The Correlation between the Results of the Sniffin’ Sticks Test, Demographic Data, and Questionnaire of Olfactory Disorders in a Hungarian Population after a SARS-CoV-2 Infection
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Examinations
2.3. Patient-Reported Outcome Measures
2.4. Statistical Analysis
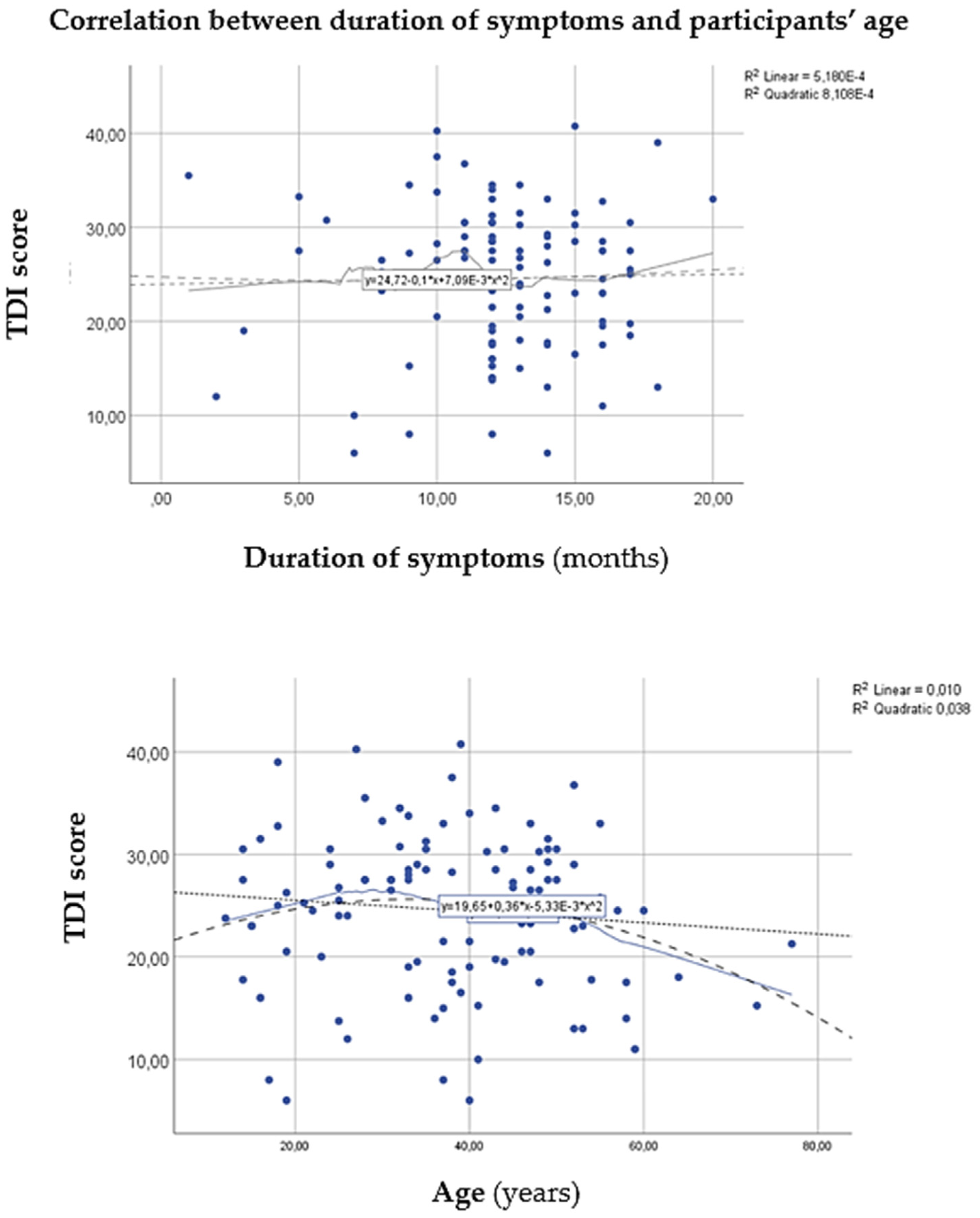
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gao, Y.-D.; Ding, M.; Dong, X.; Zhang, J.-J.; Azkur, A.K.; Azkur, D.; Gan, H.; Sun, Y.-L.; Fu, W.; Li, W.; et al. Risk factors for severe and critically ill COVID-19 patients: A review. Allergy 2021, 76, 428–455. [Google Scholar] [CrossRef]
- Chams, N.; Chams, S.; Badran, R.; Shams, A.; Araji, A.; Raad, M.; Mukhopadhyay, S.; Stroberg, E.; Duval, E.J.; Barton, L.M.; et al. COVID-19: A Multidisciplinary Review. Front. Public Health 2020, 8, 383. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Chiesa-Estomba, C.M.; De Siati, D.R.; Horoi, M.; Le Bon, S.D.; Rodriguez, A.; Dequanter, D.; Blecic, S.; El Afia, F.; Distinguin, L.; et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): A multicenter European study. Eur. Arch. Oto-Rhino-Laryngol. 2020, 277, 2251–2261. [Google Scholar] [CrossRef]
- Beltrán-Corbellini, Á.; Chico-García, J.L.; Martínez-Poles, J.; Rodríguez-Jorge, F.; Natera-Villalba, E.; Gómez-Corral, J.; Gómez-López, A.; Monreal, E.; Parra-Díaz, P.; Cortés-Cuevas, J.L.; et al. Acute-onset smell and taste disorders in the context of COVID-19: A pilot multicentre polymerase chain reaction based case–control study. Eur. J. Neurol. 2020, 27, 1738–1741. [Google Scholar] [CrossRef] [PubMed]
- Las Casas Lima, M.H.; Cavalcante, A.L.B.; Leão, S.C. Pathophysiological relationship between COVID-19 and olfactory dysfunction: A systematic review. Braz. J. Otorhinolaryngol. 2021, 88, 794–802. [Google Scholar] [CrossRef] [PubMed]
- Ammar, A.; Distinguin, L.; Chetrit, A.; Safa, D.; Hans, S.; Carlier, R.; Lechien, J.R.; Edjlali, M. Transient modifications of the olfactory bulb on MR follow-up of COVID-19 patients with related olfactory dysfunction. J. Neuroradiol. 2022, 49, 329–332. [Google Scholar] [CrossRef] [PubMed]
- Hannum, M.E.; Ramirez, V.A.; Lipson, S.J.; Herriman, R.D.; Toskala, A.K.; Lin, C.; Joseph, P.V.; Reed, D.R. Objective Sensory Testing Methods Reveal a Higher Prevalence of Olfactory Loss in COVID-19-Positive Patients Compared to Subjective Methods: A Systematic Review and Meta-Analysis. Chem. Senses 2020, 45, 865–874. [Google Scholar] [CrossRef]
- von Bartheld, C.S.; Hagen, M.M.; Butowt, R. Prevalence of Chemosensory Dysfunction in COVID-19 Patients: A Systematic Review and Meta-analysis Reveals Significant Ethnic Differences. ACS Chem. Neurosci. 2020, 11, 2944–2961. [Google Scholar] [CrossRef]
- von Bartheld, C.S.; Hagen, M.M.; Butowt, R. The D614G Virus Mutation Enhances Anosmia in COVID-19 Patients: Evidence from a Systematic Review and Meta-analysis of Studies from South Asia. ACS Chem. Neurosci. 2021, 12, 3535–3549. [Google Scholar] [CrossRef]
- Shelton, J.F.; Shastri, A.J.; Fletez-Brant, K.; 23andMe COVID-19 Team; Aslibekyan, S.; Auton, A. The UGT2A1/UGT2A2 locus is associated with COVID-19-related loss of smell or taste. Nat. Genet. 2022, 54, 121–124. [Google Scholar] [CrossRef]
- Tan, B.K.J.; Han, R.; Zhao, J.J.; Tan, N.K.W.; Quah, E.S.H.; Tan, C.J.; Chan, Y.H.; Teo, N.W.Y.; Charn, T.C.; See, A.; et al. Prognosis and persistence of smell and taste dysfunction in patients with COVID-19: Meta-analysis with parametric cure modelling of recovery curves. BMJ 2022, 378, e069503. [Google Scholar] [CrossRef] [PubMed]
- Tan, H.Q.M.; Pendolino, A.L.; Andrews, P.J.; Choi, D. Prevalence of olfactory dysfunction and quality of life in hospitalised patients 1 year after SARS-CoV-2 infection: A cohort study. BMJ Open 2022, 12, e054598. [Google Scholar] [CrossRef] [PubMed]
- Frasnelli, J.; Hummel, T. Olfactory dysfunction and daily life. Eur. Arch. Otorhinolaryngol. 2005, 262, 231–235. [Google Scholar] [CrossRef]
- Desiato, V.M.; Levy, D.A.; Byun, Y.J.; Nguyen, S.A.; Soler, Z.M.; Schlosser, R.J. The Prevalence of Olfactory Dysfunction in the General Population: A Systematic Review and Meta-analysis. Am. J. Rhinol. Allergy 2020, 35, 195–205. [Google Scholar] [CrossRef] [PubMed]
- Boscutti, A.; Delvecchio, G.; Pigoni, A.; Cereda, G.; Ciappolino, V.; Bellani, M.; Fusar-Poli, P.; Brambilla, P. Olfactory and gustatory dysfunctions in SARS-CoV-2 infection: A systematic review. Brain Brain Behav. Immun.-Heal. 2021, 15, 100268. [Google Scholar] [CrossRef] [PubMed]
- Hummel, T.; Sekinger, B.; Wolf, S.R.; Pauli, E.; Kobal, G. ‘Sniffin’ sticks’: Olfactory performance assessed by the combined testing of odor identification, odor discrimination and olfactory threshold. Chem. Senses 1997, 22, 39–52. [Google Scholar] [CrossRef]
- Langstaff, L.; Pradhan, N.; Clark, A.; Boak, D.; Salam, M.; Hummel, T.; Philpott, C.M. Validation of the olfactory disorders questionnaire for English-speaking patients with olfactory disorders. Clin. Otolaryngol. 2019, 44, 715–728. [Google Scholar] [CrossRef]
- Romero-Gameros, C.A.; Waizel-Haiat, S.; Mendoza-Zubieta, V.; Anaya-Dyck, A.; López-Moreno, M.A.; Colin-Martinez, T.; Martínez-Ordaz, J.L.; Ferat-Osorio, E.; Vivar-Acevedo, E.; Vargas-Ortega, G.; et al. Evaluation of predictive value of olfactory dysfunction, as a screening tool for COVID-19. Laryngoscope Investig. Otolaryngol. 2020, 5, 983–991. [Google Scholar] [CrossRef]
- Lima, M.A.; Silva, M.T.T.; Oliveira, R.V.; Soares, C.N.; Takano, C.L.; Azevedo, A.E.; Moraes, R.L.; Rezende, R.B.; Chagas, I.T.; Espíndola, O.; et al. Smell dysfunction in COVID-19 patients: More than a yes-no question. J. Neurol. Sci. 2020, 418, 117107. [Google Scholar] [CrossRef]
- Lechien, J.R.; Cabaraux, P.; Chiesa-Estomba, C.M.; Khalife, M.; Plzak, J.; Hans, S.; Martiny, D.; Calvo-Henriquez, C.; Barillari, M.R.; Hopkins, C.; et al. Psychophysical Olfactory Tests and Detection of COVID-19 in Patients with Sudden Onset Olfactory Dysfunction: A Prospective Study. Ear Nose Throat J. 2020, 99, 579–583. [Google Scholar] [CrossRef]
- Le Bon, S.D.; Pisarski, N.; Verbeke, J.; Prunier, L.; Cavelier, G.; Thill, M.P.; Rodriguez, A.; Dequanter, D.; Lechien, J.R.; Le Bon, O.; et al. Psychophysical evaluation of chemosensory functions 5 weeks after olfactory loss due to COVID-19: A prospective cohort study on 72 patients. Eur. Arch. Otorhinolaryngol. 2021, 278, 101–108. [Google Scholar] [CrossRef] [PubMed]
- Agyeman, A.A.; Chin, K.L.; Landersdorfer, C.B.; Liew, D.; Ofori-Asenso, R. Smell and Taste Dysfunction in Patients With COVID-19: A Systematic Review and Meta-analysis. Mayo Clin. Proc. 2020, 95, 1621–1631. [Google Scholar] [CrossRef] [PubMed]
- Pirker-Kees, A.; Platho-Elwischger, K.; Hafner, S.; Redlich, K.; Baumgartner, C. Hyposmia Is Associated with Reduced Cognitive Function in COVID-19: First Preliminary Results. Dement. Geriatr. Cogn. Disord. 2021, 50, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Sedaghat, A.R.; Gengler, I.; Speth, M.M. Olfactory Dysfunction: A Highly Prevalent Symptom of COVID-19 With Public Health Significance. Otolaryngol. Head Neck Surg. 2020, 163, 12–15. [Google Scholar] [CrossRef]
- Salepci, E.; Turk, B.; Ozcan, S.N.; Bektas, M.E.; Aybal, A.; Dokmetas, I.; Turgut, S. Symptomatology of COVID-19 from the otorhinolaryngology perspective: A survey of 223 SARS-CoV-2 RNA-positive patients. Eur. Arch. Otorhinolaryngol. 2021, 278, 525–535. [Google Scholar] [CrossRef]
- Altin, F.; Cingi, C.; Uzun, T.; Bal, C. Olfactory and gustatory abnormalities in COVID-19 cases. Eur. Arch. Otorhinolaryngol. 2020, 277, 2775–2781. [Google Scholar] [CrossRef]
- Rojas-Lechuga, M.J.; Izquierdo-Domínguez, A.; Chiesa-Estomba, C.; Calvo-Henríquez, C.; Villarreal, I.M.; Cuesta-Chasco, G.; Bernal-Sprekelsen, M.; Mullol, J.; Alobid, I. Chemosensory dysfunction in COVID-19 out-patients. Eur. Arch. Otorhinolaryngol. 2021, 278, 695–702. [Google Scholar] [CrossRef]
- Trecca, E.M.C.; Cassano, M.; Longo, F.; Petrone, P.; Miani, C.; Hummel, T.; Gelardi, M. Results from psychophysical tests of smell and taste during the course of SARS-CoV-2 infection: A review. Acta Otorhinolaryngol. Ital. 2022, 42, S20–S35. [Google Scholar] [CrossRef]
- Boscolo-Rizzo, P.; Fabbris, C.; Polesel, J.; Emanuelli, E.; Tirelli, G.; Spinato, G.; Hopkins, C. Two-Year Prevalence and Recovery Rate of Altered Sense of Smell or Taste in Patients with Mildly Symptomatic COVID-19. JAMA Otolaryngol. Head Neck Surg. 2022, 148, 889–891. [Google Scholar] [CrossRef]
- Liu, D.T.; Prem, B.; Sharma, G.; Kaiser, J.; Besser, G.; Mueller, C.A. Depression Symptoms and Olfactory-related Quality of Life. Laryngoscope 2022, 132, 1829–1834. [Google Scholar] [CrossRef]
- Prem, B.; Liu, D.T.; Besser, G.; Sharma, G.; Dultinger, L.E.; Hofer, S.V.; Matiasczyk, M.M.; Renner, B.; Mueller, C.A. Long-lasting olfactory dysfunction in COVID-19 patients. Eur. Arch. Otorhinolaryngol. 2021, 279, 3485–3492. [Google Scholar] [CrossRef] [PubMed]
- Moein, S.T.; Hashemian, S.M.; Mansourafshar, B.; Khorram-Tousi, A.; Tabarsi, P.; Doty, R.L. Smell dysfunction: A biomarker for COVID-19. Int. Forum Allergy Rhinol. 2020, 10, 944–950. [Google Scholar] [CrossRef] [PubMed]
- Hornuss, D.; Lange, B.; Schröter, N.; Rieg, S.; Kern, W.V.; Wagner, D. Anosmia in COVID-19 patients. Clin. Microbiol. Infect. 2020, 26, 1426–1427. [Google Scholar] [CrossRef] [PubMed]
- Raad, N.; Ghorbani, J.; Safavi Naeini, A.; Tajik, N.; Karimi-Galougahi, M. Parosmia in patients with COVID-19 and olfactory dysfunction. Int. Forum Allergy Rhinol. 2021, 11, 1497–1500. [Google Scholar] [CrossRef] [PubMed]
- Lerner, D.K.; Garvey, K.L.; Arrighi-Allisan, A.E.; Filimonov, A.; Filip, P.; Shah, J.; Tweel, B.; Del Signore, A.; Schaberg, M.; Colley, P.; et al. Clinical Features of Parosmia Associated With COVID-19 Infection. Laryngoscope 2022, 132, 633–639. [Google Scholar] [CrossRef]
- Kopishinskaia, S.; Lapshova, D.; Sherman, M.; Velichko, I.; Voznesensky, N.; Voznesenskaia, V. Clinical Features in Russian Patients with COVID-Associated Parosmia/Phanthosmia. Psychiatr. Danub. 2021, 33, 130–136. [Google Scholar]
- Coelho, D.H.; Reiter, E.R.; Budd, S.G.; Shin, Y.; Kons, Z.A.; Costanzo, R.M. Quality of life and safety impact of COVID-19 associated smell and taste disturbances. Am. J. Otolaryngol. 2021, 42, 103001. [Google Scholar] [CrossRef]
- Elkholi, S.M.A.; Abdelwahab, M.K.; Abdelhafeez, M. Impact of the smell loss on the quality of life and adopted coping strategies in COVID-19 patients. Eur. Arch. Otorhinolaryngol. 2021, 278, 3307–3314. [Google Scholar] [CrossRef]
- Saniasiaya, J.; Prepageran, N. Impact of olfactory dysfunction on quality of life in coronavirus disease 2019 patients: A systematic review. J. Laryngol. Otol. 2021, 135, 947–952. [Google Scholar] [CrossRef]
- Kim, J.W.; Kim, H.S.; Kim, M.; Kim, S.H.; Cho, S.W.; Kim, J.Y. Validation of Olfactory Questionnaire in Koreans: An Alternative for Conventional Psychophysical Olfactory Tests. J. Korean Med Sci. 2021, 36, e34. [Google Scholar] [CrossRef]
- Yang, D.; Wang, J.; Ni, D.; Liu, J.; Wang, X. Reliability and validity of the Chinese version of the questionnaire of olfactory disorders (QOD) when used with patients having olfactory dysfunction. Eur. Arch. Otorhinolaryngol. 2016, 273, 3255–3261. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.M.; Larsen, K.D.; Homøe, A.S.; Simonsen, A.L.; Arndal, E.; Koch, A.; Samuelsen, G.B.; Nielsen, X.C.; Todsen, T.; Homøe, P. Subjective and psychophysical olfactory and gustatory dysfunction among COVID-19 outpatients; short- and long-term results. PLoS ONE 2022, 17, e0275518. [Google Scholar] [CrossRef] [PubMed]
- Kaya, A.; Altıparmak, S.; Yaşar, M.; Özcan, İ.; Çelik, İ. Objective Evaluation of Smell and Taste Senses in COVID-19 Patients. Turk. Arch. Otolaryngol. 2022, 60, 128–133. [Google Scholar] [CrossRef]
- Gözen, E.D.; Aliyeva, C.; Tevetoğlu, F.; Karaali, R.; Balkan, İ.İ.; Yener, H.M.; Özdoğan, H.A. Evaluation of Olfactory Function with Objective Tests in COVID-19-Positive Patients: A Cross-Sectional Study. Ear Nose Throat J. 2021, 100, 169S–173S. [Google Scholar] [CrossRef]
- Hintschich, C.A.; Wenzel, J.J.; Hummel, T.; Hankir, M.K.; Kühnel, T.; Vielsmeier, V.; Bohr, C. Psychophysical tests reveal impaired olfaction but preserved gustation in COVID-19 patients. Int. Forum Allergy Rhinol. 2020, 10, 1105–1107. [Google Scholar] [CrossRef] [PubMed]
- Lechien, J.R.; Cabaraux, P.; Chiesa-Estomba, C.M.; Khalife, M.; Hans, S.; Calvo-Henriquez, C.; Martiny, D.; Journe, F.; Sowerby, L.; Saussez, S. Objective olfactory evaluation of self-reported loss of smell in a case series of 86 COVID-19 patients. Head Neck 2020, 42, 1583–1590. [Google Scholar] [CrossRef] [PubMed]
- Villerabel, C.; Makinson, A.; Jaussent, A.; Picot, M.-C.; Nègre-Pagès, L.; Rouvière, J.-A.; Favier, V.; Crampette, L.; Morquin, D.; Reynes, J.; et al. Diagnostic Value of Patient-Reported and Clinically Tested Olfactory Dysfunction in a Population Screened for COVID-19. JAMA Otolaryngol. Neck Surg. 2021, 147, 271–279. [Google Scholar] [CrossRef]
- Landis, B.N.; Hummel, T.; Hugentobler, M.; Giger, R.; Lacroix, J.S. Ratings of overall olfactory function. Chem. Senses 2003, 28, 691–694. [Google Scholar] [CrossRef]
- Ferdenz, C.; Bousquet, C.; Aguera, P.E.; Dantec, M.; Daudé, C.; Fornoni, L.; Fournel, A.; Kassan, A.; Mantel, M.; Moranges, M.; et al. Recovery From COVID-19-Related Olfactory Disorders and Quality of Life: Insights from an Observational Online Study. Chem. Senses 2021, 46, bjab028. [Google Scholar] [CrossRef]
- Fasunla, A.J.; Thairu, Y.; Salami, H.; Ibekwe, T.S. Self-Reported Olfactory, Gustatory and Otologic Dysfunctions among COVID-19 Positive Adults in Nigeria—A Preliminary Report. Ann. Ib. Postgrad. Med. 2021, 19, S15–S21. [Google Scholar]
- Hopkins, C.; Surda, P.; Whitehead, E.; Kumar, B.N. Early recovery following new onset anosmia during the COVID-19 pandemic—An observational cohort study. J. Otolaryngol.-Head Neck Surg. 2020, 49, 26. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.-H.; Yeoh, Z.X.; Sachlin, I.S.; Gazali, N.; Soelar, S.A.; Foo, C.Y.; Low, L.L.; Alwi, S.B.S.; Kamalden, T.M.I.T.; Shanmuganathan, J.; et al. Self-reported symptom study of COVID-19 chemosensory dysfunction in Malaysia. Sci. Rep. 2022, 12, 2111. [Google Scholar] [CrossRef] [PubMed]


| Category | Values |
|---|---|
| Age (mean ± SD years) | 37.5 ± 11 |
| Gender (men/women) | 35/75 |
| Duration since first appearance of symptoms (mean ± SD months) | 12.35 ± 2.41 |
| Subjective complaint report | |
| Anosmia, n (%) | 33 (30%) |
| Hyposmia, n (%) | 77 (70%) |
| Parosmia, n (%) | 61 (56.4%) |
| TDI results | |
| Normosmia, n (%) | 17 (15.5%) |
| Hyposmia, n (%) | 78 (71%) |
| Anosmia, n (%) | 15 (13.5%) |
| Anosmia (Chemosensory Testing) | Hyposmia (Chemosensory Testing) | |
| Anosmia (subjective category) | 10 | 17 |
| Hyposmia (subjective category) | 4 | 48 |
| p = 0.001 * |
| Spearman’s Test | Pearson’s Test | |
|---|---|---|
| TDI vs. Life Quality | rho = 0.1, p = 0.305 | rho = 0.040, p = 0.680 |
| TDI vs. Positive Life Quality | rho = 0.040, p = 0.685 | rho = 0.037, p = 0.702 |
| TDI vs. Sincerity Statement | rho = 0.171, p = 0.133 | rho = 0.151, p = 0.119 |
| TDI vs. Sincerity Inverse | rho = 0.061, p = 0.532 | rho = 0.1, p = 0.306 |
| TDI vs. Parosmia | rho = 0.007, p = 0.940 | rho = 0.014, p = 0.883 |
| TDI vs. Scale 1 | rho = 0.160, p = 0.098 | rho = 0.150, p = 0.121 |
| TDI vs. Scale 2 | rho = 0.213, p = 0.027 * | rho = 0.201, p = 0.037 * |
| TDI vs. Scale 3 | rho = 0.154, p = 0.112 | rho = 0.144, p = 0.137 |
| TDI vs. Scale 4 | rho = 0.028, p = 0.776 | rho = 0.044, p = 0.652 |
| TDI vs. Scale 5 | rho = 0.093, p = 0.340 | rho = 0.064, p = 0.514 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Molnár, A.; Maihoub, S.; Mavrogeni, P.; Krasznai, M.; Tamás, L.; Kraxner, H. The Correlation between the Results of the Sniffin’ Sticks Test, Demographic Data, and Questionnaire of Olfactory Disorders in a Hungarian Population after a SARS-CoV-2 Infection. J. Clin. Med. 2023, 12, 1041. https://doi.org/10.3390/jcm12031041
Molnár A, Maihoub S, Mavrogeni P, Krasznai M, Tamás L, Kraxner H. The Correlation between the Results of the Sniffin’ Sticks Test, Demographic Data, and Questionnaire of Olfactory Disorders in a Hungarian Population after a SARS-CoV-2 Infection. Journal of Clinical Medicine. 2023; 12(3):1041. https://doi.org/10.3390/jcm12031041
Chicago/Turabian StyleMolnár, András, Stefani Maihoub, Panayiota Mavrogeni, Magdolna Krasznai, László Tamás, and Helga Kraxner. 2023. "The Correlation between the Results of the Sniffin’ Sticks Test, Demographic Data, and Questionnaire of Olfactory Disorders in a Hungarian Population after a SARS-CoV-2 Infection" Journal of Clinical Medicine 12, no. 3: 1041. https://doi.org/10.3390/jcm12031041
APA StyleMolnár, A., Maihoub, S., Mavrogeni, P., Krasznai, M., Tamás, L., & Kraxner, H. (2023). The Correlation between the Results of the Sniffin’ Sticks Test, Demographic Data, and Questionnaire of Olfactory Disorders in a Hungarian Population after a SARS-CoV-2 Infection. Journal of Clinical Medicine, 12(3), 1041. https://doi.org/10.3390/jcm12031041







