Abstract
Submacular hemorrhage (SMH) is the accumulation of blood in the macular area that can severely damage the macular structure and visual function. Recently, the intraocular administration of tissue plasminogen activator (TPA) with anti-vascular endothelial growth factor (anti-VEGF) drugs was reported to have a positive effect on SMH. This meta-analysis aimed to explore the efficacy and safety of the drug combination. We systematically searched the Web of Science, MEDLINE, EMBASE, and Cochrane Library databases and screened relevant full-length literature reports. The quality of the reports was assessed by two independent reviewers. The best-corrected visual acuity (BCVA) and foveal thickness (FT) were considered the main indicators of efficacy. RevMan 5.4 software was used for this meta-analysis. Twelve studies were analyzed, and the results showed that BCVA at 1 month (p < 0.001), 3 months (p < 0.001), 6 months (p < 0.001), and the last follow-up (p < 0.001) was improved relative to the preoperative value. The postoperative FT was lower than the preoperative FT (p < 0.001). No significant difference in efficacy was observed between subretinal and intravitreal TPA injections (p = 0.37). TPA with anti-VEGF drugs is safe for SMH treatment and can significantly improve BCVA and reduce FT.
1. Introduction
Submacular hemorrhage (SMH) is characterized by the presence of blood between the retinal pigment epithelium (RPE) and the neurosensory retina in the macular area. It is caused by choroidal and retinal vascular abnormalities [1]. SMH damages photoreceptors in several ways, including iron toxicity, fibrin meshwork contraction, outer retinal shear forces, and reduced nutrient supply, eventually resulting in macular scarring [2]. SMH caused by various ocular diseases such as neovascular age-related macular degeneration (nAMD), polypoid choroidal vasculopathy (PCV), pathological myopia, and retinal aneurysm has a significantly negative impact on the patient’s visual ability, with a poor prognosis [3]. A population-based study in 2014 estimated that the annual incidence of new and large SMH complicated with wet AMD was approximately 25 per million per year, which is detrimental to global eye health [4]. The cellular mechanism of SMH remains to be explored, as recent studies have revealed the importance of oxidative stress and inflammation response in arteriovenous pathologies [5,6]. SMH can result in sudden or progressive vision loss depending on the extent and thickness of the bleeding, and the reception of visual information by photoreceptors can be blocked, with subsequent damage. A retrospective review of eyes with massive SMH confirmed that visual acuity correlated inversely with the thickness rather than the diameter of SMH [7].
Several methods have been used for the treatment of SMH secondary to AMD. Surgical progress mainly focuses on vitrectomy along with multiple procedures such as the removal of choroidal neovascularization (CNV) lesions, macular translocation, RPE patch repair, and gas replacement, followed by intravitreal/subretinal drug injection or SMH drainage [8]. Tissue plasminogen activator (TPA) is a commonly used drug for SMH treatment. It has a molecular weight of 72 kD and a short half-life [8]. The plasminogen is activated by fibrin and transformed into plasmin, which combines with fibrin to dissolve blood clots [9]. Thus, the injection of TPA into the subretinal area would protect the retina by cleaving the fibrin, dissolving the clot, reducing iron toxicity, and improving nutritional supply [8,9]. In the past decades, many studies have shown that TPA injection and pneumatic displacement during surgery are effective in displacing SMH and, consequently, improving postoperative vision. Both intravitreal and subretinal injections of TPA are widely used [10,11,12,13]. Subretinal injection (SRI) of TPA could dissolve the clot and displace SMH, which allows the blood to be evacuated through a small retinotomy. However, this method is risky and can cause complications [14]. The intravitreal injection (IVI) of TPA is considered an alternative therapy because of its efficacy [11]. Because the incidence of complications is lower than that after a single surgery, such as pars plana vitrectomy, it is considered a minimally invasive and valuable approach [15]. TPA and gas can efficiently displace hemorrhage; however, CNV progression after SMH could limit the therapeutic effects of these techniques. In addition, anti-vascular endothelial growth factor (anti-VEGF) drugs are widely used to treat underlying CNV [16]. A few studies have reported that intravitreal anti-VEGF monotherapy could offer moderate visual gain in patients with SMH; however, the co-application of TPA and anti-VEGF is commonly chosen to maintain the treatment effects [16,17,18].
Currently, there is no gold standard treatment principle for SMH, and the order in which TPA and anti-VEGF are used remains unclear, with variable results. Bardak et al. [19] found that SMH displacement was successfully achieved with sequential TPA administration, pneumatic displacement, and anti-VEGF drug therapy in 16 eyes of 16 patients. The postoperative best-corrected visual acuity (BCVA) of all patients was significantly improved at 1, 3, 6, and 12 months. In another study by Avci et al. [20], 30 patients diagnosed with SMH received TPA and anti-VEGF drugs during the surgical procedure. Compared with that at baseline, BCVA significantly improved at 1, 2, 3, and 12 months postoperatively. Furthermore, the group that received additional anti-VEGF therapy showed a significant reduction in the SMH area. The differences in results among these studies could be attributed to differences in the indications for surgery, baseline demographics, and treatment protocols. The aim of this meta-analysis was to evaluate the efficacy and safety of TPA with anti-VEGF therapy for SMH and consolidate the available evidence.
2. Materials and Methods
2.1. Search Strategy
The Web of Science, MEDLINE, EMBASE, and Cochrane Library databases were systematically searched from inception through 10 June 2022. Keywords included submacular hemorrhage, sub-macular hemorrhage, or SMH; recombinant tissue plasminogen activator, rt-PA, rtPA, r-tPA, or rTPA; and anti-vascular endothelial growth factor, anti-VEGF, ranibizumab, aflibercept, conbercept, or bevacizumab. Only articles published in English were included in the analysis. There were no date restrictions.
2.2. Literature Inclusion and Exclusion Criteria
Only clinical trials evaluating the efficacy of combined anti-VEGF and TPA treatments for SMH were included. Case reports, review articles, medical guidelines, abstract-only publications, and conference summaries were excluded. In addition, publications in languages other than English were excluded. Two independent reviewers (X.H. and W.C.) screened the articles by reading the titles, abstracts, keywords, and full texts. Studies that did not report the number of eyes and/or involved a small sample size of fewer than eight eyes were excluded. Moreover, studies were excluded if the group setting or data analysis was inappropriate. Studies based on the sequential application of anti-VEGF drugs and TPA were also excluded. Articles that met the requirements were listed and evaluated to ensure the inclusion of all eligible studies. Disagreements between the researchers were resolved through consultation with a third author (N.Z.). This meta-analysis was performed in accordance with the PRISMA guidelines (registration number CRD42022358037).
2.3. Literature Quality Evaluation
Because all the included studies were retrospective in nature, the Newcastle–Ottawa Scale (NOS) [21] was used by the two authors to assess the methodological quality and risk of bias of the studies. NOS is based on a star system for assessing the quality of case-control or cohort studies for seven items categorized into three broad groups: (1) selection (S, four stars), (2) comparability (C, two stars), and (3) exposure or outcome (O, three stars). Thus, the maximum number of stars that a study can receive is nine. Two authors (X.H. and W.C.) independently assessed the quality of the included studies. Disagreements between the researchers were resolved through consultation with a third author (N.Z.).
2.4. Outcome Indicator
The primary outcome measures were BCVA and the foveal thickness (FT) after treatment. The secondary outcomes were hemorrhage displacement and postoperative complications.
2.5. Data Extraction
Data from the included studies were independently extracted by two authors (X.H., W.C.). Studies with unclear or missing data records were excluded, and disagreements between the researchers were resolved through consultation with a third author (N.Z.). Data were collected and recorded as follows: (1) literature information for the included studies (first author, publication time, country, or region), (2) basic information about the study participants (sample size, age, sex, duration of disease course, baseline BCVA, baseline FT, and intervention measures), and (3) outcomes (BCVA after treatment, FT after treatment, bleeding displacement, and postoperative complications).
2.6. Statistical Methods
Data analysis was performed using Review Manager (RevMan 5.4, The Cochrane Collaboration, Oxford, UK) software. Continuous variables were statistically analyzed using the mean difference and are reported as the weighted mean deviation (WMD) with a 95% confidence interval (CI). Forest plots were used to describe and represent the statistical results.
When follow-up data were available at several time points in the study, the data at each follow-up and the final reported data were extracted. A paired-samples test was used to compare data before and after treatment.
The I2 statistic was used to evaluate the heterogeneity of the results. I2 ≤ 50% indicated low heterogeneity, and a fixed effects model was used. When I2 was >50%, the heterogeneity was considered high, and a random effects model was used. Funnel plots were used for the visual assessment of publication bias.
3. Results
3.1. Search Results
The study selection flowchart is shown in Figure 1. In total, 171 articles (PubMed (n = 70), Embase (n = 58), Cochrane Library (n = 6), and Web of Science (n = 37)) were identified. No Chinese database was included in this study. Endnote literature management software was used to remove 68 duplicates. Based on the literature type and language, 47 articles were excluded, including 13 conference papers, 11 reviews, one letter, 13 case reports, and nine non-English articles. After reading the title and abstract, 30 articles were eliminated, including three clinical trials with unreported results, four articles on animal experiments, and 23 without the combined use of TPA and anti-VEGF drugs. Subsequently, two independent reviewers screened the full text of 26 possible relevant studies, 14 of which were excluded because of missing data, unclear documentation, or loss of follow-up. Thus, 12 retrospective studies [20,22,23,24,25,26,27,28,29,30,31,32] including a total of 269 eyes from 269 participants were included in this meta-analysis.
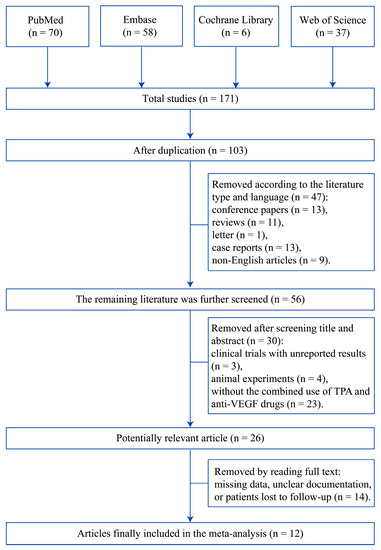
Figure 1.
Study selection flowchart.
3.2. Description of the Included Studies
The 12 articles included in this meta-analysis were retrospective studies. Table 1 summarizes the main characteristics of the included studies, including the first author, publication time, sample size, number of eyes, country, etiology of SMH, patient age, disease duration, bleeding area, and NOS star level. Based on the conversion relationship between the bleeding area and the optic disc diameter in the study by Arias et al. [22], the bleeding areas in the studies by Avci et al. [20] and Kitagawa et al. [26] were converted into a representation of the optic disc diameter.

Table 1.
Characteristics of the included studies.
Table 2 presents the treatment modalities, complications, and hemorrhage displacement procedures received by the study participants. Grohmann et al. [31] evaluated the effect of three surgical modalities for SMH treatment and termed them Grohmann G1, G2, or G3 according to the different treatment regimens received by each group.

Table 2.
Treatment regimens received by the included study participants.
The BCVA and FT data before and after SMH treatment are summarized in Table 3 and Table 4, respectively. Based on the conversion scheme of different visual acuity recording methods published by Ferris et al. [33], some of the original values in the studies by Erdogan et al. [30], Kitagawa et al. [26], and Guthoff et al. [24] were converted to logarithms of the minimum angle of resolution units to facilitate subsequent statistical analysis.

Table 3.
Follow-up of vision (logMAR).

Table 4.
Follow-up of foveal thickness.
3.3. Analysis Results
3.3.1. Analysis of BCVA
The final BCVA values in the 12 included studies were analyzed, and the comparative results are shown in the first forest plot (Figure 2). The final BCVA significantly improved relative to the initial BCVA (MD = −0.52, 95% CI= (−0.68, −0.37), I2 = 62%, p < 0.001). Heterogeneity analysis showed that I2 (62%) was more than 50%; therefore, a more conservative random effects model was used. The findings suggested that TPA combined with anti-VEGF therapy is effective in improving the final visual acuity of patients with SMH.
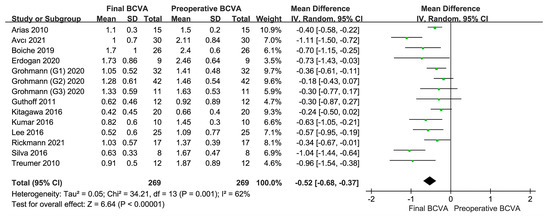
Figure 2.
Final BCVA versus preoperative BCVA [20,22,23,24,25,26,27,28,29,30,31,32]. All visual acuity data are expressed in logMAR. The results show that the BCVA of the study participants has significantly improved after combined treatment with TPA and anti-VEGF drugs. BCVA, best-corrected visual acuity; TPA, tissue plasminogen activator; anti-VEGF, anti-vascular endothelial growth factor; logMAR, logarithm of the minimum angle of resolution.
Among the included studies, six, five, and seven documented BCVA at 1, 3, and 6 months, respectively. Grohmann et al. [31] studied the influence of different surgical methods (G1, G2, and G3) on the treatment effect. The postoperative BCVA values at 1 (Figure 3A), 3 (Figure 3B), and 6 (Figure 3C) months were better than the preoperative BCVA. The results of the meta-analysis of postoperative BCVA values were as follows: 1 month: MD = −0.52, 95% CI = (−0.70, −0.35), I2 = 0%, p < 0.001; 3 months: MD = −0.63, 95% CI = (−0.87, −0.39), I2 = 45%, p < 0.001; and 6 months: MD = −0.48, 95% CI = (−0.67, −0.28), I2 = 64%, p < 0.001. The differences were statistically significant. The random effects model was used to compare the three groups at the different follow-up time points. The results suggested that TPA with anti-VEGF treatment for SMH significantly improves BCVA and the prognosis in the short and long terms, respectively.
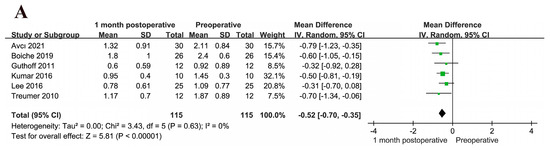
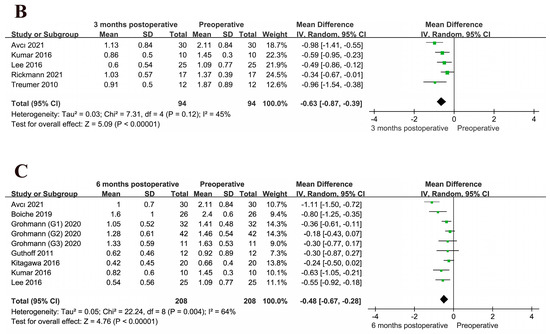
Figure 3.
(A) BCVA at 1 month postoperatively versus preoperative BCVA [20,23,24,27,28,29]. (B) BCVA at 3 months postoperatively versus preoperative BCVA [20,23,27,28,32]. (C) BCVA at 6 months postoperatively versus preoperative BCVA [20,24,26,27,28,29,31]. All visual acuity data are expressed in logMAR. BCVA values at the three different follow-up time points are significantly different from the preoperative BCVA. BCVA, best-corrected visual acuity; logMAR, logarithm of the minimum angle of resolution.
3.3.2. Effect of the Location of TPA Use on BCVA
The included studies were divided into two subgroups, SRI and IVI groups, according to the site of TPA injection. The results of this analysis are shown in Figure 4. The study by Arias et al. included both subretinal and intravitreal TPA injections, and the participants were not grouped according to the site of injection; therefore, this subgroup analysis was not included in the meta-analysis. The subgroup analysis showed that the SRI or IVI of TPA could increase BCVA (SRI group: MD = −0.63, 95% CI = (−0.92, −0.34), I2 = 71%, p < 0.001; IVI group: MD = −0.46, 95% CI = (−0.69, −0.23), I2 = 59%, p < 0.001; overall: MD = −0.54, 95% CI = (−0.72, −0.37), I2 = 64%, p = 0.37). A random effects model was used because I2 was >50%. Overall, the site of TPA administration did not affect the trend in BCVA improvement (p = 0.37 > 0.05 for the difference between groups).
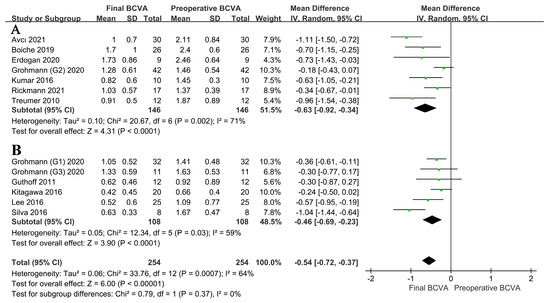
Figure 4.
(A) BCVA after the SRI [20,23,27,29,30,31,32] of TPA versus (B) BCVA after the IVI of TPA [24,25,26,28,31]. Both subgroups show improved postoperative BCVA relative to the preoperative BCVA, with no significant difference between the two subgroups. This indicates that the site of TPA injection does not affect BCVA. BCVA, best-corrected visual acuity; SRI, subretinal injection; TPA, tissue plasminogen activator; IVI, intravitreal injection.
3.3.3. Analysis of Foveal Thickness
Figure 5 shows the results of comparisons between the final FT and preoperative FT in cases subjected to combined TPA and anti-VEGF treatment for SMH. FT decreased postoperatively, and the difference was statistically significant (MD = −384.54, 95% CI = (−513.66, −255.42), I2 = 84%, p < 0.001). I2 was >50%, and the random effects model was used. The findings indicated that combined treatment with TPA and anti-VEGF drugs can promote a decrease in FT, which is beneficial for the structural recovery of the fovea in patients with SMH.
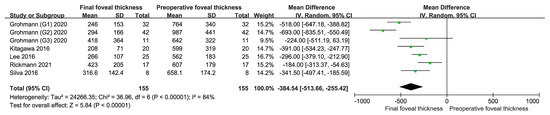
Figure 5.
Final foveal thickness versus preoperative foveal thickness [25,26,28,31,32]. The foveal thickness is expressed in microns (μm), and it has decreased after treatment. This indicates that the combination of TPA and anti-VEGF drugs is beneficial for the structural restoration of the fovea. TPA, tissue plasminogen activator; anti-VEGF, anti-vascular endothelial growth factor.
4. Discussion
The accumulation of blood in the macula can cause irreversible damage to photoreceptors within 24 h, and damage to visual function can be particularly serious [34]. The etiology of SMH can generally be divided into two categories: CNV (such as nAMD, PCV, and pathologic myopia) and non-CNV (such as retinal aneurysm, Terson syndrome, and trauma). CNV-associated SMH is more common. The choice of treatment for SMH is closely related to the cause of the hemorrhage. In non-CNV SMH, visual acuity usually improves to varying degrees after the blood is absorbed or cleared [35]. In CNV SMH, retinal neovascularization hinders physiological metabolic processes and acts as a basic factor for hemorrhage. Therefore, a reduction in the damage from hemorrhage in the macula and the inhibition of the persistent impact of neovascularization should be simultaneously achieved.
TPA is widely found in the aqueous humor, vitreous humor, and retina of the eye and plays an important role in eye development [36]. TPA can activate plasminogen into plasmin, which hydrolyzes fibrin and promotes blood clot dissolution and absorption [37]. The retinal expression of VEGF increases under hypoxia and induces neovascularization in the short term [38]. Based on the results of existing clinical trials, this article discusses the influence of the TPA injection site on the efficacy of combination therapy. Dr. Hilel Lewis showed in animals that labeled intravitreally injected TPA was present on the vitreous surface and failed to reach the neural retina or subretinal clots. This indicated that TPA does not diffuse through intact ILM in animals, and there is no scientific basis for the pure IVI of TPA in the treatment of SMH without vitreous hemorrhage, which may be caused by the rupture of the overlying retina [14]. This prompts doctors to select therapies according to the condition in clinical practice. Although we analyzed and concluded that the site of TPA administration does not affect the trend in BCVA improvement, rational selection of the TPA injection site according to the presence or absence of concomitant vitreous hemorrhage may provide greater benefits to patients. Anti-VEGF drugs can effectively inhibit neovascularization and reduce the associated damage to the eye [39]. A large number of studies have shown that the intraocular injection of TPA and anti-VEGF drugs can effectively and safely treat subretinal hemorrhage of different etiologies. However, the efficacy of combining the two drugs for the treatment of CNV SMH has not been systematically analyzed.
This meta-analysis included 269 eyes of 269 participants from 12 articles. Only a few of the reported complication rates in the included studies exceeded 30%, with most ranging from 2.4% to 20%; this indicates that TPA combined with anti-VEGF drugs is relatively safe. BCVA and FT were used as the main indicators of the efficacy of TPA with anti-VEGF drugs for the treatment of SMH. The results showed that TPA with anti-VEGF drug therapy significantly improved the BCVA of patients. At 1, 3, and 6 months after treatment, BCVA improved relative to that before treatment. In addition, five of these studies indicated that the combination of the two drugs reduced FT and promoted the structural recovery of the fovea. Furthermore, no significant differences in BCVA improvement were observed between subretinal and intravitreal TPA injections; this finding was not consistent with those of some other studies. For example, Wilkins et al. [40] and Ohayon et al. [41] found that the SRI of TPA can effectively promote the recovery of vision and facilitate the displacement and absorption of blood. In contrast, Tranos et al. [42] and Bell et al. [43] found that the IVI of TPA is beneficial for reducing the incidence of complications and has the same effect as SRI, consistent with our results. Notably, efficacy was limited by underlying diseases regardless of the type of treatment. Therefore, more research is needed to evaluate the efficacy of TPA and anti-VEGF therapy for SMH complicated by multiple eye diseases besides AMD.
This meta-analysis had some limitations. Several outcomes showed high heterogeneity in this research, probably because of the study population, duration of disease, and measurement methods. Random effects models were used for each of the primary outcomes to make the conclusions more reasonable, and subgroup analyses were performed according to the site of TPA injection. The 12 included articles were all retrospective studies; therefore, randomized controlled studies were lacking. Moreover, after the onset of SMH, patients are expected to receive the best individualized treatment; thus, setting a control group would be morally difficult. Therefore, the NOS scores of the included studies were generally five or seven stars (Table 1). After receiving the combined TPA and anti-VEGF treatment, some patients received additional anti-VEGF treatment, which was not included in this meta-analysis. During SMH treatment, in addition to TPA and anti-VEGF combination therapy, patients may have undergone other treatments such as surgery, gas replacement, and follow-up care, for a full recovery. These treatments are affected by various factors, such as the surgeon’s proficiency, medical conditions, and patient cooperation, and these factors may have introduced bias in the results of the clinical studies and secondary analyses. In addition, the sample size of some studies was slightly small, and multicenter, large-sample randomized controlled trials are needed to overcome the limitations of this study.
With the in-depth study of molecular mechanisms and the application of various experimental techniques, the treatment of SMH will predictably show standardization and precision in the future. Among vascular abnormality-related diseases, cerebral cavernous malformations have gained a lot of attention in recent years, and some studies have more deeply explored the dysregulated pathways such as oxidative stress and inflammation response in the pathogenesis by applying next-generation sequencing technology [5,6]. In ophthalmology, causative genes for abnormal angiogenic pathways are also being investigated [44]. These pioneering results based on transcriptome analysis point to genes that may be involved in pathogenesis and serve as potential therapeutic targets to diversify the diagnosis and treatment of diseases. Therefore, exploring and targeting pathogenesis at the cellular level may also become an important and insightful component of future SMH therapy.
5. Conclusions
In summary, this meta-analysis suggests that TPA with anti-VEGF drugs for SMH treatment is safe and can significantly improve BCVA and reduce FT, with no statistically significant difference in the treatment effect between subretinal and intravitreal TPA injections. Further studies should assess the optimal therapeutic doses of various anti-VEGF drugs and focus on monitoring complications.
Author Contributions
Conceptualization, N.Y. and Y.X.; writing—original draft preparation, X.H. and W.C. contributed equally to this work and should be considered co-first authors; methodology, X.H. and W.C.; software, X.H.; validation, N.Y. and N.Z.; formal analysis, N.Y., X.H. and W.C.; investigation, X.H., W.C. and N.Z.; data curation, X.H., W.C., Z.W., K.X. and L.Y.; writing—review and editing, N.Y.; supervision, N.Y. and Y.X.; funding acquisition, N.Y. and Y.X. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Hubei Key Laboratories Opening Project, grant number 2021KFY055; Natural Science Foundation of Hubei Province, grant number 2020CFB240; and Fundamental Research Funds for the Central Universities, grant number 2042020kf0065.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data that support the findings of this study are available from the online database.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kunavisarut, P.; Thithuan, T.; Patikulsila, D.; Choovuthayakorn, J.; Watanachai, N.; Chaikitmongkol, V.; Pathanapitoon, K.; Rothova, A. Submacular Hemorrhage: Visual Outcomes and Prognostic Factors. Asia-Pac. J. Ophthalmol. 2018, 7, 109–113. [Google Scholar] [CrossRef]
- Hochman, M.A.; Seery, C.M.; Zarbin, M.A. Pathophysiology and management of subretinal hemorrhage. Surv. Ophthalmol. 1997, 42, 195–213. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Kim, C.G.; Lee, D.W.; Yoo, S.J.; Lew, Y.J.; Cho, H.J.; Kim, J.Y.; Lee, S.H.; Kim, J.W. Intravitreal aflibercept for submacular hemorrhage secondary to neovascular age-related macular degeneration and polypoidal choroidal vasculopathy. Graefe’s Arch. Clin. Exp. Ophthalmol. 2020, 258, 107–116. [Google Scholar] [CrossRef] [PubMed]
- McGowan, G.F.; Steel, D.; Yorston, D. AMD with submacular hemorrhage: New insights from a population-based study. Investig. Ophthalmol. Vis. Sci. 2014, 55, 662. [Google Scholar]
- Scimone, C.; Donato, L.; Marino, S.; Alafaci, C.; D’Angelo, R.; Sidoti, A. Vis-à-vis: A focus on genetic features of cerebral cavernous malformations and brain arteriovenous malformations pathogenesis. Neurol. Sci. 2019, 40, 243–251. [Google Scholar] [CrossRef] [PubMed]
- Scimone, C.; Donato, L.; Alibrandi, S.; Esposito, T.; Alafaci, C.; D’Angelo, R.; Sidoti, A. Transcriptome analysis provides new molecular signatures in sporadic Cerebral Cavernous Malformation endothelial cells. Biochim. Biophys. Acta BBA—Mol. Basis Dis. 2020, 1866, 165956. [Google Scholar] [CrossRef] [PubMed]
- Bennett, S.R.; Folk, J.C.; Blodi, C.F.; Klugman, M. Factors prognostic of visual outcome in patients with subretinal hemorrhage. Am. J. Ophthalmol 1990, 109, 33–37. [Google Scholar] [CrossRef]
- Stanescu-Segall, D.; Balta, F.; Jackson, T.L. Submacular hemorrhage in neovascular age-related macular degeneration: A synthesis of the literature. Surv. Ophthalmol. 2016, 61, 18–32. [Google Scholar] [CrossRef] [PubMed]
- Rijken, D.C. 2 Plasminogen activators and plasminogen activator inhibitors: Biochemical aspects. Baillière’s Clin. Haematol. 1995, 8, 291–312. [Google Scholar] [CrossRef]
- Chang, W.; Garg, S.J.; Maturi, R.; Hsu, J.; Sivalingam, A.; Gupta, S.A.; Regillo, C.D.; Ho, A.C. Management of thick submacular hemorrhage with subretinal tissue plasminogen activator and pneumatic displacement for age-related macular degeneration. Am. J. Ophthalmol. 2014, 157, 1250–1257. [Google Scholar] [CrossRef]
- Chen, C.Y.; Hooper, C.; Chiu, D.; Chamberlain, M.; Karia, N.; Heriot, W.J. Management of submacular hemorrhage with intravitreal injection of tissue plasminogen activator and expansile gas. Retina 2007, 27, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Hassan, A.S.; Johnson, M.W.; Schneiderman, T.E.; Regillo, C.D.; Tornambe, P.E.; Poliner, L.S.; Blodi, B.A.; Elner, S.G. Management of submacular hemorrhage with intravitreous tissue plasminogen activator injection and pneumatic displacement. Ophthalmology 1999, 106, 1900–1907. [Google Scholar] [CrossRef] [PubMed]
- Hattenbach, L.O.; Klais, C.; Koch, F.H.; Gümbel, H.O. Intravitreous injection of tissue plasminogen activator and gas in the treatment of submacular hemorrhage under various conditions. Ophthalmology 2001, 108, 1485–1492. [Google Scholar] [CrossRef]
- Kamei, M.; Misono, K.; Lewis, H. A study of the ability of tissue plasminogen activator to diffuse into the subretinal space after intravitreal injection in rabbits. Am. J. Ophthalmol. 1999, 128, 739–746. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.I.; Drews-Botsch, C.; Sternberg, P.; Capone, A.; Aaberg, T.M. Submacular Hemorrhage Removal. Ophthalmology 1995, 102, 1393–1399. [Google Scholar] [CrossRef]
- Brown, D.M.; Kaiser, P.K.; Michels, M.; Soubrane, G.; Heier, J.S.; Kim, R.Y.; Sy, J.P.; Schneider, S. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N. Engl. J. Med. 2006, 355, 1432–1444. [Google Scholar] [CrossRef] [PubMed]
- Shienbaum, G.; Garcia Filho, C.A.; Flynn, H.W., Jr.; Nunes, R.P.; Smiddy, W.E.; Rosenfeld, P.J. Management of submacular hemorrhage secondary to neovascular age-related macular degeneration with anti-vascular endothelial growth factor monotherapy. Am. J. Ophthalmol. 2013, 155, 1009–1013. [Google Scholar] [CrossRef] [PubMed]
- Iacono, P.; Parodi, M.B.; Introini, U.; La Spina, C.; Varano, M.; Bandello, F. Intravitreal ranibizumab for choroidal neovascularization with large submacular hemorrhage in age-related macular degeneration. Retina 2014, 34, 281–287. [Google Scholar] [CrossRef]
- Bardak, H.; Bardak, Y.; Erçalık, Y.; Erdem, B.; Arslan, G.; Timlioglu, S. Sequential tissue plasminogen activator, pneumatic displacement, and anti-VEGF treatment for submacular hemorrhage. Eur J. Ophthalmol. 2018, 28, 306–310. [Google Scholar] [CrossRef]
- Avcı, R.; Yıldız, A.M.; Çınar, E.; Yılmaz, S.; Küçükerdönmez, C.; Akalp, F.D.; Avcı, E. Subretinal coapplication of tissue plasminogen activator and bevacizumab with concurrent pneumatic displacement for submacular hemorrhages secondary to neovascular age-related macular degeneration. Turk. J. Ophthalmol. 2021, 51, 38–44. [Google Scholar] [CrossRef]
- Lo, C.K.; Mertz, D.; Loeb, M. Newcastle-Ottawa Scale: Comparing reviewers’ to authors’ assessments. BMC Med. Res. Methodol. 2014, 14, 45. [Google Scholar] [CrossRef] [PubMed]
- Arias, L.; Monés, J. Transconjunctival sutureless vitrectomy with tissue plasminogen activator, gas and intravitreal bevacizumab in the management of predominantly hemorrhagic age-related macular degeneration. Clin. Ophthalmol. 2010, 4, 67–72. [Google Scholar] [CrossRef]
- Treumer, F.; Klatt, C.; Roider, J.; Hillenkamp, J. Subretinal coapplication of recombinant tissue plasminogen activator and bevacizumab for neovascular age-related macular degeneration with submacular haemorrhage. Br. J. Ophthalmol. 2010, 94, 48–53. [Google Scholar] [CrossRef] [PubMed]
- Guthoff, R.; Guthoff, T.; Meigen, T.; Goebel, W. Intravitreous injection of bevacizumab, tissue plasminogen activator, and gas in the treatment of submacular hemorrhage in age-related macular degeneration. Retin. 2011, 31, 36–40. [Google Scholar] [CrossRef] [PubMed]
- de Silva, S.R.; Bindra, M.S. Early treatment of acute submacular haemorrhage secondary to wet AMD using intravitreal tissue plasminogen activator, C3F8, and an anti-VEGF agent. Eye 2016, 30, 952–957. [Google Scholar] [CrossRef]
- Kitagawa, Y.; Shimada, H.; Mori, R.; Tanaka, K.; Yuzawa, M. Intravitreal Tissue Plasminogen Activator, Ranibizumab, and Gas Injection for Submacular Hemorrhage in Polypoidal Choroidal Vasculopathy. Ophthalmology 2016, 123, 1278–1286. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Roy, S.; Bansal, M.; Tinwala, S.; Aron, N.; Temkar, S.; Pujari, A. Modified Approach in Management of Submacular Hemorrhage Secondary to Wet Age-Related Macular Degeneration. Asia Pac. J. Ophthalmol. 2016, 5, 143–146. [Google Scholar] [CrossRef]
- Lee, J.P.; Park, J.S.; Kwon, O.W.; You, Y.S.; Kim, S.H. Management of Acute Submacular Hemorrhage with Intravitreal Injection of Tenecteplase, Anti-vascular Endothelial Growth Factor and Gas. Korean J. Ophthalmol. 2016, 30, 192–197. [Google Scholar] [CrossRef]
- Boiche, M.; Angioi-Duprez, K.; Conart, J.B.; Berrod, J.P. Treatment of hematomas in age related macular degeneration by vitrectomy and subretinal injection r-tPA: Preliminary results. J. Fr. D’ophtalmologie 2019, 42, E391–E397. [Google Scholar] [CrossRef]
- Erdogan, G.; Kirmaci, A.; Perente, I.; Artunay, O. Gravitational displacement of submacular haemorrhage in patients with age-related macular disease. Eye 2020, 34, 1136–1141. [Google Scholar] [CrossRef]
- Grohmann, C.; Dimopoulos, S.; Bartz-Schmidt, K.U.; Schindler, P.; Katz, T.; Spitzer, M.S.; Skevas, C. Surgical management of submacular hemorrhage due to n-AMD: A comparison of three surgical methods. Int. J. Retin. Vitr. 2020, 6, 27. [Google Scholar] [CrossRef] [PubMed]
- Rickmann, A.; Paez, L.R.; Della Volpe Waizel, M.; Bisorca-Gassendorf, L.; Schulz, A.; Vandebroek, A.C.; Szurman, P.; Januschowski, K. Functional and structural outcome after vitrectomy combined with subretinal rtPA Injection with or without additional intravitreal Bevacizumab injection for submacular hemorrhages. PLoS ONE 2021, 16, e0250587. [Google Scholar] [CrossRef] [PubMed]
- Ferris, F.L.; Kassoff, A.; Bresnick, G.H.; Bailey, I. New Visual Acuity Charts for Clinical Research. Am. J. Ophthalmol. 1982, 94, 91–96. [Google Scholar] [CrossRef]
- Casini, G.; Loiudice, P.; Menchini, M.; Sartini, F.; De Cillà, S.; Figus, M.; Nardi, M. Traumatic submacular hemorrhage: Available treatment options and synthesis of the literature. Int. J. Retin. Vitr. 2019, 5, 48. [Google Scholar] [CrossRef] [PubMed]
- van Zeeburg, E.J.; Cereda, M.G.; van Meurs, J.C. Recombinant tissue plasminogen activator, vitrectomy, and gas for recent submacular hemorrhage displacement due to retinal macroaneurysm. Graefe’s Arch. Clin. Exp. Ophthalmol. 2013, 251, 733–740. [Google Scholar] [CrossRef]
- Collinge, J.E.; Simirskii, V.N.; Duncan, M.K. Expression of tissue plasminogen activator during eye development. Exp. Eye Res. 2005, 81, 90–96. [Google Scholar] [CrossRef]
- Tripathi, R.C.; Tripathi, B.J. Tissue plasminogen activator therapy for the eye. Br. J. Ophthalmol. 2005, 89, 1390–1391. [Google Scholar] [CrossRef] [PubMed]
- Noma, H.; Yasuda, K.; Shimura, M. Involvement of Cytokines in the Pathogenesis of Diabetic Macular Edema. Int. J. Mol. Sci. 2021, 22, 3427. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, S.M.; Arepalli, S.; Ehlers, J.P. Current and Future Anti-VEGF Agents for Neovascular Age-Related Macular Degeneration. J. Exp. Pharmacol. 2021, 13, 905–912. [Google Scholar] [CrossRef]
- Wilkins, C.S.; Mehta, N.; Wu, C.Y.; Barash, A.; Deobhakta, A.A.; Rosen, R.B. Outcomes of pars plana vitrectomy with subretinal tissue plasminogen activator injection and pneumatic displacement of fovea-involving submacular haemorrhage. BMJ Open Ophthalmol. 2020, 5, e000394. [Google Scholar] [CrossRef]
- Ohayon, A.; Schwartz, S.; Loewenstein, A.; Seknazi, D.; Souied, E.H.; Barak, A. A Modified Surgical Technique for Submacular Injection. Ophthalmic Surg. Lasers Imaging Retin. 2021, 52, 551–555. [Google Scholar] [CrossRef] [PubMed]
- Tranos, P.; Tsiropoulos, G.N.; Koronis, S.; Vakalis, A.; Asteriadis, S.; Stavrakas, P. Comparison of subretinal versus intravitreal injection of recombinant tissue plasminogen activator with gas for submacular hemorrhage secondary to wet age-related macular degeneration: Treatment outcomes and brief literature review. Int. Ophthalmol. 2021, 41, 4037–4046. [Google Scholar] [CrossRef] [PubMed]
- Bell, J.E.; Shulman, J.P.; Swan, R.J.; Teske, M.P.; Bernstein, P.S. Intravitreal Versus Subretinal Tissue Plasminogen Activator Injection for Submacular Hemorrhage. Ophthalmic Surg. Lasers Imaging Retin. 2017, 48, 26–32. [Google Scholar] [CrossRef]
- Donato, L.; Scimone, C.; Alibrandi, S.; Scalinci, S.Z.; Rinaldi, C.; D’Angelo, R.; Sidoti, A. Epitranscriptome Analysis of Oxidative Stressed Retinal Epithelial Cells Depicted a Possible RNA Editing Landscape of Retinal Degeneration. Antioxidants 2022, 11, 1967. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).