3D-Printed Biomaterial Testing in Response to Cryoablation: Implications for Surgical Ventricular Tachycardia Ablation
Abstract
1. Introduction
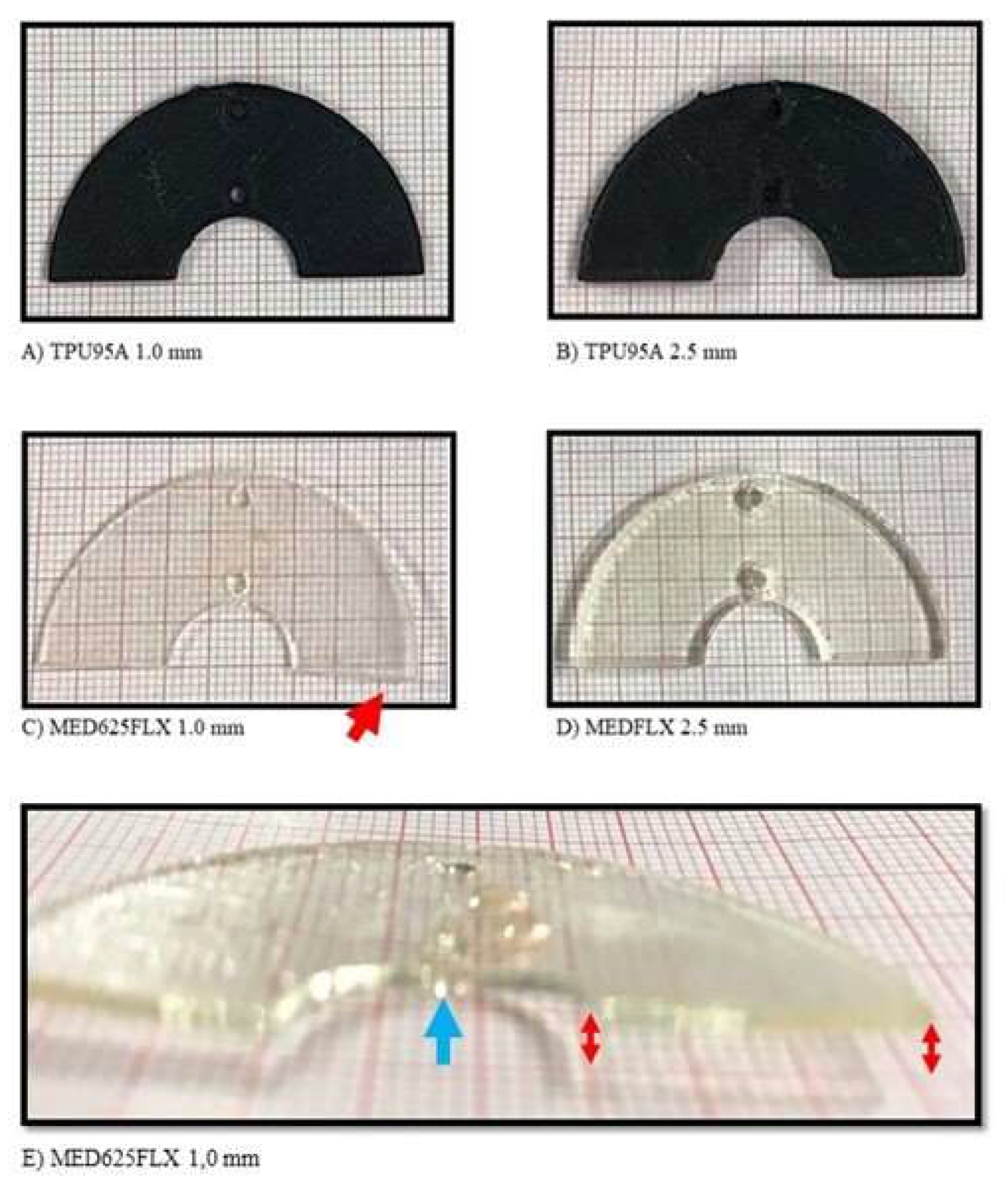
2. Material and Methods
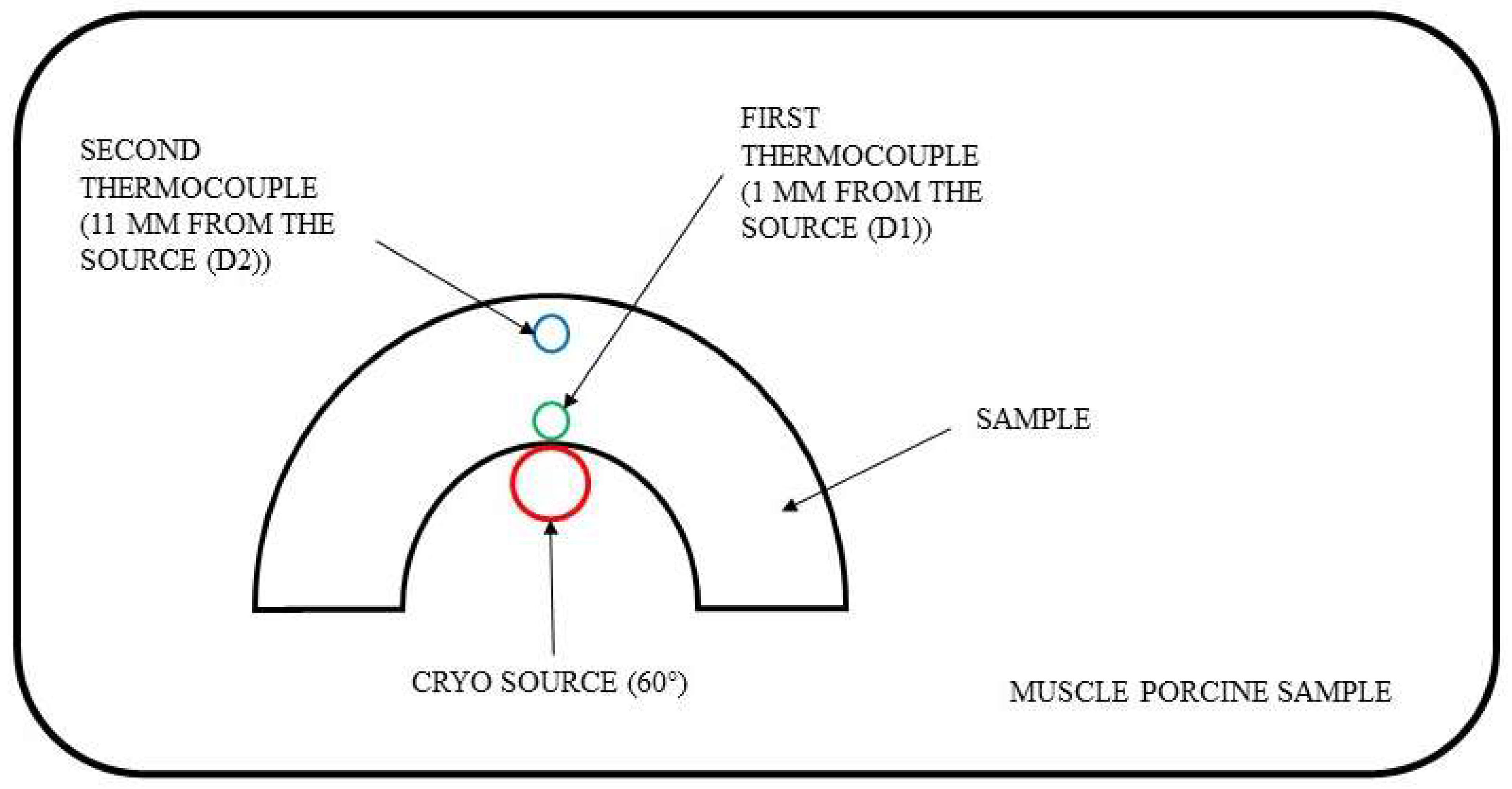
2.1. Procedure
2.2. Experimental Test
2.3. Statistical Analysis
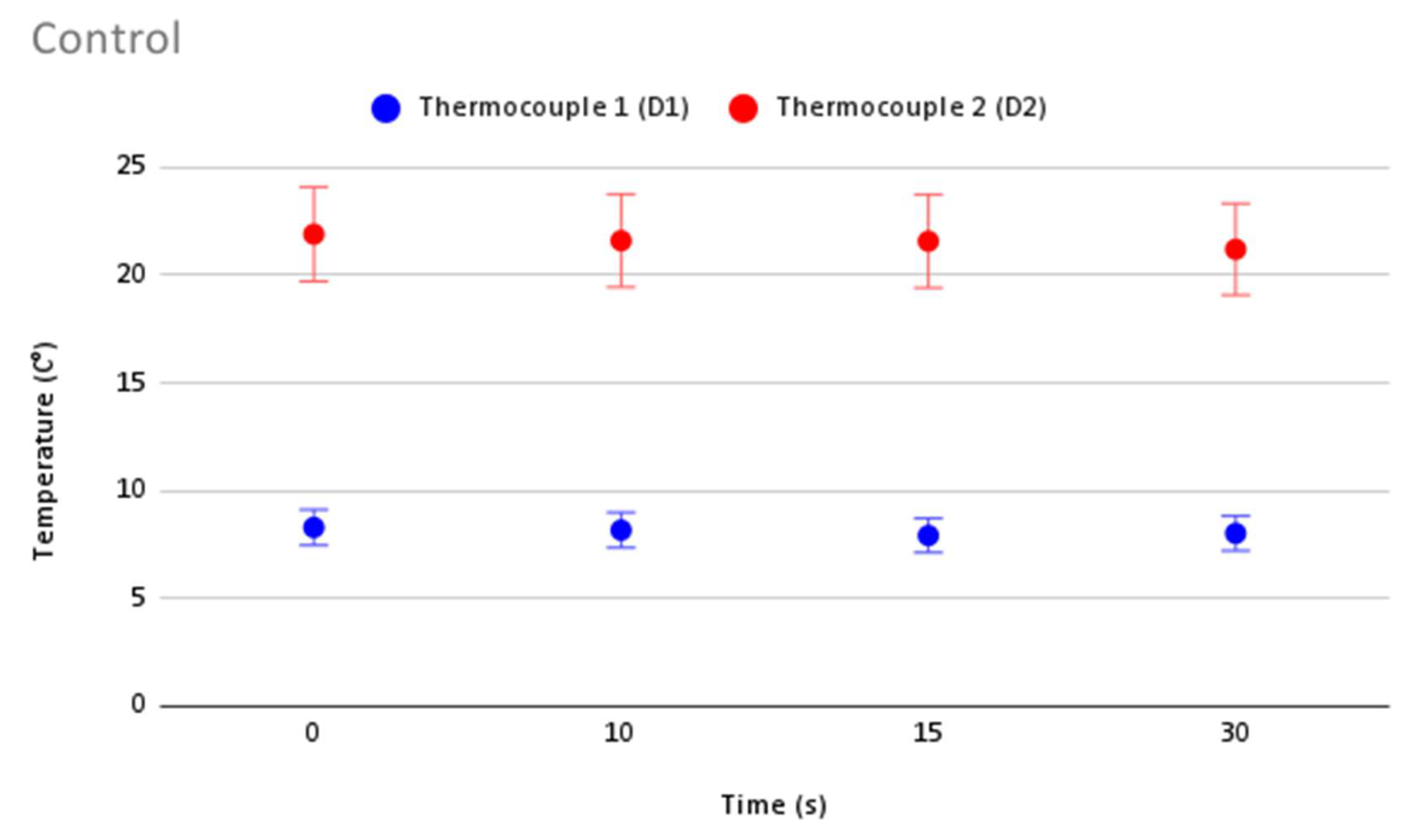
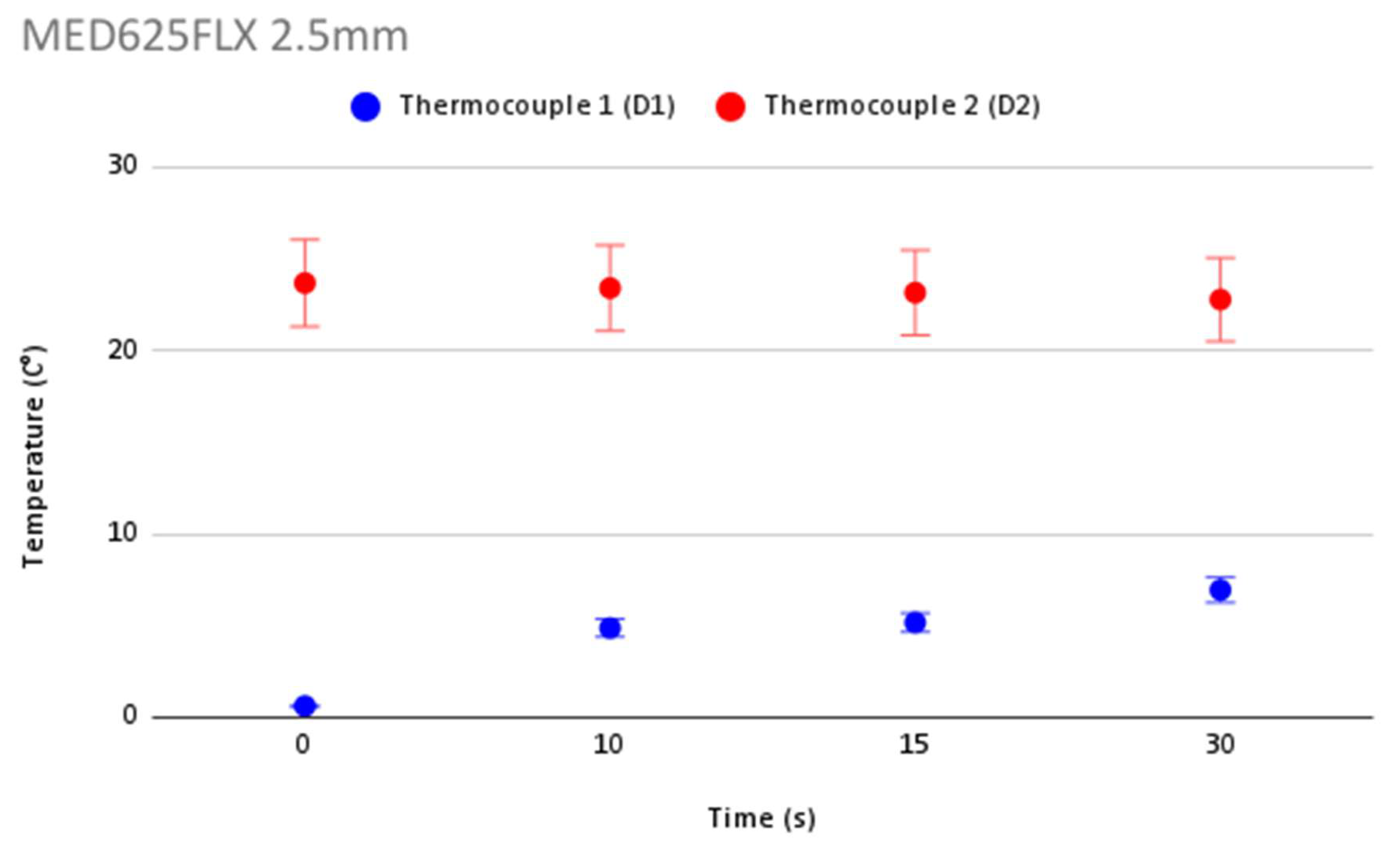
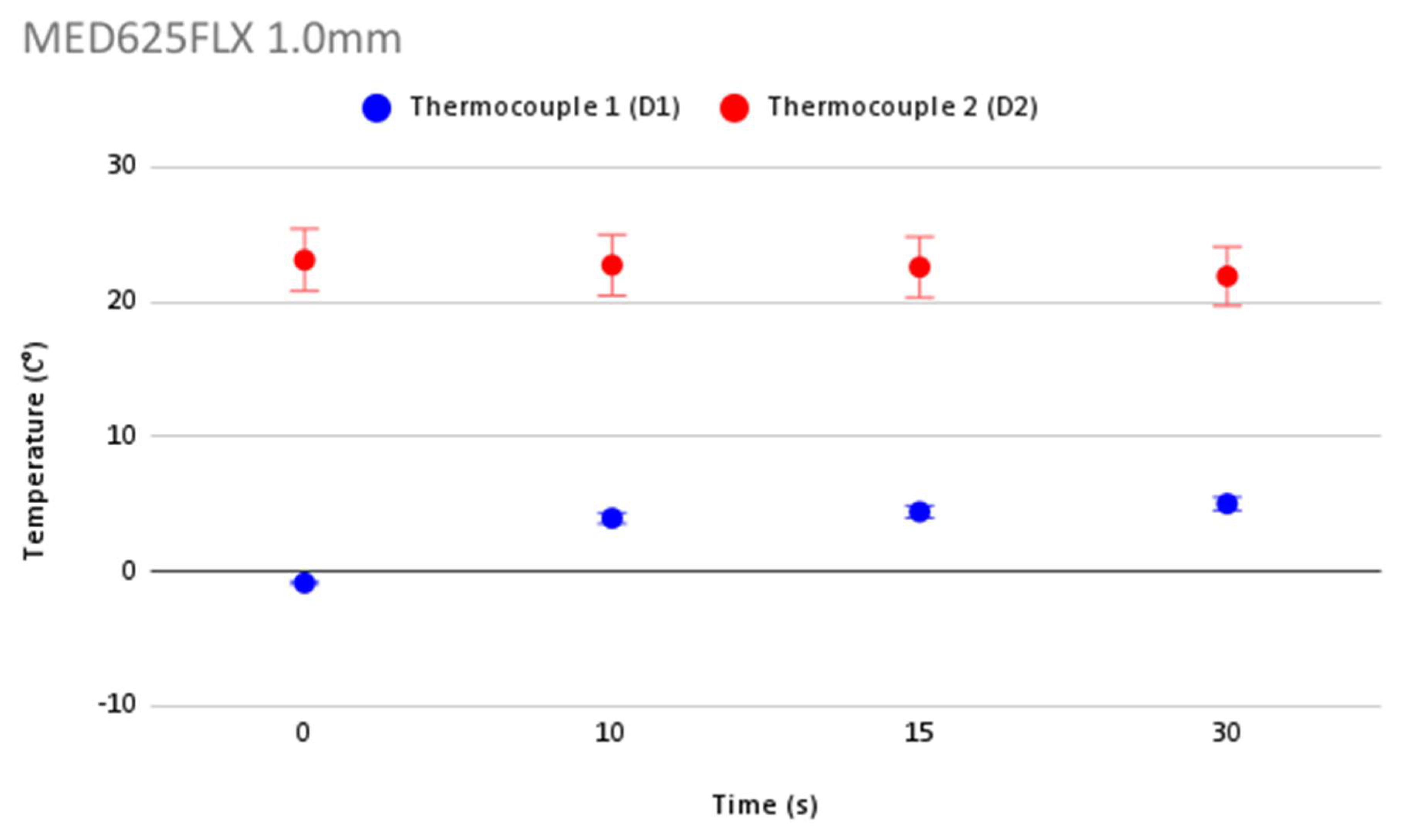
3. Results
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pugliese, R.; Beltrami, B.; Regondi, S.; Lunetta, C. Polymeric biomaterials for 3D printing in medicine: An overview. Ann. 3D Print. Med. 2021, 2, 100011. [Google Scholar] [CrossRef]
- Cox, J.L.; Malaisrie, S.C.; Churyla, A.; Mehta, C.; Kruse, J.; Kislitsina, O.N.; McCarthy, P.M. Cryosurgery for Atrial Fibrillation: Physiologic Basis for Creating Optimal Cryolesions. Ann. Thorac. Surg. 2021, 112, 354–362. [Google Scholar] [CrossRef] [PubMed]
- Gage, A.A.; Baust, J. Mechanisms of tissue injury in cryosurgery. Cryobiology 1998, 37, 17–186. [Google Scholar] [CrossRef] [PubMed]
- Gage, A.A.; Baust, J.M.; Baust, J.G. Experimental cryosurgery investigations in vivo. Cryobiology 2009, 59, 229–243. [Google Scholar] [CrossRef] [PubMed]
- Holman, W.L.; Ikeshita, M.; Douglas, J.M., Jr.; Smith, P.K.; Cox, J.L. Cardiac cryosurgery: Effects of myocardial temperature on cryolesion size. Surgery 1983, 93, 268–272. [Google Scholar] [PubMed]
- Masroor, S. Can Epicardial Ablation Create Optimal Cryolesions? Ann. Thorac. Surg. 2022, 114, 1522–1523. [Google Scholar] [CrossRef] [PubMed]
- Weimar, T.; Lee, A.M.; Ray, S.; Schuessler, R.B.; Damiano, R.J., Jr. Evaluation of a novel cryoablation system: In vivo testing in a chronic porcine model. Innovations 2012, 7, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Prohaska, J.; Jan, A.H. Cryotherapy. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Ifedili, I.; Mouksian, K.; Jones, D.; El Masri, I.; Heckle, M.; Jefferies, J.; Levine, Y.C. Ablation Therapy for Persistent Atrial Fibrillation. Curr Cardiol Rev. 2022, 18, e290721195115. [Google Scholar] [CrossRef] [PubMed]
- Baust, J.G.; Snyder, K.K.; Santucci, K.L.; Robilotto, A.T.; Van Buskirk, R.G.; Baust, J.M. Cryoablation: Physical and molecular basis with putative immunological consequences. Int. J. Hyperth. 2019, 36 (Suppl. 1), 10–16. [Google Scholar] [CrossRef] [PubMed]
- Candelari, M.; Cappello, I.A.; Pannone, L.; Monaco, C.; Talevi, G.; Bori, E.; Ramak, R.; La Meir, M.; Gharaviri, A.; Chierchia, G.B.; et al. A 3D-printed surgical guide for ischemic scar targeting and ablation. Front. Cardiovasc. Med. 2022, 9, 1029816. [Google Scholar] [CrossRef] [PubMed]
- Cappello, I.A.; Candelari, M.; Pannone, L.; Monaco, C.; Bori, E.; Talevi, G.; Ramak, R.; La Meir, M.; Gharaviri, A.; Chierchia, G.B.; et al. 3D Printed Surgical Guide for Coronary Artery Bypass Graft: Workflow from Computed Tomography to Prototype. Bioengineering 2022, 9, 179. [Google Scholar] [CrossRef] [PubMed]
- Cappello, I.A.; Candelari, M.; Pannone, L.; Monaco, C.; Bori, E.; Talevi, G.; Ramak, R.; La Meir, M.; Gharaviri, A.; Chierchia, G.B.; et al. Temperature Analysis of 3D-Printed Biomaterials During Unipolar and Bipolar Radiofrequency Ablation Procedure. Front. Cardiovasc. Med. 2022, 9, 978333. [Google Scholar] [CrossRef] [PubMed]
- Andrade, J.G.; Khairy, P.; Dubuc, M. Catheter Cryoablation: Biology and Clinical Uses. Circ. Arrhythmia Electrophysiol. 2013, 6, 218–227. [Google Scholar] [CrossRef] [PubMed]
- AtriCure. Available online: www.atricure.com (accessed on 3 October 2022).
- Stratasys. Available online: www.stratasys.com (accessed on 3 October 2022).
- Abdul Samat, A.; Abdul Hamid, Z.A.; Jaafar, M.; Yahaya, B.H. Mechanical Properties and In Vitro Evaluation of Thermoplastic Polyurethane and Polylactic Acid Blend for Fabrication of 3D Filaments for Tracheal Tissue Engineering. Polymers 2021, 13, 3087. [Google Scholar] [CrossRef] [PubMed]
- Yu, E.; Zhang, J.; Thomson, J.A.; Turng, L.S. Fabrication and Characterization of Electrospun Thermoplastic Polyurethane/Fibroin Small-Diameter Vascular Grafts for Vascular Tissue Engineering. Int. Polym. Process. 2016, 31, 638–646. [Google Scholar] [CrossRef] [PubMed]
- Ultimaker. Available online: www.ultimaker.com (accessed on 3 October 2022).
- Sterris Healthcare. Available online: www.steris.com (accessed on 3 October 2022).
- Kawel, N.; Turkbey, E.B.; Carr, J.J.; Eng, J.; Gomes, A.S.; Hundley, W.G.; Johnson, C.; Masri, S.C.; Prince, M.R.; van der Geest, R.J.; et al. Normal left ventricular myocardial thickness for middle-aged and older subjects with steady-state free precession cardiac magnetic resonance: The multi-ethnic study of atherosclerosis. Circ. Cardiovasc. Imaging 2012, 5, 500–508. [Google Scholar] [CrossRef] [PubMed]
- Ammarullah, M.I.; Santoso, G.; Sugiharto, S.; Supriyono, T.; Wibowo, D.B.; Kurdi, O.; Tauviqirrahman, M.; Jamari, J. Minimizing Risk of Failure from Ceramic-on-Ceramic Total Hip Prosthesis by Selecting Ceramic Materials Based on Tresca Stress. Sustainability 2022, 14, 13413. [Google Scholar] [CrossRef]
- Stratasys Ltd. Biocompatible. 2020. Available online: https://www.stratasys.com/materials/search/biocompatible (accessed on 20 November 2022).




| Test | Standard |
|---|---|
| Cytotoxicity | EN ISO 10993-5:2009 |
| Irritation | EN ISO 10993-10:2013 |
| Delayed-type hypersensitivity | EN ISO 10993-10:2013 |
| Material mediated pyrogenicity (FDM USP <151>) | EN ISO 10993-11:2009 |
| Acute systemic toxicity | EN ISO 10993-11:2009 |
| Chemical characterization | EN ISO 10993-18:2009 |
| Allowable limits for leachable substances | EN ISO 10993-17:2009 |
| USP plastic class VI | USP 34 <88> |
| Genotoxicity | EN ISO 10993-3:2014 |
| Control | Temperature in D1 (°C) | Temperature in D2 (°C) | ||||||
|---|---|---|---|---|---|---|---|---|
| Control * | 14.5 | 14.2 | 12.9 | 11.2 | 23.0 | 22.4 | 22.6 | 22.4 |
| Control ** | 9.7 | 9.1 | 8.7 | 8.0 | 23.9 | 23.5 | 23.4 | 22.7 |
| Control *** | 8.0 | 8.5 | 9.1 | 10.8 | 24.4 | 23.9 | 23.7 | 23.3 |
| Control **** | 1.0 | 0.9 | 1.0 | 2.1 | 16.3 | 16.6 | 16.6 | 16.4 |
| Time | 0 s | 10 s | 15 s | 30 s | 0 s | 10 s | 15 s | 30 s |
| MED625FLX | Sample N° | Temperature in D1 (°C) | Temperature in D2 (°C) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2.5 mm | 1 * | 11.0 | 10.3 | 10.2 | 11.3 | 29.0 | 28.8 | 28.5 | 28.3 |
| 1 ** | 16.0 | 15.4 | 14.2 | 17.4 | 27.0 | 26.8 | 26.7 | 26.3 | |
| 1 *** | −8.7 | −3.0 | −2.2 | −0.8 | 19.3 | 18.9 | 18.6 | 18.3 | |
| 1 **** | −15.8 | −3.2 | −1.5 | −0.1 | 19.4 | 19.1 | 18.8 | 18.2 | |
| 1.0 mm | 3 * | 5.9 | 5.7 | 6.1 | 6.9 | 29.0 | 28.5 | 28.4 | 27.2 |
| 3 ** | 15.4 | 15.2 | 15.2 | 15.3 | 27.3 | 27.2 | 27.0 | 26.8 | |
| 3 *** | −20.8 | −4.0 | −2.8 | −2.2 | 17.5 | 16.7 | 16.6 | 15.8 | |
| 3 **** | −3.9 | −1.1 | −0.8 | 0.1 | 18.6 | 18.5 | 18.3 | 17.8 | |
| Time | 0 s | 10 s | 15 s | 30 s | 0 s | 10 s | 15 s | 30 s | |
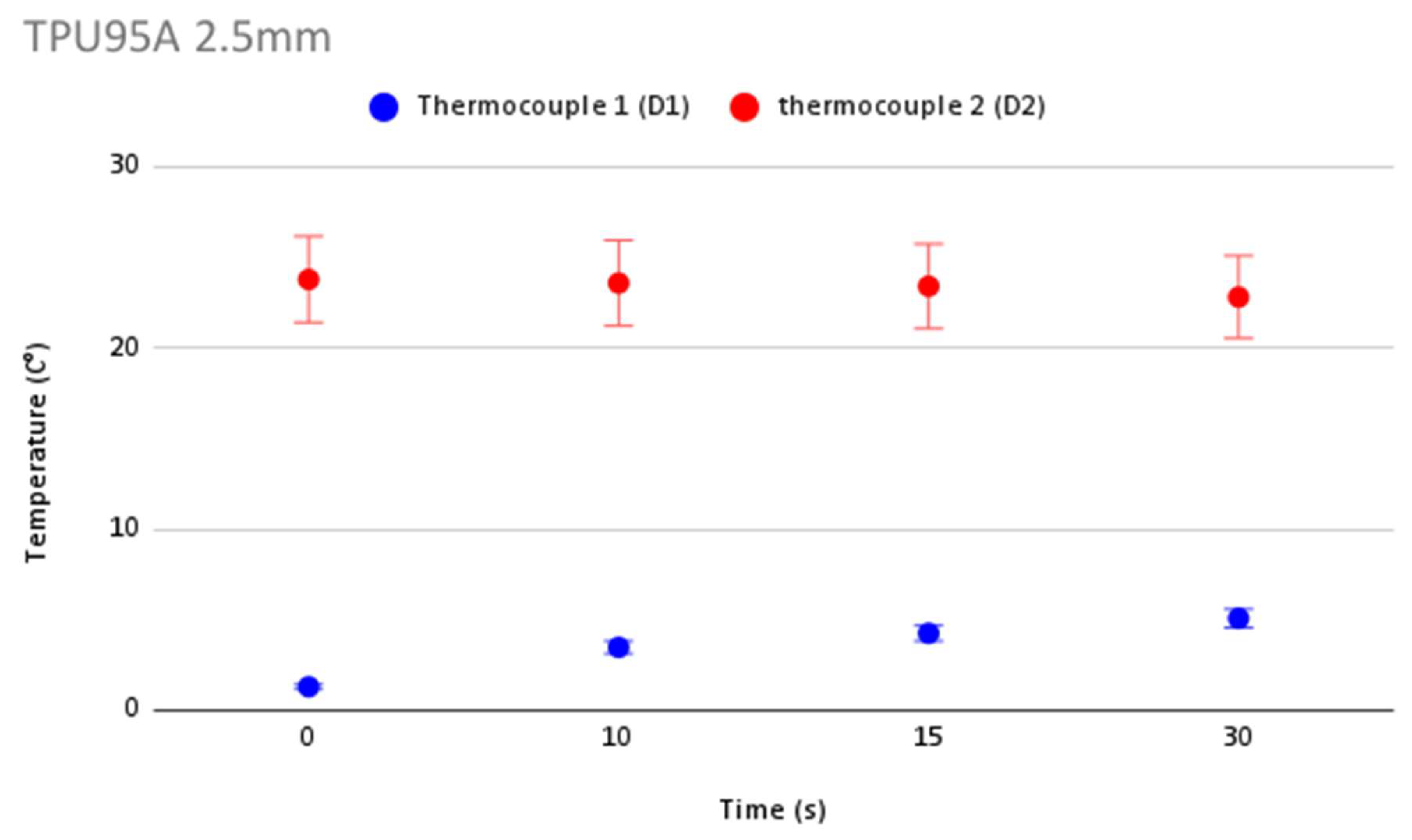
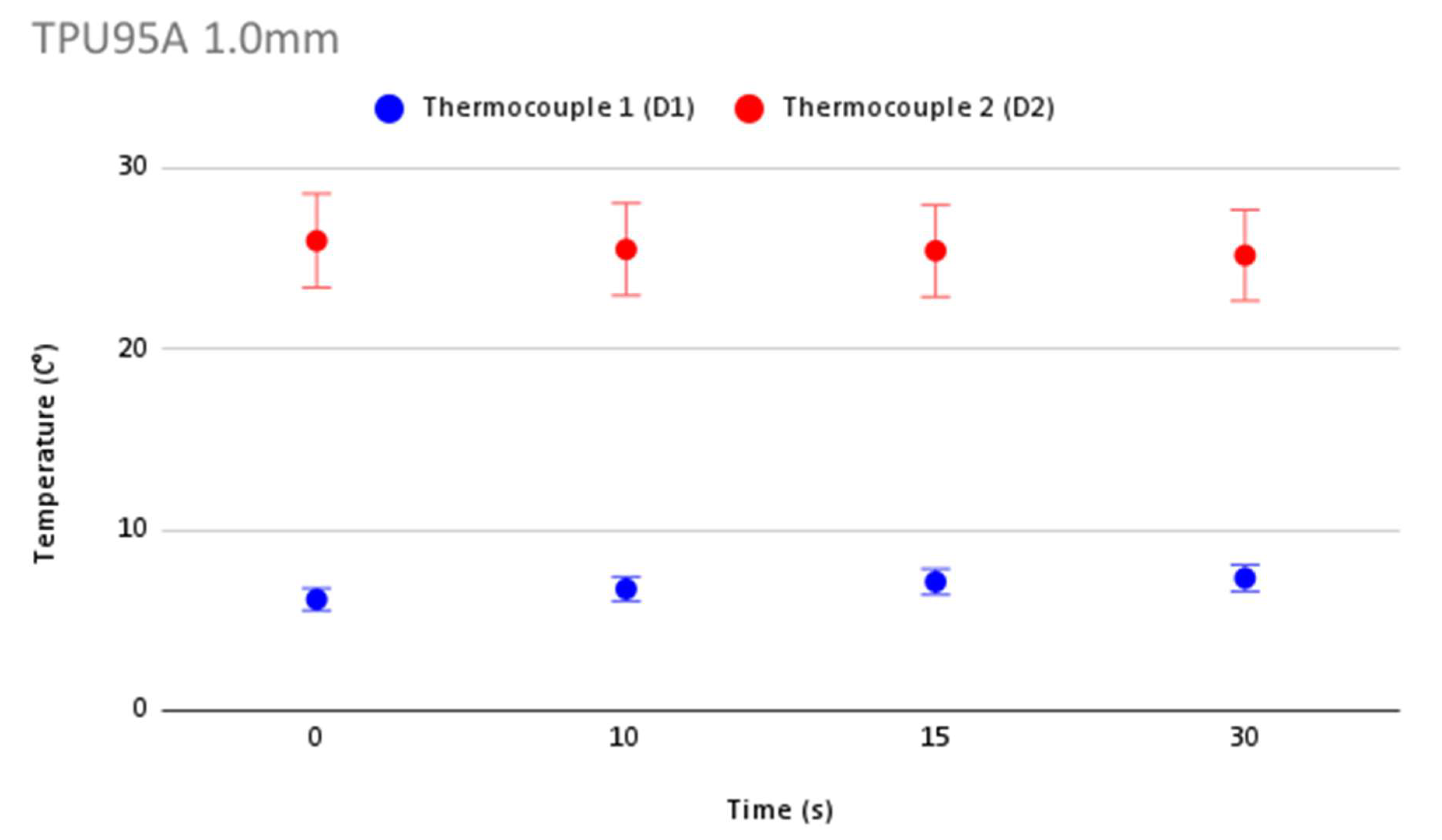
| TPU95A | Sample N° | Temperature in D1 (°C) | Temperature in D2 (°C) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2.5 mm | 2 * | 12.2 | 12.4 | 12.6 | 13.4 | 27.9 | 27.6 | 27.4 | 27.0 |
| 2 ** | 7.5 | 6.8 | 6.8 | 7.8 | 25.2 | 25.2 | 24.9 | 24.1 | |
| 2 *** | −11.1 | −4.2 | −2.1 | −1.0 | 22.2 | 21.9 | 21.8 | 21.3 | |
| 2 **** | −3.4 | −1.1 | −0.3 | 0.1 | 19.8 | 19.6 | 19.5 | 18.8 | |
| 1.0 mm | 4 * | 11.6 | 10.6 | 9.8 | 9.5 | 28.9 | 28.6 | 28.4 | 27.9 |
| 4 ** | 18.2 | 18.2 | 18.1 | 17.7 | 28.0 | 27.9 | 27.8 | 27.5 | |
| 4 *** | 0.4 | 0.9 | 1.9 | 2.6 | 23.7 | 22.6 | 22.7 | 22.8 | |
| 4 **** | −5.6 | −2.8 | −1.3 | −0.5 | 23.3 | 22.9 | 22.8 | 22.5 | |
| Time | 0 s | 10 s | 15 s | 30 s | 0 s | 10 s | 15 s | 30 s | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Candelari, M.; Cappello, I.A.; Pannone, L.; Monaco, C.; Bori, E.; Talevi, G.; Ramak, R.; La Meir, M.; Gharaviri, A.; Chierchia, G.B.; et al. 3D-Printed Biomaterial Testing in Response to Cryoablation: Implications for Surgical Ventricular Tachycardia Ablation. J. Clin. Med. 2023, 12, 1036. https://doi.org/10.3390/jcm12031036
Candelari M, Cappello IA, Pannone L, Monaco C, Bori E, Talevi G, Ramak R, La Meir M, Gharaviri A, Chierchia GB, et al. 3D-Printed Biomaterial Testing in Response to Cryoablation: Implications for Surgical Ventricular Tachycardia Ablation. Journal of Clinical Medicine. 2023; 12(3):1036. https://doi.org/10.3390/jcm12031036
Chicago/Turabian StyleCandelari, Mara, Ida Anna Cappello, Luigi Pannone, Cinzia Monaco, Edoardo Bori, Giacomo Talevi, Robbert Ramak, Mark La Meir, Ali Gharaviri, Gian Battista Chierchia, and et al. 2023. "3D-Printed Biomaterial Testing in Response to Cryoablation: Implications for Surgical Ventricular Tachycardia Ablation" Journal of Clinical Medicine 12, no. 3: 1036. https://doi.org/10.3390/jcm12031036
APA StyleCandelari, M., Cappello, I. A., Pannone, L., Monaco, C., Bori, E., Talevi, G., Ramak, R., La Meir, M., Gharaviri, A., Chierchia, G. B., de Asmundis, C., & Innocenti, B. (2023). 3D-Printed Biomaterial Testing in Response to Cryoablation: Implications for Surgical Ventricular Tachycardia Ablation. Journal of Clinical Medicine, 12(3), 1036. https://doi.org/10.3390/jcm12031036








