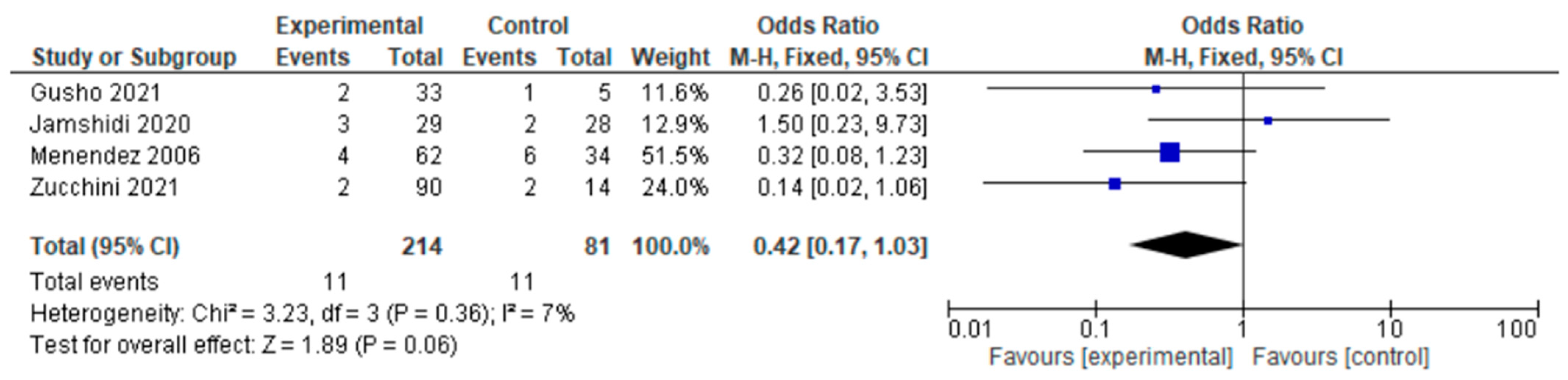
3.2. Dislocation
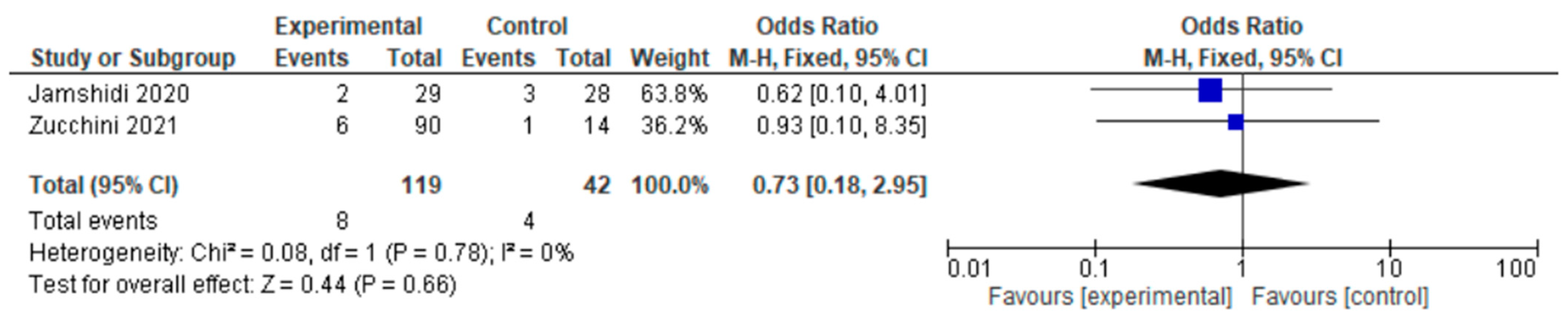
3.3. Infection
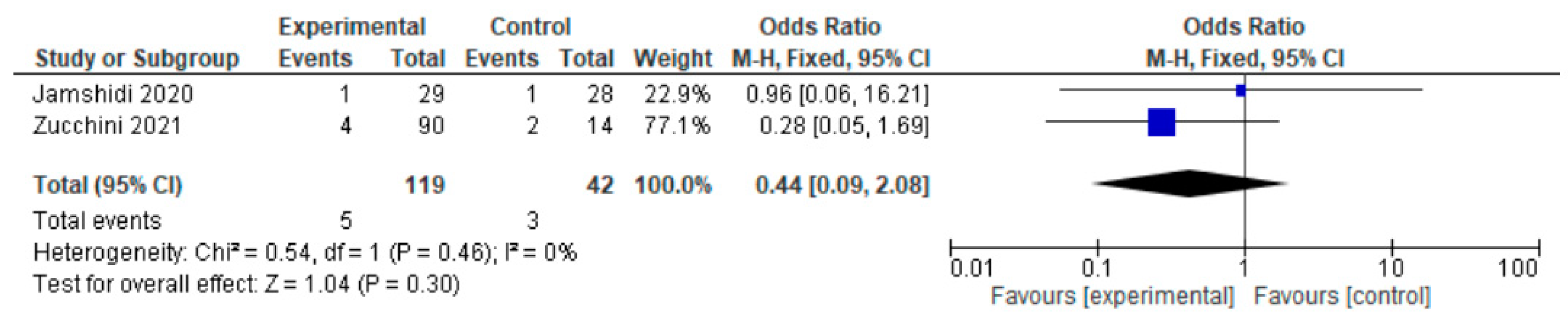
3.4. Local Recurrence
3.5. MSTS
3.6. HHS
3.7. Sensitivity Analysis
3.8. Publication Bias
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Axelrod, D.; Gazendam, A.M.; Ghert, M. The Surgical Management of Proximal Femoral Metastases: A Narrative Review. Curr. Oncol. 2021, 28, 3748–3757. [Google Scholar] [CrossRef]
- Menendez, L.R.; Ahlmann, E.R.; Kermani, C.; Gotha, H. Endoprosthetic Reconstruction for Neoplasms of the Proximal Femur. Clin. Orthop. Relat. Res. 2006, 450, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Khattak, M.J.; Ashraf, U.; Nawaz, Z.; Noordin, S.; Umer, M. Surgical management of metastatic lesions of proximal femur and the hip. Ann. Med. Surg. 2018, 36, 90–95. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Z.-B.; Chen, S.; Gao, Y.-S.; Sun, Y.-Q.; Zhang, C.-Q.; Jiang, Y. Subtrochanteric femur fracture treated by intramedullary fixation. Chin. J. Traumatol. 2015, 18, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Gainor, B.J.; Buchert, P. Fracture Healing in Metastatic Bone Disease. Clin. Orthop. Relat. Res. 1983, 178, 297–302. [Google Scholar] [CrossRef]
- Li, X.; Luo, J. Hemiarthroplasty compared to total hip arthroplasty for the treatment of femoral neck fractures: A systematic review and meta-analysis. J. Orthop. Surg. Res. 2021, 16, 172. [Google Scholar] [CrossRef]
- Riggs, B.; Melton, L., 3rd. The worldwide problem of osteoporosis: Insights afforded by epidemiology. Bone 1995, 17, S505–S511. [Google Scholar] [CrossRef]
- Kannan, A.; Kancherla, R.; McMahon, S.; Hawdon, G.; Soral, A.; Malhotra, R. Arthroplasty options in femoral-neck fracture: Answers from the national registries. Int. Orthop. 2012, 36, 1–8. [Google Scholar] [CrossRef]
- Liu, X.W.; Zi, Y.; Xiang, L.B.; Wang, Y. Total hip arthroplasty: Areview of advances, advantages and limitations. Int. J. Clin. Exp. Med. 2015, 8, 27–36. [Google Scholar]
- Berry, D.J.; Harmsen, W.S.; Cabanela, M.E.; Morrey, B.F. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: Factors affecting survivorship of acetabular and femoral components. J. Bone Jt. Surgery. Am. Vol. 2002, 84, 171–177. [Google Scholar] [CrossRef]
- Hopley, C.; Stengel, D.; Ekkernkamp, A.; Wich, M. Primary total hip arthroplasty versus hemiarthroplasty for displaced intracapsular hip fractures in older patients: Systematic review. BMJ 2010, 340, c2332. [Google Scholar] [CrossRef]
- Khan, A.M.; Rafferty, M.; Daurka, J.S. Hemiarthroplasty compared with total hip arthroplasty in fractured neck of femur: A shift in national practice? Ann. R. Coll. Surg. Engl. 2019, 101, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Ogilvie, C.M.; Wunder, J.S.; Ferguson, P.C.; Griffin, A.; Bell, R.S. Functional Outcome of Endoprosthetic Proximal Femoral Replacement. Clin. Orthop. Relat. Res. 2004, 426, 44–48. [Google Scholar] [CrossRef] [PubMed]
- Zwart, H.J.; Taminiau, A.H.; Schimmel, J.W.; van Horn, J.R. Kotz modular femur and tibia replacement 28 tumor cases followed for 3 (1-8) years. Acta Orthop. Scad. 1994, 65, 315–318. [Google Scholar]
- Guzik, G. Oncological and functional results after surgical treatment of bone metastases at the proximal femur. BMC Surg. 2018, 18, 5. [Google Scholar] [CrossRef] [PubMed]
- Puchner, S.E.; Funovics, P.T.; Hipfl, C.; Dominkus, M.; Windhager, R.; Hofstaetter, J.G. Incidence and management of hip dislocation in tumour patients with a modular prosthesis of the proximal femur. Int. Orthop. 2014, 38, 1677–1684. [Google Scholar] [CrossRef]
- Varady, N.H.; Ameen, B.T.; Hayden, B.L.; Yeung, C.M.; Schwab, P.-E.; Chen, A.F. Short-Term Morbidity and Mortality After Hemiarthroplasty and Total Hip Arthroplasty for Pathologic Proximal Femur Fractures. J. Arthroplast. 2019, 34, 2698–2703. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Lee, Y.J.; Kim, H.B. Association between anaemia and adult depression: A systematic review and meta-analysis of observational studies. J. Epidemiol. Community Health 2020, 74, 565–572. [Google Scholar] [CrossRef]
- He, X.; Gao, Z.; Xu, H.; Zhang, Z.; Fu, P. A meta-analysis of randomized control trials of surgical methods with osteosarcoma outcomes. J. Orthop. Surg. Res. 2017, 12, 5. [Google Scholar] [CrossRef]
- Zucchini, R.; Sambri, A.; Fiore, M.; Giannini, C.; Donati, D.M.; De Paolis, M. Megaprosthesis Reconstruction of the Proximal Femur following Bone Tumour Resection: When Do We Need the Cup? Hip Pelvis 2021, 33, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Jamshidi, K.; Mirkazemi, M.; Gharedaghi, M.; Izanloo, A.; Mohammadpour, M.; Pisoudeh, K.; Bagherifard, A.; Mirzaei, A. Bipolar hemiarthroplasty versus total hip arthroplasty in allograft-prosthesis composite reconstruction of the proximal femur following primary bone tumour resection. Bone Jt. J. 2020, 102-b, 524–529. [Google Scholar] [CrossRef]
- Gusho, C.A.; Clayton, B.; Mehta, N.; Colman, M.W.; Gitelis, S.; Blank, A.T. Survival and outcomes of modular endoprosthetic reconstruction of the proximal femur for primary and non-primary bone tumors: Single institutional results. J. Orthop. 2021, 25, 145–150. [Google Scholar] [CrossRef]
- Bickels, J.; Meller, I.; Henshaw, R.M.; Malawer, M.M. Reconstruction of Hip Stability After Proximal and Total Femur Resections. Clin. Orthop. Relat. Res. 2000, 375, 218–230. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekar, C.R.; Grimer, R.J.; Carter, S.R.; Tillman, R.M.; Abudu, A.; Buckley, L. Modular endoprosthetic replacement for tumours of the proximal femur. J. Bone Jt. Surg. 2009, 91, 108–112. [Google Scholar] [CrossRef]
- Weiss, R.J.; Tullberg, E.; Forsberg, J.A.; Bauer, H.C.; Wedin, R. Skeletal metastases in 301 breast cancer patients: Patient survival and complications after surgery. Breast 2014, 23, 286–290. [Google Scholar] [CrossRef] [PubMed]
- Johnsson, R.; Carlsson, A.; Kisch, K.; Moritz, U.; Zetterström, R.; Persson, B.M. Function following mega total hip arthroplasty compared with conventional total hip arthroplasty and healthy matched controls. Clin. Orthop. Relat. Res. 1985, 192, 159–167. [Google Scholar] [CrossRef]
- Kabukcuoglu, Y.; Grimer, R.J.; Tillman, R.M.; Carter, S.R. Endoprosthetic Replacement for Primary Malignant Tumors of the Proximal Femur. Clin. Orthop. Relat. Res. 1999, 358, 8–14. [Google Scholar] [CrossRef]
- Stevenson, J.D.; Kumar, V.S.; Cribb, G.L.; Cool, P. Hemiarthroplasty proximal femoral endoprostheses following tumour reconstruction: Is acetabular replacement necessary? Bone Jt. J. 2018, 100-b, 101–108. [Google Scholar] [CrossRef]
- Ogawa, T.; Yoshii, T.; Moriwaki, M.; Morishita, S.; Oh, Y.; Miyatake, K.; Nazarian, A.; Shiba, K.; Okawa, A.; Fushimi, K.; et al. Association between Hemiarthroplasty vs Total Hip Arthroplasty and Major Surgical Complications among Patients with Femoral Neck Fracture. J. Clin. Med. 2020, 9, 3203. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.P.; Bhalodiya, H.P. Head size and dislocation rate in primary total hip arthroplasty. Indian J. Orthop. 2013, 47, 443–448. [Google Scholar] [CrossRef]
- Potter, B.K.; Chow, V.E.; Adams, S.C.; Letson, G.D.; Temple, H.T. Endoprosthetic proximal femur replacement: Metastatic versus primary tumors. Surg. Oncol. 2009, 18, 343–349. [Google Scholar] [CrossRef] [PubMed]
- Bernthal, N.M.; Schwartz, A.J.; Oakes, D.A.; Kabo, J.M.; Eckardt, J.J. How long do endoprosthetic reconstructions for proximal femoral tumors last? Clin. Orthop. Relat. Res. 2010, 468, 2867–2874. [Google Scholar] [CrossRef] [PubMed]
- Hettwer, W.H.; Horstmann, P.F.; Hovgaard, T.B.; Grum-Scwensen, T.A.; Petersen, M.M. Low Infection Rate after Tumor Hip Arthroplasty for Metastatic Bone Disease in a Cohort Treated with Extended Antibiotic Prophylaxis. Adv. Orthop. 2015, 2015, 428986. [Google Scholar] [CrossRef] [PubMed]
- Jeys, L.; Grimer, R.; Carter, S.; Tillman, R. Periprosthetic Infection in Patients Treated for an Orthopaedic Oncological Condition. J. Bone Jt. Surg. 2005, 87, 842–849. [Google Scholar] [CrossRef]
- Mahvi, D.A.; Liu, R.; Grinstaff, M.W.; Colson, Y.L.; Raut, C.P. Local Cancer Recurrence: The Realities, Challenges, and Opportunities for New Therapies. CA: A Cancer J. Clin. 2018, 68, 488–505. [Google Scholar] [CrossRef]
- Enneking, W.F.; Dunham, W.; Gebhardt, M.C.; Malawar, M.; Pritchard, D.J. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin. Orthop. Relat. Res. 1993, 286, 241–246. [Google Scholar] [CrossRef]
- Harris, W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J. Bone Jt. Surg. 1969, 51, 737–755. [Google Scholar] [CrossRef]
- Wamper, K.E.; Sierevelt, I.N.; Poolman, R.W.; Bhandari, M.; Haverkamp, D. The Harris hip score: Do ceiling effects limit its usefulness in orthopedics? Acta Orthop. 2010, 81, 703–707. [Google Scholar] [CrossRef]
- Nilsdotter, A.; Bremander, A. Measures of hip function and symptoms: Harris Hip Score (HHS), Hip Disability and Osteoarthritis Outcome Score (HOOS), Oxford Hip Score (OHS), Lequesne Index of Severity for Osteoarthritis of the Hip (LISOH), and American Academy of Orthopedic Surgeons (AAOS) Hip and Knee Questionnaire. Arthritis Care Res. 2011, 63 (Suppl. 11), S200–S207. [Google Scholar] [CrossRef]
- Uehara, K.; Ogura, K.; Akiyama, T.; Shinoda, Y.; Iwata, S.; Kobayashi, E.; Tanzawa, Y.; Yonemoto, T.; Kawano, H.; Kawai, A. Reliability and Validity of the Musculoskeletal Tumor Society Scoring System for the Upper Extremity in Japanese Patients. Clin. Orthop. Relat. Res. 2017, 475, 2253–2259. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Li, X.; Wang, Z.; Xiong, J.; Wang, S. Functional evaluation for patients with lower extremity sarcoma: Application of the Chinese version of Musculoskeletal Tumor Society scoring system. Health Qual. Life Outcomes 2017, 15, 107. [Google Scholar] [CrossRef] [PubMed]
| Studies | Study Period | Patient Number | HA | THA | Male/Female | Median Age | Study Design | Newcastle–Ottawa Quality Score | Country |
|---|---|---|---|---|---|---|---|---|---|
| Zucchini et al., 2021 [21] | NA | 104 | 90 | 14 | 51/53 | NA | Retrospective | 9 | Italy |
| Menendez et al., 2006 [2] | 1992–2003 | 96 | 62 | 34 | 45/51 | 59 | Retrospective | 8 | USA |
| Jamshidi et al., 2020 [22] | 1998–2016 | 57 | 29 | 28 | 26/31 | 33 | Retrospective | 9 | Iran |
| Ogilvie et al., 2004 [13] | 1992–2002 | 33 | 21 | 12 | 21/12 | 46.4 | Retrospective | 8 | Canada |
| Gusho et al., 2021 [23] | 2005–2019 | 38 | 33 | 5 | 15/23 | NA | Retrospective | 8 | USA |
| Zwart et al., 1994 [14] | 1984–1991 | 33 | 2 | 8 | 15/18 | 38 | Retrospective | 8 | The Netherlands |
| Reference | Dislocation HA, THA | Infection HA, THA | Local Recurrence HA, THA | HHS HA/THA | MSTS HA/THA |
|---|---|---|---|---|---|
| Zucchini et al., 2021 [21] | 2/90, 2/14 | 6/90, 1/14 | 4/90, 2/14 | NA | NA |
| Menendez et al., 2006 [2] | 4/62, 6/34 | NA | NA | NA | NA |
| Jamshidi et al., 2020 [22] | 3/29, 2/28 | 2/29, 3/28 | 1/29, 1/28 | 65/88 | 73/86 |
| Ogilvie et al., 2004 [13] | NA | NA | NA | NA | 67/68 |
| Gusho et al., 2021 [23] | 2/33, 1/5 | NA | NA | NA | NA |
| Zwart et al., 1994 [14] | NA | NA | NA | 69/87 | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Banskota, N.; Fang, X.; Yuan, D.; Lei, S.; Zhang, W.; Duan, H. Comparative Study of Proximal Femur Bone Tumor Patients Undergoing Hemiarthroplasty versus Total Hip Arthroplasty: A Meta-Analysis. J. Clin. Med. 2023, 12, 1209. https://doi.org/10.3390/jcm12031209
Banskota N, Fang X, Yuan D, Lei S, Zhang W, Duan H. Comparative Study of Proximal Femur Bone Tumor Patients Undergoing Hemiarthroplasty versus Total Hip Arthroplasty: A Meta-Analysis. Journal of Clinical Medicine. 2023; 12(3):1209. https://doi.org/10.3390/jcm12031209
Chicago/Turabian StyleBanskota, Nishant, Xiang Fang, Dechao Yuan, Senlin Lei, Wenli Zhang, and Hong Duan. 2023. "Comparative Study of Proximal Femur Bone Tumor Patients Undergoing Hemiarthroplasty versus Total Hip Arthroplasty: A Meta-Analysis" Journal of Clinical Medicine 12, no. 3: 1209. https://doi.org/10.3390/jcm12031209
APA StyleBanskota, N., Fang, X., Yuan, D., Lei, S., Zhang, W., & Duan, H. (2023). Comparative Study of Proximal Femur Bone Tumor Patients Undergoing Hemiarthroplasty versus Total Hip Arthroplasty: A Meta-Analysis. Journal of Clinical Medicine, 12(3), 1209. https://doi.org/10.3390/jcm12031209






