Impacts of COVID-19 Pandemic on Sleep Quality Evaluated by Wrist Actigraphy: A Systematic Review
Abstract
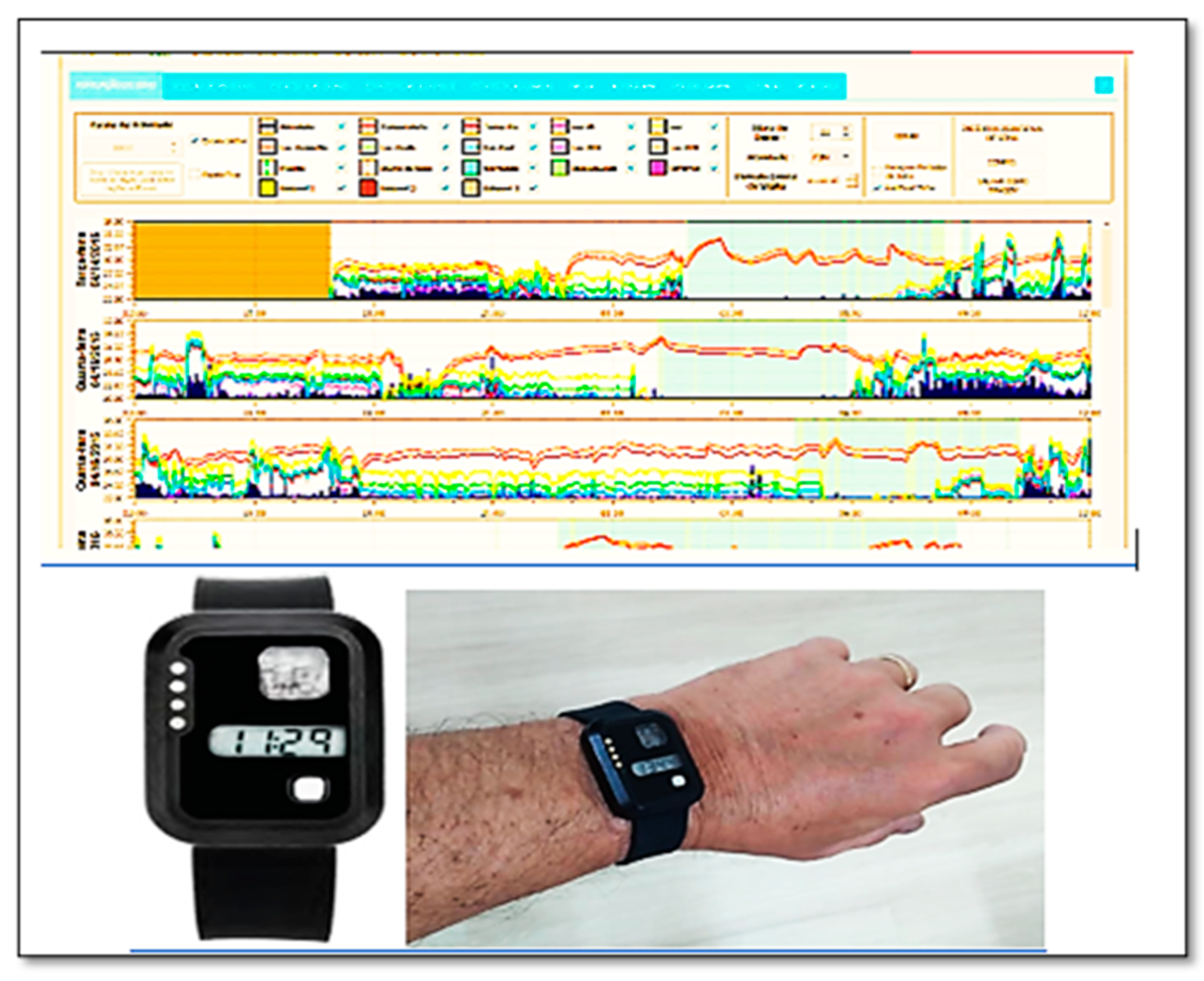
1. Introduction
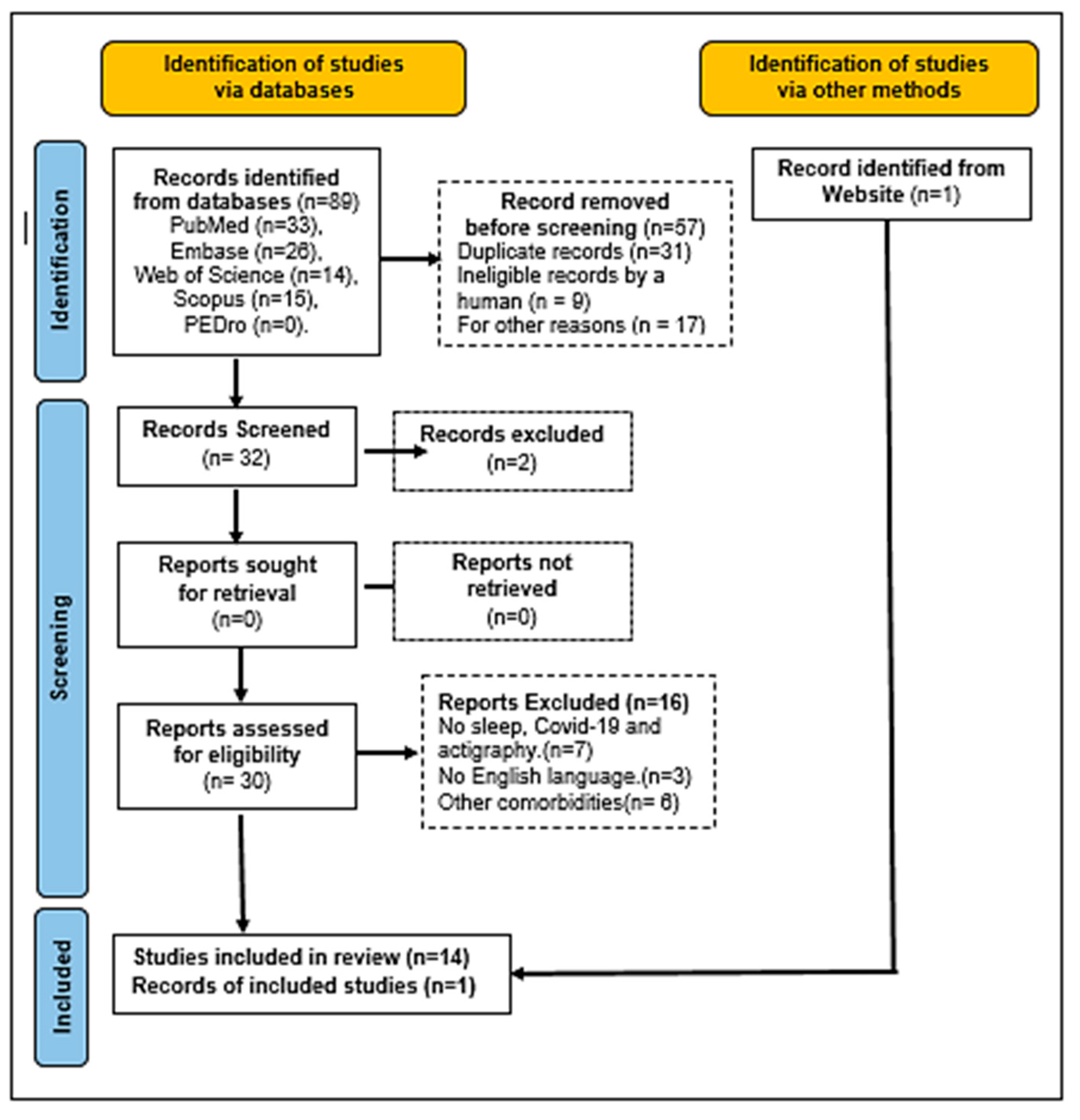
2. Materials and Methods
2.1. Research Question
2.2. Search Method
2.3. Registration
2.4. Operational Definition
2.5. Study Selection and Data Extraction
2.6. Eligibility Criteria
2.7. Level of Evidence
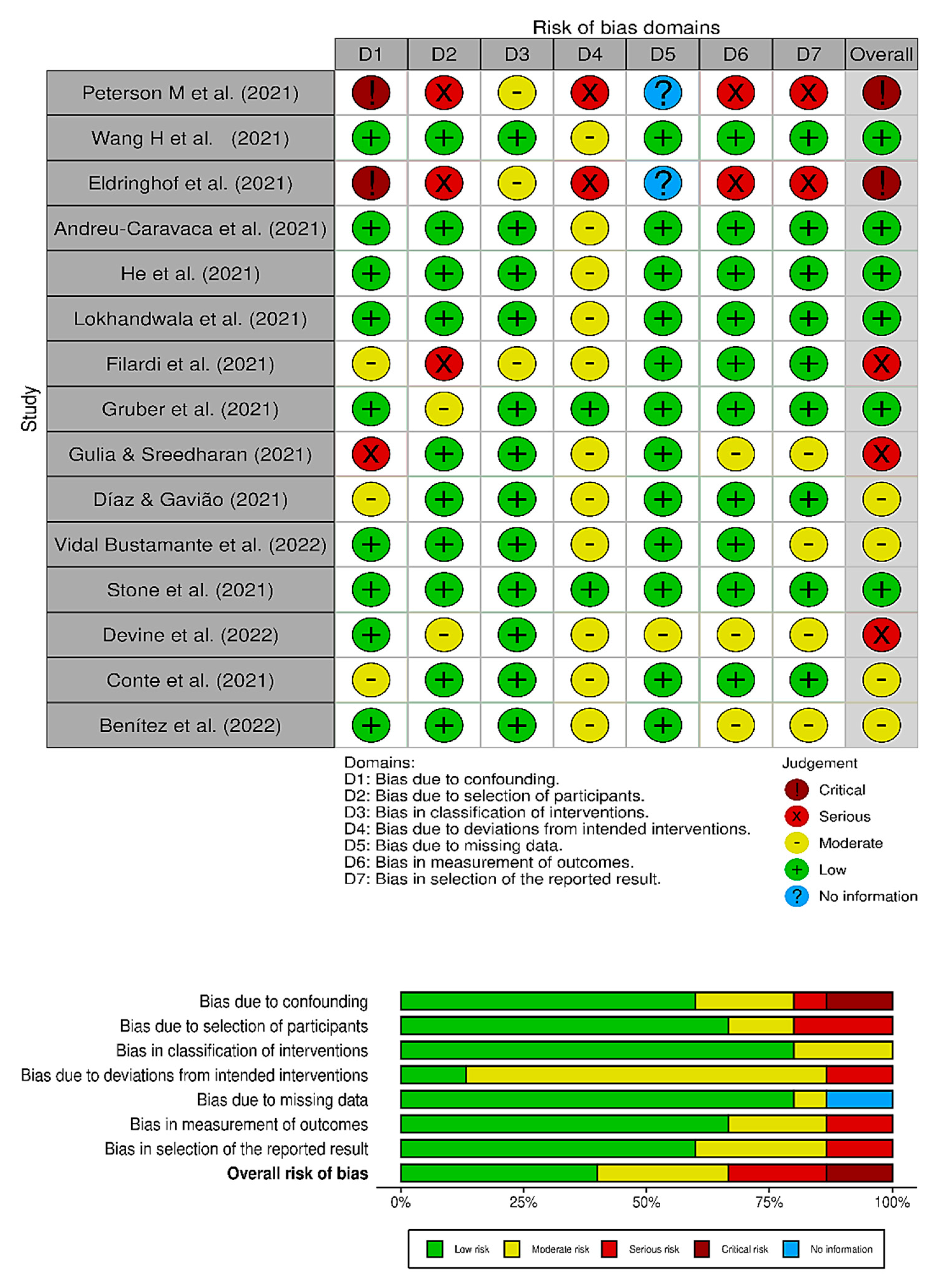
2.8. Risk of Bias
2.9. Effect Measures
2.10. Bibliographic Research
3. Results
4. Discussion
4.1. Future Directions
4.1.1. Strength of the Study
4.1.2. Limitations of the Study
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Ethical Considerations
References
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Bojdani, E.; Rajagopalan, A.; Chen, A.; Gearin, P.; Olcott, W.; Shankar, V.; Cloutier, A.; Solomon, H.; Naqvi, N.Z.; Batty, N.; et al. COVID-19 Pandemic: Impact on psychiatric care in the United States. Psychiatry Res. 2020, 289, 113069. [Google Scholar] [CrossRef]
- Thome, J.; Andrew, N.; Coogan, A.N.; Fischer, M.; Tucha, O.; Faltraco, F. Challenges for mental health services during the 2020 COVID-19 outbreak in Germany. Psychiatry Clin. Neurosci. 2020, 74, 407. [Google Scholar] [CrossRef]
- Wang, S.; Xie, L.; Xu, Y.; Yu, S.; Yao, B.; Xiang, D. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occup. Med. 2020, 70, 364–369. [Google Scholar] [CrossRef]
- Bao, Y.; Sun, Y.; Meng, S.; Shi, J.; Lu, L. 2019-nCoV epidemic: Address mental health care to empower society. Lancet 2020, 395, e37–e38. [Google Scholar] [CrossRef]
- Mak, I.W.C.; Chu, C.M.; Pan, P.C.; Yiu, M.G.C.; Ho, S.C.; Chan, V.L. Risk factors for chronic post-traumatic stress disorder (PTSD) in SARS survivors. Gen. Hosp. Psychiatry 2010, 32, 590–598. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Watson, N.F.; Badr, M.S.; Belenky, G.; Bliwise, D.L.; Buxton, O.; Buysse, D.; Dinges, D.F.; Gangwisch, J.; Grandner, M.A.; Kushida, C.; et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep 2015, 38, 843–844. [Google Scholar] [CrossRef]
- Kirwan, M.; Pickett, S.M.; Jarrett, N.L. Emotion regulation as a moderator between anxiety symptoms and insomnia symptom severity. Psychiatry Res. 2017, 254, 40–47. [Google Scholar] [CrossRef]
- Altena, E.; Baglioni, C.; Espie, C.A.; Ellis, J.; Gavriloff, D.; Holzinger, B.; Schlarb, A.; Frase, L.; Jernelöv, S.; Riemann, D. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: Practical recommendations from a task force of the European CBT-I Academy. J. Sleep Res. 2020, 29, e13052. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee on Sleep Medicine and Research. Sleep Disorders and Sleep Deprivation: An Unmet Public Health Problem; Altevogt, B.M., Colten, H.R., Eds.; National Academies Press (US): Washington, DC, USA, 2006. [Google Scholar] [CrossRef]
- Heyat, M.B.B.; Akhtar, F.; Khan, M.H.; Ullah, N.; Gul, I.; Khan, H.; Lai, D. Detection, Treatment Planning, and Genetic Predisposition of Bruxism: A Systematic Mapping Process and Network Visualization Technique. CNS Neurol Disord Drug Targets 2021, 20, 755–775. [Google Scholar] [CrossRef]
- Bin Heyat, M.B.; Akhtar, F.; Ansari, M.A.; Khan, A.; Alkahtani, F.; Khan, H.; Lai, D. Progress in Detection of Insomnia Sleep Disorder: A Comprehensive Review. Curr. Drug Targets 2021, 22, 672–684. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Ortiz, J.; Castro-Quintero, D.; Lerma-Córdoba, C.; Yela-Ceballos, F.; Escobar-Córdoba, F. Mental health consequences of the COVID-19 pandemic associated with social isolation. Colomb. J. Anesthesiol. 2020, 48, e930. [Google Scholar] [CrossRef]
- Yuan, S.; Liao, Z.; Huang, H.; Jiang, B.; Zhang, X.; Wang, Y.; Zhao, M. Comparison of the Indicators of Psychological Stress in the Population of Hubei Province and Non-Endemic Provinces in China During Two Weeks During the Coronavirus Disease 2019 (COVID-19) Outbreak in February 2020. Med. Sci. Monit. 2020, 26, e923767-1–e923767-10. [Google Scholar] [CrossRef]
- Tull, M.T.; Edmonds, K.A.; Scamaldo, K.M.; Richmond, J.R.; Rose, J.P.; Gratz, K.L. Psychological Outcomes Associated with Stay-at-Home Orders and the Perceived Impact of COVID-19 on Daily Life. Psychiatry Res. 2020, 289, 113098. [Google Scholar] [CrossRef]
- Escobar-Córdoba, F.; Ramírez-Ortiz, J.; Fontecha-Hernández, J. Effects of social isolation on sleep during the COVID-19 pandemic. Sleep Sci. 2021, 14, 86–93. [Google Scholar] [CrossRef]
- Gualano, M.R.; Lo Moro, G.; Voglino, G.; Bert, F.; Siliquini, R. Effects of COVID-19 Lockdown on Mental Health and Sleep Disturbances in Italy. Int. J. Environ. Res. Public Health 2020, 17, 4779. [Google Scholar] [CrossRef]
- Jahrami, H.; BaHammam, A.S.; Bragazzi, N.L.; Saif, M.Z.; Faris, M.; Vitiello, M.V. Sleep problems during the COVID-19 pandemic by population: A systematic review and meta-analysis. J. Clin. Sleep Med. 2021, 17, 299–313. [Google Scholar] [CrossRef]
- Ferini-Strambi, L.; Zucconi, M.; Casoni, F.; Salsone, M. COVID-19 and Sleep in Medical Staff: Reflections, Clinical Evidences, and Perspectives. Curr. Treat. Options Neurol. 2020, 22, 29. [Google Scholar] [CrossRef]
- Roenneberg, T.; Merrow, M. The Circadian Clock and Human Health. Curr. Biol. 2016, 26, R432–R443. [Google Scholar] [CrossRef]
- Grandin, L.D.; Alloy, L.B.; Abramson, L.Y. The social zeitgeber theory, circadian rhythms, and mood disorders: Review and evaluation. Clin. Psychol. Rev. 2006, 26, 679–694. [Google Scholar] [CrossRef]
- Rezaei, N.; Grandner, M.A. Changes in sleep duration, timing, and variability during the COVID-19 pandemic: Large-scale Fitbit data from 6 major US cities. Sleep Health 2021, 7, 303–313. [Google Scholar] [CrossRef]
- de Souza, L.F.F.; Paineiras-Domingos, L.L.; Melo-Oliveira, M.E.D.S.; Pessanha-Freitas, J.; Moreira-Marconi, E.; Lacerda, A.C.R.; Mendonça, V.A.; Sá-Caputo, D.d.C.; Bernardo-Filho, M. The impact of COVID-19 pandemic in the quality of sleep by Pittsburgh Sleep Quality Index: A systematic review. Cien. Saude Colet. 2021, 26, 1457–1466. [Google Scholar] [CrossRef]
- Alqahtani, S.S.; Banji, D.; Banji, O.J. A survey assessing sleep efficiency among Saudis during COVID-19 home confinement using the Pittsburgh sleep quality index: A call for health education. Saudi Pharm. J. 2021, 29, 692–698. [Google Scholar] [CrossRef]
- Romdhani, M.; Rae, D.E.; Nédélec, M.; Ammar, A.; Chtourou, H.; Al Horani, R.; Ben Saad, H.; Bragazzi, N.; Dönmez, G.; Driss, T.; et al. COVID-19 Lockdowns: A Worldwide Survey of Circadian Rhythms and Sleep Quality in 3911 Athletes from 49 Countries, with Data-Driven Recommendations. Sports Med. 2021, 52, 1433–1448. [Google Scholar] [CrossRef]
- Peterson, L.M.; Miller, K.G.; Wong, P.M.; Anderson, B.P.; Kamarck, T.W.; Matthews, K.A.; Kirschbaum, C.; Manuck, S.B. Sleep duration partially accounts for race differences in diurnal cortisol dynamics. Health Psychol. 2017, 36, 502–511. [Google Scholar] [CrossRef]
- Gargiulo, A.T.; Peterson, L.M.; Grafe, L.A. Stress, coping, resilience, and sleep during the COVID-19 pandemic: A representative survey study of US adults. Brain Behav. 2021, 11, e2384. [Google Scholar] [CrossRef]
- Vitale, J.A.; Perazzo, P.; Silingardi, M.; Biffi, M.; Banfi, G.; Negrini, F. Is disruption of sleep quality a consequence of severe Covid-19 infection? A case-series examination. Chronobiol. Int. 2020, 37, 1110–1114. [Google Scholar] [CrossRef]
- He, L.; Zhao, W.; Gao, Y.; Gao, X.; Lei, X. The effect of COVID-19 lockdowns on sleep time perception: Comparing actigraphy and sleep diary measures. Int. J. Psychophysiol. 2021, 167, 86–93. [Google Scholar] [CrossRef]
- Garcia, A.D.S.; Das Neves, J.D.; Vicentini, S.C.; Nogueira, G.D.A.; Marques, J.M.; Barreiros, R.N.; Marta, C.B.; Da Silva, R.C.L.; Silva, C. Actigraphy versus Polysomnography to Identify Changes in the Sleep Patterns of Adults with Insomnia. Rev. Neurocienc. 2020, 28, 1–25. [Google Scholar] [CrossRef]
- Driller, M.W.; O’Donnell, S.; Tavares, F. What wrist should you wear your actigraphy device on? Analysis of dominant vs. non-dominant wrist actigraphy for measuring sleep in healthy adults. Sleep Sci. 2017, 10, 132–135. [Google Scholar] [CrossRef]
- Smith, M.T.; McCrae, C.S.; Cheung, J.; Martin, J.L.; Harrod, C.G.; Heald, J.L.; Carden, K.A. Use of Actigraphy for the Evaluation of Sleep Disorders and Circadian Rhythm Sleep-Wake Disorders: An American Academy of Sleep Medicine Clinical Practice Guideline. J. Clin. Sleep Med. 2018, 14, 1231–1237. [Google Scholar] [CrossRef]
- Sadeh, A.; Hauri, P.J.; Kripke, D.F.; Lavie, P. The Role of Actigraphy in the Evaluation of Sleep Disorders. Sleep 1995, 18, 288–302. [Google Scholar] [CrossRef] [PubMed]
- McDevitt, B.; Moore, L.; Akhtar, N.; Connolly, J.; Doherty, R.; Scott, W. Validity of a Novel Research-Grade Physical Activity and Sleep Monitor for Continuous Remote Patient Monitoring. Sensors 2021, 21, 2034. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; He, L.; Gao, Y.; Gao, X.; Lei, X. Effects of physical activity and sleep quality on well-being: A wrist actigraphy study during the pandemic. Appl. Psychol. Health Well-Being 2021, 13, 394–405. [Google Scholar] [CrossRef]
- Krystal, A.D. Non-rem sleep EEG spectral analysis in insomnia. Psychiatr Ann. 2008, 38, 615–620. [Google Scholar] [CrossRef]
- Peterson, M.; Lundholm, K.; Skeiky, L.; Van Dongen, H.; Hansen, D. 727 Impact of Washington State COVID-19 Lockdown on Sleep. Sleep 2021, 44, A283–A284. [Google Scholar] [CrossRef]
- Krishnan, V.; Gupta, R.; Grover, S.; Basu, A.; Tripathi, A.; Subramanyam, A.; Nischal, A.; Hussain, A.; Mehra, A.; Ambekar, A.; et al. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J. Psychiatry 2020, 62, 370–378. [Google Scholar] [CrossRef]
- Li, Y.; Qin, Q.; Sun, Q.; Sanford, L.D.; Vgontzas, A.N.; Tang, X. Insomnia and psychological reactions during the COVID-19 outbreak in China. J. Clin. Sleep Med. 2020, 16, 1417–1418. [Google Scholar] [CrossRef]
- Bin Heyat, M.B.; Akhtar, F.; Sultana, A.; Tumrani, S.; Teelhawod, B.N.; Abbasi, R.; Amjad Kamal, M.; Muaad, A.Y.; Lai, D.; Wu, K. Role of Oxidative Stress and Inflammation in Insomnia Sleep Disorder and Cardiovascular Diseases: Herbal Antioxidants and Anti-inflammatory Coupled with Insomnia Detection Using Machine Learning. Curr. Pharm. Des. 2022, 28, 3618–3636. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Healthcare Interventions: Explanation and Elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed]
- PROSPERO-International Prospective Register of Systematic Reviews. 2020. Available online: https://www.crd.york.ac.uk/prospero (accessed on 23 January 2022).
- Golubnitschaja, O.; Flammer, J. Individualised patient profile: Clinical utility of Flammer syndrome phenotype and general lessons for predictive, preventive and personalised medicine. EPMA J. 2018, 9, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Lichstein, K.L.; Stone, K.C.; Donaldson, J.; Nau, S.D.; Soeffing, J.P.; Murray, D.; Lester, K.W.; Aguillard, R.N. Actigraphy Validation with Insomnia. Sleep 2006, 29, 232–239. [Google Scholar] [CrossRef]
- Mazza, S.; Bastuji, H.; Rey, A. Objective and Subjective Assessments of Sleep in Children: Comparison of Actigraphy, Sleep Diary Completed by Children and Parents’ Estimation. Front. Psychiatry 2020, 11, 495. [Google Scholar] [CrossRef] [PubMed]
- Cole, R.J.; Kripke, D.F.; Gruen, W.; Mullaney, D.J.; Gillin, J.C. Automatic Sleep/Wake Identification From Wrist Activity. Sleep 1992, 15, 461–469. [Google Scholar] [CrossRef]
- Acker, J.; Golubnitschaja, O.; Büttner-Teleaga, A.; Richter, K. Wrist actigraphic approach in primary, secondary and tertiary care based on the principles of predictive, preventive and personalised (3P) medicine. EPMA J. 2021, 12, 349–363. [Google Scholar] [CrossRef]
- Bellone, G.J.; Plano, S.A.; Cardinali, D.P.; Chada, D.P.; Vigo, D.E.; Golombek, D.A. Comparative analysis of actigraphy performance in healthy young subjects. Sleep Sci. 2016, 9, 272–279. [Google Scholar] [CrossRef]
- Merlin, T.; Weston, A.; Tooher, R. Extending an evidence hierarchy to include topics other than treatment: Revising the Australian ‘levels of evidence’. BMC Med. Res. Methodol. 2009, 9, 34. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- Cohen, J. A Coefficient of Agreement for Nominal Scales. Educ. Psychol. Meas. 1960, 20, 37–46. [Google Scholar] [CrossRef]
- Campbell, M.; McKenzie, J.E.; Sowden, A.; Katikireddi, S.V.; Brennan, S.E.; Ellis, S.; Hartmann-Boyce, J.; Ryan, R.; Shepperd, S.; Thomas, J.; et al. Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ 2020, 368, l6890. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Filardi, M.; D’Anselmo, A.; Mazzoni, A.; Moresco, M.; Pizza, F.; Plazzi, G. The importance of social zeitgeber in paediatric type 1 narcolepsy: What we can learn from the COVID-19 restrictions adopted in Italy? J. Sleep Res. 2021, 31, e13423. [Google Scholar] [CrossRef] [PubMed]
- Gulia, K.K.; Sreedharan, S.E. Yogic Sleep and Walking Protocol Induced Improvement in Sleep and Wellbeing in Post-menopausal Subject: A Longitudinal Case Study During COVID Lockdown. Sleep Vigil. 2021, 6, 229–233. [Google Scholar] [CrossRef]
- Díaz, D.Z.R.; Gavião, M.B.D. Sleep-wake circadian rhythm pattern in young adults by actigraphy during social isolation. Sleep Sci. 2022, 15, 172–183. [Google Scholar] [CrossRef] [PubMed]
- Bustamante, C.M.V.; Coombs, G.; Rahimi-Eichi, H.; Mair, P.; Onnela, J.-P.; Baker, J.T.; Buckner, R.L. Fluctuations in behavior and affect in college students measured using deep phenotyping. Sci. Rep. 2022, 12, 1932. [Google Scholar] [CrossRef] [PubMed]
- Devine, J.K.; Garcia, C.R.; Simoes, A.S.; Guelere, M.R.; de Godoy, B.; Silva, D.S.; Pacheco, P.C.; Choynowski, J.; Hursh, S.R. Predictive Biomathematical Modeling Compared to Objective Sleep during COVID-19 Humanitarian Flights. Aerosp. Med. Hum. Perform. 2022, 93, 4–12. [Google Scholar] [CrossRef]
- Benítez, I.D.M.; Moncusí-Moix, A.M.; Vaca, R.M.; Gort-Paniello, C.M.; Minguez, O.M.; Santisteve, S.M.; Carmona, P.M.; Torres, G.; Fagotti, J.; Labarca, G.; et al. Sleep and Circadian Health of Critical COVID-19 Survivors 3 Months After Hospital Discharge. Crit. Care Med. 2022, 50, 945–954. [Google Scholar] [CrossRef]
- Eldringhoff, H.; Mickelson, C.; Moore, L.; Pirner, M.; Doyle, S.; Mantua, J.; Mckeon, A. 690 An Analysis of Objective and Subjective Sleep and Infection Symptoms of Medical Personnel Working through the COVID-19 Pandemic. Sleep 2021, 44, A269–A270. [Google Scholar] [CrossRef]
- Andreu-Caravaca, L.; Ramos-Campo, D.; Manonelles, P.; Abellán-Aynés, O.; Chung, L.H.; Rubio-Arias, J. Effect of COVID-19 home confinement on sleep monitorization and cardiac autonomic function in people with multiple sclerosis: A prospective cohort study. Physiol. Behav. 2021, 237, 113392. [Google Scholar] [CrossRef]
- Lokhandwala, S.; Holmes, J.F.; Mason, G.M.; Laurent, C.W.S.; Delvey, C.; Hanron, O.; Andre, C.; Rodheim, K.; Kaur, S.; Spencer, R.M.C. Sleep and Coping in Early Childhood During the COVID-19 Pandemic. Front. Pediatr. 2021, 9, 716608. [Google Scholar] [CrossRef]
- Gruber, R.; Gauthier-Gagne, G.; Voutou, D.; Somerville, G.; Saha, S.; Boursier, J. Pre-pandemic sleep behavior and adolescents’ stress during Covid-19: A prospective longitudinal study. Child Adolesc. Psychiatry Ment. Health 2021, 15, 43. [Google Scholar] [CrossRef] [PubMed]
- Stone, J.E.; Phillips, A.J.K.; Chachos, E.; Hand, A.J.; Lu, S.; Carskadon, M.A.; Klerman, E.B.; Lockley, S.W.; Wiley, J.F.; Bei, B.; et al. In-person vs home schooling during the COVID-19 pandemic: Differences in sleep, circadian timing, and mood in early adolescence. J. Pineal Res. 2021, 71, e12757. [Google Scholar] [CrossRef]
- Conte, F.; De Rosa, O.; Rescott, M.L.; Arabia, T.P.; D’Onofrio, P.; Lustro, A.; Malloggi, S.; Molinaro, D.; Spagnoli, P.; Giganti, F.; et al. High sleep fragmentation parallels poor subjective sleep quality during the third wave of the Covid-19 pandemic: An actigraphic study. J. Sleep Res. 2021, 31, e13519. [Google Scholar] [CrossRef] [PubMed]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2021, 12, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Wu, K.K.; Chan, S.K.; Ma, T.M. Posttraumatic Stress after SARS. Emerg. Infect. Dis. 2005, 11, 1297–1300. [Google Scholar] [CrossRef]
- Lee, S.M.; Kang, W.S.; Cho, A.-R.; Kim, T.; Park, J.K. The psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatry 2018, 87, 123–127. [Google Scholar] [CrossRef]
- Zhou, H.; Lu, S.; Chen, J.; Wei, N.; Wang, D.; Lyu, H.; Shi, C.; Hu, S. The landscape of cognitive function in recovered COVID-19 patients. J. Psychiatr. Res. 2020, 129, 98–102. [Google Scholar] [CrossRef]
- Korman, M.; Tkachev, V.; Reis, C.; Komada, Y.; Kitamura, S.; Gubin, D.; Kumar, V.; Roenneberg, T. COVID-19-mandated social restrictions unveil the impact of social time pressure on sleep and body clock. Sci. Rep. 2020, 10, 22225. [Google Scholar] [CrossRef]
- Ferreira-Souza, L.F.; Coelho-Oliveira, A.C.; Julianelli-Peçanha, M.; de Souza Melo-Oliveira, M.E.; Moura-Fernandes, M.C.; Paineiras-Domingos, L.L.; da Cunha de Sá-Caputo, D.; Bernardo-Filho, M. Physical exercise as a potential strategy to mitigate the effects of Covid-19 in sleep quality: A systematic review. Prev. Med. Community Health 2021, 4, 15761. [Google Scholar] [CrossRef]
- Sonza, A.; da Cunha de Sá-Caputo, D.; Sartorio, A.; Tamini, S.; Seixas, A.; Sanudo, B.; Süßenbach, J.; Provenza, M.M.; Xavier, V.L.; Taiar, R.; et al. COVID-19 Lockdown and the Behavior Change on Physical Exercise, Pain and Psychological Well-Being: An International Multicentric Study. Int. J. Environ. Res. Public Health 2021, 18, 3810. [Google Scholar] [CrossRef] [PubMed]
- Pinto, J.; van Zeller, M.; Amorim, P.; Pimentel, A.; Dantas, P.; Eusébio, E.; Neves, A.; Pipa, J.; Clara, E.S.; Santiago, T.; et al. Sleep quality in times of Covid-19 pandemic. Sleep Med. 2020, 74, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Bailes, S.; Baltzan, M.; Rizzo, D.; Fichten, C.S.; Grad, R.; Wolkove, N.; Creti, L.; Amsel, R.; Libman, E. Sleep disorder symptoms are common and unspoken in Canadian general practice. Fam. Pract. 2009, 26, 294–300. [Google Scholar] [CrossRef] [PubMed]
- Casagrande, M.; Favieri, F.; Tambelli, R.; Forte, G. The enemy who sealed the world: Effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020, 75, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Cheng, Y.; Germain, A.; Moul, D.E.; Franzen, P.L.; Fletcher, M.; Monk, T.H. Night-to-night sleep variability in older adults with and without chronic insomnia. Sleep Med. 2010, 11, 56–64. [Google Scholar] [CrossRef]
- Neves, G.S.M.L.; Macedo, P.; Gomes, M.d.M. Sleep disorders: Up to date (1/2). Rev. Bras. Neurol. 2017, 53, 19–30. [Google Scholar] [CrossRef]
- Telles, S.C.L.; Corrêa, E.A.; Caversan, B.L.; Mattos, J.M.; Alves, R.S.C. The Actigraph Clinical Significance. Rev. Neurocienc. 2011, 19, 153–161. [Google Scholar] [CrossRef]
- Park, S.; Park, K.; Shim, J.-S.; Youm, Y.; Kim, J.; Lee, E.; Kim, H.C. Psychosocial factors affecting sleep misperception in middle-aged community-dwelling adults. PLoS ONE 2020, 15, e0241237. [Google Scholar] [CrossRef]
- Jackowska, M.; Dockray, S.; Hendrickx, H.; Steptoe, A. Psychosocial Factors and Sleep Efficiency: Discrepancies between subjective and objective evaluations of sleep. Psychosom. Med. 2011, 73, 810–816. [Google Scholar] [CrossRef]
- Sadeh, A.; Acebo, C. The role of actigraphy in sleep medicine. Sleep Med. Rev. 2002, 6, 113–124. [Google Scholar] [CrossRef]
- Kang, L.; Li, Y.; Hu, S.; Chen, M.; Yang, C.; Yang, B.X.; Wang, Y.; Hu, J.; Lai, J.; Ma, X.; et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry 2020, 7, e14. [Google Scholar] [CrossRef] [PubMed]
- Ancoli-Israel, S.; Cole, R.; Alessi, C.; Chambers, M.; Moorcroft, W.; Pollak, C.P. The Role of Actigraphy in the Study of Sleep and Circadian Rhythms. Sleep 2003, 26, 342–392. [Google Scholar] [CrossRef] [PubMed]
- Danzig, R.; Wang, M.; Shah, A.; Trotti, L.M. The wrist is not the brain: Estimation of sleep by clinical and consumer wearable actigraphy devices is impacted by multiple patient- and device-specific factors. J. Sleep Res. 2019, 29, e12926. [Google Scholar] [CrossRef] [PubMed]
- Salles, C.; Lopes, J.R.; Neves, M.; Brito, R.S.; Bacelar, A. Is there a link between COVID-19 and obstructive sleep apnea? Sleep Sci. 2021, 14, 299–302. [Google Scholar] [CrossRef] [PubMed]
- Wu, K.; Wei, X. Analysis of Psychological and Sleep Status and Exercise Rehabilitation of Front-Line Clinical Staff in the Fight against COVID-19 in China. Med Sci. Monit. Basic Res. 2020, 26, e924085. [Google Scholar] [CrossRef]
- Wang, X.; Lei, S.M.; Le, S.; Yang, Y.; Zhang, B.; Yao, W.; Gao, Z.; Cheng, S. Bidirectional Influence of the COVID-19 Pandemic Lockdowns on Health Behaviors and Quality of Life among Chinese Adults. Int. J. Environ. Res. Public Health 2020, 17, 5575. [Google Scholar] [CrossRef] [PubMed]
- Yin, Q.; Sun, Z.; Liu, T.; Ni, X.; Deng, X.; Jia, Y.; Shang, Z.; Zhou, Y.; Liu, W. Posttraumatic stress symptoms of health care workers during the corona virus disease 2019. Clin. Psychol. Psychother. 2020, 27, 384–395. [Google Scholar] [CrossRef]
- Pappa, S.; Ntella, V.; Giannakas, T.; Giannakoulis, V.G.; Papoutsi, E.; Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 2020, 88, 901–907. [Google Scholar] [CrossRef]
- Cellini, N.; Canale, N.; Mioni, G.; Costa, S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 2020, 29, e13074. [Google Scholar] [CrossRef]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954. [Google Scholar] [CrossRef]
- Liu, K.; Chen, Y.; Wu, D.; Lin, R.; Wang, Z.; Pan, L. Effects of progressive muscle relaxation on anxiety and sleep quality in patients with COVID-19. Complement. Ther. Clin. Pract. 2020, 39, 101132. [Google Scholar] [CrossRef] [PubMed]
- Vitale, J.A.; Roveda, E.; Montaruli, A.; Galasso, L.; Weydahl, A.; Caumo, A.; Carandente, F. Chronotype influences activity circadian rhythm and sleep: Differences in sleep quality between weekdays and weekend. Chronobiol. Int. 2014, 32, 405–415. [Google Scholar] [CrossRef] [PubMed]
| Author (Year) | Country | Population Size | Gender (Female/Male) | Age (Years or Mage ± SD) * or Median (25–75) ** | Specific Condition |
|---|---|---|---|---|---|
| Peterson et al. (2021) [38] | USA | 9 individuals in stay-at-home order | 5/4 | From 22 to 48 | in-home confinement |
| Wang et al. (2021) [36] | China | 70 individuals in stay-at-home-order | 46/24 | From 31 to 60 | in-home confinement |
| Eldringhof et al. (2021) [61] | USA | 50 medical personnel working through the pandemic | Not reported | 35.15 ± 9.97 | working in the pandemic. |
| Andreu-Caravaca et al. (2021) [62] | Spain | 17 individuals with multiple sclerosis | 10/7 | 43.50 ± 11.23 | in-home confinement |
| He et al. (2021) [30] | China | 70 participants into home stayers and area-restricted workers | 46/24 | From 31 to 65 | isolation at home or working during COVID-19 |
| Lokhandwala et al. (2021) [63] | USA | 16 preschool-aged children | 3/13 | 56.4 ± 10.8 months | in online learning remote programs or not |
| Filardi et al. (2021) [55] | Italy | 18 type 1 narcolepsy children and adolescents | 7/11 | 14.44 ± 2.01 | in-home confinement |
| Gruber et al. (2021) [64] | Canada | 62 adolescents | 44/18 | From 12 to 16 | in a domestic environment during COVID-19 |
| Gulia & Sreedharan (2021) [56] | India | 1 postmenopausal woman | 1/0 | 56 | during COVID lockdown period |
| Dias & Gavião, (2022) [57] | Brazil | 19 students | 10/9 | From 19 to 33 | during social isolation in COVID-19 pandemic |
| Vidal Bustamante et al. (2022) [58] | USA | 43 university students | 25/24 | From 18 to 19 | studying during the COVID-19 pandemic |
| Stone et al. (2021) [65] | Australia | 59 students | 33/26 | 12.8 ± 0.4 | during COVID-19 pandemic |
| Devine et al. (2022) [59] | Brazil | 20 pilots flying across five humanitarian missions | Not reported | Over 18 | in humanitarian missions during the COVID-19 pandemic in ULR |
| Conte et al. (2021) [66] | Italy | 82 patients | 40/42 | 32.5 ± 11.5 | during distinct phases of the COVID pandemic emergency |
| Benítez et al. (2022) [60] | Spain | 172 patients | 56/116 | 61 (52.8–67.0) | three months after hospital discharge during COVID-19 |
| Author | Wrist Actigraph | Sleep Monitoring Time | Aim | Result | Conclusion |
|---|---|---|---|---|---|
| Peterson et al. [38] | Actiwatch-2 (Philips Respironics) | Two weeks | Measure the sleep disturbances during stay-at-home orders | Delayed sleep onset by 53.4 ± 15.1 min (F[1,101] = 12.46, p < 0.001), delayed final awakening by 104.3 ± 19.6 min (F[1,101] = 28.43, p < 0.001), longer sleep duration (F[1,101] = 6.06, p = 0.016), increased number of awakenings (F[1,101] = 13.00, p < 0.001), trend for increased intermittent wakefulness (F[1,101] = 3.88, p = 0.052) post lockdown. | Evidence of increased sleep disruption. Observed later wake times and decreases in sleep quality. |
| Wang et al. [36] | wGT3X-BT | Five consecutive days and nights | assess effects of night-time sleep and daytime activity on well-being | Sleep onset time M (23:50) SD (1:25) range (22:29–5:21); wake-up time M (8:02) SD (1:26) range (4:52–12:39); sleep midpoint M (3:56) SD (1:19) range (1:11–9:00); TST M (8:13) SD (1:9) range (5:46–13:6). | Sleep, daytime activity levels, and light exposure were negatively affected by the COVID-19 pandemic. |
| Eldringhof et al. [61] | Actiwatch Philips. | Over six months | Understand the effects of sleep on the severity of COVID-19 symptoms in medical personnel | Poorer sleep quality t(255.59) = 5.78, p =< 0.001,poorer mood upon waking t(258.03) = 6.53, p =< 0.001, feeling less alert upon waking t(255.61) = 4.56, p =< 0.001, and spending more time awake at night t(266.98) = −7.29, p =< 0.001. | Medical personnel with symptoms of infection may have trouble sleeping properly. |
| Andreu-Caravaca et al. [62] | wGT3X-BT | Measured in two moments (pre- and post-home confinement of 5 days each) | Analyze the effect of home confinement on sleep quality in people with MS | Sleep quality decreased with significant and moderate effects on sleep efficiency (ES = 1.27, p = 0.01) and sleep time (ES = 0.81, p = 0.01), CI 95%. | Worsening of sleep quality variables was seen in people with MS. |
| He et al. [30] | wGT3X-BT | Five consecutive days, one participant for three days | Assess the impact of COVID-19 lockdown on sleep time perception | A significant difference in wake-up times [t(68) = 2.576, p = 0.012, d = 0.625] and sleep onset times [t(68) = 2.513, p = 0.014, d = 0.609], however not in TST. | Home isolation affected participants’ perception of sleep onset and wake-up time, but not their perceived total sleep time. |
| Lokhandwala et al. [63] | Actiwatch Spectrum Plus (Philips Respironics) | Sixteen consecutive days and nights | Investigate children’s previous sleep patterns with coping during COVID-19 | Longer sleep duration in remote students who slept 44 min more during the night [t(14) = 2.92, p = 0.01, d = 1.46]. | Remote students slept significantly more through the night than students not involved in home learning. |
| Filardi et al. [55] | Micro Motionlogger Watch, Ambulatory Monitoring | Fourteen consecutive days | Evaluate the effects of lockdown COVID-19 on nighttime sleep and daytime naps of NT1 children and adolescents | Lower levels of DMA (t(17) = 5.75, p< 0.0001), higher and DTST (t(17) = −2.59, p < 0.05) and increased frequency of naps (t(17) = −2.89, p = 0.01), while the mean nap duration was not changed (t(17) = −1.46, p = ns). | NT1 children and adolescents slept more during the daytime and napped more frequently during the lockdown. |
| Gruber et al. [64] | Actiwatch (AW-64 series; Mini-Mitter) | Seven consecutive nights | Compare the sleep patterns of adolescents and behaviors immediately before and during COVID-19 pandemic | Average bedtime was 1:28 h later, average wake-up time was 2:13 h later than their pre-pandemic schedules (F(1.61) = 68.55, p < 0.000, ηp2 = 0.53 and F(1.61) = 94.33, p < 0.000, ηp2 = 0.61, respectively. Daytime sleepiness was lower during the pandemic compared to pre-pandemic (F(1.61) = 13.17, p < 0.01, ηp2 = 0.18. Sleep quality did not change between the two time points. Sleep duration was 1:01 h longer during the pandemic compared to the pre-pandemic (F(1.47) = 14.68, p < 0.000, ηp2 = 0.19). | Sleep schedule was delayed and sleep duration was longer in the period of the COVID-19 pandemic compared to pre-pandemic sleep. |
| Gulia & Sreedharan. [56] | Somnowatch plus (Somnomedics) | Four weeks without intervention; twenty-four weeks with interventions (yoga-hydra and walking exercise) | Investigate yoga-hydra and walking intervention as a strategy to induce improved sleep and well-being in the elderly population during COVID lockdown | Pre-intervention values of 4 weeks sleep latency (score), as M ± SD (2.07 ± 0.55) and post-intervention of 24 weeks (1.24 ± 0.58), p < 0.001. TST pre-intervention ((h:min),as M ± SD (6.09 ± 1.38) and post-intervention of 24 weeks (6.53 ± 1.34), p < 0.05. | Regular practice of yoga-hydra with walking exercise improved the feeling of satisfying sleep and the sleep latency. |
| Dias & Gavião. [57] | ActTrust® (model AT0503 Condor Instruments) | 24 h period for seven consecutive days | Investigate nocturnal sleep parameters, estimate the activity-rest pattern, and determine the exposure to light with actigraphy. | Two clusters were formed: normal sleepers (n = 13) and short sleepers (n = 6). Circadian function index. Normal sleepers M ± SD (0.44 ± 0.08), short sleepers M ± SD (0.43 ± 0.08) p < 0.05. Sleep parameters M ± SD. Normal sleepers-bedtime (h:min)—(01:33 ± 10.560), Get up time (h:min)—(08:59 ± 1.88), TIB (h:min)—(8.19 ± 1.11), sleep period (h:min)—(7.18 ± 1.10), sleep efficiency (%)—(93.26 ± 4.80); short sleepers—bedtime (h:min)—(03:04 ± 7.03), get-up time (h:min)—(09:09 ± 2.09), TIB (h:min)—(6.46 ± 1.32), sleep period (h:min)—(5.40 ± 1.41), sleep efficiency (%)—(89.43 ± 7.22) p < 0.05. Normal sleepers had significant higher exposure to daylight (U = 37.00; p = 0.015) than short sleepers. | During social isolation presented inconsistent sleep parameters, irregular circadian rhythm and decreased exposure to daylight during the morning. |
| Vidal Bustamante et al. [58] | GENEActiv Original, Activinsights Ltd. | Three-month remote monitoring during the third year of college during the COVID-19 pandemic | Assess affective and behavioral experiences associated with mental health and sleep outcomes in students during the COVID-19 pandemic | Daily actigraphy per subject: range (132–249), M (220), med (227), SD (24.44); sleep duration (r): range (0.28–16.05), M (7.28), med (7.26), SD (0.54); sleep timing regularity index: range (0–1), M (0.75), Med (0.76), SD (0.05). | For most students, academic stress was common. Important psychological distress was emphasized for stressors involving social relationships. |
| Stone et al. [65] | GENEActiv (original, Activinsights) | For one to two weeks during in-person learning and during remote learning | Examine whether COVID-19 induced change in a school mode (in-person versus remote learning) was associated with changes in sleep, circadian timing, and mood in early adolescents. | During remote learning on average went to sleep 26 min later and woke 49 min later, compared to in-person school days. Sleep duration was longer in remote learning. In-person learning—sleep onset time (h:min), M ± SD (22:16 0:40), Wake time (h:min), M ± SD (7:12 0:34), sleep duration (h:min), M ± SD (8:55 0:35); remote learning—sleep onset time (h:min), M ± SD (22:44 1:03), wake time (h:min), M ± SD (7:55 0:41), sleep duration (h:min), M ± SD (9:10 0:45). | During remote learning in the face of lockdown, adolescents slept more, and less self-reported anxiety, slept longer/later, and were more in line with their circadian rhythms. |
| Devine et al. [59] | Zulu watch, (Institutes for Behavior Resources) | Five round-trip flights from humanitarian missions (Brazil/China/Brazil), with a duration of 30 flight hours each | Evaluate the ability of the SAFTE-FAST 4.0 AutoSleep function to predict pilot sleep duration throughout the missions compared to subjective (sleep diary) and objective (Zulu watch) measures of sleep during the airline’s COVID-19 humanitarian missions | Comparison of average in-flight sleep duration by flight segment: AutoSleep predicted 235 ± 20 min, compared to the 325 ± 128 min reported by the sleep diary, or the 246 ± 132 min recorded by Zulu watches. Paired samples t-tests showed that diary reports were higher than AutoSleep predictions (t = 6.05, df = 151, p ≤ 0.001) or Zulu watch sleep duration (t = 3.73, df = 150, p ≤ 0.001). AutoSleep predictions of sleep duration were not significantly different from Zulu watch sleep duration during FDPs (t = 0.69, df = 151, p = 0.48). | It is important to get adequate rest not only during periods of active duty but also during downtime. Giving up sleep during layovers may pose a risk of fatigue during ULR. however, the time zone difference must be considered. |
| Conte et al. [66] | Motionlogger® Microwatches | Two nights of recording during weekdays | Compare findings in the third wave with data collected during previous pandemic waves | No significant differences were found in any actigraphy sleep parameter between the 2 nights of recording bedtime (h:min), M ± SD (00:33 ± 1), wake time (h:min), M ± SD 08:33 ± 1:22), sleep midpoint (h:min), M ± SD (04:36 ± 1:21), frequency of awakenings ≥ 1 min/TST(h), M ±SD (1.78 ± 0.94). TIB and WASO (%) are M ± SD (8.09 ± 1.10 h) and (6.71% ± 5.82%), respectively. | Unfavorable effects on sleep verified by the initial pandemic outbreak have not decreased throughout the subsequent waves of contagion. |
| Benítez et al. [60] | Actiwatch 2 (Philips Respironics) | Seven days | To assess the sleep and circadian rest-activity pattern of critical survivors of COVID-19 three months after discharge from the hospital | Objective evaluation of sleep (actigraphy), TST (h), med (25~75) 6.98 (6.33–7.67), TIB (h), 8.38 (7.73–9.10), sleep efficiency (%), 84.6 (81.0–88.3), latency (min), 10.0 (5.00–18.0), WASO (min), 51.0 (39.0–66.0). | Critical survivors of COVID-19 may present bad sleep quality and modifications in the circadian rest–activity pattern three months after discharge from the hospital. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferreira-Souza, L.F.; Julianelli-Peçanha, M.; Coelho-Oliveira, A.C.; da Silva Bahia, C.M.C.; Paineiras-Domingos, L.L.; Reis-Silva, A.; Moura-Fernandes, M.C.; Trindade-Gusmão, L.C.; Taiar, R.; da Cunha Sá-Caputo, D.; et al. Impacts of COVID-19 Pandemic on Sleep Quality Evaluated by Wrist Actigraphy: A Systematic Review. J. Clin. Med. 2023, 12, 1182. https://doi.org/10.3390/jcm12031182
Ferreira-Souza LF, Julianelli-Peçanha M, Coelho-Oliveira AC, da Silva Bahia CMC, Paineiras-Domingos LL, Reis-Silva A, Moura-Fernandes MC, Trindade-Gusmão LC, Taiar R, da Cunha Sá-Caputo D, et al. Impacts of COVID-19 Pandemic on Sleep Quality Evaluated by Wrist Actigraphy: A Systematic Review. Journal of Clinical Medicine. 2023; 12(3):1182. https://doi.org/10.3390/jcm12031182
Chicago/Turabian StyleFerreira-Souza, Luiz Felipe, Marize Julianelli-Peçanha, Ana Carolina Coelho-Oliveira, Christianne Martins Corrêa da Silva Bahia, Laisa Liane Paineiras-Domingos, Aline Reis-Silva, Márcia Cristina Moura-Fernandes, Luiza Carla Trindade-Gusmão, Redha Taiar, Danubia da Cunha Sá-Caputo, and et al. 2023. "Impacts of COVID-19 Pandemic on Sleep Quality Evaluated by Wrist Actigraphy: A Systematic Review" Journal of Clinical Medicine 12, no. 3: 1182. https://doi.org/10.3390/jcm12031182
APA StyleFerreira-Souza, L. F., Julianelli-Peçanha, M., Coelho-Oliveira, A. C., da Silva Bahia, C. M. C., Paineiras-Domingos, L. L., Reis-Silva, A., Moura-Fernandes, M. C., Trindade-Gusmão, L. C., Taiar, R., da Cunha Sá-Caputo, D., Rapin, A., & Bernardo-Filho, M. (2023). Impacts of COVID-19 Pandemic on Sleep Quality Evaluated by Wrist Actigraphy: A Systematic Review. Journal of Clinical Medicine, 12(3), 1182. https://doi.org/10.3390/jcm12031182












